Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 18
Double Burden of Malnutrition and Validity of Overweight/Obesity Indicators Among Students in the Democratic Republic of Congo: A Cross Sectional Study From the University of Kinshasa
Authors Makulo JR , Tshiswaka Mutombo T, Kamitalu Kabongo R, Tunda AK, Sumaili EK , Kisoka Lusunsi C, Beni Kasangwala B, Mulundu Lakwon C , Boluta B, Lubamba Mubiala G, Niangi Mawana T, Mbau Modju Jnr D, Betela CK, Mbala Kintoki F, Kasiam Lasi On'Kin JB, Bayauli Mwasa P, Ekolo Adiaka J, Lokangaka Odiko C, Mangani Nseka N , Ntumba Kayembe JM
Received 29 March 2025
Accepted for publication 26 June 2025
Published 28 June 2025 Volume 2025:18 Pages 2057—2065
DOI https://doi.org/10.2147/DMSO.S527585
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Rebecca Conway
Jean-Robert Makulo,1 Trésor Tshiswaka Mutombo,2 Ramsès Kamitalu Kabongo,3 Audace Kilolo Tunda,4 Ernest Kiswaya Sumaili,1 Christian Kisoka Lusunsi,2 Beni Beni Kasangwala,3 Christian Mulundu Lakwon,3 Benit Boluta,3 Guvanie Lubamba Mubiala,3 Tatiana Niangi Mawana,3 Diva Mbau Modju Jnr,3 Christelle Kimbe Betela,3 Fabien Mbala Kintoki,2 Jean-Bosco Kasiam Lasi On’Kin,5 Pascal Bayauli Mwasa,5 John Ekolo Adiaka,6 Charles Lokangaka Odiko,6 Nazaire Mangani Nseka,1 Jean-Marie Ntumba Kayembe6,7
1Nephrology Unit, Department of Internal Medicine, University Hospital of Kinshasa, Kinshasa, Congo; 2Cardiology Unit, Department of Internal Medicine, University Hospital of Kinshasa, Kinshasa, Congo; 3Students Health Centre, University of Kinshasa, Kinshasa, Congo; 4Department of Clinical Biology, University Hospital of Kinshasa, Kinshasa, Congo; 5Endocrinology Unit, Department of Internal Medicine, University Hospital of Kinshasa, Kinshasa, Congo; 6Administrative Management Committee of the University of Kinshasa, University of Kinshasa, Kinshasa, Congo; 7Pneumology Unit, Department of Internal Medicine, University Hospital of Kinshasa, Kinshasa, Congo
Correspondence: Jean-Marie Ntumba Kayembe, Email [email protected]
Background and Aims: The prevalence of overweight/obesity increases worldwide, including among students. BMI is a commonly used indicator to assess excess fat mass (FM). Our objective was to determine the prevalence of malnutrition (overweight, obesity and underweight) and correlation with FM among Congolese students, and to assess the correlation between BMI and FM measured by bioimpedance.
Methods: Cross-sectional study among students applying for registration at the University of Kinshasa during the 2024– 2025 academic year. Underweight, overweight and obesity were defined according to WHO criteria. FM values ≥ percentile 90 were considered as pathological. Student’s T test, Mann Whitney U, Pearson correlation, ROC curves and Youden index were the statistical analyses used, with p < 0.05.
Results: We included 13,381 students (59.7% male; mean age 19.8 ± 3.3 years). The prevalence of overweight and obesity in women (13.4%, 95% CI [12.5– 14.3] and 4.6% [4.1– 5.2]) was higher than in men (9.0% [8.4– 9.6] and 2.2% [1.9– 2.5]), p < 0.001. The underweight was also more frequent in women (10.2[9.4– 11.0]) than in men (9.0[8.4– 9.7]), p = 0.021. Women had a higher percentage of FM (median 23.6%, IQ 25: 15.1% and IQ 75: 30.1%) compared to men (13.8%; 10.4% and 19.4%), p < 0.01. The correlation between FM and BMI (r = 0.414; p < 0.001) was better in women compared to the men (r = 0.318, p < 0.001). The areas under the ROC curves plotted from BMI values and FM cut-offs ≥ percentile 90 (women = 35.8% and men = 26.0%), were 0.9038 in women (youden index = 0.73) versus 0.5899 in men (youden index = 0.14).
Conclusion: Overweight/obesity and underweight coexist among candidates particularly in women for student recruitment, at the University of Kinshasa, which illustrate the double burden of malnutrition in the academic young population. Using bioimpedance to assess body composition, BMI correlates better with FM in women; the usual thresholds defining overweight and obesity were not valid in men.
Keywords: obesity, fat mass, bioimpedance, correlation, students, DR Congo
Introduction
Over the past three decades, obesity has become a major public health problem worldwide. Reports from the World Health Organization (WHO) show that in 30 years, the prevalence of obesity has quadrupled in children and young people and doubled in adults.1 This worrying trend reflects the impact of a sedentary lifestyle, physical inactivity and the consequences of eating foods high in sugar and fat.2,3 This scourge suggests that a generation of young people will be more exposed to obesity-related diseases in the years to come. Indeed, obesity increases the risk of high blood pressure (HBP), type 2 diabetes, heart and lung diseases (sleep apnea, chronic obstructive pulmonary disease = COPD, pulmonary embolism).4 Obesity also affects bone health, reproductive health, and increases the risk of some cancers.5 According to the Organization for Economic Cooperation and Development (OECD), obesity and related diseases will reduce global life expectancy by 0.9 to 4.2 years over the next 30 years.6 In some developing countries, Studies also reports cases of underweight in the population.7 This can pose a paradoxical dual challenge in terms of nutrition and nutrition-related clinical pathologies.
Based on the WHO recommendation’s, a commonly used definition of obesity and underweight are determined by body mass index (BMI), calculated by dividing weight in kilograms by height in meters squared.8 While BMI is a good indicator of an individual’s overall corpulence and the risks associated with obesity, it does not take into account the proportion of fat mass (FM) of the individual.9 For example, a muscular athlete will have a high BMI but little FM, and he will only become a cardiovascular risk profile when he stops his physical activity and begins to accumulate FM. BMI also does not allow us to assess the distribution of adipose tissue. This is why its measurement is supplemented by other measurements such as waist circumference (WC), the waist-to-height ratio (WHR), the thickness of fat folds, etc.9 Another fundamental problem concerns the thresholds for BMI and WC which define obesity. These thresholds vary across age, gender and racial groups.10–12
Although widely reported in many studies in DR Congo,13–15 BMI and WC have not been studied compared to FM percentage per se. In young subjects, local studies of obesity, overweight and abdominal obesity have used thresholds reported in the literature. A few years ago, Kasiam et al, on a large sample largely made up of young Congolese living in the city of Kinshasa, had proposed local thresholds to define nutritional status/body composition disorders for men and women. They had considered the 97.5 percentiles in the population to define obesity (≥27 kg/m2) and abdominal obesity (≥90 cm).16 Very few studies have focused on students. In order to better assess the extent of obesity and underweight among Congolese students, this study conducted in a university setting had the main objective of determining the FM among students applying for registration at the University of Kinshasa (UNIKIN) during the 2024–2025 academic year. The secondary objectives were as follows: to study the correlation between FM and anthropometric parameters (BMI, WC, waist-to-height ratio = WHR).
Methods
Study Design, Setting and Population
The present cross-sectional study selected all students who applied to UNIKIN. It has been conducted at the UNIKIN student health centre as part of the students’ fitness exams. Data were collected from September 1, 2024 to October 31, 2024. The examiners were 12 internal medicine specialists, 30 general practitioners and 5 nurses. Every week, from Monday to Saturday, 200–400 students were examined.
Data Section
The parameters of interest examined were sociodemographic and anamnestic (age, sex, past medical history, province of origin), anthropometric (weight, height, BMI, WC, WHR), blood pressure (BP) and its components (systolic BP = SBP, and diastolic BP = DBP) and the body composition to assess the percentage of FM.
The BP was measured while sitting, with the left arm brought down to heart level using an Omron® BP monitors after a rest of at least 5 minutes. Two measurements spaced at least two minutes apart were taken for each student, and the second measurement was considered in this study. The weight was measured in a standing, barefoot and slightly vetus person using a Seca® scale. The height was measured using a ruler, the waist with a tape measure. FM was evaluated by the bioimpedance method using a TANIKABC 545 scale.
Definitions
Overweight, obesity and abdominal obesity were defined according to WHO and IDF.12,13
The cut-off point of obesity is ≥ 30 kg/m².
Hypertension was defined as SBP ≥ 140 mmHg and/or a DBP ≥ 90 mmHg or the notion of taking hypotensive treatment.17 Systolic HBP was defined as SBP ≥ 140 mmHg and a DBP < 90 mmHg; diastolic HBP was defined as DBP ≥ 90 mmHg and a SBP < 140 mmHg.17 Excess FM percentage was defined according to literature data (≥ 32% in women and ≥ 25% in men)18 and, the 90th percentile in the study population was also taken into account.
Statistical Analyses
Data were entered into Excel and transferred to SPSS 21 and STATA 17 software for statistical analyses. Local pathological FM thresholds were determined as percentile values (90th percentiles) with 95% confidence interval (CI) both in the general population and for each sex. Groups were compared using Pearson’s Chi-square and Student’s t tests. Results are presented in tables or figures as mean ± standard deviation (SD), median and interquartiles 25 and 75 or as absolute frequencies (percentage) with 95% confidence interval. We used Pearson’s correlation coefficient to measure the relationship between FM and other variables of interest (BMI, WC, WHR, SBP, DBP, age). Receiver Operating Characteristic (ROC) curves were used to represent sensitivity and 1- specificity for all possible cut-off values of obesity markers. The Youden index (J) was used to select the optimal probability threshold for each prediction. The cut-off point for having an acceptable Youden index was 50%. Any value below 50% denotes an absence to detect the excess of FM. A p-value < 0.05 was considered statistically significant.
Results
The present study included 13,831 students, with a great number of men (8,258 = 59.7%) than women (5,573 = 40.3%). Table 1 shows that they had a mean age of 19.8 ± 3.3 years, with a difference in favor of men. Overweight, obesity and abdominal obesity were more common in women. The proportion of young people with underweight was also more marked among women than men. Hypertension, especially its systolic component (SHBP), was more marked in men. The mean DBP was the same in the two groups. The mean percentage of FM was higher in women than men. All these parameters are presented in Table 1.
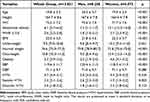 |
Table 1 Characteristcs of the Study Population |
Figure 1 shows the distribution of FM percentage in men and women. In the whole group, the median, 25th and 75th interquartile values of FM percentage were 16.5%, 11.5% and 25.1%.
 |
Figure 1 Percentage of FM distribution in men (a) and women (b). |
The comparison between men and women, showed a very significant difference in favor of women, namely 23.6%, 15.1% and 30.1% vs 13.8%, 10.4% and 19.4% (Figure 2).
 |
Figure 2 Median, 25th and 75th percentile values in the whole group (a), in men and women (b). |
Table 2 reports the correlation between the percentage of FM and anthropometric parameters and those related to blood pressure.
 |
Table 2 Pearson Correlation Between FM and Other Parameters |
Figure 2 Median, 25th and 75th percentile values in the whole group, in men and women.
In both men and women, BMI was the anthropometric parameter best correlated with FM. Among the components of blood pressure, DBP was the best correlated with FM; age was correlated with FM in men but not in women (Table 2).
The results of the sensitivity and 1-specificity of different anthropometric values in relation to the pathological FM thresholds of 25% in men and 32% in women are presented in Figure 3 (ROC curves) and in Table 3 which also reports the Youden indices for the most significant thresholds.
 |
Table 3 Youden Index (J) Based on Obesity Indicators/Literature Thresholds |
 |
Figure 3 ROC curves predicting anthropometric values associated with excess of FM (literature thresholds) in women (a) and men (b). |
In the study population, the 90th percentile values of FM were 26.0 (CI 95%: 25.5–26.5) in men versus 35.8 in women (CI 95%: 35.4–36.2), p < 0.05. Based on the FM values ≥ 90th percentiles (local thresholds), the ROC curves were redone (Figure 4) and the Youden indices are recalculated (Table 4).
 |
Table 4 Youden Index (J) Based on Obesity Indicators/Local Thresholds |
 |
Figure 4 ROC curves predicting anthropometric values associated with excess of FM (local thresholds) in women (a) and men (b). |
Discussion
This study found that many students are overweight, obese or underweight. It also showed that compared to bioimpedance, the usual BMI thresholds for defining obesity are valid in women but obsolete in men.
Obesity (3.2%) and overweight (11.8%) combined affected 14% of students examined. This is indicative of a neglected health problem among young people in the student environment of Kinshasa. The rise of overweight/obesity is influenced by changes in social environment (physical inactivity, food habits, transport systems as child and schools, etc).2,3 Kinshasa young people are not sufficiently active due to the loss of public recreation space, the increase in motorised transport and decrease in active transport (eg, cycling, walking). Specially in students, there is growing evidence that short sleep duration, poor sleep quality and a late bedtime are associated with a higher risk of obesity and insulin resistance.19,20 On the other hand, obesity might occur secondary to a range of medical conditions as hypothyroidism, hypercortisolism, treatment with glucocorticoids and some antiepileptics drugs.21
The prevalence found in the present study remains lower than that reported among young people of the same age in other countries. Prevalence of overweight/obesity in young people is highest (>30%) in many Pacific Island nations and is high (>20%) in several countries in America, Europe and north Africa.1,22–24 In sub-Saharan Africa (SSA), higher frequencies of obesity among adolescents and young adults have been reported in Ghana, Cameroon and South Africa.25–27 We explain this difference by the double burden of obesity and malnutrition. Indeed, approximately one in 10 students examined (9.2%) had a BMI below 18.5 kg/m2. In more than a third of the world’s countries, multiple forms of malnutrition are present simultaneously, particularly in SSA, South Asia and the East Asia and Pacific region.28 All these forms of malnutrition have a common denominator: food systems that fail to provide people with healthy, safe, sustainable and affordable food.
In the present study, women were more affected by obesity and overweight than men. It is well known that women are at higher risk of developing overweight or obesity due to physical inactivity, psychological comorbidities, factors such as pregnancy, hormones and genetic differences.29,30 Kapoor et al have shown that living with obesity/overweight is not only a consequence of a long-term energy imbalance between too many calories consumed (overeating) and too few calories expended (sedentary lifestyles), but is also linked to the way our brain develops.31 Their findings suggest that obesity risk may be influenced by how our brains develop early in life, which can be affected by both our genes and the environment we are exposed to. The researchers believe that understanding these developmental processes could be crucial to preventing and more effectively addressing the global obesity problem.
For epidemiological purposes and routine clinical practice, simple anthropometric measures are generally used as screening tools.1,8 BMI is used as an indirect measure of FM. According to our results, anthropometric measures of obesity (BMI, TT and WHR thresholds) were better correlated with FM in women compared to men, and the thresholds determining obesity had a good prediction of excess FM only in women. A woman’s FM is on average 20% compared to 13% for a man.32 Knowing that muscular activity is the source of energy expenditure during exercise, women have a lower capacity to produce energy and therefore less strength and endurance. In addition, men generally have thicker skin about 25%, and their density of the protein collagen is higher.33 This difference in density is not limited to the skin, since men also have stronger bones as well as denser tendons and ligaments than women.33 BMI thresholds defining obesity and overweight in young men should logically be reevaluated in our population. Body composition assessment is a more accurate measure for diagnosing obesity in this age group.
In the present study, approximately one out of 20 students had high blood pressure. SBP was higher in men compared to women. Our results corroborate data from the literature including data from the DR Congo EDS survey in 2024.34,35 The correlation between FM and DBP was positive, but was not significant between FM and SBP. It is known that diastolic hypertension indicates damage to the microcirculation: the small arteries, which have become rarer and thicker, resist the passage of blood, which increases the pressure.36 This phenomenon occurs before the stiffening of the large arteries, which causes systolic hypertension. DBP increases with age, reaching a plateau around 30–35 years of age, then decreases from the age of 60, due to the progressive increase in arterial stiffness.37 An isolated increase in DBP occurs in 2% to 8% of the population depending on the study, mainly in young patients with metabolic syndrome.37 In these young patients, the absolute short-term cardiovascular risk is low. However, in the long term, there is an increased risk of coronary heart disease and stroke.37
Despite the relevance of the results found, the study has some limitations. The study population was very selective. Other strata and age groups of the population were not included. Some determinants of nutritional status such as physical activity and dietary composition were not assessed. It would also be ideal to follow up the cases to better study the risk of occurrence of cardiovascular events linked to obesity in order to better determine the thresholds of FM and BMI at risk.
In conclusion, this study showed that a significant proportion of students admitted to the University of Kinshasa have overweight/obesity or underweight; which illustrates the double burden of malnutrition in academic population. These pathologies are more frequent in women. Using bioimpedance to assess body composition, the usual thresholds that define obesity are better correlated with fat mass in women; these thresholds are not valid in men. Hypertension is associated with obesity and the fat mass. These data encourage students to adopt healthy lifestyle.
Ethical Approval and Consent to Participate
The investigators agreed to conduct the present study in agreement with the principles of the Declaration of Helsinki. All data were fully anonymized before they have been accessed. The protocol (Approval number: ESP/CE/107/2024).
Acknowledgments
We thank the authorities of the University of Kinshasa.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was funded by the University of Kinshasa.
Disclosure
The authors declare that the research was conducted without any commercial or financial relationships that could be viewed as a potential conflict of interest.
References
1. World Obesity Day. 2022 – accelerating action to stop obesity.
2. Jebeile H, Kelly AS, O’Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022;10(5):351–365. doi:10.1016/S2213-8587(22)00047-X
3. Mambrini SP, Menichetti F, Ravella S, et al. Ultra-Processed Food Consumption and Incidence of Obesity and Cardiometabolic Risk Factors in Adults: a Systematic Review of Prospective Studies. Nutrients. 2023;15(11):2583. doi:10.3390/nu15112583
4. Sarma S, Sockalingam S, Dash S. Obesity as a multisystem disease: trends in obesity rates and obesity-related complications. Diabetes Obes Metab. 2021;23(1):3–16. doi:10.1111/dom.14290
5. Friedenreich CM, Ryder-Burbidge C, McNeil J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biologic mechanisms. Mol Oncol. 2021;15(3):790–800. doi:10.1002/1878-0261.12772
6. OECD. The Heavy Burden of Obesity: The Economics of Prevention. 2019. doi:10.1787/67450d67-en
7. Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. doi:10.1016/S0140-6736(19)32497-3
8. Engin A. The Definition and Prevalence of Obesity and Metabolic Syndrome. Adv Exp Med Biol. 2017;960:1–17. doi:10.1007/978-3-319-48382-5_1
9. Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177–189. doi:10.1038/s41574-019-0310-7
10. Caleyachetty R, Barber TM, Mohammed NI, et al. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2021;9(7):419–426. doi:10.1016/S2213-8587(21)00088-7
11. Okobi OE, Beeko PKA, Nikravesh E, et al. Trends in Obesity-Related Mortality and Racial Disparities. Cureus. 2023;15(7):e41432. doi:10.7759/cureus.41432
12. Prasad DS, Kabir Z, Revathi Devi K, Peter PS, Das BC. Gender differences in central obesity: implications for cardiometabolic health in South Asians. Indian Heart J. 2020;72(3):202–204. doi:10.1016/j.ihj.2020.04.008
13. Mapatano MA, Muyer MC, Buntinx F, et al. Obesity in diabetic patients in Kinshasa, Democratic Republic of Congo. Acta Clin Belg. 2007;62(5):293–297. doi:10.1179/acb.2007.044
14. Mawaw PM, Yav T, Mukuku O, et al. Increased prevalence of obesity, diabetes mellitus and hypertension with associated risk factors in a mine-based workforce, Democratic Republic of Congo. Pan Afr Med J. 2019;34:135. doi:10.11604/pamj.2019.34.135.20226
15. Masimango MI, Sumaili EK, Wallemacq P, et al. Prevalence and Risk Factors of CKD in South Kivu, Democratic Republic of Congo: a Large-Scale Population Study. Kidney Int Rep. 2020;5(8):1251–1260. doi:10.1016/j.ekir.2020.05.028
16. Lasi On’kin JB K, Longo-Mbenza B, Nge Okwe A, Kangola Kabangu N. Survey of abdominal obesities in an adult urban population of Kinshasa, Democratic Republic of Congo. Cardiovasc J Afr. 2007;18(5):300–307.
17. Carey RM, Moran AE, Whelton PK. Treatment of Hypertension: a Review. JAMA. 2022;328(18):1849–1861. doi:10.1001/jama.2022.19590
18. Meeuwsen S, Horgan GW, Elia M. The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin Nutr Edinb Scotl. 2010;29(5):560–566. doi:10.1016/j.clnu.2009.12.011
19. Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, et al. Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc Health. 2022;6(3):158–170. doi:10.1016/S2352-4642(21)00374-6
20. Chaput JP, McHill AW, Cox RC, et al. The role of insufficient sleep and circadian misalignment in obesity. Nat Rev Endocrinol. 2023;19(2):82–97. doi:10.1038/s41574-022-00747-7
21. Prospective Studies Collaboration. Whitlock G, Lewington S, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies Lancet Lond Engl. 2009;373(9669):1083–1096. doi:10.1016/S0140-6736(09)60318-4.
22. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet Lond Engl. 2024;403(10431):1027–1050. doi:10.1016/S0140-6736(23)02750-2.
23. Jaacks LM, Vandevijvere S, Pan A, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–240. doi:10.1016/S2213-8587(19)30026-9
24. Aounallah-Skhiri H, Traissac P, El Ati J, et al. Nutrition transition among adolescents of a south-Mediterranean country: dietary patterns, association with socio-economic factors, overweight and blood pressure. A cross-sectional study in Tunisia. Nutr J. 2011;10(1):38. doi:10.1186/1475-2891-10-38
25. Ofori EK, Angmorterh SK. Relationship between physical activity, body mass index (BMI) and lipid profile of students in Ghana. Pan Afr Med J. 2019;33:30. doi:10.11604/pamj.2019.33.30.17889
26. Ebouki RE, Pefura-Yone EW, Sobngwi E, et al. Prévalence et Facteurs Associés à l’Excès de Poids et à l’Obésité Centrale chez les Enfants et les Adolescents Camerounais. Health Sci Dis. 2023;24(5):4407. doi:10.5281/hsd.v24i5.4407
27. Negash S, Agyemang C, Matsha TE, Peer N, Erasmus RT, Kengne AP. Differential prevalence and associations of overweight and obesity by gender and population group among school learners in South Africa: a cross-sectional study. BMC Obes. 2017;4(1):29. doi:10.1186/s40608-017-0165-1
28. Wells JC, Sawaya AL, Wibaek R, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet Lond Engl. 2020;395(10217):75–88. doi:10.1016/S0140-6736(19)32472-9
29. Singh P, Covassin N, Marlatt K, Gadde KM, Heymsfield SB. Obesity, Body Composition, and Sex Hormones: implications for Cardiovascular Risk. Compr Physiol. 2021;12(1):2949–2993. doi:10.1002/cphy.c210014
30. Srikanthan P, Horwich TB, Calfon Press M, Gornbein J, Watson KE. Sex Differences in the Association of Body Composition and Cardiovascular Mortality. J Am Heart Assoc. 2021;10(5):e017511. doi:10.1161/JAHA.120.017511
31. Kapoor N, Arora S, Kalra S. Gender Disparities in People Living with Obesity - An Unchartered Territory. J Life Health. 2021;12(2):103–107. doi:10.4103/jmh.jmh_48_21
32. Muth ND. What are the guidelines for percentage of body fat loss. Am Counc Exerc ACE Ask Expert Blog. 2009.
33. Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med Auckl NZ. 2006;36(3):239–262. doi:10.2165/00007256-200636030-00005
34. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet Lond Engl. 2002;360(9349):1903–1913. doi:10.1016/s0140-6736(02)11911-8
35. RDC-Institut National de la Statistique, École de Santé Publique de Kinshasa et ICF. RDC, Enquête Démographique et de Santé 2023–24: Rapport des indicateurs clés. Kinshasa, RDC et Rockville, Maryland, USA: ICF; 2024. Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwi155WNpvaLAxVYAtsEHVN0DyEQFnoECBkQAQ&url=https%3A%2F%2Fwww.dhsprogram.com%2Fpubs%2Fpdf%2FPR156%2FPR156.pdf&usg=AOvVaw3yrxkh3PlrxFTEjaETbSwl&opi=89978449.
36. Zhao J, Hong F, Lu S, Zhou F, Xu M. Adolescent Hypertension Induced by Obesity and the Efficacy of Comprehensive Intervention. Altern Ther Health Med. 2023;29(5):6–11.
37. Mancia G, Kreutz R, Brunström M, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41(12):1874–2071. doi:10.1097/HJH.0000000000003480
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

