Back to Journals » Open Access Emergency Medicine » Volume 16
Droperidol Plus Diphenhydramine for Symptom Improvement in Suspected Cannabinoid Hyperemesis Syndrome: A Prospective Cohort Study
Authors Chopra Q, Peyko V , Lee JA , Puhalla L, Gemmel DJ, Bolotin T
Received 28 June 2024
Accepted for publication 20 November 2024
Published 26 November 2024 Volume 2024:16 Pages 267—273
DOI https://doi.org/10.2147/OAEM.S473627
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Quincy Chopra,1 Vincent Peyko,2 Jessica Annie Lee,3 Leo Puhalla,3 David J Gemmel,4 Todd Bolotin5,6
1Department of Emergency Medicine, Palmdale Regional Medical Center, Palmdale, CA, USA; 2Department of Pharmacy, Mercy Health St. Elizabeth Boardman Hospital, Boardman, OH, USA; 3Northeastern Ohio Medical University, College of Medicine, Rootstown, OH, USA; 4Department of Research, Mercy Health St Elizabeth Youngstown Hospital, Youngstown, OH, USA; 5Department of Emergency Medicine, Mercy Health St. Elizabeth Boardman Hospital, Boardman, OH, USA; 6Lake Erie College of Osteopathic Medicine, College of Medicine, Erie, PA, USA
Correspondence: Vincent Peyko, Department of Pharmacy, Mercy Health St. Elizabeth Boardman Hospital, 8401 Market St, Boardman, OH, 44512, USA, Email [email protected]
Background: Cannabinoid Hyperemesis Syndrome (CHS) is characterized by recurrent, paroxysmal episodes of nausea, vomiting, and abdominal discomfort in chronic cannabis users. Optimized CHS treatment data remain limited. Recent prospective evidence have demonstrated haloperidol superiority over ondansetron. Retrospective data suggest the utility of droperidol, a dopamine antagonist like haloperidol, for treating acute CHS.
Objective: To prospectively assess the utility of droperidol plus diphenhydramine to mitigate common CHS symptoms.
Methods: This was a multicenter, prospective interventional study in the emergency department (ED). Participants were administered a study regimen of droperidol and diphenhydramine to treat CHS after enrollment. The primary outcome measure was the change in VAS scores within the droperidol prospective cohort. Symptoms of nausea, vomiting, and abdominal pain were measured using a visual analogue scale (VAS) up to 120 minutes. Secondary measures assessed include repeat visits to the ED within seven days.
Results: Amongst 47 droperidol participants, VAS for nausea and vomiting declined from baseline 8.3± 2.0 to 3.1± 3.3 at 30 minutes post treatment (p < 0.05), and 1.4± 2.4 at 120 minutes (p < 0.05). For abdominal pain, VAS mean was 7.8± 2.4 at baseline declining to 3.6± 2.9 at 30 minutes (p < 0.05) and 1.7± 2.9 at 120 minutes (p < 0.05). Return to the ED within 7 days following droperidol was 12.9% (n=47).
Conclusion: This trial shows significant improvement in symptoms from baseline, 30 and 120 minutes post-treatment and return to the ED within a week post treatment with the study regimen.
Keywords: cannabinoid hyperemesis syndrome, nausea, vomiting, abdominal pain, droperidol
Introduction
Background
Cannabinoid Hyperemesis Syndrome (CHS) was initially characterized by recurrent, paroxysmal episodes of nausea, vomiting, and abdominal discomfort in chronic cannabis users, relieved by frequent hot bathing, followed by symptom-free periods.1 Over time, hot bathing and symptom-free periods were omitted from the definition, which now considers hyperemesis to follow a cyclic pattern over weeks to months, often for many years, against a background of cannabis abuse.2 The exact cause remains speculative, making CHS primarily a diagnosis of exclusion, however genetic mutations explaining its pathophysiology have been identified3,4 Distinct features of CHS include resistance to traditional antiemetics and the need for prolonged abstinence as a cure.3
Anecdotal evidence suggests benzodiazepines, propranolol, topical capsaicin, and haloperidol as effective emergency treatments.5–9 A randomized, controlled study has demonstrated haloperidol to be superior to ondansetron for the acute treatment of CHS.3 Retrospective data suggests the utility of droperidol, a dopamine antagonist like haloperidol, for treating acute CHS.2 Diphenhydramine also has antiemetic properties and has the added benefit by counteracting the extrapyramidal reactions associated with droperidol.10 Offsetting potential extrapyramidal symptoms are why diphenhydramine was part of the study protocol and administered to all patients with droperidol in our study. While droperidol carries a boxed warning for QTc-interval prolongation, recent prospective data suggest the risk of complication, including torsades de pointes, to be minimal and rare, even at high doses.2 Indeed, in a 2021 policy statement, The American Academy of Emergency Physicians consider droperidol safe for the treatment of nausea, vomiting, headaches, and agitation in the emergency department (ED).11
Since 2000, teen cannabis use in the United States is up 245%, with 43% of young adults between 19 and 30 years reporting cannabis use in 2021.12,13 In 2019, 48.2 million Americans (18%) used cannabis at least once and 3 of 10 people who use cannabis have cannabis use disorder.14 Drug shortages are not resolving, new shortages are increasing, and active shortages are the highest since 2014.15 The continued increase use and abuse of cannabis in the United States, coupled with volatile availability of effective agents to treat CHS, suggests the value of validating the utility of more agents, like droperidol plus diphenhydramine, to add to the armamentarium.
Goals of This Investigation
Given haloperidol’s superiority to ondansetron, retrospective evidence of droperidol utility, and pharmacological similarity of the agents, we conducted a prospective, interventional study to determine whether droperidol plus diphenhydramine reduces nausea, vomiting, and abdominal pain for acute CHS in the ED and limits return to the ED within 7 days.
Methods
Study Design
This prospective, multicenter, open-label interventional study was conducted at four academic emergency EDs, with a combined annual ED volume of 169,000. The study was approved by the Mercy Health Youngstown regional institutional review board and registered at ClinicalTrials.gov (NCT05244460).
Patient Selection
From February 2022 to January 2023, consecutive eligible patient’s ≥18 years of age identified by ED providers with a working diagnosis of CHS were screened for participation. To be eligible, the patient had to report at least weekly cannabis use for one year or more and three episodes of emesis in a cyclic pattern separated by more than one month during the preceding two years and a viable contact telephone number. Prisoners, individuals allergic or intolerant to the study drugs or with QTc-interval ≥440 milliseconds (males) or ≥450 milliseconds (females) on electrocardiogram on the day of presentation, or pregnant females were excluded.
After consenting to participate, subjects were asked to rate their baseline nausea and abdominal pain on two separate ten point visual analog scales (VAS), with higher scores to indicate greater severity of symptoms. Subjects were then administered intravenous droperidol 2.5 mg and intravenous diphenhydramine 25 mg. Serial measurements of VAS scores for nausea and abdominal pain were assessed at 30, 60, 90, and 120 minutes after pharmacologic intervention. Subjects were contacted by phone at 24 and 48 hours after ED discharge and values from the VAS scale for nausea, vomiting and abdominal pain were recorded. Per protocol, other medications and even additional doses of droperidol could be administered at the discretion of the treating physician. Additional data beyond the VAS scores collected included: age, sex, weight, temperature, blood pressure, respiratory rate, pulse, oxygen saturation, basic metabolic panel, urine ketone values, toxicology results, QTc interval, beta-hydroxybutyrate levels, total white blood count, and history of cannabis use.
Outcomes
The primary outcome measure was the change in VAS scores amongst patients receiving droperidol plus diphenhydramine from baseline to 120 minutes. VAS scores were assessed by telephone follow-up at 24 and 48 hours. Secondary measures evaluated include repeat visits to the ED within seven days.
Analysis
All analyses were performed on a per protocol basis on cases with complete data. Statistical analysis was performed using SPSS 25.0 (IBM Corp Released 2017. IBM SPSS Statistics for Windows, Version 25.0 Armonk, NY; IBM Corp). Continuous variables were expressed as mean and standard deviation with categorical data as percentages. Student’s t-test and chi-square test were used for continuous and categorical variables respectively.
Results
Enrolled patients (n=47) are described in Table 1. Among patients diagnosed with CHS, average age was 34 ± 11 years; 27 patients (57%) were male. Thirty-three (70%) of CHS patients reported daily cannabis use, with the remaining patients reporting weekly cannabis use. Twenty-three (49%) of CHS patients reported cannabis use in the last 24 hours. An additional 10 patients (21%) reported use in the last 48 hours. CHS patients reported 8.8 ± 8.5 joints smoked per week and the average age at initiation of cannabis use was 18.7 ± 8.9 years (range 9–51). One-third of CHS patients reported initiation of cannabis use before age 16.
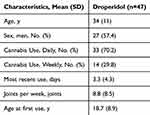 |
Table 1 Patient Characteristics |
Nausea and vomiting and abdominal pain improved rapidly after droperidol plus diphenhydramine administration. See Table 2. For nausea and vomiting, baseline VAS was 8.3 2.0 and 30 minute VAS was 3.1 ± 3.2, dropping 63% (t=11.536, p < 0.001). Mean VAS for abdominal pain at ED presentation was 7.8 ± 2.4, declining 54% to 3.6 ± 2.9 at 30 minutes (t=11.147, p < 0.001). Sustained decreased nausea and vomiting and abdominal pain symptoms were recorded on VAS at 60 minutes, reaching nadir at 120 minutes.
 |
Table 2 Visual Analog Scale for Patients Administered Droperidol |
On telephonic follow-up at 24 and 48 hours, VAS for both nausea and vomiting and abdominal pain remained significantly below baseline VAS in the ED. While some rebound occurred at 24 hours post ED discharge on both nausea and vomiting and abdominal pain VAS, patient evaluation of symptoms was similar to those observed at 30 minutes in the ED and further declined at 48 hours. At 24 hours, 33 patients (70%) were lost to follow-up and 39 patients (83%) were lost to follow-up at 48 hours.
Six patients receiving droperidol plus diphenhydramine (12.8%) returned to the ED within 7 days.
Discussion
This multicenter, prospective interventional study demonstrates effectiveness of intravenous droperidol plus diphenhydramine in controlling symptoms associated with CHS, including nausea, vomiting and abdominal pain. Similar to Ruberto et al, the average improvement in all measured variables exceeded the pre-specified minimal clinically significant difference of 20 mm, representing a meaningful improvement in symptoms.3,16 In our study, 6/47 (12.8%) returned to the ED within 7 days compared to 4/13 (30.8%) in Ruberto et al3. Subjects in both studies were required to remain in the ED for 120 minutes per study parameters. Some patients clinically improved by 30 minutes and may have been considered for discharge prior to 120 minutes.
While this study did have a low number of participants, clinically and statistically significant improvements with droperidol plus diphenhydramine suggest its utility for CHS treatment.
While the underlying cause of CHS is uncertain, growing evidence suggests the effectiveness of dopamine antagonists like droperidol and haloperidol for the emergency treatment of CHS.17 Furthermore, genomics of the CHS affecting two dopamine genes explain the relationship of antagonists to clinical improvement.18 Cannabis has well-known antiemetic properties, but paradoxically chronic use may lead to CHS.19 Endogenous cannabinoids bind to the G protein-coupled cannabinoid receptors Cannabinoid receptor one (CB1) and Cannabinoid receptor two (CB2).18 The CB1 receptors located in the central nervous system and nerves throughout the gastrointestinal tract can modulate certain gut functions like motility and secretion.19 It is believed antiemetic properties of cannabinoids are mediated through CB1 activation in the hypothalamus and pro-emetic properties from CB1 activation in the gastrointestinal tract. Activating CB1 receptors by endogenous cannabinoids suppress activation of hypothalamic-pituitary axis (HPA) and sympathetic nervous system in stress.19
The active compound in cannabis, Δ-9-tetrahydrocannabinol (THC) binds CB1 and CB2 receptors. Chronic THC exposure leads to accumulation in adipose cells and prolonged supranormal levels of THC desensitize and downregulate CB1 receptors, thus increasing the stress response may induce CHS.19
Cannabidiol is a cannabinoid molecule in cannabis that has anti-emetic properties at low doses but is pro-emetic at higher doses.19 Like THC, accumulation of cannabidiol in chronic cannabis users may play a role in CHS.19
Dopamine receptors (D2 and D3) in the medulla are involved in the pathophysiology of emesis.20 Antagonists of dopamine receptors are often used as antiemetics.19 Droperidol is a butyrophenone, which mainly works through D2 antagonism. It also has histamine and serotonin antagonistic properties, alpha-2-agonist, gamma-aminobutyric acid (GABA) agonist (at low dose) and antagonist (at high dose), anticholinesterase agent, muscarinic and nicotinic antagonist, and blocks sodium channels.20,21
Histamine activates neurons in the medulla that are implicated in nausea, emesis, and motion sickness. Serotonin also plays a major role in regulation of emesis.19
Droperidol plus diphenhydramine has demonstrated effectiveness for the treatment of refractory hyperemesis gravidarum.10 Histamine receptors (H1 and H2) are located in the central nervous system (CNS) in multiple sites including the postrema and vomiting center in the vestibular nuclei.22 Diphenhydramine is an H1 receptor antagonist that can block the effects of histamine in the CNS, and has anticholinergic properties, which can block muscarinic receptors at the same sites, serving as an antiemetic, which is why this study cannot credit the antiemetic effect to droperidol alone.22
While the exact mechanism of CHS remains to be elucidated, the effects of THC and cannabidiol may play a role in CHS development and the effects of droperidol on D2, serotonin, and histamine antagonism demonstrate why droperidol leads to cessation of nausea and vomiting in CHS.19
Droperidol has demonstrated better effect than haloperidol in IM administration of agitated patients, which are attributed to more rapid peak levels of droperidol versus haloperidol when given IM, where as intravenously, both are rapidly absorbed.23
Data of post-surgical patients and incidence of vomiting demonstrate that haloperidol has a faster onset of action than droperidol, but the antiemetic effect of droperidol lasts longer.24 Of the 65 patients in this study, haloperidol performed much better in the first hour, but by hour 3 and between 4 and 24 hours, droperidol was about twice as effective as haloperidol at decreasing the incidence of vomiting.24
Vomiting is a complicated reflex mediated by the vomiting center and influenced by the chemoreceptor trigger zones in the medulla.24 Butryophenones, like droperidol and haloperidol, are thought to elicit their effects of vomiting by blocking chemoreceptor zone excitation and inhibiting excitation of the vomiting center directly.20,24
Data indicate that antiemetic activity of butyrophenones are due to unaltered butyrophenone molecule, metabolites not being effective antiemetics, and are primarily dependent on blockade of dopamine receptors in the chemoreceptor trigger zone.24 Suggesting that while unaltered haloperidol probably penetrates the chemoreceptor zone in the medulla faster, droperidol is probably retained at the site longer or is more effective as an antiemetic than haloperidol.24
Limitations
This study was not blinded or placebo-controlled, leading to potential bias specific to effect. All eligible subjects who consented were entered and treated with the experimental protocol. Subjects were recruited from a convenience sample of patients who presented to the ED meeting the pre-specified definition of CHS. While the patients represent a convenience sample, self-reported cannabis use, frequency of use, and age at initiation of cannabis use strongly suggest a consecutive series of CHS patients were identified and suggest that findings would be generalizable to similar patients. The subjects were aware they were in an experimental protocol and this could have biased their reported response to the treatment in favor of the intervention. All cases were presumptive CHS. However, CHS can only be distinguished from cyclic vomiting syndrome (CVS) if symptoms resolve after cannabis abstinence.24 With CHS, symptoms would resolve with cannabis abstinence, whereas with CVS they would not and this was not assessed in our study.23 In assessing return to ED within 7 days, patients may have sought care at a different site, not affiliated with the study, skewing the results for return to ED within 7 days. High dropout rates are common in studies involving cannabis users.25–27 While our study also had a high dropout rate, exactly why this occurs in cannabis-related studies requires further research.27 Both droperidol and diphenhydramine are antiemetic medications. Because diphenhydramine is also an antiemetic, the effect of droperidol cannot be said to be autonomous of diphenhydramine. The population studied was from four distinct emergency departments, but was in a relatively small geographic location, which could threaten the external validity of these results. The number of individuals contacted for 24 and 48-hour follow-up was low which could bias the results in favor of the intervention. The limitation related to relatively low response to telephone follow-up is likely to be recurrent in any cohort of frequent cannabis users.
Conclusions
In summary, droperidol plus diphenhydramine is a safe and effective medication in the treatment of CHS. This combination effectively decreases nausea, vomiting, and abdominal pain and is associated with decreased return to ED within one week. Further study in the form of a prospective, randomized, blinded trial of droperidol ± diphenhydramine versus haloperidol or other agents should be performed to elucidate which are the most effective agents for CHS.
Data Sharing Statement
The entire de-identified dataset, data dictionary and analytic code for this investigation are available upon request, from the date of article publication by contacting Quincy Chopra, MD at [email protected]
Ethics and Consent Statements
The study was approved by the Mercy Health Youngstown regional institutional review board and registered at ClinicalTrials.gov (NCT05244460). All patient data was kept confidential and the study was in compliance with the Declaration of Helsinki. All participants were informed about the purpose of this trial prior to enrollment.
Funding
Funding for this study came in the support of an academic grant from Lake Erie College of Medicine (Grant #: J2021-17). The authors have no personal sponsorship, financial support, or involvement with organization(S) having a financial interest in the subject matter.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Allen GH, de Moore GM, Heddle R, et al. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis use. Gut. 2004;53:1566–1570. doi:10.1136/gut.2003.036350
2. Lee C, Greene SL, Wong A. The utility of droperidol in the treatment of cannabinoid hyperemesis syndrome. Clin Toxicol. 2019;57:773–777. doi:10.1080/15563650.2018.1564324
3. Ruberto AJ, Sivilotti ML, Forrester S, et al. Intravenous haloperidol versus ondansetron for cannabis hyperemesis syndrome (HaVOC): a randomized, controlled trial. Ann Emerg Med. 2021;77:613–619. doi:10.1016/j.annemergmed.2020.08.021
4. Bonnet U. Cannabis-related cyclic/episodic hyperemesis conditions: from suspected to definitive cannabinoid hyperemesis syndrome. Med Princ Pract. 2022;31:497–498. doi:10.1159/000525991
5. Kheifets M, Karniel E, Landa D, et al. Resolution of cannabinoid hyperemesis syndrome with benzodiazepines: a case series. Isr Med Assoc J. 2019;21:404–407.
6. Wagner S, Hoppe J, Zuckerman M, et al. Efficacy and safety of topical capsaicin for cannabinoid hyperemesis syndrome in the emergency department. Clin Toxicol. 2020;58:471–475. doi:10.1080/15563650.2019.1660783
7. Richards JR, Dutczak O. Propranolol treatment of cannabinoid hyperemesis syndrome: a case report. J Clin Psychopharmacol. 2017;37:482–484. doi:10.1097/JCP.0000000000000735
8. Witsil JC, Mycyk MB. Haloperidol, a novel treatment for cannabinoid hyperemesis syndrome. Am J Ther. 2017;24:e64–e67. doi:10.1097/MJT.0000000000000157
9. Hickey JL, Witsil JC, Mycyk MB. Haloperidol for treatment of cannabinoid hyperemesis syndrome. Am J Emerg Med. 2013;31(6):e5–6. doi:10.1016/j.ajem.2013.02.021
10. Ferreira E, Bussières JF, Turcotte V, et al. Case-control study comparing droperidol plus diphenhydramine with conventional treatment in hyperemesis gravidarum. J Pharm Technol. 2003;19:349–354. doi:10.1177/875512250301900602
11. American College of Emergency Physicians. Policy statement. Use of droperidol in the emergency department. 2021. Available from: https://www.acep.org/siteassets/new-pdfs/policy-statements/use-of-droperidol-in-the-emergency-department.pdf.
12. National Institutes of Health. Marijuana and hallucinogen use among young adults reached all-time high in 2021. 2022. Available from: https://www.nih.gov/news-events/news-releases/marijuana-hallucinogen-use-among-young-adults-reached-all-time-high-2021.
13. Rideout N. Teen cannabis abuse has increased 245% over 20 years, study finds. 2022. Available from: https://news.ohsu.edu/2022/12/07/teen-cannabis-abuse-has-increased-245-over-20-years-study-finds.
14. Centers for Disease Control and Prevention. Marijuana and public health. 2021. Available from: https://www.cdc.gov/marijuana/data-statistics.htm.
15. American Society of Health-systems Pharmacists. Drug shortage statistics. 2023. Available from: https://www.ashp.org/drug-shortages/shortage-resources/drug-shortages-statistics.
16. Meek R, Egerton-Warburton D, Mee M, et al. Measurement and monitoring of nausea severity in emergency department patients: a comparison of scales and exploration of treatment efficacy measures. Acad Emerg Med. 2015;22:685–693. doi:10.1111/acem.12685
17. Macht M, Mull A, McVaney K, et al. Comparison of droperidol and haloperidol for use by paramedics: assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18:375–380. doi:10.3109/10903127.2013.864353
18. Russo E, Spooner C, May L, et al. Cannabinoid hyperemesis syndrome survey and genomic investigation. Cannabis Cannabinoid Res. 2022;7:336–344. doi:10.1089/can.2021.0046
19. Richards J, Gordon B, Danielson A, et al. Pharmacologic treatment of cannabinoid hyperemesis syndrome: a systematic review. Pharmacotherapy. 2017;37:725–734. doi:10.1002/phar.1931
20. Lai PC, Huang Y. Evidence-based review and appraisal of the use of droperidol in the emergency department. Tzu Chi Med J. 2018;30:1–4. doi:10.4103/tcmj.tcmj_195_17
21. Atkins M, Lopez IG, Kuo B. Nausea and vomiting. Compr Pharmacol. 2022:57–92.
22. Shaefer TS, Zito PM. Antiemetic histamine H1 receptor blockers. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022.
23. Thomas H, Schwartz E, Petrelli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21:407–413. doi:10.1016/S0196-0644(05)82660-5
24. Loeser EA, Bennett G, Stanley T, et al. Comparison of droperidol, haloperidol, and prochlorperazine as postoperative antiemetics. Can Anaesth Soc J. 1979;26:125–127. doi:10.1007/BF03013781
25. Stockings E, Campbell G, Hall W, et al. Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled observational studies. Pain. 2018;159:1932–1954. doi:10.1097/j.pain.0000000000001293
26. Vuilleumier C, Scherbaum N, Bonnet U, Roser P. Cannabinoids in the treatment of cannabis use disorder: systematic review of randomized control trials. Front Psychiatry. 2022;13:867878. doi:10.3389/fpsyt.2022.867878
27. Lintzeris N, Bhardwaj A, Mills L, et al. Nabiximols for the treatment of cannabis dependence. JAMA Intern Med. 2019;179:1242–1253. doi:10.1001/jamainternmed.2019.1993
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

