Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 20
Effect of Telemonitoring on Moderate and Severe Exacerbations in Patients with COPD: Pooled Analysis of Two Randomized Controlled Trials in Denmark
Authors Hyldgaard C , Ringbæk T , Andersen FD, Hansen EF , Jensen MS, Fenger-Grøn M , Trolle C , Ulrik CS
Received 3 April 2025
Accepted for publication 1 July 2025
Published 11 July 2025 Volume 2025:20 Pages 2361—2369
DOI https://doi.org/10.2147/COPD.S528852
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Fanny Wai San Ko
Charlotte Hyldgaard,1,2 Thomas Ringbæk,3 Frank Dyekjær Andersen,1 Ejvind Frausing Hansen,4 Michael Skov Jensen,1 Morten Fenger-Grøn,1 Christian Trolle,1,2 Charlotte Suppli Ulrik4,5
1Medical Diagnostic Center, University Clinic for Innovative Patient Pathways, Regional Hospital Central Jutland, Silkeborg/Viborg, Denmark; 2Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 3Allergy and Lung Clinic, Helsingør, Denmark; 4Respiratory Research Unit and Department of Respiratory Medicine, Copenhagen University Hospital- Hvidovre, Hvidovre, Denmark; 5Institute for Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Correspondence: Charlotte Hyldgaard, Medical Diagnostic Center, University Clinic for Innovative Patient Pathways, Regional Hospital Central Jutland, Falkevej 1-3, Silkeborg, 8600, Denmark, Email [email protected]
Background: Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) are serious events with high morbidity and mortality. Previous studies investigated telemonitoring as a tool for prevention of hospitalizations with ambiguous results. The aim of the present study was to combine data from two randomized controlled trials conducted in Denmark in similar healthcare settings to explore number of hospitalizations for COPD, days of admission, and exacerbations treated outside hospitals.
Methods: Recruitment took place during hospitalization for AECOPD and from outpatient COPD clinics. Patients were equally randomized to telemonitoring (N=251) in addition to usual care for six months or usual care alone (N=252). We used a negative binomial regression model with between-group comparisons expressed as incidence rate ratios (IRRs) for assessment of hospitalizations, admission days and moderate exacerbations and Kaplan-Meier time-to-event analysis for assessment of time to first COPD hospitalization.
Results: No significant differences between the two studies were identified. In combined analyses, numerically fewer hospitalizations (IRR 0.85, 95% CI 0.62– 1.17) and hospitalization days (IRR 0.72, 95% CI 0.42– 1.23) were seen in the telemonitoring group, but the findings did not reach statistical significance whereas treatment for moderate exacerbations was significantly more frequent in the telemonitoring group (IRR 1.91, 95% CI 1.49– 2.45).
Conclusion: No effect of telemonitoring on hospitalizations for AECOPD was documented in this large cohort of patients with severe COPD. However, the telemonitoring group received significantly more treatment for moderate exacerbations. This risk of overtreatment should be considered when telemonitoring is used in the care of patients with COPD.
Keywords: chronic obstructive pulmonary disease, telemonitoring, exacerbations, hospitalization
Introduction
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is a serious complication with high morbidity and mortality. Telemonitoring has been investigated as a tool for preventing hospitalizations and improvement of care, but with ambiguous results. Several large, well-conducted studies of telemonitoring as the only addition to standard care have failed to show a reduction in COPD hospitalizations.1–3 A meta-analysis of telemonitoring as addition to usual care showed no effect of the intervention on hospital admission for acute exacerbation (10 studies, 1290 patients), but showed a small reduction in emergency room visits for acute exacerbation (7 studies, 875 patients).4
The first study in Denmark of telemonitoring in COPD showed a reduction in hospital admissions in the intervention group,5 but in the following larger study, the positive effect of telemonitoring on admissions was not retrieved, and no improvement in admissions days or quality of life was seen.6,7
Two randomized controlled trials of telemonitoring in COPD have been conducted in comparable healthcare settings in Denmark, one in the Capital Region8 and one in the Central Denmark Region.9
One showed no significant difference in the mean number of hospitalizations with AECOPD (0.55 vs 0.54, p=0.74)8 and the other showed significantly fewer hospitalizations in the telemonitoring group (IRR 0.70, 95% CI 0.51–0.96).9 Both studies reported no significant reduction with telemonitoring in time to first AECOPD hospitalization or number of admission days with AECOPD. Results regarding health-related quality of life (QoL) have also been published; the study from the Capital Region showed an improvement of within group and between group QoL using the 15D QoL questionnaire with the improvement mainly seen among patients with poorest QoL score at baseline, whereas the study from the Central Denmark Region documented no significant difference between groups using the Hospital Anxiety and Depression Scale and the Saint George Respiratory Questionnaire.10,11
The study from the Capital Region reported a significantly higher number of exacerbations treated outside hospital, classified as moderate exacerbations by the definition used at the time of the study,12 in the telemonitoring group. Data on this outcome have not previously been reported from the Central Denmark cohort.
This finding raises concern due to the risk of side effects associated with corticosteroid therapy13,14 if clear benefit of the extra treatment is uncertain.
The use of telemonitoring in COPD is currently being implemented in Denmark as part of a national strategy aiming at improving COPD care, especially for patients with the highest symptom burden and risk of hospitalization.15
The aim of this study was to compare and combine data from the two Danish telemonitoring studies focusing on hospital admissions for AECOPD, admission days with AECOPD, time to hospitalization with AECOPD, and treated exacerbations without hospitalization.
Methods
We included patients who participated in two previously conducted randomized trials:
In the Central Denmark Region, patients were included at hospital admission for AECOPD in case of a FEV1<50% prior to hospitalization or of suspected severe COPD if no spirometry prior to hospitalization was available.
In the Capital Region, patients diagnosed with COPD with FEV1<60% were included in the outpatient clinic if they had been admitted to hospital for AECOPD within the preceding 36 months and/or had been treated with long-term oxygen for at least three months.
All patients were randomized to telemonitoring for six months in addition to usual care or to usual care alone.
Inclusion took place between March 2011 and July 2016 at the regional hospitals in Viborg and Silkeborg in Central Denmark and between November 2013 and April 2014 at four respiratory outpatient clinics at hospitals in the Capital Region (Hvidovre Hospital, Amager Hospital, Herlev Hospital and Bispebjerg Hospital).
Usual Care
Usual care provided to all study participants consisted of pharmacological and non-pharmacological treatment according to clinical recommendations for COPD and regular follow-up with 3–6 months intervals at the respiratory outpatient clinic or home visits by specialized respiratory nurses if required.
Intervention
In both studies, the telemonitoring intervention included measurements of oxygen saturation, heart rate, and body weight as well as changes in dyspnea, sputum color, volume, and purulence. In the Capital Region study, home spirometry was performed as part of the intervention, while the Central Denmark study included peak flow measurements. In both studies, spirometry was used as part of regular follow-up. In the Capital Region study, home measurements were taken three times a week for the first four weeks and then once a week. Video consultations including spirometry were scheduled once a week for the first four weeks, and once a month for the remaining five months of the study period. In the Central Denmark study, the patients conducted home measurements on all weekdays for the first month and then three times a week. Video consultations were not included. In both studies, the patients could perform additional measurements as needed. An algorithm generated alerts if a trend of worsening was detected, resulting in the patient being contacted by a respiratory nurse. Further details of the telemonitoring intervention and usual care have been reported previously.8,9
Statistical Analysis
Data were analyzed by the intention-to-treat principle. Clinical characteristics at baseline are presented for each treatment group. Continuous variables are presented with medians and ranges, and categorical variables with numbers and percentages. Comparison was made using Wilcoxon rank-sum for continuous data and chi-square test for categorical data. We compared the number of hospital admissions, admission days with AECOPD, and moderate exacerbations using a negative binomial regression model estimating incidence rate ratios (IRR) with corresponding 95% confidence intervals (CIs). Results are reported with the control group as reference. All models accounted for the participants´ follow-up time, ie time until death or exclusion in case of withdrawal of informed consent. As sensitivity analyses, additional adjustments were made for center/region as well as gender and cohabitation status which were unevenly distributed in the randomization. Time to first COPD hospitalization was assessed using Kaplan-Meier time-to-event analysis with time of inclusion as index date and comparison by the Log rank test.
Ethical Considerations
All patients gave written informed consent prior to inclusion. The studies were approved by the Research Ethics Committee of the Capital Region of Denmark (H-4-2013-052) and the Central Denmark Region (M-20100242) and complies with the Declaration of Helsinki.
Results
A total of 1093 patients underwent screening, and 503 (46%) met the inclusion criteria and were included in the studies after providing informed consent; 251 were randomized to the telemonitoring group and 252 to the control group. Sixteen patients in the telemonitoring group (6.4%) and 13 patients in the control group (5.2%) died during the study period and 16 (6.4%) and 22 (8.7%) discontinued for other reasons (Figure 1). Clinical characteristics are shown in Table 1. The percentage of women and participants living alone were higher in the telemonitoring group, but other clinical characteristics were similar between the groups. Clinical characteristics for each sub-cohort are shown in supplementary Table 1S. Minor differences were seen between centers; the Capital Region cohort had slightly higher median BMI and percentage of patients living alone, and lower median FEV1 and percentage of patients on long-term oxygen therapy.
 |
Figure 1 Consort diagram. |
 |
Table 1 Clinical Characteristics |
In the telemonitoring group, 33% experienced AECOPD hospital admission during the six-months study period compared with 36% in the control group. No significant difference was seen in time to first hospitalization using the Log rank test, p=0.24 (Figure 2). The total number of hospitalizations for AECOPD was 133 in the telemonitoring group and 155 in the control group, corresponding to insignificantly fewer hospitalizations in the telemonitoring group, crude IRR 0.85, 95% CI 0.62–1.17) and IRR 0.87, 95% CI 0.63–1.19 after adjustment for gender, cohabitation status and center. The number of admission days with AECOPD was insignificantly lower with 468 in the telemonitoring group and 684 in the control group, crude IRR 0.72, 95% CI 0.42–1.23 and adjusted IRR 0.82, 95% CI 0.49–1.40.
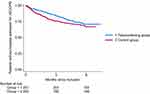 |
Figure 2 Kaplan-Meier plot showing time to first hospitalization for exacerbation of COPD. No significant difference was seen between the groups, log-rank p=0.24. |
Treatment with corticosteroids and/or antibiotics for moderate exacerbations without hospitalization was significantly more frequent in the telemonitoring group, 333 in the telemonitoring group and 174 in the control group, crude IRR 1.91, 95% CI 1.49–2.45 and adjusted IRR 1.97, 95% CI 1.53–2.53 (Tables 2 and 3). The incidence rate ratios with confidence intervals for the entire cohort and the two sub-cohorts are presented graphically in Figure 3 and results from each subcohort in Supplementary Table 2s.
 |
Figure 3 Forest plot showing incidence rate ratios for hospital admission, admission days and moderate exacerbations in the 6 months study period for the entire cohort and for each subcohort. For consistency, pooled estimates in this figure are adjusted for center as this adjustment is immanent in the center-specific estimates. P-values for comparison of incidence rate ratios for each outcome: hospital admissions with AECOPD, admission days and moderate exacerbations. The previously published analysis of admissions in Central Denmark7 used a slightly different analysis approach, in which a higher weighting of risk time during the first month was allowed for, whereas correlation between the same patient’s admission counts in different periods was not. This yielded the estimation of a slightly weaker association but a slightly narrower confidence interval that left the association barely significant. However, the discrepancies are small. |
 |
Table 2 Hospital Admissions, Admission days with AECOPD and Moderate Exacerbations in the Telemonitoring and Control Groups |
 |
Table 3 Incidence Rate Ratios for Hospital Admissions, Hospitalization days and Exacerbations Without Hospital Admission in the 6 months Study Period |
Discussion
The pooled analysis in our study showed no reduction in hospital admissions for AECOPD when telemonitoring was added to usual care in this large cohort of patients with COPD from two randomized controlled trials conducted in Denmark with similar standards for COPD care across the country. The study included patients with severe COPD at high risk of exacerbations and the two cohorts were similar regarding age, smoking status, and disease severity. Of course, it must be considered whether the two populations differ to a degree that affects the overall effect of the telemonitoring intervention, but based on the investigators’ clinical judgement, this is unlikely to be the case.
No difference was seen regarding admission days or time to hospitalization with AECOPD, but for moderate exacerbations, our study showed that the number of treated exacerbations was significantly higher in the telemonitoring group, which was also the case for the Capital Region cohort and the Central Denmark cohort in separate analyses.
The telemonitoring intervention was slightly different in the two studies with regards to the frequency and setup, and inclusion in one study was during hospital admission and from outpatient clinics in the other (patients with previous hospitalization for AECOPD or on long-term oxygen therapy). Since the combination of these approaches reflects how telemonitoring is used in clinical practice after its introduction in standard care, we believe that the results of the pooled analysis are highly relevant.
Our findings are consistent regarding no improvement with telemonitoring in the number of hospitalizations, length of stay, and time to hospitalization. No solid evidence exists for telemonitoring as a tool for prevention of hospital admission due to AECOPD by earlier identification and treatment in case of symptom worsening. The mainstay of treatment for exacerbation has been unchanged for decades and does not address the complex nature of exacerbations.16 Furthermore, no objective definition of acute exacerbations in COPD has been implemented in clinical practice, which adds to the complexity of the management of symptom worsening. Recently, a definition and severity classification of exacerbations was presented in the Rome proposal17 with the purpose of better informing clinical care, research, and health service planning. The implementation of objective measures will support clinicians’ choice of therapy and may also help to reduce corticosteroid and antibiotic use, and the possibility of home monitoring may even support this.
The evidence supporting corticosteroids for treatment of AECOPD was summarized in a Cochrane review from 201418 including nine studies with a total of 917 patients in outpatient as well as inpatient settings. The review concluded that treatment with corticosteroids reduced the likelihood of treatment failure, shortened length of stay in hospital inpatients and gave earlier improvement in lung function and symptoms, with an increase in adverse drug effects with corticosteroid treatment. Considering the frequency worldwide of hospitalizations and contacts to GPs for AECOPD, the number of studies in this field is small, and the optimal use of corticosteroids for severe and moderate exacerbations needs more elaboration, in terms of subgroups benefitting from the treatment, optimal length of treatment, and severity of symptom worsening that warrants use of oral corticosteroids. In the recent study by Thebault et al, patients with AECOPD treated in general practice were randomized to prednisolone or placebo. The study included 175 patients, which was only 43% of the planned sample. The study showed a 42% failure rate in the prednisolone group compared with 34.5% in the placebo group with failure defined as new contact to GP or emergency clinic, hospitalization or death within 8 weeks.19 The findings must be interpreted with caution due to the lack of statistical power, but the study provides a signal that must be investigated in additional studies.
Growing evidence supports the use of blood-eosinophil levels to select patients most likely to benefit from corticosteroids for AECOPD20–22 and, just as important, to avoid treatment of patients unlikely to benefit. Furthermore, anti-IL5 treatment seems to be a promising new approach to therapy for at least a subgroup of patients with high biomarker levels, as shown in the recent ABRA-trial.23
The use of antibiotics for treatment of COPD exacerbations was assessed in a Cochrane review24 which was based on relatively few studies considering the common use. For treatment failure, the effects were inconsistent and absent for the outcomes mortality and length of hospital stay.
Guidelines, eg, in the UK, stress that clinicians must weigh up the limited benefits of antibiotics against the risk of antimicrobial resistance when treating patients with acute exacerbations of chronic obstructive pulmonary disease whereas greater benefit with antibiotic treatment is seen in patients with severe exacerbations requiring hospitalization.25 The PACE study conducted in primary care, showed that C-reactive protein-guided prescribing of antibiotics for exacerbations of COPD reduced antibiotic use with no evidence of harm.26 These results support CRP testing to guide antibiotic use, but further studies are needed to establish which patients will benefit from antibiotic therapy.
Closer monitoring will identify symptom variation that may or may not lead to an exacerbation. The finding of the present study, that telemonitoring significantly increased treatment for moderate exacerbations, highlights the need to consider risk of overtreatment. However, the close contact to respiratory healthcare professionals in a telemonitoring set up may ideally provide an opportunity to optimize inhaled therapies, smoking cessation support, referral for pulmonary rehabilitation and management of comorbidities, all of which may support long-term prevention of exacerbations.
We cannot conclude with certainty that the additional treatment is without any benefit for the patients, but given that there is no or, at best, limited effect on hard outcomes, it must be considered whether the extra treatment associated with the use of telemonitoring is acceptable or could be avoided.
Strengths and Limitations
The strengths of the present study are the large dataset; a study population of patients with severe COPD at high risk of exacerbations; two distinct geographical regions, but in similar, publicly funded health care settings. The minor differences in the way the intervention was organized may to some extent be a limitation, but these differences reflect how the national telemonitoring service has been implemented in Denmark. Minor differences were seen in clinical characteristics between the centers; however, from an overall perspective, the two subpopulations represented a fairly homogenous population with severe COPD and high risk of exacerbations. The combined analysis with a total of 503 patients provides more robust estimates and reduces the risk of a type II error due to insufficient power. However, although the incidence rate ratios for admissions and admission days estimated in this relatively large study document no beneficial effect of telemonitoring, we note that the corresponding confidence intervals are quite wide (ie compatible with a potentially clinically relevant risk reduction of up to 38%, respectively 58%, although also with a risk increase of 17%, respectively 23%).
It may also be considered a limitation that the use of different quality of life measures in the Capital Region study and the Central Denmark study, prevented a pooled analysis of these aspects of the telemonitoring intervention.
Conclusion
This pooled analysis of two randomized controlled trials of telemonitoring in COPD does not document an effect on hospitalizations or days in hospital but shows that the telemonitoring group received significantly more frequent treatment for moderate exacerbations, which may imply a risk of overtreatment with possibly serious side effects.
Data Sharing Statement
The data that support the findings of this study are not publicly available. Data sharing requires permission from Danish health authorities.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
Prof. Dr. Charlotte Ulrik reports grants, personal fees from AZ, personal fees from GSK, personal fees from BI, personal fees from TEVA, personal fees from Chiesi, personal fees from Novo Nordisk, grants, personal fees from Sanofi, personal fees from IQVIA, personal fees from Hikma Pharmaceuticals, personal fees from Roche, personal fees from Takeda, personal fees from TFF Pharmaceuticals, personal fees from Orion Pharma, outside the submitted work. The authors have no financial or non-financial competing interests to report.
References
1. Pinnock H, Hanley J, McCloughan L, et al. Effectiveness of telemonitoring integrated into existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: researcher blind, multicentre, randomised controlled trial. BMJ. 2013;347(oct17 3):f6070. doi:10.1136/bmj.f6070
2. Soriano JB, García-Río F, Vázquez-Espinosa E, et al. A multicentre, randomized controlled trial of telehealth for the management of COPD. Respir Med. 2018;144:74–81. doi:10.1016/j.rmed.2018.10.008
3. Walker PP, Pompilio PP, Zanaboni P, et al. Telemonitoring in chronic obstructive pulmonary disease (CHROMED). A randomized clinical trial. Am J Respir Crit Care Med. 2018;198(5):620–628. doi:10.1164/rccm.201712-2404OC
4. Jang S, Kim Y, Cho WK. A systematic review and meta-analysis of telemonitoring interventions on severe COPD exacerbations. Int J Environ Res Public Health. 2021;18(13):6757. doi:10.3390/ijerph18136757
5. Dinesen B, Haesum LK, Soerensen N, et al. Using preventive home monitoring to reduce hospital admission rates and reduce costs: a case study of telehealth among chronic obstructive pulmonary disease patients. J Telemed Telecare. 2012;18(4):221–225. doi:10.1258/jtt.2012.110704
6. Witt Udsen F, Lilholt PH, Hejlesen O, Ehlers L. Cost-effectiveness of telehealthcare to patients with chronic obstructive pulmonary disease: results from the Danish ‘TeleCare North’ cluster-randomised trial. BMJ Open. 2017;7(5):e014616. doi:10.1136/bmjopen-2016-014616
7. Lilholt PH, Witt Udsen F, Ehlers L, Hejlesen OK. Telehealthcare for patients suffering from chronic obstructive pulmonary disease: effects on health-related quality of life: results from the Danish ‘TeleCare North’ cluster-randomised trial. BMJ Open. 2017;7(5):e014587. doi:10.1136/bmjopen-2016-014587
8. Ringbæk T, Green A, Laursen LC, Frausing E, Brøndum E, Ulrik CS. Effect of tele health care on exacerbations and hospital admissions in patients with chronic obstructive pulmonary disease: a randomized clinical trial. Int J Chron Obstruct Pulmon Dis. 2015;10:1801–1808. doi:10.2147/COPD.S85596
9. Andersen FD, Trolle C, Pedersen AR, et al. Effect of telemonitoring on readmissions for acute exacerbation of chronic obstructive pulmonary disease: a randomized clinical trial. J Telemed Telecare. 2024;30(9):1417–1424. doi:10.1177/1357633X221150279
10. Tupper OD, Gregersen TL, Ringbaek T, et al. Effect of tele-health care on quality of life in patients with severe COPD: a randomized clinical trial. Int J Chron Obstruct Pulmon Dis. 2018;13:2657–2662. doi:10.2147/COPD.S164121
11. Køpfli ML, Børgesen S, Jensen MS, Hyldgaard C, Bell C, Andersen FD. Effect of telemonitoring on quality of life for patients with chronic obstructive pulmonary disease-A randomized controlled trial. Chron Respir Dis. 2023;20:14799731231157771. doi:10.1177/14799731231157771
12. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8
13. Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. 2017;357:j1415. doi:10.1136/bmj.j1415
14. Tse G, Emmanuel B, Ariti C, et al. A long-term study of adverse outcomes associated with oral corticosteroid use in COPD. Int J Chron Obstruct Pulmon Dis. 2023;18:2565–2580. doi:10.2147/COPD.S433326
15. Danish Health Data Authority. Strategies and projects, telemedicine. Available from: htpps://sundhedsdatastyrelsen.dk/digitale-loesninger/telemedicin.
16. Mathioudakis AG, Janssens W, Sivapalan P, et al. Acute exacerbations of chronic obstructive pulmonary disease: in search of diagnostic biomarkers and treatable traits. Thorax. 2020;75(6):520–527. doi:10.1136/thoraxjnl-2019-214484
17. Celli BR, Fabbri LM, Aaron SD, et al. An updated definition and severity classification of chronic obstructive pulmonary disease exacerbations: the Rome proposal. Am J Respir Crit Care Med. 2021;204(11):1251–1258. doi:10.1164/rccm.202108-1819PP
18. Walters JA, Tan DJ, White CJ, Gibson PG, Wood-Baker R, Walters EH. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;2014(9):CD001288. doi:10.1002/14651858.CD001288.pub4
19. Thebault JL, Roche N, Abdoul H, Lorenzo A, Similowski T, Ghasarossian C. Efficacy and safety of oral corticosteroids to treat outpatients with acute exacerbations of COPD in primary care: a multicentre pragmatic randomised controlled study. ERJ Open Res. 2023;9(5):00057–2023. doi:10.1183/23120541.00057-2023
20. Ramakrishnan S, Jeffers H, Langford-Wiley B, et al. Blood eosinophil-guided oral prednisolone for COPD exacerbations in primary care in the UK (STARR2): a non-inferiority, multicentre, double-blind, placebo-controlled, randomised controlled trial. Lancet Respir Med. 2024;12(1):67–77. doi:10.1016/S2213-2600(23)00298-9
21. Bafadhel M, McKenna S, Terry S, et al. Blood eosinophils to direct corticosteroid treatment of exacerbations of chronic obstructive pulmonary disease: a randomized placebo-controlled trial. Am J Respir Crit Care Med. 2012;186(1):48–55. doi:10.1164/rccm.201108-1553OC
22. Sivapalan P, Lapperre TS, Janner J, et al. Eosinophil-guided corticosteroid therapy in patients admitted to hospital with COPD exacerbation (CORTICO-COP): a multicentre, randomised, controlled, open-label, non-inferiority trial. Lancet Respir Med. 2019;7(8):699–709. doi:10.1016/S2213-2600(19)30176-6
23. Ramakrishnan S, Russell REK, Mahmood HR, et al. Treating eosinophilic exacerbations of asthma and COPD with benralizumab (ABRA): a double-blind, double-dummy, active placebo-controlled randomised trial. Lancet Respir Med. 2024;13(1):59–68.
24. Vollenweider DJ, Frei A, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2018;10(10):CD010257. doi:10.1002/14651858.CD010257.pub2
25. NICE. Chronic obstructive pulmonary disease (acute exacerbation): antimicrobial prescribing. Available from: https://www.nice.org.uk/guidance/ng114.
26. Butler CC, Gillespie D, White P, et al. C-reactive protein testing to guide antibiotic prescribing for COPD exacerbations. N Engl J Med. 2019;381(2):111–120. doi:10.1056/NEJMoa1803185
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

