Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Earlier Use of Long-Acting Injectable Paliperidone Palmitate Once-Monthly versus Oral Antipsychotics in Patients with Schizophrenia: An Integrated Patient-Level Meta Analysis of the PROSIPAL and PRIDE Studies
Authors Sajatovic M, Doring M, Lopena OJ, Johnston K, Turkoz I , Josiah N, Obando C
Received 25 July 2024
Accepted for publication 1 November 2024
Published 21 November 2024 Volume 2024:20 Pages 2227—2235
DOI https://doi.org/10.2147/NDT.S427227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Taro Kishi
Martha Sajatovic,1 Monica Doring,2 Oliver J Lopena,2 Karen Johnston,2 Ibrahim Turkoz,3 Nia Josiah,4 Camilo Obando2
1University Hospitals Cleveland Medical Center, Case Western Reserve University School of Medicine, Cleveland, OH, USA; 2Janssen Scientific Affairs, LLC, a Johnson & Johnson company, Titusville, NJ, USA; 3Janssen Research & Development, LLC, Titusville, NJ, USA; 4The University of Pennsylvania School of Nursing, Philadelphia, PA, USA
Correspondence: Monica Doring, Janssen Scientific Affairs, LLC, a Johnson & Johnson company, 1125 Trenton Harbourton Road, Titusville, 08560, NJ, Email [email protected]
Purpose: A previous integrated patient-level analysis demonstrated a significant benefit of implementing once-monthly injectable paliperidone palmitate (PP1M) earlier in the treatment course for schizophrenia. Earlier therapeutic interventions during the first 3– 5 years after disease onset can positively impact long-term outcomes in schizophrenia. This present analysis evaluated the risk of relapse both overall and by different durations of illness (0– 3 years, > 3– 5 years, and > 5 years from diagnosis) in adult patients with schizophrenia who received PP1M or oral antipsychotics (OAPs).
Patients and Methods: This analysis included integrated patient-level data from the Paliperidone Palmitate Research in Demonstrating Effectiveness (PRIDE) and Prevention of Relapse with Oral Antipsychotics versus Injectable Paliperidone Palmitate (PROSIPAL) studies. Both studies assessed relapse as the primary outcome in patients treated either PP1M or OAPs.
Results: Overall, the risk of relapse was reduced by 31% with PP1M compared to OAP (HR 0.69; 95% CI [0.56– 0.86], P < 0.001). Fewer relapses were observed with PP1M versus OAP in the 0– 3-year subgroup (15.8% and 21.7%, respectively), > 3– 5-year subgroup (19.6% and 29.9%, respectively), and > 5-year subgroup (41.7% and 51.6%, respectively). These results represent a reduction in risk of relapse by 33% for patients receiving PP1M versus OAP in the 0– 3-year subgroup (HR 0.67; 95% CI [0.44– 1.00], P = 0.050), 43% in the > 3– 5-year subgroup (HR 0.57; 95% CI [0.35– 0.93], P = 0.025), and 26% in the > 5-year subgroup (HR 0.74; 95% CI [0.55– 1.00], P = 0.049). Treatment-emergent adverse event rates were similar between treatment groups.
Conclusion: This analysis indicates that PP1M provides significant benefits in reducing relapse rates compared to OAPs, regardless of the duration of illness. These findings emphasize the importance of initiating PP1M treatment early in the course of schizophrenia to achieve better long-term outcomes.
Keywords: early intervention, critical period, long-acting injectable antipsychotics, PRIDE, PROSIPAL
Corrigendum for this paper has been published.
Introduction
Schizophrenia is a chronic mental illness that affects approximately 0.32% of people worldwide.1 Patients diagnosed with schizophrenia experience impacts to personal, social, educational, and occupational functioning.1 Patients also encounter an increased likelihood of comorbidities, a high risk of hospitalization, a 42% higher prevalence of substance use disorder, a 2 to 3 times higher mortality rate than the general population, a 10- to 20-year decrease in life expectancy, and increased likelihood of incarceration.2–7 If untreated or inadequately controlled, symptoms may persist or continue to worsen and can lead to disability.8 Over time, especially when symptoms are undertreated due to partial or nonadherence to antipsychotic medication, schizophrenia can result in detrimental outcomes.8 These negative outcomes include repeated relapses, hospitalization, incarceration, impact on social determinants of health, and incomplete recovery.5,8–11 Treatment response may also be reduced or delayed after repeated relapses with the same antipsychotic treatment.12
The duration of time after schizophrenia onset during which patients experience progressive disease development and are the most vulnerable to relapse has been referred to as the critical period.8 In this period, estimated as the first 3–5 years after diagnosis, a rapid decline in social, cognitive, and occupational functioning occurs before reaching a plateau.13 Therapeutic interventions earlier after diagnosis can help control repeated relapses, worsening symptoms, and increasing disability.8,13 In a previous post-hoc analysis, use of risperidone long-acting injection (RISPERDAL CONSTA®) in patients with recent onset of illness, defined as ≤3 years from diagnosis, showed significantly lower relapse rates and greater improvements in symptom scores versus patients >3 years from diagnosis. While early intervention is effective in symptom improvement and maintenance, treatment adherence remains a significant barrier to improving clinical outcomes in patients with schizophrenia.14 In a 3-year study to evaluate the consequences of antipsychotic treatment nonadherence, it was found that nonadherence was associated with a higher risk of relapse, hospitalization, and suicide attempts.15 In a real-world pharmacy-based study using pharmacy refill records (medication possession ratio < 80%), 76% of patients with schizophrenia were nonadherent to their oral medication over the 15-month study period.16 Additionally, in a retrospective Medicaid claims analysis, 67.7% of schizophrenia patients were nonadherent to their oral antipsychotic (OAP) and 39.4% discontinued their medication within 6 months of hospital discharge.17 Compared to OAPs, long-acting injectable antipsychotics (LAIs) have shown to improve adherence and reduce treatment discontinuations and (re)hospitalizations in addition to delaying time to relapse.17–20 A retrospective Medicaid claims analysis showed that patients on LAIs had a 65% lower risk of being nonadherent, a 55% lower risk of discontinuation, and a 27% lower risk of schizophrenia-related rehospitalization compared to OAPs.17 A recent meta-analysis of prospective and retrospective cohort studies found a 15.2% reduction in the hospitalization rates with LAIs compared to OAPs.18 LAIs have undergone evaluation for their impact on early treatment and have demonstrated effectiveness, offering physicians additional clinical guidance.21
Existing treatment guidelines support the use of LAIs earlier in the treatment course of adults with schizophrenia, although LAIs remain underused in many clinical settings and often are reserved for the most severely ill or poorly adherent individuals, who may already have experienced loss of functional status due to repeated relapses.22–25 Notably in the Guide to Long-acting Medications, the National Council for Mental Wellbeing recommends LAI discussions with the patient early after a diagnosis of schizophrenia in adults.22 The Florida Best Practice Psychotherapeutic Medication Guidelines also recommend LAIs as an initial treatment option for adult patients with schizophrenia.23 Despite the benefits and call to action for the use of LAIs, OAPs have been the standard for first line treatment.20
A previous integrated patient-level analysis of the PRIDE, PROSIPAL, and DREaM studies evaluated the efficacy of paliperidone palmitate (PP) compared to OAPs in adults diagnosed with schizophrenia overall and for varying durations of illness (0–3 years and >3 years).26 The analysis revealed that implementing PP earlier in the course of schizophrenia provides significant benefit compared to OAPs, as fewer relapses (17.7% versus 25.3% in the 0–3 year group; 32.3% versus 42.2% in the >3 year group) and a significantly longer time to relapse was observed with PP versus OAP. Given these results, a more granular analysis of patient-level outcomes with PP1M versus OAP within the first 5 years after diagnosis, focusing on the clinically relevant critical period, 3–5 years after diagnosis, is merited and would be generalizable to real-world populations with schizophrenia. This patient-level meta-analysis evaluated the risk of relapse in adult patients with schizophrenia overall and by varying durations of illness (0–3 years, >3–5 years, and >5 years) receiving PP1M or OAP treatment.
Material and Methods
Study Selection
The PROSIPAL (NCT01081769) and PRIDE (NCT01157351) studies were included in this patient-level meta-analysis because of their similar study designs and data collection methods, including the selection of the target patient population and the criteria for relapse.10,19 The PROSIPAL study was a randomized, controlled, open-label, rater-blinded study that examined the efficacy of PP1M versus OAP in recently diagnosed patients with schizophrenia (ie, up to 5 years after diagnosis). The PRIDE study was a randomized, prospective, open-label, event-monitoring board-blinded, parallel-group study that was designed to reflect real-world patients, treatment approaches, and clinically meaningful outcomes with PP1M and OAPs. The definition of relapse, and inclusion and exclusion criteria were similar between the two studies (Figure 1). Patient-level data from patients with schizophrenia were used in the analysis. Authors were able to access patient-level data (ie, raw data for each individual patient in the study) because both studies and the current analysis were sponsored by Janssen. This enabled the maintenance of patient clustering within studies for the post hoc analysis and the compilation of evidence for a specific clinical question, such as treatment effectiveness, from several related studies.
Outcomes
The analysis assessed outcome measures such as relapse evaluations and treatment-emergent adverse events (TEAEs). In both studies, treatment failure (TF) was identified by instances of relapse, including psychiatric hospitalizations, arrests or incarcerations, suicidal or homicidal ideation or behaviors, discontinuation due to inadequate efficacy, safety, or tolerability, treatment supplementation due to insufficient efficacy, but differed in measuring significant symptom worsening as measured by the Positive and Negative Syndrome Scale (PANSS) or the Clinical Global Impressions (CGI) Scale in the PROSIPAL study and an increase in psychiatric services in the PRIDE study.20,21
Statistical Analysis
With individual patient-level data available for both studies, it was possible to analyze duration of illness cutoffs of 0–3 years, >3–5 years, and >5 years. The Kaplan-Meier method was used to calculate the cumulative distribution functions of time to first treatment failure (TtFTF) or relapse. A log rank test was used to evaluate the significance of differences between groups. Hazard ratios (HRs) and 95% confidence intervals (CIs) for between-group differences in treatment failure risk were generated using a Cox proportional hazards model. Graphical diagnostics and statistical tests were conducted to verify the proportional hazards assumptions for each comparison. TEAEs were recorded and reported descriptively.
Results
Patient Characteristics
A sample of 1157 patients was included in the analysis set; most patients were male (68.7%), and the mean age was 34.7 years (Table 1). The mean (SD) age of first psychiatric diagnosis, mean (SD) age of first psychiatric treatment, and mean (SD) age of first psychiatric hospitalization were similar between the PP1M and OAP groups within each duration of illness subgroup. In comparing duration of illness subgroups, the mean (SD) age of first psychiatric diagnosis, treatment, and hospitalization in the total >5-year duration of illness subgroup were lower compared with the 0–3 years and >3–5 years subgroups. The mean (SD) number of total psychiatric hospitalizations was higher in the >5 years subgroup (PP1M: 8.1 [17.78]; OAP: 5.8 [5.54]) compared with the 0–3 years subgroup (PP1M: 2.6 [1.73]; OAP: 2.9 [2.15]) and the >3–5 years subgroup (PP1M: 3.9 [2.99]; OAP: 4.1 [3.43]). The number of patients who discontinued the study was similar between the PP1M and OAP cohorts within each duration-of-illness subgroup (Table 1).
 |
Table 1 Patient Baseline Characteristics and Discontinuation Rates by Duration of Illness Subgroup |
Efficacy
Fewer TFs were observed overall with PP1M versus OAP (25.2% and 32.9%, respectively), in the 0–3-year subgroup (15.8% and 21.7%, respectively), the >3–5-year subgroup (19.6% and 29.9%, respectively), and the >5-year subgroup (41.7% and 51.6%, respectively) (Figure 2). Overall, the risk of relapse was delayed by 31% for patients receiving PP1M versus OAP (HR 0.69; 95% CI [0.56–0.86], P < 0.001), independent of duration of illness category. Furthermore, risk of relapse was reduced by 33% for patients receiving PP1M versus OAP in the 0–3-year subgroup (HR 0.67; 95% CI [0.44–1.00], P = 0.050), by 43% in the >3–5-year subgroup (HR 0.57; 95% CI [0.35–0.93], P = 0.025) and by 26% in the >5-year subgroup (HR 0.74; 95% CI [0.55–1.00], P = 0.049) (Figure 3).
 |
Figure 3 Kaplan-Meier Plot of Time to First Treatment Failure for (a) Overall Study Population and (b) <3-Year, (c) >3–5-Year, and (d) >5-Year Duration of Illness Subgroups. |
Safety
A total of 875 patients (75.6%) experienced a TEAE (0–3-year: PP1M, n=253 [77.9%], OAP, n=263 [69.2%]; >3–5-year: PP1M, n=138 [71.7%], OAP, n=134 [69.4%]; >5-year: PP1M, n=187 [82.9%], OAP, n=182 [81.9%]. The most common TEAEs (occurring in ≥10% of patients) included injection site pain (in the PP1M group), nasopharyngitis, weight increase, akathisia, headache, anxiety, insomnia, and schizophrenia (Table 2). A similar proportion of patients treated with PP1M or OAP discontinued the study due to adverse events (3.3% and 2.6%, respectively).
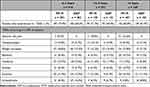 |
Table 2 Incidence of Treatment-Emergent Adverse Events |
Discussion
Schizophrenia is a chronic psychiatric disorder that can often lead to poor quality of life, extensive disability, and premature mortality.27 The need for care and treatment approaches that might change a negative trajectory of outcome, especially early in the course of illness, remains urgent. In this analysis using pooled data from studies that enrolled individuals generalizable to real-world populations with schizophrenia, risk of relapse was significantly delayed by 31% with PP1M versus OAPs regardless of duration of illness. Additionally, risk of relapse was delayed by 33% for the 0–3 years cohort, 43% for the >3–5-year cohort, and 26% for the >5-year cohort with PP1M compared to OAPs. TEAE rates were similar between PP1M and OAP treatment groups within each duration of illness category. These results reinforced the results of a previous post hoc analysis of the PRIDE, PROSIPAL, and DREaM studies on early intervention with PP1M compared to OAPs, confirming the overall effectiveness of PP1M early in the course of schizophrenia in adults.18
Both studies assessed in the current analysis, PROSIPAL and PRIDE, were designed to reflect real-world clinical practice. Although PROSIPAL was an open-label study, it was rater blinded and the choice of OAP was at the investigator’s discretion.28 PRIDE included flexible treatment interventions and patients who are typically excluded from clinical trials (ie, patients with comorbid substance abuse, history of incarceration, and unstable living conditions).16 Medication adherence was monitored but not required to complete either trial.
Prior studies have shown earlier treatment with LAIs has significant benefits compared to OAPs, including reduced risk of relapse, delayed time to relapse, and delayed time to first hospitalization.26,29 To address the need for early intervention, the National Institute of Mental Health sponsored the RAISE-ETP and NAVIGATE programs, which leveraged a comprehensive care plan that included early pharmacologic and psychosocial interventions. The investigators found that this plan improved clinical, functional, and quality of life outcomes for patients.30,31 A systematic literature review explored early intervention services (EIS) compared to usual care and found that EIS was associated with a reduced risk of hospitalization.32
Relapses experienced by patients with schizophrenia present profound humanitarian and economic burdens. A multinational survey of psychiatrists and their patients with schizophrenia found that compared to patients without relapses, patients who relapsed were significantly more likely to be homeless, unemployed, previously incarcerated, and have difficulties living independently.7 Moreover, those who experienced relapse had greater impairment in work status and worse quality of life versus those who did not. In the United States alone, it has been estimated that about $37.7 billion is spent annually in direct healthcare costs associated with patients with schizophrenia.33 Our findings suggest that LAIs, especially when used relatively early in the course of illness, have the potential to positively impact recovery trajectory and health outcomes.
Limitations of this post hoc analysis should be considered. Patients included in the analysis may not be fully representative of the real-world population with recent-onset schizophrenia. The PROSIPAL and PRIDE studies differed in design, including observation time and inclusion/exclusion criteria. A longer observation time may have identified larger differences between duration of illness groups. Individuals may have been excluded due to enrollment hesitancy. There are potential biases inherent in any study; however, the studies had oversight from a scientific and an independent data monitoring committee.
Conclusion
The current analysis shows that the risk of relapse was significantly reduced with PP1M compared to OAPs regardless of the duration of illness. The findings emphasize the importance of early intervention after schizophrenia diagnosis with PP1M. Additionally, PP1M was well tolerated, and no new safety concerns were observed. Further investigation is warranted to elucidate the broader impact of earlier treatment with LAIs.
Abbreviations
DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; LAI, long-acting injectable antipsychotic; OAP, oral antipsychotic; PP, paliperidone palmitate; PP1M, paliperidone palmitate once monthly; PRIDE, Paliperidone Palmitate Research in Demonstrating Effectiveness; PROSIPAL, Prevention of Relapse with Oral Antipsychotics versus Injectable Paliperidone Palmitate; TEAE, treatment-emergent adverse event; TF, treatment failure; TtFTF, time to first treatment failure.
Data Sharing Statement
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
Ethics Approval and Informed Consent
The study protocol was approved by an independent ethics committee or review board at each study center (for list of ethics committees, see Supplemental Table 1) and was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent.
Acknowledgments
The authors thank ApotheCom (Yardley, PA), for editorial assistance, which was funded by Janssen Scientific Affairs, LLC, a Johnson & Johnson company.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by Janssen Scientific Affairs, LLC, a Johnson & Johnson company, and the funder participated in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication.
Disclosure
MS has received research grants from Alkermes, Centers for Disease Control and Prevention, International Society for Bipolar Disorders, Intra-Cellular, Inc., Merck, National Institutes of Health, Neurelis, Otsuka, and Patient-Centered Outcomes Research Institute; has served as a consultant for Alkermes, Janssen, Lundbeck, Neurelis, Otsuka, and Teva; has received royalties from Johns Hopkins University Press, Oxford Press, Springer Press, and UpToDate; and has received compensation for preparation of/participating in continuing medical education activities for the American Academy of Child and Adolescent Psychiatry, American Epilepsy Society, American Physician’s Institute (CMEtoGo), Clinical Care Options, Neurocrine, and Psychopharmacology Institute. OL, KJ, MD, and CO are employees of Janssen Scientific Affairs, LLC, a Johnson & Johnson company. IT is an employee of Janssen Research & Development, LLC. OL, KJ, IT, MD, and CO hold stock in Johnson & Johnson, Inc. NJ reports no conflicts of interest in this work.
References
1. World Health Organization. Schizophrenia. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia.
2. Correll CU, Solmi M, Croatto G, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022;21(2):248–271. doi:10.1002/wps.20994
3. Chan JKN, Correll CU, Wong CSM, et al. Life expectancy and years of potential life lost in people with mental disorders: a systematic review and meta-analysis. EClinicalMedicine. 2023;65:102294. doi:10.1016/j.eclinm.2023.102294
4. Lafeuille MH, Gravel J, Lefebvre P, et al. Patterns of relapse and associated cost burden in schizophrenia patients receiving atypical antipsychotics. J Med Econ. 2013;16(11):1290–1299. doi:10.3111/13696998.2013.841705
5. Prins SJ. Prevalence of mental illnesses in US State prisons: a systematic review. Psychiatr Serv. 2014;65(7):862–872. doi:10.1176/appi.ps.201300166
6. Hunt GE, Large MM, Cleary M, Lai HMX, Saunders JB. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990-2017: systematic review and meta-analysis. Drug Alcohol Depend. 2018;191:234–258. doi:10.1016/j.drugalcdep.2018.07.011
7. Smith DJ, Langan J, McLean G, Guthrie B, Mercer SW. Schizophrenia is associated with excess multiple physical-health comorbidities but low levels of recorded cardiovascular disease in primary care: cross-sectional study. BMJ Open. 2013;3(4):e002808. doi:10.1136/bmjopen-2013-002808
8. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884–897. doi:10.1016/S0006-3223(01)01303-8
9. MacEwan JP, Forma FM, Shafrin J, Hatch A, Lakdawalla DN, Lindenmayer JP. Patterns of adherence to oral atypical antipsychotics among patients diagnosed with schizophrenia. J Manag Care Spec Pharm. 2016;22(11):1349–1361. doi:10.18553/jmcp.2016.22.11.1349
10. Pelayo-Terán JM, Gajardo Galán VG, de la Ortiz-García de la Foz V, et al. Rates and predictors of relapse in first-episode non-affective psychosis: a 3-year longitudinal study in a specialized intervention program (PAFIP). Eur Arch Psychiatry Clin Neurosci. 2017;267(4):315–323. doi:10.1007/s00406-016-0740-3
11. Ascher-Svanum H, Zhu B, Faries DE, Furiak NM, Montgomery W. Medication adherence levels and differential use of mental-health services in the treatment of schizophrenia. BMC Res Notes. 2009;2(1):6. doi:10.1186/1756-0500-2-6
12. Takeuchi H, Siu C, Remington G, et al. Does relapse contribute to treatment resistance? Antipsychotic response in first- vs. second-episode schizophrenia. Neuropsychopharmacology. 2019;44(6):1036–1042. doi:10.1038/s41386-018-0278-3
13. Birchwood M. Early intervention and sustaining the management of vulnerability. Aust N Z J Psychiatry. 2000;34(Suppl):S181–S184. doi:10.1177/000486740003401S27
14. World Health Organization. Adherence to long-term therapies: evidence for action.
15. Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2–3):109–113. doi:10.1016/j.psychres.2009.05.004
16. Alphs L, Benson C, Cheshire-Kinney K, et al. Real-world outcomes of paliperidone palmitate compared to daily oral antipsychotic therapy in schizophrenia: a randomized, open-label, review board-blinded 15-month study. J Clin Psychiatry. 2015;76(5):554–561. doi:10.4088/JCP.14m09584
17. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754–768. doi:10.18553/jmcp.2015.21.9.754
18. Kishimoto T, Hagi K, Nitta M, et al. Effectiveness of long-acting injectable vs oral antipsychotics in patients with schizophrenia: a meta-analysis of prospective and retrospective cohort studies. Schizophr Bull. 2018;44(3):603–619. doi:10.1093/schbul/sbx090
19. Brissos S, Veguilla MR, Taylor D, Balanzá-Martinez V. The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal. Ther Adv Psychopharmacol. 2014;4(5):198–219. doi:10.1177/2045125314540297
20. Lafeuille MH, Laliberté-Auger F, Lefebvre P, Frois C, Fastenau J, Duh MS. Impact of atypical long-acting injectable versus oral antipsychotics on rehospitalization rates and emergency room visits among relapsed schizophrenia patients: a retrospective database analysis. BMC Psychiatry. 2013;13(1):221. doi:10.1186/1471-244X-13-221
21. Stevens GL, Dawson G, Zummo J. Clinical benefits and impact of early use of long-acting injectable antipsychotics for schizophrenia. Early Interv Psychiatry. 2016;10(5):365–377. doi:10.1111/eip.12278
22. National Council for Behavioral Health. Guide to long-acting medications for providers and organizations. Nat Council Behav Health. Accessed https://www.thenationalcouncil.org/wp-content/uploads/2019/06/Guide-to-Long-acting-Medications.pdf?daf=375ateTbd56.
23. The University of South Florida, Florida Center for Behavioral Health Improvements and Solutions. 2023-2024 Florida best practice psychotherapeutic medication guidelines for adults.
24. American Psychiatric Association. The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. Updated 2020. Accessed June 14, 2024. https://www.psychiatry.org/psychiatrists/practice/clinical-practice-guidelines.
25. Mental Health Clinical Advisory Group. Mental health care guide for licensed practitioners and mental health professionals. Oregon Health Authority.
26. Lopena OJ, Alphs LD, Sajatovic M, et al. Earlier use of long-acting injectable paliperidone palmitate versus oral antipsychotics in patients with schizophrenia: an integrated patient-level post hoc analysis. J Clin Psychiatry. 2023;84(6):23m14788. doi:10.4088/JCP.23m14788
27. Rivelli A, Fitzpatrick V, Nelson M, Laubmeier K, Zeni C, Mylavarapu S. Real-world predictors of relapse in patients with schizophrenia and schizoaffective disorder in a large health system. Schizophrenia. 2024;10(1):28. doi:10.1038/s41537-024-00448-2
28. Schreiner A, Aadamsoo K, Altamura AC, et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr Res. 2015;169(1–3):393–399. doi:10.1016/j.schres.2015.08.015
29. Kane JM, Schooler NR, Marcy P, et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2020;77(12):1217–1224. doi:10.1001/jamapsychiatry.2020.2076
30. Kane JM, Schooler NR, Marcy P, et al. The RAISE early treatment program for first-episode psychosis: background, rationale, and study design. J Clin Psychiatry. 2015;76(3):240–246. doi:10.4088/JCP.14m09289
31. Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173(4):362–372. doi:10.1176/appi.ajp.2015.15050632
32. Correll CU, Galling B, Pawar A, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. 2018;75(6):555–565. doi:10.1001/jamapsychiatry.2018.0623
33. Cloutier M, Aigbogun MS, Guerin A, et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–771. doi:10.4088/JCP.15m10278
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



