Back to Journals » Journal of Pain Research » Volume 18
Effect of Pericapsular Nerve Group Block with Wound Infiltration vs Modified Supra-Inguinal Fascia Iliaca Block on Postoperative Analgesia in Adult Patients Undergoing Total Hip Arthroplasty – A Randomized Clinical Trial
Authors Huang Y, Peng S, Wang J, Liu L, Dong CS
Received 15 January 2025
Accepted for publication 8 May 2025
Published 24 May 2025 Volume 2025:18 Pages 2679—2688
DOI https://doi.org/10.2147/JPR.S517578
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jinlei Li
Ying Huang,1 Sheng Peng,1 Jun Wang,2 Lang Liu,2 Chun-Shan Dong2
1 Department of Anesthesiology, Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 2 Department of Anesthesiology, Anhui Medical University Third Affiliated Hospital (Hefei First People’s Hospital), Hefei, Anhui, People’s Republic of China
Correspondence: Chun-Shan Dong, Department of Anesthesiology, Anhui Medical University Third Affiliated Hospital (Hefei First People’s Hospital), Hefei Huaihe Road No. 390, 230061, People’s Republic of China, Tel +86-13023030292, Email [email protected]
Purpose: Pericapsular nerve group (PENG) block and supra-inguinal fascia iliaca block (S-FICB) provides incomplete analgesia for total hip arthroplasty (THA) due to anatomical limitations. This study compares two modified approaches—PENG block with wound infiltration (WI) and a modified S-FICB—to identify the optimal analgesic technique for THA.
Patients and Methods: Eighty-six subjects were randomly allocated to either the PENG block + WI group or the modified S-FICB group. The primary outcome was the postoperative numeric rating scale (NRS) pain scores (rest/hip adduction) at 6 hours. The secondary outcomes were pain scores at 12, 24, 48 hours postoperatively and postoperative day 5, the incidence of postoperative quadriceps motor block at 6, 12, 24, 48 hours and postoperative day 5, the mean blood pressure (MAP) at five time points, patient-controlled intravenous analgesia (PCIA) usage and adverse effects such as the incidence of rescue analgesia, local anesthetic systemic toxicity (LAST), postoperative hip infection, the incidence of postoperative nausea and vomiting (PONV) within 5 days after surgery.
Results: PENG + WI group had lower NRS at rest (6h) (95% CI 0.51– 1.64, p< 0.001). Compared with the PENG block + WI, the modified S-FICB resulted in a higher incidence of quadriceps motor block at 6 hours (82.1% vs 25.6%; OR=13.257, 95% CI 4.46– 39.38; p< 0.001) and 12 hours (71.8% vs 41%; OR=3.659, 95% CI 1.42– 9.42; p=0.001).
Conclusion: PENG block + WI provides sufficient postoperative analgesia with no quadriceps motor block compared to modified S-FICB, supporting early ambulation and in line with the enhanced recovery after surgery (ERAS) protocols.
Keywords: total hip arthroplasty, nerve block, analgesia and anesthesia, enhanced recovery after surgery
Introduction
Total hip arthroplasty (THA) is a common surgical treatment for treating hip fractures and femoral head necrosis, which is often accompanied by severe pain.1 Nociceptive nerves that cause hip pain are mainly innervated in the anterior capsule of the joint, which controlled by the joint branches of the femoral nerve (FN), obturator nerve (ON), and accessory obturator nerve (AON).2 Additionally, surgical incision-related pain cannot be ignored and is mainly controlled by the lateral femoral cutaneous nerve (LFCN).3 Peripheral nerve blocks have been used as part of a multimodal analgesic strategy.4,5
The supra-inguinal fascia iliaca block (S-FICB) has been widely used6,7 and involves the FN, LFCN and ON, but its blocking effect of the ON is not clear.8 Zheng et al and Huang et al9,10 proposed a modified ultrasound-guided supra-inguinal fascia iliaca compartment block (modified S-FICB). Guided by the deep iliac circumflex artery, the needle was pushed from cephalad to caudad using an in-plane technique to puncture the iliac fascia, which improved satisfactory ON blockade. The pericapsular nerve group block (PENG block), a new regional block introduced by Girón--Arango et al,11 blocks the joint branches of the FN, ON, and AON, providing satisfactory analgesia at the hip but not the surgical wound. This necessitates adjunctive wound infiltration (WI), where local anesthetics are administered directly into the surgical site post-procedure—a safe, motor-sparing method for postoperative pain relief.12,13 While prior studies14,15 reported comparable pain scores between S-FICB and PENG block, no blinded randomized trials have yet compared the modified S-FICB with PENG block with WI (PENG block + WI), both representing advancements in nerve block techniques.
Our primary objective was to assess the efficacy of PENG block + WI in postoperative analgesia and motor recovery and to compare its effectiveness with modified S-FICB. Our hypothesis was that PENG block + WI would have lower pain scores.
Material and Methods
The prospective trial was approved by the ethics committee of Hefei First People’s Hospital (ID: 2022 [71]) on October 31, 2022, and registered in the Chinese Clinical Trial Registry (https://www.chictr.org.cn; Study ID: ChiCTR2200065321) on November 2, 2022, prior to patient recruitment. The study was conducted between November 5, 2022, and May 5, 2023, in accordance with the Declaration of Helsinki.
After obtaining written informed consent, we enrolled 86 patients scheduled to undergo THA. The inclusion criteria were as follows: scheduled for THA with lateral approach under general anesthesia, ASA I–III, aged ≥18 years, and no contraindication to regional anesthesia. The exclusion criteria were as follows: declined participation, coagulation disorders, septicemia or liver or renal failure, local anesthesia (LA) allergy, pregnancy and chronic preoperative opioid use.
Intervention, Randomization and Blinding
Patients were randomized 1:1 to either the PENG block + WI group or modified S-FICB group using a computer-generated sequence. Allocation was concealed in sealed envelopes managed by an independent research assistant. On the day of surgery, an unblinded investigator assigned patients to the PENG block + WI group: PENG block (10 mL 0.5% ropivacaine) + wound infiltration (20 mL 0.25% ropivacaine) or the modified S-FICB group: Modified S-FICB (40 mL 0.25% ropivacaine). The operating room nurse prepared solutions based on group assignment. Surgeons, postoperative assessors, and patients remained blinded to group allocation.
Anesthesia Management
All patients fasted from heavy meals for 8 hours, light meals for 6 hours and from clear liquids for 4 hours before surgery. Upon arrival in the monitoring and treatment room, venous access was established, and blood pressure, heart rate, and oxygen saturation were monitored. Both groups received mild sedation with intravenous dexmedetomidine (0.6 µg/kg) over 20 minutes. A radial artery puncture was performed for patients with an ASA III and hemodynamic instability. Under routine monitoring, nerve blocks were conducted using ultrasound (Navi s, Wisonic, Shenzhen, China) by a senior anesthesiologist, followed by anesthesia induction. General anesthesia was induced with propofol (1.2–2 mg/kg), sufentanil (0.3–0.5 µg/kg), and rocuronium bromide (0.6 mg/kg), and maintained with propofol (2–5 mg/kg/h), remifentanil (0.1–0.5 µg/kg/min), and sevoflurane (1%), targeting a bispectral index (BIS) of 40–60.
In the PENG block + WI group, 20 mL of 0.25% ropivacaine was administered via surgical wound infiltration postoperatively, whereas the modified S-FICB group received 20 mL of 0.9% normal saline. Both groups received identical postoperative multimodal analgesia: flurbiprofen axetil (50 mg) and sufentanil (5 µg) 5 minutes preoperatively, followed by patient-controlled intravenous analgesia (PCIA). The PCIA regimen included sufentanil (100 µg), ondansetron (8 mg), and dexmedetomidine (2–3 µg/kg) in 100 mL normal saline, initiated preoperatively with a 5 mL bolus, 3 mL/h background infusion, 2 mL patient-controlled doses, and a 20-minute lockout interval. Postoperatively, parecoxib sodium (40 mg/24 h) was administered intravenously for 48 hours. Rescue analgesia (oral tramadol 50 mg) was provided if numeric rating scale (NRS) pain scores reached ≥5.
Performance of Nerve Blocks
All blocks were performed preinduction with patients supine. For the modified S-FICB, according to the technique described by Zheng et al and HUANG Yonghua,9,10 the anterior superior iliac spine was palpated, and the high-frequency linear ultrasound probe (5–10 MHz) (Navi, Wisonic, Shenzhen China) was placed at the patient’s navel to obtain an image of the anterior superior iliac spine and the iliac muscle was identified by sliding the probe inwards. Then, the probe was adjusted to identify the subcutaneous tissue, internal oblique muscle, sartorius muscle, fascia iliaca, and iliac muscle. The inner side of the probe was fixed, the outer side of the probe was rotated approximately 15° inwards, and color Doppler localized the deep iliac circumflex artery overlying the fascia iliaca. Guided by the deep iliac circumflex artery, the needle was pushed from cephalad to caudad using an in-plane technique to puncture the iliac fascia (Figure 1a). We administered 2–3 mL of physiological saline, observed the downwards movement of the iliac muscle, and then withdrew and injected 40 mL of 0.25% ropivacaine in batches (Figure 1a). Sensory loss on the lateral/anterior thigh (assessed via pinprick 15 min postinjection) defined successful blockade. Failed blocks were excluded. For the PENG block, according to the technique described by Giron-Arango,11 a curvilinear probe was used (5–10 MHz) for ultrasound (Navi, Wisonic, Shenzhen China). Puncture was performed in a lateromedial direction until the needle tip reached the plane between the iliopsoas tendon and periosteum and between the anterior inferior iliac spine and iliopubic eminence. After a negative aspiration test, 10 mL of 0.5% ropivacaine was injected in the plane beneath the iliopsoas muscle to obtain an image of the psoas tendon uplift (Figure 1b). Two blinded anesthesiologists (5+ years of regional anesthesia experience) performed all blocks.
Study Outcomes
Our primary outcome was the postoperative NRS pain scores (0 no pain, 10 worst imaginable pain) at rest and during adduction at 6 hours. The secondary outcomes were static (at rest) and dynamic (hip adduction) pain scores at 12, 24, 48 hours and day 5, the incidence of postoperative quadriceps motor block (paralysis or paresis) at 6, 12, 24 48 hours and day 5, the mean blood pressure (MAP) at five time points: T1: admission; T2: 3 minutes after induction; T3: positioning; T4: skin incision; T5: 5 minutes after extubation in the operation room, perioperative anesthetic and vasoactive drug use, the incidence of rescue analgesia, PCIA usage and adverse effects such as local anesthetic systemic toxicity (LAST), postoperative hip infection, the incidence of postoperative nausea and vomiting (PONV) within 5 days. All the study variables we collect are real-time.
Patients were positioned supine with hips and knees flexed at 45° and 90°, respectively, using the knee extension test. The patient was first asked to extend the knee against gravity and then against resistance. Knee extension was graded according to a 3-point scale: 0=normal strength (extension against gravity and against resistance); 1=paresis (extension against gravity but not against resistance); and 2=paralysis (no extension possible).16
Statistical Analysis
To calculate the sample size, we considered our primary hypothesis that the patients who underwent PENG block + WI would have lower pain scores than those who underwent the modified S-FICB. Previous publications9,10 showed that the pain scores of the patients who underwent the S-FICB was approximately 1.7 (SD 0.7) at rest at 6 hours postoperatively. In our preliminary experiment, we estimated the mean pain score and the SD of the patients who underwent the PENG block + WI would be 1 and 1, respectively. To obtain a study power of 80%, we selected an SD of 1 for both groups and a type 1 error of 5%. We calculated that at least 34 patients were needed per group. We decided to recruit 90 patients in total in case of any exclusions and patients lost to follow-up.
Parametricity of continuous variables was evaluated using the Shapiro‒Wilk normality test. Normally distributed continuous variables are expressed as the mean with SD, and non-parametric variables are expressed as the median (IQR [range]). For continuous parametric variables, Student’s t test was used, while the Wilcoxon-Mann‒Whitney U-test was used for non-parametric continuous variables. Generalized estimating equation approaches was applied to compare the NRS among groups. The results were expressed by P value and 95% confidence index (CI). For categorical data, the χ²-test was used. Fisher’s exact test was used when any cell for the aforementioned categorical data had an expected count of less than five, and univariate logistic regression was used to calculate the odds ratio and 95% CI for postoperative quadriceps motor block. Repeated measures analysis of variance and Student’s t test were used to compare MAP at five time points. P value < 0.05 was considered statistically significant.
Results
Of 90 screened patients, 4 patients refused to sign informed consent forms and thus were not included. Eighty-six patients were randomized equally into two groups (Figure 2). Four subjects in the modified S-FICB group (nerve block failure) and four in the PENG + WI group (3 early discharges, 1 non-compliance with strength testing) were excluded, leaving 39 subjects per group for analysis (Figure 2). Demographic characteristics were comparable between groups (Table 1).
 |
Table 1 Demographic Data and Patient Characteristics |
 |
Figure 2 Flow diagram of the patients’ recruitment. |
Compared with the modified S-FICB group, the PENG block + WI group demonstrated significantly lower NRS scores at rest at 6 hours postoperatively (95% CI 0.51–1.64, p<0.001 Table 2), with a median (IQR [range]) of 1 (0–2 [0–5]) vs 2 (2–3 [1–6]). Similarly, the PENG block + WI group exhibited reduced NRS scores during hip adduction at both 6 hours (95% CI 0.27–1.47, p=0.004) and 12 hours postoperatively (95% CI 0.04–1.29, p=0.037 Table 2). In addition, modified S-FICB group showed significantly lower mean arterial pressure (MAP) at T4 (P < 0.05, Figure 3), with no inter-group differences at other time points.
 |
Table 2 Postoperative Static and Dynamic Pain Scores |
Compared with the PENG block + WI, the modified S-FICB resulted in a higher incidence of quadriceps motor block at 6 hours (82.1% vs 25.6%; OR=13.257, 95% CI 4.46–39.38; p<0.001) and 12 hours (71.8% vs 41%; OR=3.659, 95% CI 1.42–9.42; p=0.001) (Table 3), with no inter-group differences at other time points.
 |
Table 3 Postoperative Motor Block Assessment |
No inter-group differences were found in terms of intraoperative opioids and vasoactive drug consumption or the incidence of rescue analgesia, PCIA usage, LAST, PONV or postoperative hip infection (Table 4).
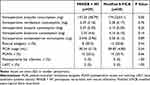 |
Table 4 Intraoperative Drugs Consumption and Other Postoperative Outcomes |
Discussion
Our randomized trial demonstrated that the addition of WI to PENG block provided sufficient postoperative analgesia with no motor block in patients undergoing THA with lateral approach.
Hip surgeries, particularly for fractures, are associated with moderate-to-severe perioperative pain.4 Adequate pain management can facilitate postoperative mobilization and promote functional recovery,17,18 which is an important component of the enhanced recovery after surgery (ERAS) protocols. While prior studies14,15 reported comparable analgesia between PENG block and supra-inguinal fascia iliaca compartment block (S-FICB), both techniques have limitations. For S-FICB, whether the ON is involved is rather controversial.19 And multiple studies have shown that the obturator nerve is not completely located within the iliac fascia compartment,20,21 which means that its analgesic effect can be limited by sparing of the anteromedial side of the hip joint. In addition, although PENG block is a nerve block technique for intracapsular analgesia of the hip joint,11 it spares the LFCN, failing to address incision-site pain. Some researchers have suggested combining PENG block with LFCN block to provide a better analgesic effect than PENG block alone.22 Modified S-FICB is guided by the deep iliac circumflex artery. The needle was pushed from cephalad to caudad using an in-plane technique to puncture the iliac fascia, providing satisfactory blockade FN, ON and sciatic nerves (SN), especially for ON.9,10 WI complements the PENG block by addressing its inability to anesthetize the surgical incision. Therefore, this study directly compared these optimized approaches to redefine postoperative analgesia strategies for THA.
Both groups achieved consistently low postoperative pain scores. S-FICB relies on volume-dependent diffusion, with previous studies14,23 supporting 40 mL of low-concentration ropivacaine. While PENG block targets a confined anatomical space, requiring smaller volumes. Previous studies24–26 have shown that 10 mL local anesthetic is sufficient to provide postoperative analgesia. To standardize total ropivacaine doses (100 mg), we administered: 40 mL 0.25% ropivacaine for S-FICB; 10 mL 0.5% ropivacaine for PENG block +20 mL 0.25% ropivacaine for WI. This approach aligned with evidence-based dosing while maintaining efficacy. Current guidelines27 emphasize multimodal analgesia combining regional blocks, non-opioids, and selective COX-2 inhibitors. By integrating optimized nerve blocks into this framework—targeting gaps in existing techniques (variable obturator coverage of S-FICB and lacking of incision analgesia for PENG block)—we validated a feasible, motor-sparing strategy for THA. However, it is crucial to consider whether the observed statistical differences in pain scores (NRS < 4) at 6 and 12 hours postoperatively carry substantial clinical significance. Three key arguments support the limited clinical relevance of these numerical differences. Firstly, comparable PCIA consumption and rescue analgesia incidence between groups indicate similar clinical needs. This phenomenon likely reflects achievement of the clinical target of “adequate analgesia” in both groups.28 Secondly, pain scales exhibit reduced discriminative validity at lower scores (NRS < 4). Studies29 have demonstrated reduced patient discrimination accuracy when NRS <4, suggesting these minor differences may not represent true clinical differentiation. Finally, from a clinical perspective, the primary objectives of pain management are to prevent moderate-to-severe pain (NRS ≥4) while minimizing analgesic-related adverse effects. When both groups achieved the predefined pain control target (NRS < 4) with comparable requirements for supplemental analgesia, the marginal numerical differences should not serve as primary determinants of therapeutic superiority.30 Pain management should prioritize functional outcomes and safety profiles over pursuit of statistically significant differences within clinically equivalent mild pain ranges.31
Our results revealed elevated blood pressure in the PENG + WI group following skin incision. Previous study32 suggested that pain activates the sympathetic nervous system, and hypertension may reflect inadequate intraoperative analgesia. While the modified S-FICB stabilized blood pressure post-blockade of the lateral femoral cutaneous nerve, the PENG + WI group’s hypertensive response suggests incomplete nociceptive inhibition during incision.
The PENG block + WI group exhibited superior postoperative quadriceps muscle strength compared to controls, consistent with prior studies.33,34 Notably, no patients in the PENG + WI group experienced complete motor block, contrasting with earlier studies. This may be explained as follows: First, administration of 10 mL 0.5% ropivacaine in our study (vs 20 mL in prior studies33,34), aligning with evidence that motor-sparing effects of PENG blocks depend critically on injectate volume.35,36 Second, postoperative pain at the surgical incision cannot be ignored. Pain is also an important factor affecting postoperative activity.17,18 Incisional infiltration in our study provided targeted analgesia at the surgical site without impairing quadriceps function.12,13 Preserved quadriceps strength mitigates patient-reported dissatisfaction (inability to lift legs, numbness). Therefore, early postoperative motor rehabilitation management is crucial. The PENG block offers distinct advantages, including a lower required dose of local anesthetic, rapid onset, and the absence of motor blockade.37,38 These benefits facilitate early postoperative ambulation, aligning with the principles of ERAS protocols.
However, this study has some limitations. First, the time between modified S-FICB and surgical initiation was not recorded, which may have influenced blood pressure fluctuations during patient positioning and skin incision. Second, since the outcome here is pain scores, the baseline pain scores were not recorded nor were the type of painkillers that were consumed during their stay in the ward, in addition, we did not record the use of rescue analgesics, only the incidence of rescue analgesia. All of these will affect our postoperative comparison of pain scores with the two groups. Third, factors such as frailty and days between fracture and surgery need to be very balanced between the study groups to avoid bias. Fourth, the time of first ambulation and discharge should be recorded in order to better elaborate the ERAS protocols.
Conclusion
In summary, PENG block + WI provides sufficient postoperative analgesia with no quadriceps motor block for THA compared to modified S-FICB, supporting early ambulation and in line with the enhanced recovery ERAS protocols.
Data Sharing Statement
Raw data (de-identified) used in this clinical trial are available from the corresponding author Chun-Shan Dong.
Ethics Statement
This is a randomized controlled clinical trial comparing the analgesic effect of pericapsular nerve group block of hip joint with different concentrations and volumes of ropivacaine in elderly patients undergoing hip replacement. This study conforms with Helsinki Declaration.
Acknowledgments
The authors would like to thank the reviewer, Wen-rui Zhang, for the effort and the time spent in the linguistic revision of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare no competing interests in this work.
References
1. Gerbershagen HJ, Aduckathil S, van Wijck AJ. et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934–944. doi:10.1097/ALN.0b013e31828866b3
2. Nagpal AS, Brennick C, Occhialini AP, et al. Innervation of the posterior Hip capsule: a cadaveric study. Pain Med. 2021;22(5):1072–1079. doi:10.1093/pm/pnab057
3. Thybo KH, Mathiesen O, Dahl JB, Schmidt H, Hagi-Pedersen D. Lateral femoral cutaneous nerve block after total Hip arthroplasty: a randomised trial. Acta Anaesthesiol Scand. 2016;60(9):1297–1305. doi:10.1111/aas.12764
4. Hojer Karlsen AP, Geisler A, Petersen PL, Mathiesen O, Dahl JB. Postoperative pain treatment after total Hip arthroplasty: a systematic review. Pain. 2015;156(1):8–30. doi:10.1016/j.pain.0000000000000003
5. Johnson RL, Kopp SL, Hebl JR, Erwin PJ, Mantilla CB. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth. 2013;110(4):518–528. doi:10.1093/bja/aet013
6. Desmet M, Vermeylen K, Van Herreweghe I, et al. A longitudinal supra--inguinal fascia iliaca compartment block reduces morphine consumption after total Hip arthroplasty. Reg Anesth Pain Med. 2017;42(3):327–333. doi:10.1097/AAP.0000000000000543
7. Vermeylen K, Desmet M, Leunen I, et al. Supra-inguinal injection for fascia iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: a volunteer study. Reg Anesth Pain Med. 2019;2018:100092.
8. Swenson JD, Davis JJ, Stream JO, et al. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: the pattern of distribution and effects on the obturator nerve. J Clin Anesth. 2015;27(8):652–657. doi:10.1016/j.jclinane.2015.07.001
9. Zheng T, Hu B, Zheng CY, et al. Improvement of analgesic efficacy for total Hip arthroplasty by a modified ultrasound-guided supra-inguinal fascia iliaca compartment block. BMC Anesthesiol. 2021;21(1):75. doi:10.1186/s12871-021-01296-8
10. Huang YH, Zhang RB, Liang GS. Application of Ultrasound-Guided Modified Suprainguinal Fascia Iliaca Compartment Block in the Operation of Intertrochanteric Fracture of Femur in the Elderly. Pract J Cardiac Cereb Pneumal Vasc Dis. 2020;28(S1):47–50.
11. Girón--Arango L, Peng PWH, Chin KJ, et al. Pericapsular nerve group (PENG) block for Hip fracture. Reg Anesth Pain Med. 2018;43:1–63. doi:10.1097/AAP.0000000000000847
12. Raines S, Hedlund C, Franzon M, et al. Ropivacaine for continuous wound infusion for postoperative pain management: a systematic review and meta--analysis of randomized controlled trials. Eur Surg Res. 2014;53(1–4):43–60. doi:10.1159/000363233
13. Ventham NT, Hughes M, O’Neill S, et al. Systematic review and meta-analysis of continuous local anaesthetic wound infiltration versus epidural analgesia for postoperative pain following abdominal surgery. Br J Surg. 2013;100(10):1280–1289. doi:10.1002/bjs.9204
14. Aliste J, Layera S, Bravo D, et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total Hip arthroplasty. Reg Anesth Pain Med. 2021;46(10):874–878. doi:10.1136/rapm-2021-102997
15. Choi YS, Park KK, Lee B, et al. Pericapsular nerve group (PENG) block versus supra-inguinal fascia iliaca compartment block for total Hip arthroplasty: a randomized clinical trial. J Pers Med. 2022;12(3):408. doi:10.3390/jpm12030408
16. Bravo D, Layera S, Aliste J, et al. Lumbar plexus block versus suprainguinal fascia iliaca block for total Hip arthroplasty: a single--blinded, randomized trial. J Clin Anesth. 2020;66:109907. doi:10.1016/j.jclinane.2020.109907
17. Karam JA, Schwenk ES, Parvizi J. An update on multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am. 2021;103(17):1652–1662. doi:10.2106/JBJS.19.01423
18. Tan M, Law LS, Gan TJ. Optimizing pain management to facilitate Enhanced Recovery After Surgery pathways. Can. J Anaesth. 2015;62(2):203–218.
19. Nielsen TD, Moriggl B, Søballe K, et al. A cadaveric study of ultrasound-guided subpectineal injectate spread around the obturator nerve and its Hip articular branches. Reg Anesth Pain Med. 2017;42(3):357–361. doi:10.1097/AAP.0000000000000587
20. Hebbard P, Ivanusic J, Sha S. Ultrasound--Guided supra--inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66(4):300–305. doi:10.1111/j.1365-2044.2011.06628.x
21. Bendtsen TF, Pedersen EM, Peng P. Course of the obturator nerve. Reg Anesth Pain Med. 2019;44(11):1039.2–40. doi:10.1136/rapm-2019-100655
22. Roy R, Agarwal G, Pradhan C, Kuanar D. Total postoperative analgesia for Hip surgeries, PENG block with LFCN block. Reg Anesth Pain Med. 2019;44(6):
23. Carella M, Beck F, Piette N, et al. Comparison between supra-inguinal fascia iliaca and pericapsular nerve group blocks on postoperative pain and functional recovery after total Hip arthroplasty: a noninferiority randomised clinical trial. Eur J Anaesthesiol. 2023;40(9):660–671.
24. Tran J, Agur A, Peng P. Is pericapsular nerve group (PENG) block a true pericapsular block? Reg Anesth Pain Med. 2019;2018:100278.
25. Wang DH, Chen LP, Xue JJ. Comparison of analgesic effect of pericapsular nerve group block of Hip joint with different concentrations and volumes of ropivacaine in elderly patients with hip fracture. J Clin Anesthesiol. 2022;38(05):497–502.
26. Huang Y, Lu Y, Wang J, et al. Effect of Pericapsular Nerve Group Block with Different Concentrations and Volumes of Ropivacaine on Functional Recovery in Total Hip Arthroplasty: a Randomized, Observer-Masked, Controlled Trial. J Pain Res. 2024;17:677–685. doi:10.2147/JPR.S445000
27. Anger M, Valovska T, Beloeil H, et al. Prospect guideline for total Hip arthroplasty: a systematic review and procedure-specific postoperative pain management recommendations[J]. Anaesthesia. 2021;76(8):1082–1097. doi:10.1111/anae.15498
28. George R, Huang T, Kandasamy R, et al. ‘Sufficient Pain relief ‘as a Practical Benchmark in Cancer Pain Management: a Prospective Study of Serial Pain Scores, Patient-rated Pain Relief and Perceived Sufficiency of Analgesics. Indian. J Palliat Care. 2022;28(2):160–166.
29. Krebs EE, Carey TS, Weinberger M. Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med. 2007;22(10):1453–1458. doi:10.1007/s11606-007-0321-2
30. Ruyssen-Witrand A, Tubach F, Ravaud P. Systematic review reveals heterogeneity in definition of a clinically relevant difference in pain. J Clin Epidemiol. 2011;64(5):463–470. doi:10.1016/j.jclinepi.2010.06.008
31. Olsen MF, Bjerre E, Hansen MD, et al. Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: systematic review of empirical studies. J Clin Epidemiol. 2018;101:87–106.e2. doi:10.1016/j.jclinepi.2018.05.007
32. Sch€uttler J, Albrecht S, Breivik H, et al. A comparison of remifentanil and alfentanil in patients undergoing major abdominal surgery. Anaesthesia. 1997;52(4):307–317. doi:10.1111/j.1365-2044.1997.24-az0051.x
33. Lin DY, Morrison C, Brown B, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in Hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med. 2021;46(5):398–403. doi:10.1136/rapm-2020-102315
34. Pascarella G, Costa F, Del Buono R, et al. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total Hip arthroplasty: a randomised, observer-masked, controlled trial. Anaesthesia. 2021;76(11):1492–1498. doi:10.1111/anae.15536
35. Ciftci B, Ahiskalioglu A, Altintas HM, et al. A possible mechanism of motor blockade of high volume pericapsular nerve group (PENG) block: a cadaveric study. J Clin Anesth. 2021;74:110407. doi:10.1016/j.jclinane.2021.110407
36. Kim JY, Kim J, Kim DH, et al. Anatomical and Radiological Assessments of Injectate Spread Stratified by the Volume of the Pericapsular Nerve Group Block. Anesth Analg. 2023;136(3):597–604. doi:10.1213/ANE.0000000000006364
37. Mysore K, Sancheti SA, Howells SR, et al. Postoperative analgesia with pericapsular nerve group (PENG) block for primary total Hip arthroplasty: a retrospective study. Can. J Anaesth. 2020;67(11):1673–1674.
38. Noaman SS, Abdallah ES, Elsawy SMA, et al. The Efficacy of Pericapsular Nerve Group Block Versus Facia Iliaca Block on Immediate Postoperative Pain and Opioid Consumption After Hip Arthroscopy Randomized Trial. Pain Physician. 2023;26(4):357–367. doi:10.36076/ppj.2023.26.357
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



