Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
Effect of a Shared Decision-Making-Based Exercise Management Program on Blood Glucose Control in Patients with Gestational Diabetes Mellitus
Received 28 February 2025
Accepted for publication 22 May 2025
Published 9 June 2025 Volume 2025:18 Pages 3311—3320
DOI https://doi.org/10.2147/JMDH.S525616
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Bei Liu, Ge Jia, Fengcheng Cai
Childbirth Center, Hangzhou Women’s Hospital, Hangzhou, 310008, People’s Republic of China
Correspondence: Fengcheng Cai, Email [email protected]
Objective: To analyze the application of a shared decision-making (SDM)-based exercise management program in patients with gestational diabetes mellitus (GDM) and its impact on blood glucose control.
Methods: A retrospective analysis was conducted on the clinical data of 88 GDM patients who delivered at the Hangzhou Women’s Hospitalbetween December 2022 and April 2024. Patients were divided into the control group (n=44, receiving conventional exercise management program) and the observation group (n=44, receiving SDM-based exercise management program). Compliance with medical advice, quality of life (DSQL), self-management ability (SDSCA), blood glucose indicators (FBG, 2 h PG, and HbAlc), adverse self-management behaviors, and maternal and neonatal pregnancy outcomes were compared between the two groups.
Results: The observation group had higher rates of standardized medication use, scientific diet, regular blood glucose monitoring, adherence to exercise, and regular sleep patterns compared to the control group (P< 0.05). After intervention, the DSQL scores in both groups decreased, while the SDSCA scores increased, with the observation group showing a greater change (P< 0.05). The FBG, 2 h PG, and HbAlc levels were all lower after intervention in both groups, with the observation group showing a greater change (P< 0.05). The observation group had lower rates of poor blood glucose control, excessive weight gain during pregnancy, and unsatisfactory post-delivery oral glucose tolerance test (OGTT) compared to the control group (P< 0.05). The total incidence of adverse maternal pregnancy outcomes and neonatal adverse pregnancy outcomes was also lower in the observation group compared to the control group (P< 0.05).
Conclusion: Compared to conventional exercise management programs, the SDM-based individualized exercise management program can further improve GDM patients’ compliance with medical advice, enhance self-management abilities and quality of life, regulate blood glucose control, and improve maternal and neonatal pregnancy outcomes.
Keywords: shared decision-making, individualized exercise management plan, GDM, self-management ability, impact
Introduction
Gestational diabetes mellitus (GDM) is a state of glucose metabolism disorder that is induced or first diagnosed during pregnancy and is one of the common high-risk pregnancy complications.1 In recent years, with the increasing age of pregnant women and the influence of unhealthy lifestyles, the incidence of GDM has been rising annually.2 The occurrence of GDM not only significantly affects the health of the pregnant woman but also poses a serious threat to the short- and long-term health of the fetus and newborn. Pregnant women with GDM are prone to complications such as pregnancy-induced hypertension, polyhydramnios, preterm labor, and cesarean section, while the fetus may face risks such as macrosomia, respiratory distress syndrome, and hypoglycemia.3 Moreover, long-term follow-up studies4 have shown that GDM patients have a significantly increased risk of developing type 2 diabetes postpartum, and the incidence of obesity and metabolic syndrome in offspring is also significantly higher. Therefore, how to effectively manage and intervene in GDM to improve maternal-fetal pregnancy outcomes has become one of the key challenges in clinical research. Existing studies5 suggest that GDM management should focus on comprehensive intervention, including non-pharmacological measures such as dietary control, exercise therapy, and blood glucose monitoring. Among various intervention strategies, exercise therapy has become an essential component of GDM management due to its ability to effectively improve insulin sensitivity, reduce fasting blood glucose and postprandial blood glucose levels.6 Through scientifically designed exercise interventions, patients can achieve appropriate weight gain during pregnancy and reduce the risk of adverse maternal-fetal pregnancy outcomes.7 However, traditional exercise management plans often follow a fixed pattern, failing to fully consider individual differences, actual needs, and lifestyle habits of patients, which may result in suboptimal intervention effects for some patients.8 More importantly, the traditional physician-centered management model may put patients in a passive role, diminishing their initiative and involvement in the management process, which further impairs the enhancement of self-management ability.9 In recent years, the healthcare service model has gradually shifted from “disease-centered” to “patient-centered”, with management concepts such as shared decision-making (SDM) gaining increasing attention. SDM is a collaborative decision-making model that emphasizes mutual communication between healthcare providers and patients. It incorporates patients’ preferences and values into the formulation of individualized treatment strategies, guided by the best available clinical evidence.10 Recent studies have confirmed the effectiveness of SDM in improving clinical outcomes and patient satisfaction across various chronic disease management settings, including diabetes.11–13 Furthermore, evidence suggests that SDM may improve health literacy, treatment adherence, and empowerment in pregnant women with GDM by promoting active participation in care decisions.14,15 Therefore, incorporating the SDM concept into exercise management for GDM patients is a promising approach that may help stimulate patients’ initiative in health behavior change, improve adherence, and optimize maternal-fetal outcomes. Based on this background, this study constructs an individualized exercise management plan based on SDM and explores its application effect in GDM patients, aiming to provide scientific evidence for comprehensive management of GDM and investigate the feasibility and value of SDM in pregnancy-related disease management.
Materials and Methods
General Information
A retrospective analysis was conducted on the clinical data of 88 GDM patients admitted to our hospital from December 2022 to April 2024. The inclusion criteria were as follows: (1) Patients aged 20–35 years with a singleton pregnancy; (2) Clear diagnosis of GDM,16 confirmed in the early pregnancy period (24–28 weeks of gestation); (3) Patients voluntarily participated in the study, signed an informed consent form, and were willing to receive the relevant exercise intervention program and follow-up; (4) No severe complications during pregnancy (such as severe pregnancy-induced hypertension, preeclampsia, severe cardiovascular disease, severe liver or kidney dysfunction, etc)., and no medication that might affect physical activity; (5) The fetus was in normal gestational condition, with no severe structural abnormalities or significant fetal growth restriction, and the placenta function was normal; (6) Patients were able to complete the relevant examinations and assessments on time during the specified follow-up period and participate in the research activities. The exclusion criteria were as follows: (1) Known severe medical conditions (such as diabetic complications, heart disease, chronic kidney disease, etc). or musculoskeletal, joint, or neurological diseases that affect physical activity; (2) Severe complications during pregnancy, such as severe pregnancy-induced hypertension, preeclampsia, fetal distress, or placental abruption, requiring immediate medical intervention; (3) Long-term use of medications that affect physical activity or metabolic function (such as steroids, β-blockers, etc). or other drugs that may affect pregnancy and maternal-fetal health; (4) Severe psychological disorders (such as severe depression, anxiety, etc). that prevent cooperation with the exercise management plan, or patients who were unable to participate in related treatments due to unstable mental status; (5) Patients unable or unwilling to accept the exercise intervention plan, or who had aversion to it, leading to non-compliance with the individualized exercise management plan; (6) Other major pregnancy-related diseases or abnormalities (such as severe anemia, uncontrolled thyroid disease, etc). that affect maternal and fetal health; (7) Patients or their families refused to participate in the study or follow-up. Based on the exercise management plan, the patients were divided into the control group (n=47, who received the conventional exercise management plan intervention) and the observation group (n=47, who received the SDM-based individualized exercise management plan intervention). This study was approved by the Medical Ethics Committee of Hangzhou Women’s hospital childbirth center (Approval No.: [2023] Medical Review A (162) and was conducted in strict accordance with the ethical guidelines of the Declaration of Helsinki.
Methods
Control Group
The control group received the conventional exercise management plan intervention, which included the following details: (1) Health Education: Providing patients with basic knowledge about gestational diabetes, including the dangers of the disease, the importance of blood glucose control, and the role of exercise in blood glucose management; (2) Exercise Recommendations: Recommending low-intensity, primarily aerobic exercises such as walking, pregnancy yoga, swimming, etc., while avoiding high-intensity or strenuous exercises to reduce maternal and fetal safety risks; (3) Exercise Frequency and Duration: Recommending at least 150 minutes of moderate to low-intensity exercise per week, with each session lasting 20–30 minutes, arranged according to the patient’s daily routine; (4) Exercise Precautions: Emphasizing blood glucose monitoring before and after exercise, avoiding exercising in a fasted or hypoglycemic state, and being cautious of potential discomforts such as dizziness or fatigue during exercise; (5) Supervision and Feedback: Follow-up every two weeks to record the patient’s adherence to the exercise plan and provide targeted suggestions based on the patient’s feedback.
Observation Group
The observation group received an individualized exercise management plan based on (SDM, implemented through the following structured steps: (1) Individualized Assessment: ① Comprehensive Health Evaluation: Conducted by trained clinicians using standardized evaluation forms. Key indicators included: (i) Gestational age and blood glucose levels, extracted from electronic medical records. (ii) Physical activity readiness and tolerance, evaluated through the Physical Activity Readiness Questionnaire (PAR-Q) and the Modified Borg Rating of Perceived Exertion (RPE) Scale. (iii) Maternal-fetal risk factors, including hypertension, fetal development abnormalities, and comorbidities, screened using obstetric clinical guidelines. ② Lifestyle and Psychological Assessment: (i) Daily behavior, dietary intake, and sleep patterns were assessed via structured lifestyle questionnaires. (ii) Psychological status was evaluated using the Generalized Anxiety Disorder-7 (GAD-7) scale and a Likert-type questionnaire assessing exercise confidence and perceived barriers. (2) Functional Evaluation and Goal Setting (SDM): After the assessments, a structured face-to-face SDM session was held. Clinicians and patients jointly reviewed physical and psychological status to determine functional capacity. Goals were tailored to each patient’s needs, such as: Short-term: eg, “completing four 30-minute walking sessions per week”; Long-term: eg, “reducing HbA1c by 0.5%”, “controlling gestational weight gain to <500g/week.” (3) Personalized Exercise Plan Design: ① Exercise Type: Based on interests, safety, and physical ability, low-impact options were selected, such as walking, prenatal yoga, low-resistance training, and dynamic stretching. ② Intensity and Frequency: Determined using PAR-Q and Borg scores. Patients were assigned low to moderate intensity exercises (Borg 9–11 for low, 12–14 for moderate). ③ Adjustment Protocols: Plans were adjusted every two weeks based on: Subjective symptoms (eg, fatigue, dizziness), Wearable device activity tracking, Capillary blood glucose monitoring. Adjustments included modifying exercise duration, rest intervals, or switching exercise types. (4) Health Education and Exercise Skills Training: Provided through weekly group classes and video tutorials, covering: Exercise mechanisms and safety in gestational diabetes, Instruction in correct postures, breathing, and pacing, Emergency protocols (eg, managing hypoglycemia, when to stop exercise). (5) Patient Engagement and Real-Time Monitoring: Participants recorded daily logs of activity type, duration, intensity, and blood glucose levels. A WeChat group was maintained for real-time communication with the medical team, facilitating feedback, troubleshooting, and motivational reinforcement. (6) Follow-up and Evaluation: Every two weeks, comprehensive follow-up visits were conducted to review compliance, glycemic control, and patient satisfaction. For patients with low adherence, motivational interviewing and individualized psychological support were provided to promote long-term engagement.
The intervention lasted until delivery, with outcome assessment at the 8th week.
Observation Indicators
Compliance with Medical Advice
This includes standardized medication use, scientific diet, regular blood glucose monitoring, adherence to exercise, and regular sleep patterns. Compliance with these aspects was uniformly recorded by the relevant medical staff at our hospital.
Quality of Life
The Diabetes-Specific Quality of Life Scale (DSQL, Cronbach’s α coefficient = 0.833, validity = 0.802)17 was used to assess patients’ quality of life before and after the intervention (at 8 weeks of intervention). The score range for this scale is 27–135, with lower scores indicating worse quality of life.
Self-Management Ability
The Diabetes Self-Management Behavior Scale (SDSCA, Cronbach’s α coefficient = 0.847, validity = 0.811)18 was used to assess patients’ self-management ability before and after the intervention (at 8 weeks of intervention). The score range for this scale is 0–77, with higher scores indicating better self-management behavior.
Blood Glucose Indicators
Blood samples (5 mL of fasting venous blood) were collected from patients in the morning before and after the intervention, and were tested for fasting blood glucose (FBG), 2-hour postprandial blood glucose (2 h PG), and glycosylated hemoglobin (HbAlc) levels using an automated biochemical analyzer.
Adverse Self-Management Behavior in Pregnant Women
This includes poor blood glucose control leading to hospitalization, excessive weight gain during pregnancy, and unsatisfactory post-delivery oral glucose tolerance test (OGTT) results. These adverse situations were uniformly recorded by the relevant medical staff at our hospital.
Maternal and Neonatal Pregnancy Outcomes
This includes both maternal and neonatal outcomes. Adverse maternal pregnancy outcomes include gestational hypertension, abnormal amniotic fluid, postpartum hemorrhage, and premature rupture of membranes. Adverse neonatal pregnancy outcomes include premature birth, macrosomia, fetal distress, neonatal hypoglycemia, and neonatal asphyxia. These adverse pregnancy outcomes were uniformly recorded by the relevant medical staff at our hospital.
Statistical Analysis
GraphPad Prism 8 was used for drawing; statistical analysis was performed using SPSS22.0 software. Categorical data were expressed as percentages (%) and analyzed using the χ²-test. Continuous data were expressed as ( ), and comparisons between groups were made using independent sample t-tests, while paired t-tests were used for intra-group comparisons. A P-value of <0.05 was considered statistically significant.
), and comparisons between groups were made using independent sample t-tests, while paired t-tests were used for intra-group comparisons. A P-value of <0.05 was considered statistically significant.
Results
Comparison of Basic Information
The comparison of basic information such as age, gestational age, pre-pregnancy BMI, number of pregnancies, history of primiparity, family history of diabetes, history of GDM, and educational level between the two groups showed no significant differences (P > 0.05), indicating comparability. See Table 1.
 |
Comparison of Compliance with Medical Advice
The compliance rates for standardized medication, scientific diet, regular blood sugar monitoring, adherence to exercise, and regular sleep were higher in the observation group compared to the control group (P < 0.05), as shown in Table 2.
 |
Table 2 Comparison of Compliance with Medical Advice [n(%)] |
Comparison of Quality of Life and Self-Management Ability
After the intervention, the DSQL scores in both groups decreased, while the SDSCA scores increased, with the observation group showing a greater change (P<0.05), as shown in Figure 1.
 |
Figure 1 Comparison of Quality of Life and Self-Management Ability ( Note: Compared with pre-intervention, *P < 0.05; Between groups comparison, #P < 0.05. |
Comparison of Blood Sugar Indicators
After intervention, FBG, 2 h PG, and HbA1c levels decreased in both groups, with the observation group showing a larger improvement (P < 0.05), as shown in Figure 2.
 |
Figure 2 Comparison of Blood Sugar Indicators ( Note: Compared with pre-intervention, *P < 0.05; Between groups comparison, #P < 0.05. |
Comparison of Poor Self-Management Behaviors
The rates of poor blood sugar control, excessive weight gain during pregnancy, and failure to meet OGTT standards post-delivery were lower in the observation group than in the control group (P < 0.05), as shown in Table 3.
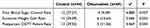 |
Table 3 Comparison of Poor Self-Management Behaviors [n(%)] |
Comparison of Maternal and Neonatal Pregnancy Outcomes
The total incidence of poor maternal and neonatal pregnancy outcomes was lower in the observation group compared to the control group (P < 0.05), as shown in Table 4.
 |
Table 4 Comparison of Maternal and Neonatal Pregnancy Outcomes [n(%)] |
Discussion
This study constructs an individualized exercise management plan based on Shared Decision-Making (SDM) and explores its application in patients with Gestational Diabetes Mellitus (GDM). The results show that compared to conventional exercise management plans, the SDM-based individualized exercise management plan significantly improved patient adherence, self-management ability, and demonstrated advantages in improving blood glucose control and pregnancy outcomes. These results fully demonstrate the importance and feasibility of patient-centered individualized exercise management plans in GDM management.
Intervention Model Based on SDM Improves Patient Compliance
Compliance with medical advice is a key determinant of the effectiveness of disease management. In this study, the observation group showed significantly higher rates of standardized medication use, scientific diet, regular blood glucose monitoring, adherence to exercise, and regular sleep patterns compared to the control group (P<0.05). This result suggests that, through SDM, both the medical staff and patients can reach a consensus on the exercise management goals, content, and execution strategies, enhancing patients’ sense of involvement and initiative, thereby improving their compliance. This result is consistent with findings from previous related studies,19,20 and it is hypothesized that the core of SDM lies in respecting patients’ individual needs and values, transforming them from “passive recipients” to “active participants”,21,22 which significantly improves patient behavioral compliance and promotes the sustainability of healthy behaviors.
Improving Patient Quality of Life and Self-Management Ability is a Key Aspect of SDM Intervention
Self-management ability is a core capability for GDM patients to control their condition, encompassing self-protection, fetal monitoring, adherence to medical advice, and daily life management, all of which significantly impact quality of life. This study found that SDM-based interventions significantly improved patients’ self-management ability and quality of life after the intervention (P<0.05), with the observation group showing a significantly higher increase than the control group. This may be attributed to SDM’s focus on personalized patient education during the intervention, offering targeted guidance and support that helps patients better understand the disease mechanism and management key points, thereby enhancing their confidence and ability in self-management. Additionally, the individualized approach better meets patients’ actual needs, encouraging them to implement the intervention measures more efficiently.23 For instance, in exercise interventions, personalized exercise plans tailored to the patient’s physical condition and lifestyle habits help improve adherence and satisfaction.
Improvement in Blood Glucose Control Effectiveness Verifies the Advantages of SDM Intervention
The core management goal of GDM is to control blood glucose levels in order to reduce the incidence of adverse maternal and neonatal pregnancy outcomes.24,25 In this study, the observation group had significantly lower levels of FBG, 2 h PG, and HbA1c after the intervention compared to the control group (P<0.05), indicating that the SDM-based individualized exercise management program had a significant effect on blood glucose control. This result may be related to the two-way communication and goal-setting emphasized in SDM. By jointly setting goals and monitoring plans with patients, healthcare providers can promptly identify problems in blood glucose control and provide targeted guidance, ensuring the maximization of intervention effectiveness.26,27 Additionally, personalized exercise management improves patients’ tolerance and adherence to exercise interventions, which in turn more effectively regulates glucose metabolism.28
Reducing Adverse Maternal and Neonatal Pregnancy Outcomes is a Direct Reflection of SDM Intervention
Maternal and neonatal pregnancy outcomes are key indicators for evaluating the effectiveness of GDM management. The results of this study showed that the observation group had significantly lower rates of poor blood glucose control leading to hospitalization, excessive weight gain during pregnancy, unsatisfactory post-delivery OGTT, and adverse maternal and neonatal pregnancy outcomes compared to the control group (P<0.05). This suggests that the SDM-based individualized exercise management program effectively reduces the risk of adverse maternal and neonatal pregnancy outcomes. The possible mechanism is that SDM intervention improves patients’ health behaviors (such as exercise, diet, and blood glucose monitoring), effectively reducing blood glucose fluctuations and insulin resistance.29,30 Furthermore, the management strategy under the doctor-patient collaborative model better identifies high-risk factors and intervenes early,31 thus optimizing pregnancy outcomes.
Innovation and Clinical Significance of This Study
Unlike conventional one-way guidance models, SDM facilitates communication between doctors and patients to build a consensus, enabling more precise and personalized interventions. The application of this model in GDM management not only embodies the modern patient-centered healthcare concept but also provides new insights for chronic disease management. Particularly for diseases like GDM that require long-term management, SDM helps enhance patients’ disease coping abilities and reduce the risk of long-term complications.
Limitations and Prospects
Although this study confirms the advantages of SDM in GDM management, it still has some limitations. For example, this study is a single-center retrospective study with a small sample size, which may limit the generalizability of the results. Additionally, the study only focused on short-term effects after the intervention, lacking follow-up data on long-term outcomes. Future research should expand the sample size and conduct multi-center, randomized controlled trials to verify the reliability and applicability of the conclusions. At the same time, information technology tools (such as health management apps) can be integrated to further optimize the implementation path of SDM, thereby improving intervention effectiveness.
Conclusion
The individualized exercise management plan based on SDM significantly enhanced medical adherence, self-management behaviors, and blood glucose regulation in patients with GDM. Specifically, patients in the SDM group demonstrated better control of fasting blood glucose, 2-hour postprandial glucose, and HbA1c, along with higher rates of standardized exercise, diet, and glucose monitoring. Furthermore, this approach was associated with a reduced incidence of excessive gestational weight gain, poor postpartum OGTT results, and adverse maternal-neonatal outcomes. These findings highlight the practical value of integrating SDM into GDM care pathways and suggest potential applicability in managing other chronic metabolic disorders requiring lifestyle intervention.
Funding
Zhejiang Provincial Health Science and Technology Project (2024KY226).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li GJ, Chen XF, Wang H, et al. [The association between visceral adipose thickness and gestational diabetes mellitus in the first trimester]. Zhonghua Yu Fang Yi Xue Za Zhi. 2024;58(7):1004–1010. Wolof
2. Fu JH, Huo J, Han YM, et al. [Predictive value of serum Gal-13, GLP-1 and VEGF levels in adverse pregnancy outcomes of gestational diabetes mellitus]. Zhonghua Yu Fang Yi Xue Za Zhi. 2023;57(12):2140–2146. Wolof. doi:10.3760/cma.j.cn112150-20230926-00226
3. Jiao XC, Xiao M, Gao ZX, et al. [Effects of comorbid gestational diabetes mellitus and depression on glucose metabolism during pregnancy and neonatal morphological outcome]. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(9):968–973. Wolof. doi:10.3760/cma.j.cn112150-20200307-00276
4. Su SF, Gao S, Zhang EJ, et al. [Analysis of incidence and associated factors of preterm birth based on pre-pregnancy body mass index stratification]. Zhonghua Yu Fang Yi Xue Za Zhi. 2023;57(6):899–904. Wolof
5. Huang FL, Hu H-Y, Zhang S-H, et al. [Effect of mobile health for standardized management on women with gestational diabetes mellitus]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2021;43(4):551–557. Danish. doi:10.3881/j.issn.1000-503X.13044
6. Wang LS, Tang YB, Liang ZX. [Research progress on the preventive and therapeutic effects of exercise on gestational diabetes mellitus]. Zhonghua Yu Fang Yi Xue Za Zhi. 2023;57(11):1808–1812. Wolof. doi:10.3760/cma.j.cn112150-20230119-00047
7. Stith BJ, Buls SM, Keim SA, et al. Moms in motion: weight loss intervention for postpartum mothers after gestational diabetes: a randomized controlled trial. BMC Pregnancy Childbirth. 2021;21(1):461. doi:10.1186/s12884-021-03886-3
8. Woodside A, Bradford H. Exercise and the prevention of gestational diabetes mellitus. Nurs Womens Health. 2021;25(4):304–311. doi:10.1016/j.nwh.2021.05.009
9. Tan Y, Huang F, Wang Y, et al. Effects of exercise intervention based on self-efficacy theory on pregnant women with gestational diabetes mellitus. Z Geburtshilfe Neonatol. 2023;227(3):186–196. doi:10.1055/a-2004-0740
10. Yan HB, Han YL. [Interventional strategy for left main artery disease: comprehensive evaluation, shared decision-making, and procedural considerations]. Zhonghua Xin Xue Guan Bing Za Zhi. 2023;51(2):103–105. Polish. doi:10.3760/cma.j.cn112148-20221230-01023
11. Wu AW. [Necessity of studies on intentional watch and wait strategy in rectal cancer from the perspective of history of surgical oncology]. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23(3):225–229. Hawaiian. doi:10.3760/cma.j.cn.441530-20200224-00076
12. Huang RC, Ding HY, Guo HZ. [Implement and improvement of patient-physician shared decision making in clinical practice in China]. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(10):890–894. Polish. doi:10.3760/cma.j.cn112148-20200519-00409
13. Gärtner FR, et al. Shared decision-making in the context of pregnancy and childbirth: a scoping review. BMC Pregnancy Childbirth. 2020;20:145. doi:10.1186/s12884-020-2837-x
14. Tran VT. Development and preliminary validation of a patient-reported experience measure of shared decision-making in pregnancy. BMC Pregnancy Childbirth. 2019;19:146. doi:10.1186/s12884-019-2307-2
15. McLaughlin K, Jensen, M, Foureur M, et al. Are pregnant women with asthma receiving guideline-recommended antenatal asthma management? A survey of pregnant women receiving usual care in Australia. Women Birth. 2023;36(1):108–116. doi:10.1016/j.wombi.2022.03.008
16. Wu HH. [Focus on the importance of classification of hyperglycemia in pregnancy and diagnostic criteria for gestational diabetes mellitus]. Zhonghua Yi Xue Za Zhi. 2022;102(6):389–392. Danish. doi:10.3760/cma.j.cn112137-20210730-01694
17. Lin L, Chen Y, Li Y, et al. 10.6-μm infrared laser as adjuvant therapy for diabetic peripheral neuropathy: study protocol for a double-blind, randomized controlled trial. Trials. 2022;23(1):53. doi:10.1186/s13063-021-05901-6
18. Oakley LL, Namara A, Sahu B, et al. Educational films for improving screening and self-management of gestational diabetes in India and Uganda (GUIDES): study protocol for a cluster-randomised controlled trial. Trials. 2021;22(1):501.
19. Chen W, Zhang M, Shen C. [Application of patient-reported outcomes and shared decision-making in thoracic surgery]. Zhongguo Fei Ai Za Zhi. 2024;27(10):792–798. Danish. doi:10.3779/j.issn.1009-3419.2024.106.26
20. Birkner B, Rech J, Edelmann E, et al. Treatment patterns of individualized real-life tapering approaches based on shared decision-making in rheumatoid arthritis. Z Rheumatol. 2024;83(2):142–150.
21. van der Weijden T, van der Kraan J, Brand PL, et al. Shared decision-making in the Netherlands: progress is made, but not for all. Time to become inclusive to patients. Z Evid Fortbild Qual Gesundhwes. 2022;171:98–104.
22. Hedberg B, Wijk H, Andersson Gäre B, et al. Shared decision-making and person-centred care in Sweden: exploring coproduction of health and social care services. Z Evid Fortbild Qual Gesundhwes. 2022;171:129–134. doi:10.1016/j.zefq.2022.04.016
23. Ji LL, Yang QB, Zhang XY, et al. [The effect of strengthening nutrition education in the second trimester on the basis of the first trimester on blood glucose]. Zhonghua Yi Xue Za Zhi. 2023;103(33):2614–2618. Danish. doi:10.3760/cma.j.cn112137-20230410-00576
24. Wang SS, Yue ZH, Han N, et al. [Association of maternal pre-pregnancy BMI, gestational weight gain, and gestational diabetes mellitus with BMI trajectory in early childhood: a prospective cohort study]. Zhonghua Liu Xing Bing Xue Za Zhi. 2024;45(10):1348–1355. Danish. doi:10.3760/cma.j.cn112338-20240513-00270
25. Zhang A, Su MY, Zheng LJ, et al. [Association between abnormal oral glucose tolerance test patterns in the second trimester and large for gestational age newborns]. Zhonghua Fu Chan Ke Za Zhi. 2024;59(3):184–191. Tonga. doi:10.3760/cma.j.cn112141-20231107-00178
26. de Abreu MM, Maia MN, Telles AO, et al. Advances in shared decision making in Brazil: the role of patient autonomy in curriculum reform, health system and clinical care. Z Evid Fortbild Qual Gesundhwes. 2024.
27. Bravo P, Dois A, Martínez A, et al. Advancing towards the implementation of patient-centred care in Chile: an opportunity to effectively practice shared decision-making. Z Evid Fortbild Qual Gesundhwes. 2022;171:30–35.
28. Anzoategui S, Gibbone E, Wright A, et al. Midgestation cardiovascular phenotype in women who develop gestational diabetes and hypertensive disorders of pregnancy: comparative study. Ultrasound Obstet Gynecol. 2022;60(2):207–214.
29. Fan SQ, Yan SQ, Zhu XZ, et al. [Independent and combined effects of pre-pregnancy BMI and gestational diabetes on early adiposity rebound timing in children]. Zhonghua Liu Xing Bing Xue Za Zhi. 2022;43(10):1626–1631. Danish
30. Feng YH, Zhan YL, Lyu Y, et al. [Associations between physical activities and gestational diabetes mellitus in the first trimester of pregnancy]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(6):829–833. Danish. doi:10.3760/cma.j.cn112338-20190914-00671
31. Perestelo-Perez L, Rivero-Santana A, Alvarez-Perez Y, et al. Shared decision-making in Spain in 2022: an updated revision of the current situation. Z Evid Fortbild Qual Gesundhwes. 2022;171:122–128.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




