Back to Journals » Drug Design, Development and Therapy » Volume 19
Effect of Subanesthetic Dose of Esketamine on Liver Function Following Microvascular Reconstruction for Head and Neck Cancer: A Randomized Controlled Trial
Authors Lv XL, Liu Q, Yu JP, Cai XC , Wu L, Yang JJ , Dong YC
Received 6 November 2024
Accepted for publication 5 May 2025
Published 15 May 2025 Volume 2025:19 Pages 3971—3981
DOI https://doi.org/10.2147/DDDT.S505020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Qiongyu Guo
Xue-Li Lv,1,* Qing Liu,1,* Jin-Ping Yu,1 Xue-Chun Cai,1 Lin Wu,1 Jian-Jun Yang,2 Ying-Chun Dong1
1Department of Anesthesiology, Nanjing Stomatological Hospital, Affiliated Hospital of Medical School, Institute of Stomatology, Nanjing University, Nanjing, Jiangsu, People’s Republic of China; 2Department of Anesthesiology, Pain and Perioperative Medicine, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ying-Chun Dong, Department of Anesthesiology, Nanjing Stomatological Hospital, Affiliated Hospital of Medical School, Institute of Stomatology, Nanjing University, 30 Zhongyang Road, Nanjing, Jiangsu, 210008, People’s Republic of China, Tel +86-25-83620382, Email [email protected] Jian-Jun Yang, Department of Anesthesiology, Pain and Perioperative Medicine, The First Affiliated Hospital of Zhengzhou University, 1 Jianshe East Road, Zhengzhou, Henan, 450052, People’s Republic of China, Tel +86-371-66271657, Email [email protected]
Purpose: Abnormal liver function is common post-surgery and is linked to poor prognosis. We investigated whether intraoperative subanesthetic esketamine could improve postoperative liver function and recovery quality by reducing surgery-induced inflammation in patients with head and neck squamous cell carcinoma (HNSCC).
Patients and methods: In this randomized controlled trial, 172 hNSCC patients were randomly assigned to receive esketamine or saline intravenously. The primary outcome was serum alanine aminotransferase (ALT) on postoperative day (POD) 1. Secondary outcomes included aspartate aminotransferase (AST), abnormal liver function event (ALFE), inflammatory markers (serum C-reactive protein [CRP], white blood cell [WBC] count, neutrophil percentage (NE%) and the neutrophil-to-lymphocyte ratio [NLR]) on POD1, and recovery quality measured by the quality of recovery (QoR)-40 questionnaire on POD1 and POD7.
Results: The esketamine group showed a lower mean [standard deviation, SD] ALT (27.72 [13.04] vs 50.74 [20.14] U/L; P = 0.001), AST (20.88 [8.60] vs 26.05 [15.31] U/L; P =0. 007), rate of ALFE (12% vs 31%; odds ratio [OR], 95% confidence interval [CI]: 0.308, 0.138 to 0.688; P = 0.003), CRP (53.30 [22.98] vs 60.70 [23.51] mg/L; P = 0.039), WBC count (13.37 [3.40] vs 15.02 [3.97] 109/L; P = 0.004), NE% (85.58 [4.77] vs 87.38 [4.02]; P = 0.008), and NLR (15.05 [6.08] vs 17.25 [7.04]; P = 0.042), and higher QoR-40 scores on POD1 (171 [169 to 174] vs 168 [166 to 171]; P < 0.001) and POD7 (177 [174 to 180] vs 175 [172 to 178]; P < 0.001) compared to the control group.
Conclusion: Subanesthetic esketamine improved postoperative liver function and recovery quality in HNSCC patients, possibly by reducing surgery-induced inflammation.
Keywords: esketamine, inflammation, liver, recovery quality, surgery, randomized controlled trial
Introduction
Surgical procedures often trigger a variety of perioperative inflammatory reactions, which can lead to multi-system organ dysfunctions and increase perioperative morbidity and mortality.1 The intensity of this inflammatory response is influenced by factors such as the type of surgery, the degree of tissue trauma, surgery duration, ischemia-reperfusion injury (IRI), and blood loss and transfusion.2–4 Radical resection of lesions followed by microvascular free flap reconstructions is the standard treatment for major trauma, prolonged surgical duration, significant blood loss, and substantial hemodynamic fluctuations. Consequently, HNSCC patients are at higher risk for postoperative systemic inflammatory response and abnormal liver function.1,5 Evidence suggests that preoperative and postoperative liver dysfunction can lead to prolonged hospitalization, extended ICU stay, and increased mortality.6 Therefore, protecting liver function during surgery in HNSCC patients poses a significant challenge for anesthesiologists.
The choice of intraoperative medication is a critical factor influencing perioperative inflammatory response and organ function. Intravenous (IV) infusions of propofol and remifentanil have been shown to reduce systemic inflammation and improve postoperative liver and kidney function. However, even with total IV anesthesia primarily using propofol and remifentanil, serum liver enzymes and bilirubin levels often increase postoperatively.7–9 The search for an anesthetic drug that can effectively reduce inflammation while protecting perioperative liver function remains ongoing.
The impact of N-methyl-D-aspartate (NMDA) receptor antagonist ketamine on organ functions has been a subject of interest. Ketamine has been shown to cause liver and kidney damage in experimental animals.10,11 Interestingly, ketamine also demonstrated a hepatoprotective effect in lipopolysaccharide (LPS)-induced liver injury in rats by reducing COX-2 protein levels or HO-1 mediation.12,13 These diverse effects on the liver appear to be dose-dependent. Esketamine, the (S)-enantiomer of ketamine, has a higher affinity for NMDA receptors. It is increasingly used in perioperative care for cancer patients due to its potent analgesic effects,14,15 antidepressant and anxiolytic properties,16–18 improvement in postoperative sleep disturbances,19 and anti-inflammatory potential,20,21 all with mild psychological side effects. A study showed that subanesthetic doses of esketamine infusion did not affect kidney function during ischemic postconditioning in rats with renal IRI.22 Additionally, Xu and co-workers reported that esketamine alleviated carbon tetrachloride-induced liver injury by inhibiting oxidative stress and inflammatory cell infiltration through the Nrf2/HO-1 signaling pathway.23 However, the effect of intraoperative esketamine infusion on postoperative liver function remains unclear. Microvascular free flap reconstruction in HNSCC patients is associated with IRI, leading to oxidative stress, inflammation, and endothelial dysfunction. Therefore, we speculate that esketamine’s hepatoprotective effects may, in part, be due to its ability to mitigate IRI-induced damage and inflammation during the perioperative period.
This trial aimed to assess the effect of intraoperative subanesthetic dose of esketamine on postoperative liver function and recovery quality in HNSCC patients undergoing radical resection followed by microvascular reconstruction. As we know, this study is the first to explore the organ-protective effects of esketamine in patients with HNSCC.
Methods
Study Design and Ethics
This double-blinded, placebo-controlled randomized clinical trial was approved by the Institutional Scientific Research and Clinical Trials Ethics Committee of Nanjing Stomatological Hospital, Affiliated Hospital of Medical School, Nanjing University (No.: NJSH-2023NL-018-1). The trial was registered at https://www.chictr.org.cn (Registration No.: ChiCTR2300070945). No significant changes were made after the trial commenced. A total of 183 hNSCC patients were enrolled from June 2023 to June 2024. Written informed consent was obtained from all participants. This study complied with the Declaration of Helsinki and the CONSORT guidelines.
Participant Recruitment
Inclusion Criteria
- Patients diagnosed with HNSCC based on biopsy and scheduled for elective radical resection with functional reconstruction using microvascular free flaps under general anesthesia.
- Age 18–75 years, of either sex.
- American Society of Anesthesiologists (ASA) classification I-III.
- Voluntary participation with signed informed consent.
Exclusion Criteria
- Emergency or recurrent surgery.
- Body mass index (BMI) < 18 or ˃ 30 kg/m2, calculated as weight in kilograms divided by height in meters squared.
- Abnormal liver function defined as serum alanine aminotransferase (ALT) or aspartate aminotransferase (AST) > 40 U/L.
- Severe cardiovascular, pulmonary, renal, or liver diseases, alcohol or drug abuse, neuropsychiatric disease, hyperthyroidism, or glaucoma.
- Uncontrolled hypertension (baseline > 180/100 mm Hg), or diabetes (fasting blood glucose > 8.0 mmol/L).
- Surgery duration less than 5 hours.
- Recent use of sedatives, antidepressants, glucocorticoids, hypnotics, or analgesics within the last 3 months.
- Communication impairment due to cognitive or audio-visual issues.
- Contraindications or allergy to esketamine.
Randomization and Blinding
Eligible patients were randomly assigned in a 1:1 ratio to receive either IV esketamine or placebo using computer-generated randomization table (http://www.random.org). Group assignments were sealed in envelopes and managed by a nurse anesthetist not involved in data collection, postoperative follow-up, or analysis. The anesthesiologists (XLL, XCC, LW and YCD) managing intraoperative care and postoperative follow-up were blinded to the group assignment.
Study Intervention
The esketamine group received an IV loading dose of 0.5 mg/kg esketamine (Jiangsu Hengrui Pharmaceutical Co., Ltd). before incision, followed by a continuous infusion 0.2 mg/kg/h during surgery until 30 minutes before the procedure’s end. For infusion, 50 mg esketamine was diluted with normal saline to a total volume of 20 mL for loading dose, 50 mL for maintenance dose. The control group received an equivalent volume of normal saline. Infusions were prepared by the same nurse anesthetist for both groups.
Anesthesia and Postoperative Management
No premedication was given. Routine monitoring included electrocardiogram (ECG), blood pressure, pulse oxygen saturation, end-expiratory carbon dioxide, and bispectral index (BIS). A radial artery catheter was used for real-time arterial blood pressure and gas monitoring, and a femoral vein catheter for liquid input and blood sampling. Anesthesia was induced with midazolam (0.02–0.06 mg/kg), propofol (1–2 mg/kg), sufentanil (0.2–0.4 μg/kg), and cisatracurium (0.3 mg/kg) for intubation or tracheotomy. Maintenance involved propofol (4–5 mg/kg), remifentanil (0.1–0.2 μg/kg/min), and 1% sevoflurane in 60% O2/air, keeping heart rate and systolic blood pressure within 20% of baseline. BIS was maintained between 40–60. Vasoactive drugs such as atropine, ephedrine or deoxyepinephrine, were administered as needed. A loading dose of 0.2–0.4 μg/kg sufentanil was given before incision, and no sufentanil was added afterwards. Postoperative pain was managed by a patient-controlled IV analgesia pump containing dezocine 20 mg, tropisetron 10 mg, and dexmedetomidine 1 μg/kg in 100 mL normal saline. Patients were transferred to the postoperative intensive care unit (ICU) with nasal endotracheal or tracheotomy tubes for further observation.
Data Collection and Outcome Assessment
Blood samples were collected from the femoral vein preoperatively and on postoperative day (POD) 1 to measure the serum levels of liver enzymes and bilirubin levels using an automatic biochemistry analyzer (SIEMENS, ADVIA® 1800). Blood cell analysis was performed using an automatic hematology analyzer (Sysmex Corporation, XS-9001). The biochemical analyzer and automatic hematology analyzer are calibrated according to Chinese quality control requirements and the manufacturers’ instructions. The primary outcome was serum ALT level on POD1. Secondary outcomes are listed as follows:
- Serum levels of AST, total bilirubin (TBI), direct bilirubin (DBI), and indirect bilirubin (IBI) on POD1.
- Incidence of abnormal liver function events (ALFE) on POD1, defined as ALT or AST > 40 U/L.24
- Serum C-reactive protein (CRP) levels, white blood cell (WBC) count, neutrophil percentage (NE%) and the neutrophil-to-lymphocyte ratio (NLR) on POD1. NE% was calculated by dividing the absolute neutrophil count by WBC count while the NLR was done by dividing the absolute neutrophil count by the absolute lymphocyte count.
- Recovery Quality measured by the QoR-40 questionnaire on POD1 and POD7, which assesses pain, physical comfort, physical independence, emotional state, and psychological support. Scores range from 0 to 200, with higher scores indicating better recovery.
Additional data included cumulative anesthetic drug use (sufentanil, remifentanil and propofol), surgery duration, infusion volume (crystalloid, colloidal solution, red blood cell and fresh frozen plasma infusion), estimated blood loss, urine output, vasoactive drugs (atropine, ephedrine, or phenylephrine) use, and incidence of postoperative adverse events, including nausea, vomiting, blurred vision, diplopia, restlessness, and nightmares.
Sample Size Calculation
Based on pre-experimental data showing mean ALT levels of 44.35 U/mL in the control group and 37.68 U/mL in the esketamine group on POD1, with an assumed standard deviation (SD) of 12.62 U/mL, 77 patients per group were needed to detect a significant difference with 90% power and a two-sided α of 0.05. Considering a 10% dropout rate, 86 patients were planned for each group. Sample size was calculated using PASS 15.0 software, version 15.0 (NCSS).
Statistical Analysis
Continuous variables with a normal distribution, as verified by Kolmogorov–Smirnov test, were expressed as mean±SD and compared between the two groups using an independent-sample t-test. For variables with a non-normal distribution, the median and interquartile range (IQR) were used, and comparisons were made using the Mann–Whitney U-test. Categorical variables, presented as numbers or percentages, were compared using the χ2 test or Fisher’s exact test. Statistical analyses were performed using SPSS version 24.0 (IBM, Armonk, NY, USA), with a two-sided P < 0.05 considered statistically significant.
Results
Patients
A total of 183 patients were initially enrolled in the study. One patient declined to participate and 10 patients were excluded due to surgery cancellation – 7 for an upper respiratory tract infection and others due to a change in the planned surgical procedure (Figure 1). One patient in the control group was eliminated who developed postoperative hematoma exploration. Therefore, this left 171 patients were followed up in two groups: the control group (n=85; mean [SD] age, 59.79 [12.79] years) and the esketamine group (n=86; mean [SD] age, 58.24 [12.29] years) (Table 1). Demographic data, including age, gender, BMI, ASA physical status, preexisting medical conditions, microvascular free flap type, and preoperative total QoR-40 scores, were comparable between the two groups (Table 1).
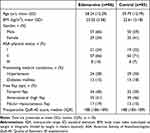 |
Table 1 Subject and Baseline Characteristics |
 |
Figure 1 Participant Flowchart. |
Efficacy Outcomes
The cumulative consumptions of anesthetics were significantly lower in the esketamine group compared to the control group: sufentanil (median [IQR], 20 [20 to 30] vs 30 [25 to 40] μg; P = 0.020), remifentanil (median [IQR], 1.75 [1.51 to 2.00] vs 1.90 [1.58 to 2.41] mg; P = 0.029), and propofol (median [IQR], 1680 [1450 to 1980] vs 1860 [1580 to 2220] mg; P = 0.039). No significant differences were observed in surgery duration, intraoperative liquid input and output, or the use of vasoactive drugs between the two groups (Table 2).
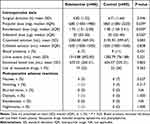 |
Table 2 Perioperative Parameters |
Baseline serum levels of ALT, AST, TBI, DBI, IBI, CRP, WBC count, NE% and NLR were similar between the two groups. However, on POD1, the esketamine group had significantly lower serum ALT (27.72 [13.04] vs 50.74 [20.14] U/L; P = 0.001), AST (20.88 [8.60] vs 26.05 [15.31] U/L; P =0. 007), incidence of ALFE (12% vs 31%; odds ratio [OR], 95% confidence interval [CI]: 0.308, 0.138 to 0.688; P = 0.003), CRP (53.30 [22.98] vs 60.70 [23.51] mg/L; P = 0.039), WBC count (13.37 [3.40] vs 15.02 [3.97] 109/L; P = 0.004), NE% (85.58 [4.77] vs 87.38 [4.02]; P = 0.008), and NLR (15.05 [6.08] vs 17.25 [7.04]; P = 0.042) compared to the control group. There were no significant differences in serum TBI, DBI or IBI levels between the two groups on POD1 (Table 3).
 |
Table 3 Liver Functions and Inflammatory Markers |
The total QoR-40 scores were significantly higher in the esketamine group on both POD1 (171 [169 to 174] vs 168 [166 to 171]; P < 0.001) and POD7 (177 [174 to 180] vs 175 [172 to 178]; P < 0.001). Notably, the esketamine group showed significant improvements in pain (POD1: 29 [29 to 30] vs 28 [27 to 29]; P < 0.001), physical comfort (POD1: 51 [49 to 53] vs 50 [46 to 52]; P = 0.004), and emotional state (POD1: 39 [38 to 40] vs 38 [36 to 39]; P < 0.001); POD7: 41 [40 to 42] vs 40 [39 to 40]; P < 0.001). However, no significant differences were observed in postoperative physical independence or psychological support scores between the two groups (Figure 2).
Safety Outcomes
There were no significant differences in adverse reactions between the two groups on POD1. Nightmares and diplopia were reported by one patient in the esketamine group on POD1 (Table 2).
Discussion
The present study demonstrated that intraoperative esketamine infusion significantly reduced serum levels of ALT and AST, alleviated systemic inflammation response, and increased postoperative recovery quality in HNSCC patients undergoing radial resection followed by microvascular reconstruction. Previous research has shown that both the analgesic and adverse effects of esketamine are dose-dependent, a subanesthetic dose of esketamine can maintain its anti-inflammatory activity and analgesic efficacy while minimizing neuropsychiatric side effects, such as hallucinations, nightmares, and delirium.25–27 Based on these findings, this study opted for a subanesthetic dose (0.5 mg/kg followed by a continuous infusion of 0.2 mg/kg/h) as informed by prior research outcomes.28–30
This study found that patients with normal preoperative liver function experienced abnormal liver function after surgery, with an incidence of ALFE at 31%. Esketamine infusion lowered postoperative ALT and AST levels significantly with the incidence of ALFE at only 12%. The results suggested that a subanesthetic dose of esketamine may help protect the liver by mitigating damage to the liver cell membrane in patients undergoing head and neck cancer surgery. However, there was no significant difference in postoperative serum bilirubin levels between the two groups. This could be due to the limited sensitivity of TBI, DBI, or IBI in indicating liver function. Alternatively, it may suggest that elevated serum bilirubin levels post-surgery primarily are caused by hemolysis from major surgical trauma rather than liver hypoperfusion or hepatocyte injury.31 According to Shang and et.al, abnormal levels of ALT, AST, and TBI are associated with lower 90-day and 4-year survival and can serve as independent risk factors for prognosis in cardiac surgeries.6 Therefore, a subanesthetic dose of esketamine may provide both short-term and long-term survival benefits for HNSCC patients.
The underlying mechanisms of esketamine’s protective effect on liver remains unclear. During surgery, patients often experience a systemic inflammation response involving neutrophils activation, pro-inflammatory cytokine release, and glycocalyx damage, all of which can lead to abnormal liver function postoperatively.1 Our findings indicate that esketamine possesses potent anti-inflammatory effects, as evidenced by reductions in CRP levels, WBC count, NE%, and NLR, which were consistent with the previous studies.21,27 NLR is a biomarker that is closely correlated with systemic inflammation and poor prognosis in solid tumors including HNSCC.32 Many recent studies demonstrated the NLR was a prognostic indicator for overall and cancer-specific survival in HNSCC, and elevated NLR in HNSCC patients confers a poor prognosis.33,34 Taken together, it is plausible that esketamine’s liver-protective effects during surgery may arise from its anti-inflammatory and anti-stress properties, and intraoperative esketamine administration may be useful for the prognosis for patients with HNSCC due to the anti-inflammatory property. However, further research is needed to fully elucidate the underlying mechanism.
In this study, we found that patients in the esketamine group required significantly lower doses of remifentanil and sufentanil, indicating that esketamine has reliable analgesic properties. Given esketamine’s moderate affinity for μ-type opioid receptor,35,36 it is likely that this interaction contributes to the reduced need for remifentanil and sufentanil. Remifentanil is known be hydrolyzed by non-specific esterases in the body, without impacting hepatic or renal functions. On the other hand, sufentanil offers protection against hepatic IRI by downregulating inflammatory factors such as hypoxia-inducible factor 1α (HIF-1a), tumor necrosis factor-α (TNF-a), IL-1β, and IL-6 through the suppression of p38/ERK/JNK/NF-kB-p65/COX2 signal pathways.37 Therefore, the hepatoprotective effect may be due to esketamine itself rather than reduced consumptions of opioid usage. Future research should adjust opioid dose in multivariable analysis to isolate esketamine’s direct hepatoprotective effects. Additionally, total propofol consumption decreased by approximately 10% in the present study. Esketamine has been shown to reduce propofol consumption in a dose-dependent manner during certain endoscopic surgeries, while maintaining the same level of sedation.38,39 These findings indicates that esketamine has reliable sedative properties in addition to its analgesic effects. Moreover, we observed a transient elevation in BIS value following esketamine infusion during anesthesia induction, although the BIS value did not differ during anesthesia maintenance. Esketamine has been reported to increase BIS value in children during gastro-duodenoscopy at doses of 0.3 and 0.5 mg/kg, with propofol consumptions similar to that of the placebo. These results suggest that BIS value alone may not be sufficient to monitor anesthesia depth when esketamine is used.40 Further investigation is needed to understand the relationship between esketamine dosage and BIS value during surgery.
Using the overall QoR-40 score, we found that esketamine infusion during surgery contributed to enhanced postoperative recovery quality, with patients experiencing less pain, better physical comfort, and an improved emotional state. Accumulating evidence suggest that esketamine had the potential to improve postoperative pain and sleep quality, as well as to provide rapid and sustained antidepressant effects in patients with treatment-resistant depression, though transient psychotomimetic and dissociative adverse effects have been observed.17,19,41,42 Additionally, esketamine has been shown to improve postoperative depression-like symptoms through its anti-inflammatory effects, partly mediated by the brain-derived neurotrophic factor (BDNF)/TrkB signaling pathway.20 There were no significant difference between the two groups in terms of intraoperative liquid input and output, use of vasoactive drugs, or postoperative adverse events. Overall, intraoperative subanesthetic dose of esketamine appear to be safe and effective, offering benefits linked to its analgesic, antidepressant, and sleep-enhancing properties.
Limitations
There are several limitations to this study. First, it is a single-center study with a relatively small sample size, focusing exclusively on HNSCC patients, which may introduce bias. Future multicenter RCTs with larger and more diverse populations are needed to confirm these findings. Second, previous reports indicate that the incidence of preoperative abnormal ALT or AST is 3.6% or 9.3%, respectively,43 and that 12.6% of HNSCC patients have abnormal liver enzyme levels before surgery.44 However, this study only included patients with normal preoperative liver function, so the effects of esketamine on preexisting abnormal liver function require further investigation. Third, liver function was only assessed on the first day after surgery, leaving the long-term effect of esketamine on liver unknown. Finally, this study only examined a subanesthetic dose of esketamine, so additional research is needed to explore different dosage regimens and the dose-response relationship of esketamine.
Conclusions
This study suggests that intraoperative infusion of subanesthetic esketamine may benefit postoperative liver function and recovery quality in HNSCC patients undergoing radical resection followed by microvascular flap reconstruction, likely by attenuating the systemic inflammatory responses induced by major surgery. Further studies are needed to confirm these findings and to explore the underlying mechanisms.
Data Sharing Statement
The individual deidentified participant data, the study protocol, and the statistical analysis plan can be accessed from the corresponding author upon reasonable request.
Acknowledgments
We extend our sincere gratitude to all the patients for their participation in this study. We also thank the anesthesiologists, surgeons, and nursing staff at Nanjing Stomatological Hospital for their invaluable support throughout the research process.
Funding
This study was supported by the National Natural Science Foundation of China (grant No. 81772880) and High-Level Hospital Construction Project of Nanjing Stomatological Hospital, Affiliated Hospital of Medical School, Institute of Stomatology, Nanjing University (grant No. 0224C058).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Margraf A, Ludwig N, Zarbock A, Rossaint J. Systemic inflammatory response syndrome after surgery: mechanisms and protection. Anesth Analg. 2020;131:1693–1707. doi:10.1213/ANE.0000000000005175
2. Squiccimarro E, Labriola C, Malvindi PG, et al. Prevalence and clinical impact of systemic inflammatory reaction after cardiac surgery. J Cardiothorac Vasc Anesth. 2019;33:1682–1690. doi:10.1053/j.jvca.2019.01.043
3. Stevens JL, Feelisch M, Martin DS. Perioperative oxidative stress: the unseen enemy. Anesth Analg. 2019;129:1749–1760. doi:10.1213/ANE.0000000000004455
4. Mantziari S, Hubner M, Coti-Bertrand P, et al. A novel approach to major surgery: tracking its pathophysiologic footprints. World J Surg. 2015;39:2641–2651. doi:10.1007/s00268-015-3181-7
5. Jeong GA, Cho GS, Shin EJ, et al. Liver function alterations after laparoscopy-assisted gastrectomy for gastric cancer and its clinical significance. World J Gastroenterol. 2011;17:372–378. doi:10.3748/wjg.v17.i3.372
6. Shang L, Ao Y, Lv L, et al. Preoperative liver function test abnormalities were associated with short-term and long-term prognosis in cardiac surgery patients without liver disease. Front Cardiovasc Med. 2021;8:772430. doi:10.3389/fcvm.2021.772430
7. Jiang Q, Song X, Chen Z, Wang C, Luo H. Effects of remifentanil on hemodynamics, liver function and ICAM-1 expression in liver cancer patients undergoing surgery. Oncol Lett. 2017;14:872–876. doi:10.3892/ol.2017.6247
8. Matsumi J, Sato T. Protective effect of propofol compared with sevoflurane on liver function after hepatectomy with Pringle maneuver: a randomized clinical trial. PLoS One. 2023;18:e0290327. doi:10.1371/journal.pone.0290327
9. Oladimeji MA, Desalu I, Adekola OO, Akanmu O, Adesida AA. A comparison of the effect of isoflurane and propofol on liver enzymes. J West Afr Coll Surg. 2022;12:28–33. doi:10.4103/jwas.jwas_69_22
10. Uahomo PO, Isirima JC. Attenuating ketamine-induced nephrotoxicity with bryophyllum pinnatum extract: biochemical and histological investigation. J Complement Altern Med Res. 2025;26:21–36. doi:10.9734/jocamr/2025/v26i1612
11. Uahomo PO, Isirima JC. Biochemical and histological assessment of the hepatoprotective effects of Bryophyllum pinnatum leaf extract in Ketamine-induced liver toxicity in male Wistar rats. J Res Appl Basic Med Sci. 2025;11:32–47. doi:10.61186/rabms.11.1.32
12. Suliburk JW, Helmer KS, Gonzalez EA, Robinson EK, Mercer DW. Ketamine attenuates liver injury attributed to endotoxemia: role of cyclooxygenase-2. Surgery. 2005;138:134–140. doi:10.1016/j.surg.2005.03.024
13. Suliburk JW, Ward JL, Helmer KS, et al. Ketamine-induced hepatoprotection: the role of heme oxygenase-1. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1360–1369. doi:10.1152/ajpgi.00038.2009
14. Liu J, Wang T, Song J, Cao L. Effect of esketamine on postoperative analgesia and postoperative delirium in elderly patients undergoing gastrointestinal surgery. BMC Anesthesiol. 2024;24:46. doi:10.1186/s12871-024-02424-w
15. Zheng H, Zhang P, Shi S, et al. Sub-anesthetic dose of esketamine decreases postoperative opioid self-administration after spine surgery: a retrospective cohort analysis. Sci Rep. 2024;14:3909. doi:10.1038/s41598-024-54617-5
16. Lou XJ, Qiu D, Ren ZY, et al. Efficacy and safety of esketamine for perioperative depression in patients undergoing elective surgery: a meta-analysis of randomized controlled trials. Asian J Psychiatr. 2024;95:103997. doi:10.1016/j.ajp.2024.103997
17. Singh JB, Fedgchin M, Daly E, et al. Intravenous esketamine in adult treatment-resistant depression: a double-blind, double-randomization, placebo-controlled study. Biol Psychiatry. 2016;80:424–431. doi:10.1016/j.biopsych.2015.10.018
18. Zhou D, Liu F, Jiang F, et al. Sub-anesthesia dose of s-ketamine reduces postoperative pain and anxiety in patients receiving breast and thyroid surgery: a randomized, controlled trial. Pain Physician. 2023;26:257–264. doi:10.36076/ppj.2023.26.257
19. Qiu D, Wang XM, Yang JJ, et al. Effect of intraoperative esketamine infusion on postoperative sleep disturbance after gynecological laparoscopy: a randomized clinical trial. JAMA Network Open. 2022;5:e2244514. doi:10.1001/jamanetworkopen.2022.44514
20. Wang T, Weng H, Zhou H, et al. Esketamine alleviates postoperative depression-like behavior through anti-inflammatory actions in mouse prefrontal cortex. J Affect Disord. 2022;307:97–107. doi:10.1016/j.jad.2022.03.072
21. Welters ID, Feurer MK, Preiss V, et al. Continuous S-(+)-ketamine administration during elective coronary artery bypass graft surgery attenuates pro-inflammatory cytokine response during and after cardiopulmonary bypass. Br J Anaesth. 2011;106:172–179. doi:10.1093/bja/aeq341
22. de Resende MA, Pantoja AV, Barcellos BM, et al. Ischemic postconditioning and subanesthetic S(+)-Ketamine infusion: effects on renal function and histology in rats. Biomed Res Int. 2015;2015:864902. doi:10.1155/2015/864902
23. Xu W, Wang P, Wang D, et al. S-ketamine alleviates carbon tetrachloride-induced hepatic injury and oxidative stress by targeting the Nrf2/HO-1 signaling pathway. Can J Physiol Pharmacol. 2021;99:1308–1315. doi:10.1139/cjpp-2020-0763
24. Ding ZY, Li GX, Chen L, et al. Association of liver abnormalities with in-hospital mortality in patients with COVID-19. J Hepatol. 2021;74:1295–1302. doi:10.1016/j.jhep.2020.12.012
25. Sloekers JCT, Bos M, Hoogland G, et al. Assessing the effectiveness of perioperative s-ketamine on new-onset headache after resective epilepsy surgery (ESPAIN-trial): protocol for a randomised, double-blind, placebo-controlled trial. BMJ Open. 2019;9:e030580. doi:10.1136/bmjopen-2019-030580
26. Wang X, Lin C, Lan L, Liu J. Perioperative intravenous S-ketamine for acute postoperative pain in adults: a systematic review and meta-analysis. J Clin Anesth. 2021;68:110071. doi:10.1016/j.jclinane.2020.110071
27. Zhang J, Ma Q, Li W, Li X, Chen X. S-Ketamine attenuates inflammatory effect and modulates the immune response in patients undergoing modified radical mastectomy: a prospective randomized controlled trial. Front Pharmacol. 2023;14:1128924. doi:10.3389/fphar.2023.1128924
28. Argiriadou H, Himmelseher S, Papagiannopoulou P, et al. Improvement of pain treatment after major abdominal surgery by intravenous S+-ketamine. Anesth Analg. 2004;98:1413–1418. doi:10.1213/01.ane.0000111204.31815.2d
29. Argiriadou H, Papagiannopoulou P, Foroulis CN, et al. Intraoperative infusion of S(+)-ketamine enhances post-thoracotomy pain control compared with perioperative parecoxib when used in conjunction with thoracic paravertebral ropivacaine infusion. J Cardiothorac Vasc Anesth. 2011;25:455–461. doi:10.1053/j.jvca.2010.07.011
30. Wang H, Duan CY, Huang WQ, et al. Perioperative intravenous S(+)-ketamine for acute postoperative pain in adults: study protocol for a multicentre, randomised, open-label, positive-controlled, pragmatic clinical trial (SAFE-SK-A trial). BMJ Open. 2021;11:e054681. doi:10.1136/bmjopen-2021-054681
31. Allen LA, Felker GM, Pocock S, et al. Liver function abnormalities and outcome in patients with chronic heart failure: data from the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) program. Eur J Heart Fail. 2009;11:170–177. doi:10.1093/eurjhf/hfn031
32. Guthrie GJ, Charles KA, Roxburgh CS, et al. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88:218–230. doi:10.1016/j.critrevonc.2013.03.010
33. Yang L, Huang Y, Zhou L, Dai Y, Hu G. High pretreatment neutrophil-to-lymphocyte ratio as a predictor of poor survival prognosis in head and neck squamous cell carcinoma: systematic review and meta-analysis. Head Neck. 2019;41:1525–1535. doi:10.1002/hed.25583
34. Ferrandino RM, Roof S, Garneau J, et al. Neutrophil-to-lymphocyte ratio as a prognostic indicator for overall and cancer-specific survival in squamous cell carcinoma of the head and neck. Head Neck. 2020;42:2830–2840. doi:10.1002/hed.26329
35. Hirota K, Lambert DG. Ketamine; history and role in anesthetic pharmacology. Neuropharmacology. 2022;216:109171. doi:10.1016/j.neuropharm.2022.109171
36. Hirota K, Okawa H, Appadu BL, et al. Stereoselective interaction of ketamine with recombinant mu, kappa, and delta opioid receptors expressed in Chinese hamster ovary cells. Anesthesiology. 1999;90:174–182. doi:10.1097/00000542-199901000-00023
37. Lian YH, Fang J, Zhou HD, Jiang HF, Xie KJ. Sufentanil preconditioning protects against hepatic ischemia-reperfusion injury by suppressing inflammation. Med Sci Monit. 2019;25:2265–2273. doi:10.12659/MSM.913145
38. Eberl S, Koers L, van Hooft J, et al. The effectiveness of a low-dose esketamine versus an alfentanil adjunct to propofol sedation during endoscopic retrograde cholangiopancreatography: a randomised controlled multicentre trial. Eur J Anaesthesiol. 2020;37:394–401. doi:10.1097/EJA.0000000000001134
39. Zheng XS, Shen Y, Yang YY, et al. ED(50) and ED(95) of propofol combined with different doses of esketamine for children undergoing upper gastrointestinal endoscopy: a prospective dose-finding study using up-and-down sequential allocation method. J Clin Pharm Ther. 2022;47:1002–1009. doi:10.1111/jcpt.13635
40. Wang J, Hu W, Zhao X, et al. Sedative effect and safety of different doses of S-ketamine in combination with propofol during gastro-duodenoscopy in school-aged children: a prospective, randomized study. BMC Anesthesiol. 2022;22:346. doi:10.1186/s12871-022-01885-1
41. Lahtinen P, Kokki H, Hakala T, Hynynen M. S(+)-ketamine as an analgesic adjunct reduces opioid consumption after cardiac surgery. Anesth Analg. 2004;99:1295–1301. doi:10.1213/01.ANE.0000133913.07342.B9
42. Reif A, Bitter I, Buyze J, et al. Esketamine nasal spray versus quetiapine for treatment-resistant depression. N Engl J Med. 2023;389:1298–1309. doi:10.1056/NEJMoa2304145
43. Korver KD, Graham SM, Hoffman HT, McCulloch T, Funk GF. Liver function studies in the assessment of head and neck cancer patients. Head Neck. 1995;17:531–534. doi:10.1002/hed.2880170611
44. Chen PG, Schoeff SS, Watts CA, et al. Utility of abdominal imaging to assess for liver metastasis in patients with head and neck cancer and abnormal liver function tests. Am J Otolaryngol. 2014;35(2):137–140. doi:10.1016/j.amjoto.2013.10.004
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


