Back to Journals » Journal of Pain Research » Volume 18
Effectiveness of Electromagnetic Field Therapy in Mechanical Low Back Pain: A Randomized Controlled Trial
Authors Koura GMR, Elshiwi AMF, Alshahrani MS, Elimy DA, Alshahrani RAN, Alfaya FF, Alshehri SHS, Hadi AA, Alshehri MA, Alnakhli HH, Ahmad F, Ahmad I
Received 2 November 2024
Accepted for publication 25 February 2025
Published 8 March 2025 Volume 2025:18 Pages 1131—1142
DOI https://doi.org/10.2147/JPR.S500698
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Dawood Sayed
Ghada Mohamed Rashad Koura,1 Ahmed Mohamed Fathi Elshiwi,2 Mastour Saeed Alshahrani,1 Doaa Ayoub Elimy,3 Razan Abdurahman Nasser Alshahrani,2 Fareed F Alfaya,4 Shaker Hassan S Alshehri,4 Amal A Hadi,2 Mohammed Abdullah Alshehri,5 Hani Hassan Alnakhli,1 Fuzail Ahmad,6 Irshad Ahmad1
1Program of Physical Therapy, Department of Medical Rehabilitation Sciences, College of Applied Medical Sciences, King Khalid University, Abha, 61421, Saudi Arabia; 2Consultant and Head of Physical Therapy Department, Saudi German Hospital, Aseer, Saudi Arabia; 3Basic Sciences Department, Faculty of Physical Therapy, Cairo University, Cairo, Egypt; 4Department of Orthopedic Surgery, College of Medicine, King Khalid University, Abha, Saudi Arabia; 5Department of Physiotherapy, Abha, International Private Hospital, Abha, Saudi Arabia; 6Respiratory Care Department, College of Applied Sciences, AlMaarefa University, Dirirya, Riyadh, Saudi Arabia
Correspondence: Irshad Ahmad, Email [email protected]
Background: Between half and three quarters of the working-age population in today’s industrialized globe suffers from lower back pain. The presence of a myofascial trigger point—a hyperirritable painful area comprised of a small number of muscle fibers—identifies mechanical back pain sufferers as suffering from myofascial pain syndrome, a chronic pain disorder. This research objectives to determine whether mechanical back pain patients’ pain severity and functional disabilities are influenced by electromagnetic field therapy.
Methods and Subjects: Two groups of thirty patients were randomly assigned. The 15 participants in group A underwent conventional physical therapy (including ultrasound, stretches, and strength training for the back muscles), while the 15 participants in group B received a combination of conventional physical therapy and electromagnetic field therapy. Pre- and post-treatment assessments of pain intensity, functional impairment, and lumbar range of motion (including extension, flexion, and right and left side bending) were examined. The variables of interest that were examined at various testing groups and measuring periods were compared using a 2× 2 mixed design MANOVA.
Results: After treatment, there was a significant difference in all dependent variables between the two groups in terms of between-subject effects (p < 0.05). Group B benefited from a significant decrease in pain, right and left side bending, and function disability, as well as an increase in flexion and extension.
Conclusion: Patients suffering from mechanical back pain can find relief from their discomfort and functional impairment through the use of electromagnetic field therapy, according to the current study’s conclusions.
Keywords: myofascial trigger point, mechanical back pain, conventional physical therapy, electromagnetic field
Introduction
Low back pain (LBP) is a leading cause of disability worldwide, affecting individuals across all age groups and placing a significant socioeconomic burden on society. It is estimated that 50–80% of people will experience LBP at some point in their lives, with working-age adults being the most vulnerable population.1,2 Mechanical low back pain, a subtype of LBP, is typically associated with overuse or repetitive trauma to the spine, intervertebral discs, and surrounding tissues. Common causes include disc herniation, vertebral compression fractures, lumbar spondylosis, spondylolisthesis, and lumbosacral muscular strain.3 This condition is characterized by pain and functional limitations that can severely affect quality of life and productivity.
Electromagnetic field therapy (EMF), a non-invasive and FDA-approved modality, has gained attention for its potential to promote tissue repair and alleviate pain without causing thermal damage. Pulsed electromagnetic fields (PEMF) are widely used to treat conditions such as osteoarthritis, post-operative pain and edema, chronic wounds, and non-union fractures.4,5 The proposed mechanism of EMF therapy involves the stimulation of cellular and molecular processes, including increased microcirculation, modulation of inflammatory pathways, and enhanced cellular repair. This therapy has been shown to improve physical function and reduce pain in various musculoskeletal conditions, making it a promising adjunct to conventional physical therapy.6
Evidence supporting EMF therapy in low back pain management is growing but remains inconsistent. For instance, several studies have demonstrated significant pain relief and improved functional outcomes in patients with non-specific LBP when EMF was combined with standard physiotherapy.7,8 A systematic review by Kull et al (2023) highlighted the safety and efficacy of PEMF therapy as an adjunct for musculoskeletal pain but noted variability in treatment protocols and dosimetry across studies. Similarly, other investigations have reported moderate benefits for pain relief in osteoarthritis and other musculoskeletal disorders, emphasizing the need for standardized treatment parameters.9,10
Despite the emerging evidence, there is a lack of robust clinical studies evaluating the effects of EMF therapy specifically on mechanical low back pain. Moreover, while the general benefits of EMF therapy have been explored, its impact on key outcomes such as pain severity, functional disability, and lumbar range of motion (ROM) in this population remains under-researched. This study aimed to fill this gap by investigating the efficacy of EMF therapy in reducing pain, improving functional ability, and enhancing lumbar ROM in patients with mechanical low back pain. We hypothesized that EMF therapy, when used in conjunction with conventional physical therapy, would result in significant improvements in these outcomes.
Materials and Methods
Study Design
This experiment followed the CONSORT standards by implementing a randomized and double-blind design. Using a pre- and post-test methodology, the research was structured like a randomized clinical trial. The study was approved by the Research Ethics Committee of King Khalid University (HAPO-06-B-001; ECM#2023-2104, Date: 30/05/2023). The study protocol followed by all experiments with human subjects were compliant with the Declaration of Helsinki. Written informed consent was obtained from every single subject, who willingly participated in this study. Subjects were also informed that keeping their privacy rights, subject’s data and pictures may be send for publications study was registered for Clinical Trial Registry (gov ID: NCT06133855; Date: 14/11/2023).
Participants
The sample size for this study was determined using a priori power analysis to ensure adequate statistical power for detecting significant differences between the two groups. A two-tailed test with an alpha level of 0.05 and a power of 80% (1-β = 0.80) was established as the threshold for significance. Based on effect sizes reported in previous studies on interventions for mechanical low back pain, an effect size of 0.8 (Cohen’s d) was assumed, indicating a large effect. Using these parameters, the required sample size was calculated to be 15 participants per group, resulting in a total of 30 participants. To account for potential dropout or loss to follow-up, an additional 20% of participants were included in the recruitment target, increasing the goal to 36 participants. The sample size calculation was conducted using G*Power version 3.1.
The inclusion criteria required participants to be office workers aged 25 to 45 years who had experienced mechanical low back pain for at least three months and exhibited active myofascial trigger points (MTrPs) in the lower back muscles. The age range of 25 to 45 years was specifically chosen to ensure a homogeneous sample and to exclude potential confounding factors such as age-related degenerative changes. To minimize any potential effect of age on the outcomes, participants were evenly distributed across this age range during the randomization process. This distribution was further verified during data analysis to confirm that age did not significantly influence the study results.
Exclusion criteria included pregnancy or nursing, a history of back surgery or vertebral compression fractures, neurological impairments, lower limb signs and symptoms, or any cardiac or pulmonary conditions that could limit physical exertion. To assess heart and lung diseases as part of the exclusion process, a combination of self-reported medical histories and reviews of prior medical records was used. Where required, additional documentation from participants’ primary healthcare providers was obtained to confirm their eligibility. This thorough screening ensured that individuals with contraindications to physical activity, such as cardiopulmonary disorders, were excluded from the study.
The study was conducted over a 3-month period, from 15 November 2023 to 15 February 2024, at the Physical Therapy Clinic of King Khalid University. Patients diagnosed with mechanical low back pain were referred to the clinic, where one of the authors, with over 10 years of clinical experience in musculoskeletal physiotherapy, managed recruitment. A total of 42 patients with back pain were screened, out of which 30 met the inclusion criteria for mechanical low back pain and were enrolled in the study. All study procedures, including pre- and post-assessments as well as the intervention plan, were clearly explained to the participants. Written informed consent was obtained, and participants were informed of their right to withdraw from the study at any point.
Pre-intervention assessments included measurements of pain intensity, functional impairment, and lumbar spinal range of motion. Participants were randomized into two equal groups of 15 each using a lottery method. The control group (Group A) received a conventional physical therapy regimen, which included infrared and ultrasonic treatments as well as stretching and strengthening exercises targeting the back. The experimental group (Group B) received a combination of magnetic field therapy and conventional physical therapy for 12 sessions over four weeks. Post-intervention assessments were conducted in the same manner as the baseline evaluations. Importantly, the therapist conducting these assessments was blinded to the group allocation and intervention details to minimize bias.
Procedure and Outcome Measures Used for Assessment
Pre- and post-treatment assessments were conducted on patients. Listed below are the components of the evaluation processes.
Pain Evaluation: In order to facilitate continuous data processing, the visual analogue scale (VAS) is a 10-centimeter line with zero representing no discomfort and ten representing the worst possible agony. Patients were asked to mark their pain levels on the line according to their perception.9
Functional Impairment Evaluation: The Arabic version of the ODI, which is a valid, relevant, and reliable scale for assessing disability in LBP, was used to assess functional disability (Algarni et al, 2014). Assessing low back functional disability using a self-report questionnaire. Pain levels, social and sexual lives, and daily routines are just a few of the subjects covered in its ten sections. There are six possible choices for each part, ranging from zero to five. Elevated values signify a significant decline in functional capacity.10
Range of Motion Evaluation: The flexibility of the lower back in Flexion & Extension: The modified-modified Schober test is both a popular and easy way to measure lumbar range of motion. Along with these advantages, it includes accurate measurements, is adaptable to any environment, and uses cheap, easily accessible materials. Both the therapist and the patient will find it pleasant, valid, and dependable because there is no fixation required and landmarks are easy to palpate. The posterior superior iliac spine (PSIS) was marked inferiorly at a midline location. Finally, the lumbar spine (superior mark) was marked fifteen centimeters higher than the midline PSIS mark. The therapist adjusted the upper end of the tape to 15 cm and the lower end to zero. The measuring tape was kept firmly against the skin of the patient while they were told to bend forward as much as they could while keeping their knees straight. While patient moving, the measuring tape was placed across the patient’s back. The procedure for testing lumbar extension was identical to that of testing flexion. The therapist next had the patient bend back as far as they could while holding the tape firmly on their skin, with their palms on their buttocks.
When the patients fully extended their backs into a lumbar flexion position, we measured the new distance between the upper and lower skin markings using a tape measure.11
Lateral Bending: Our definition of maximal comfortable lateral flexion is the distance between the tip of the index finger and the floor, based on the research of Ponte et al (1984). The subject was told to bend laterally as far as they could go. The results of a three-times-per-side approach that was used to calculate the range of motion (ROM) for lateral flexion.12
Equipment Used for Medical Treatment
Automated PMT Quattro pro with ASA magnetic field: Manufacturer, model, and serial number (Automatic PMT Quattro pro: 00001543). This magnetotherapy device is known as the ASA magnetic field. On top of that, it includes solenoids and a motorized bed. The device cannot be used without an earth connection and a power source of 230v 10% at 50 or 60 hz. The intensity and dispersion of the produced magnetic field are defined by the solenoid type.
IRR- Infrared Radiation: The usage of infrared heat is widespread in physical therapy department; we have used a 4004/2N model Infrared lamp with 50–60Hz of frequency and 203 w voltage. A model 4004/2N is what it is. It is allowed to use infrared treatments first, before moving on to other types of heat therapy including exercise, myofascial release, traction, stretching, or mobilization.
Therapeutic Ultrasonic Machine: A Model 2745, Phyaction 190 ultrasonic generator, 8 watts, 230 volts, 300 milliamperes, 50–60 hertz was used in the study. It is commonly used to relieve pain and break up adhesions in cases of low back discomfort.
Treatment Procedure
Group A—Control
The sample size for this group was fifteen patients. They had participated in a conventional treatment regimen: For a month, patients taken 12 sessions of infrared radiation therapy, each lasting 20 minutes, with a distance of 60 cm from the lumbar region, alternate days per week in prone position.13 Ultrasonic machine, continuous mode, 1.5 watts per square centimeter is applied continuously for 5 minutes at 1 hertz.13 In a long sitting, gently stretch of hamstrings, calves, and back for 30 seconds.14 Back strengthening exercises (active back extension and bridging).15–17 These exercises were done with three sets of each exercise, with a 6-second hold between sets (Figures 1–4 Fingers to toes exercise, Bridging exercise, Active back extension, and Sit-up exercise).
 |
Figure 1 Fingers to toes. |
 |
Figure 2 Bridging exercise. |
 |
Figure 3 Active back extension. |
 |
Figure 4 Sit-up exercise. |
Group B—Experimental
There were fifteen patients in this group. In addition to the conventional physical therapy treatment program, they also had a 15-minute session of electromagnetic field therapy with a frequency of 10 hz and an intensity of 20 gauss.3 Patients undergo lumbar electromagnetic therapy three times weekly, alternate days, in prone position, 12 sessions in a month while lying face down (Figure 5 Application of magnetic field).
 |
Figure 5 Application of magnetic field. |
Statistical Analysis
All statistical analyses were conducted by using SPSS (Statistical Package for the Social Sciences) Version 23, developed by IBM Corporation, Armonk, New York, United States, windows version. Before the final analysis, we made sure the data followed the normality assumption and did not have any outliers. This examination was conducted in order to set the stage for the parametric calculation of associated measures and the study of difference. All the dependent variables were found to have normal distributions when descriptive analysis was conducted using histograms based on the normal distribution curve. Additionally, at the 0.05 level of significance, Box’s test for homogeneity of covariance did not reveal any significant difference. All the dependent variables were found to have normally distributed data when the Shapiro–Wilk test was used to check for this. All these findings made parametric analysis feasible. To accomplish this, we compared the relevant tested variables across groups and time points using a two-way mixed-design repeated-measures analysis of variance (2×2 MANOVA). We utilized an alpha value of 0.05.
Results
This study involved 30 patients who were randomly divided into two groups. One group was the control group, which included 15 patients with an average age of 37.27 (± 2.52) years and a mean weight of 72.73 (±8.66) kg, mean height of 164.27 (± 8.71) cm, mean duration of disease was 7.53 (± 3.27) months, and mean numbers of session 11.35 (±.83).
Fifteen patients made up the experimental group. Their average age was 36.73 (±2.52) years, weight was 77.4 (± 10.23) kg, height was 162.2 (± 9.73 cm), the average duration of disease was 8.6 (± 2.93) months, and mean numbers of ses-sion11.66 (±.81). In terms of these demographic variables, an unpaired t-test revealed no statistically significant differences between the groups prior to therapy (Table 1).
 |
Table 1 Demographic Data of Patients |
Unpaired t-test was used to detect differences between groups before treatment. There was no significant differences between groups regarding pain severity (t=1.311, p=0.20), functional disability (t=0.797, p= 0.43), lumbar flexion (t= 0.125, p= 0.90), lumbar extension (t= 0.950, p= 0.35), lumbar right bending (t= 0.581, p= 0.56), and lumbar left bending (t= 1.93, p= 0.06) (Table 2).
 |
Table 2 Comparison Between Groups Before Treatment |
After treatment paired t-test was used to examine with in group difference of experimental group for: pain severity, functional disability, lumbar flexion, lumbar extension, lumbar right bending, and lumbar lift bending. The study demonstrated significant within-group differences in the control group following the treatment. Pain severity decreased from 7.66 pre-test to 41.13 post-test, reflecting an 82.4% reduction (t(14)=12.68, p<0.001). Functional disability scores reduced by 39.8%, dropping from 48.73 to 29.33 (t(14)=14.33, p<0.001). Flexion increased by 50%, improving from 3.20 to 4.80 (t(14)=9.99, p<0.001). Similarly, extension improved by 28.1%, increasing from 1.53 to 1.96 (t(14)=10.98, p<0.001). Right side bending showed a significant improvement, decreasing by 74.3%, from 67.80 to 17.40 (t(14)=16.22, p<0.001). Left side bending similarly decreased by 73.3%, from 66.93 to 17.87 (t(14)=19.20, p<0.001). These findings indicate that the intervention significantly improved pain severity, functional disability, and range of motion across all measured outcomes (Table 3).
 |
Table 3 Within Group Difference of Control Group After Treatment |
Paired t-test was used to detect differences between groups after treatment. The study demonstrated significant within-group differences in the experimental group following the treatment. Pain severity increased significantly from 8.05 to 52.4, with a mean difference of 52.4 (t(14)=27.02, p<0.001). Functional disability scores decreased from 50.67 to 35.53, with a mean difference of 35.53 (t(14)=29.94, p<0.001). Flexion improved significantly from 3.23 to 6.1 (t(14)=15.85, p<0.001), and extension increased from 1.36 to 2.83 (t(14)=10.48, p<0.001). Right side bending showed a significant reduction from 68.53 to 24.87 (t(14)=24.20, p<0.001), while left side bending decreased from 69.47 to 25.73 (t(14)=26.04, p<0.001). These findings highlight the substantial improvements in pain, functional disability, and range of motion within the experimental group after treatment (Table 4).
 |
Table 4 Within Group Difference of Experimental Group After Treatment |
Significant between-group differences were observed after the intervention. Pain severity was significantly lower in the experimental group (52.4) compared to the control group (41.13), t(28)=2.981, p=0.006. Functional disability was also significantly reduced in the experimental group (35.53) compared to the control group (29.33), t(28)=2.621, p=0.014. Flexion was higher in the experimental group (6.1) compared to the control group (4.80), t(28)=2.113, p=0.044. Similarly, extension was significantly greater in the experimental group (2.83) compared to the control group (1.96), t(28)=2.674, p=0.012. Right side bending showed a marked improvement in the experimental group (24.87) compared to the control group (17.40), t(28)=5.027, p=0.0001. Left side bending followed a similar trend, with the experimental group (25.73) outperforming the control group (17.87), t(28)=5.797, `p=0.0001. These results demonstrate the superior effectiveness of the intervention in the experimental group compared to the control group across all variables (Table 5).
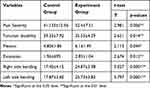 |
Table 5 Post Treatment Inter Group Difference |
Discussion
The aim of this research was to evaluate the effects of electromagnetic field therapy on pain severity, functional impairment, and lumbar range of motion (ROM) in patients with mechanical low back pain. The study hypothesized that electromagnetic field therapy, applied in conjunction with conventional physical therapy, would reduce pain severity, improve functional disability, and enhance lumbar ROM.
Participants in the experimental group received electromagnetic field therapy three times weekly for 12 sessions over four weeks, with a frequency of 10 hz, an intensity of 20 gauss, and a duration of 15 minutes per session. Patients in both the control and experimental groups were diagnosed with mechanical low back pain. The findings of this study partially conflicted with those reported by Morki and Sinaki3 who identified that functional impairments were primarily aggravated by activities such as sitting, twisting, lifting, bending, and standing, all of which contributed to low back pain. However, the results of this study are consistent with the findings of Elshiwi et al,18 which demonstrated that pain and muscle spasm associated with mechanical low back pain led to decreased functional ability and reduced lumbar ROM.
There was a statistically significant decrease in back pain after therapy in the control group, according to an analysis of their pain assessment levels before and after treatment. Traditional physical therapy may have its pain-relieving benefits due to the use of infrared heat, which also reduces muscular spasms. The production of endorphins may also increase sensory responses, which could have an impact on the pain gate system.18 Because it reduces pain, muscular spasms, and impairment, heat can be useful for both acute and chronic low back pain.19
Ultrasound makes the procedure more bearable for individuals by increasing their pain threshold. The use of ultrasound increased the conduction velocity of A-beta nerve fibers, which have a big diameter, and decreased the conduction velocity of A-delta fibers, which have a small diameter and cause pain.20
There is a dramatic increase in tissue temperature, which changes the viscoelastic properties of connective tissue and makes it more pliable.14 Lower back pain (LBP) sufferers experienced less pain and more flexibility after doing hamstring and back stretching exercises, according to research by Khalil et al (1992).21 People with functional disabilities saw significant improvements after receiving the traditional physical therapy program.
To find out if patients’ functional disabilities have improved, O’Sullivan et al (1997) used the Oswestry Disability Questionnaire.22 An increase in myoelectric activity level after strength training is consistent with better neuromuscular system function, as suggested by the capacity to deliberately engage motor neurons and raise their firing rate.23 Johannsen et al (1995) discovered that the best exercises for minimizing functional impairment were those that combined dynamic back and abdominal activity with stretching. One possible solution is to strengthen the multifidus muscle, which tends to weaken as we get older and is a known source of back pain.24,25
This group received the traditional physical therapy program showed a statistically significant increase in lumbar ROM (flexion, extension, right and left side bending) when comparing values taken before and after treatment. Strength and flexibility exercises are an integral part of physical therapy programs. Patients who participated in these programs reported improvements in their motor control skills, pain levels, range of motion in the back (lumbar region), and overall functional ability.26
Researchers Battie et al (1990) reported that people with persistent low back pain (LBP) experienced less pain after receiving flexibility training program.27 The study conducted by Jari et al (2004)17 reported that flexion and extension exercises can enhance flexibility and mobility of the trunk, ultimately leading to a greater range of motion (ROM) in trunk flexion. Patients who engage in more physical activity, have better mental health, and have their pain managed report less impairment and greater mobility.27
The analgesic benefits of PEMF were assessed by measuring the pain levels of the experimental group’s patients before and after treatment. There was a marked decrease in low back pain by the conclusion of the treatment period. This conclusion is shared by Segal et al (1999), Trock et al (1993), Jacobson et al (2001), and Hinman (2002). There are several studies that support our study findings that patients with low back pain (LBP) reported a considerable improvement in their pain levels3,19,28–30 with the use of Pulse Electro-Magnetic Therapy. Physiological mechanisms of relieving pain with the use of a magnetic field may involve presynaptic inhibition or decreased excitability of pain fibers. One or more of these processes may account for how magnetic field therapy could alleviate pain. Studies hypothesized31 that small C-fibers are sensitive to magnetic field effects. Likewise, the authors found that the magnetic field shortly prevented both the calcium-dependent response to the irritant and the sodium-dependent action potential firing.
In a study the chemical mechanism by which a magnetic field applies its influence may include alterations to the structure of ion channels or the neurological membrane. A number of processes, some of which might be indirect, such as a reduction in the activity of channel phosphorylating enzymes, must be operating in order to affect action potentials within the allotted time.29 PEMF has the potential to change the surface receptor sites of hormones, antibodies, and neurotransmitters of many cell types.32
Results from the Oswestry Disability Questionnaire taken by patients in the study group both before and after PEMF therapy showed a statistically significant improvement in functional impairment, suggesting that the treatment was successful in alleviating symptoms. There is less inflammation, better circulation, less discomfort, and improved function when magnetic fields are applied to higher-level structures including connective tissue, muscle, and organs reported by (Jacobson et al, 2001).29 PMF’s anti-inflammatory, hematoma-healing, and water-repositioning properties, microcirculation improvement and edema reduction was some of the other findings.33 Synovitis and inflammation symptoms can be significantly alleviated with the use of a magnetic field.34
Findings of our study, like back improvement in functions and inflammation reduction, we believe that was due to the analgesic and anti-inflammatory effects of the magnetic field. The range of motion (ROM) of the spine, which includes bending to the right and left, as well as flexion and extension, was considerably improved in patients who had magnetic field therapy. These results are in line with those of Hinman (2002),30 who also noted that applying a magnetic field to a musculoskeletal problem reduced inflammation, increased range of motion, and relieved pain. Because it reduces pain and relaxes tight muscles, a magnetic field can help patients with chronic mechanical LBP who suffer from trunk hypo-mobility.35
By easing muscular and joint pain, decreasing swelling and stiffness, and accelerating the repair of injured soft tissues, magnetic fields can enhance mobility and quality of life.36 The study’s analgesic effects, anti-inflammatory effects, and reduced muscle spasm led to improvements in both lumbar mobility and range of motion (ROM).34
In another study, it has been concluded that lower back MPS patients benefit from magnetic field therapy, which increases lumbar range of motion (ROM) due to its analgesic and anti-inflammatory properties and helps reduce pain and functional impairment. So far, magnetic fields have not been associated with any negative side effects.37,38
Limitations
One of the limitations of our study is that the numbers of subject for both the groups were less, that’s why it is difficult to make study finding generality for all the patients suffering from mechanical low back pain.
Conclusion
The findings of this study suggest that electromagnetic field therapy effectively reduces pain severity and functional dysfunction in individuals with mechanical low back pain. This non-invasive therapy is safe, easy to administer, and simple to integrate into treatment regimens, provided proper dosages are maintained to avoid potential overdosing. Additionally, electromagnetic field therapy offers a promising alternative for minimizing the excessive use of anti-inflammatory drugs, thereby reducing their associated risks and side effects. By improving pain management and functional outcomes, this therapy has the potential to enhance the quality of life for patients suffering from mechanical low back pain, making it a valuable addition to conventional treatment approaches.
Abbreviations
MPS, Myofascial Pain Syndrome; ROM, Range of Motion; VAS, Visual Analogue Scale; ODI, Oswestry Disability Index; LBP, Low Back Pain; ATP, Adenosine Triphosphate; MTrPs, Myofascial Trigger Points; FDA, Food and Drug Administration; LTR, Local Twitch Response; PEMFs, Pulse Electromagnetic Fields; PSIS, Posterior Superior Iliac Spine; PMF, Pulse Magnetic Field; SD, Standard Deviation; Rt/Lt, Right/Left.
Data Sharing Statement
The authors intend to share individual deidentified participant data upon reasonable request. This includes demographic information, clinical outcomes, and any other relevant data collected during the study that are necessary to replicate or verify the research findings. Deidentified participant demographic data (eg, age, gender, ethnicity). Clinical outcome measures (eg, laboratory results, survey responses, or intervention outcomes). Study protocol and statistical analysis plan, Informed consent form. The data will be made accessible through a secure, publicly available repository or upon direct request to the corresponding author, Requests for data access can be made via Email to the corresponding author. The data will be made available starting from 6 months after publication and will remain accessible for a minimum of 5 years following publication.
Ethics Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of King Khalid University (HAPO-06-B-001; ECM#2023-2104, Approval Date: 30/05/2023) and enrolled prospectively in ClinicalTrials.gov (gov ID: NCT06133855; Date: 14/11/2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients who participated in this study for publishing their photos.
Acknowldegments
We are very much thankful for King Khalid University, and Hospital for their great technical and financial support. Fuzail Ahmad would like to thank AlMaarefa University for supporting this research.
Funding
The authors extend their appreciation to the Deanship of Research and Graduate Studies at King Khalid University for funding this work through large Research Project, under grant number RGP-2/205/45.
Disclosure
References
1. George SZ, Fritz JM, Silfies SP, et al. Interventions for the management of acute and chronic low back pain: revision. J Orthop Sports Phys Ther. 2021;11:CPG1–CPG60.PMID: 34719942. doi:10.2519/jospt.2021.0304
2. Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;4:619–626.Epub 2019 Mar 8. PMID: 30848349. doi:10.1007/s00296-019-04273-0
3. Elshiwi AM, Mohamed AM, Al Shahrani BA, Al-khathami SA, Koura GM. Influence of electromagnetic field therapy versus acupuncture dry needle in treatment nonspecific low back pain patients: a randomized clinical trial. J Positive School Psychol. 2022;6(11):3014–3031.
4. Harden RN, Remble TA, Houle TT, Long JF, Markov MS, Gallizzi MA. Prospective, randomized, single-blind, sham treatment-controlled study of the safety and efficacy of an electromagnetic field device for the treatment of chronic low back pain: a pilot study. Pain Pract. 2007;7(3):248–255. doi:10.1111/j.1533-2500.2007.00145.x
5. Paolucci T, Pezzi L, Centra AM, Giannandrea N, Bellomo RG, Saggini R. Electromagnetic field therapy: a rehabilitative perspective in the management of musculoskeletal pain - a systematic review. J Pain Res. 2020;13:1385–1400. doi:10.2147/JPR.S231778
6. Krath A, Klüter T, Stukenberg M, et al. Electromagnetic transduction therapy in non-specific low back pain: a prospective randomised controlled trial. J Orthopaedics. 2017;14(3):410–415. doi:10.1016/j.jor.2017.06.016
7. Elshiwi AM, Hamada HA, Mosaad D, Ragab IMA, Koura GM, Alrawaili SM. Effect of pulsed electromagnetic field on nonspecific low back pain patients: a randomized controlled trial. Braz J Physical Ther. 2019;23(3):244–249. doi:10.1016/j.bjpt.2018.08.004
8. Kull P, Keilani M, Remer F, Crevenna R. Efficacy of pulsed electromagnetic field therapy on pain and physical function in patients with non-specific low back pain: a systematic review. Wirksamkeit von gepulster Magnetfeldtherapie bei Patienten mit unspezifischen Rückenschmerzen – eine systematische Literaturübersicht. Wiener medizinische Wochenschrift. 2023. doi:10.1007/s10354-023-01025-5
9. Li S, Yu B, Zhou D, He C, Zhuo Q, Hulme JM. Electromagnetic fields for treating osteoarthritis. Cochrane Database Syst Rev. 2013;12:CD003523. doi:10.1002/14651858.CD003523.pub2
10. Will JS, Bury DC, Miller JA. Mechanical Low Back Pain. Am Fam Physician. 2018;98(7):421–428. PMID: 30252425.
11. Gaynor JS, Hagberg S, Gurfein BT. Veterinary applications of pulsed electromagnetic field therapy. Res Vet Sci. 2018;119:1–8.Epub 2018 May 7. PMID: 29775839. doi:10.1016/j.rvsc.2018.05.005
12. Mellin GP. Accuracy of measuring lateral flexion of the spine with a tape. Clin Biomech. 1986;1(2):85–89. doi:10.1016/0268-0033(86)90081-1
13. Brockow T, Wagner A, Franke A, Offenbächer M, Resch KL. A randomized controlled trial on the effectiveness of mild water-filtered near infrared whole-body hyperthermia as an adjunct to a standard multimodal rehabilitation in the treatment of fibromyalgia. Clin J Pain. 2007;(23):67–75. doi:10.1097/AJP.0b013e31802b4f80
14. Barian V, Ashikage T, Bradan CF, Nancy JZ. The effect of ultrasound and stretch on knee ligament Extensibility. JOSPT. 2000;30(6):341–347. doi:10.2519/jospt.2000.30.6.341
15. El Naggar IM, Nardin M, Sheikhzaden A, Parnianpour M, Kahanovitra N. Effects of spinal flexion and extension exercises on low back pain and spinal mobility in chronic mechanical low back pain patients. Spine. 1991;16:967–972. doi:10.1097/00007632-199108000-00018
16. Elshiwi AM, Alrawaili SM, Asiri RM, Alasmri SA, Koura GM. Effect of myofascial release on spinal adjustment in treatment of postural scoliosis: a randomized controlled clinical trial. Fizjoterapia Polska. 2022;22(3):156–163.
17. Jari PA, Taru V, Markkuk, Ölavi A. Activation at lumbar paraspinal and abdominal muscles during therapeutic exercises in chronic low back pain patients. Arch of Phy Med and Rehab. 2004;85(5):823.
18. Morki B, Sinaki M. Painful disorders of the spine and back pain syndromes. In: editor. Sianki M: Basic Clinical Rehabilitation Medicine. St. Louis: Mobsy- yearbook; 1993:489–502.
19. Trock D, Bollet A, Duer R, Fielding L, Miner W, Markell R. A double-blind trial of the clinical effects of pulsed electromagnetic fields in osteoarthrosis. J Rheumatol. 1993;20(3):456–460.
20. Draper D, Schulthies S, Sorrito P, Hautala A. Temperature changes in deep muscles of humans during ice and ultrasound study. JOSPT. 1995;21:151–157. doi:10.2519/jospt.1995.21.3.153
21. Khalil TM, Sfour S A, Martiner L, Maly S, Rosomff H, Rosomoff HL. Stretching in the rehabilitation of low back pain patients. Spine. 1992;17(3):311–322. doi:10.1097/00007632-199203000-00012
22. O’Sullivan PB, Mampphyty D, Tweny CT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiological diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22(24):2959–2967. doi:10.1097/00007632-199712150-00020
23. Nadler SF, Steiner DJ, Detty SR, et al. Over height use of continuous low level heat wrap therapy for relief of low back pain. Arch Phys Med Rehabil. 2003;84(3):335–342. doi:10.1053/apmr.2003.50103
24. Johannsen F, Remvig L, Kryger P, Back P, Warming S. Exercises for chronic low back pain: a clinical trial. JOSPT. 1995;22(2):52–59. doi:10.2519/jospt.1995.22.2.52
25. Hides JA, Stroke MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/sub acute low back pain. Spine. 1994;19(2):165–172. doi:10.1097/00007632-199401001-00009
26. Magnusson ML, Bishop JB, Hasselquist L, Spratt K, Fond Pope MH, Pope MH. Range of motion and motion pattern in patients with low back pain before and after rehabilitation. Spine. 1998;23(23):2631–2639. doi:10.1097/00007632-199812010-00019
27. Battie MC, Biogs SJ, Fisher LD, Spengler DM, Hansson TH. The role of flexibility in back pain complaints with in industry. A prospective study. Spine. 1990;15(8):768–774. doi:10.1097/00007632-199008000-00006
28. Segal NH, Fuchs J, H HR, Mclean M. Efficacy of static magnetic device against knee pain associated with inflammatory arthritis. J Clinical Rheumatol. 1999;5:302–304. doi:10.1097/00124743-199910000-00016
29. Jacobson J, Gorman R, Amanasbin Y, W SB, Clayton L. Low amplitude extremely low frequency magnetic field for the treatment of osteoarthritic knee, a double blind clinical study.Altern Ther Health Med. 2001;7(5):54–69.
30. Hinman M-R, Ford J, Heyl H. “Effects of Static magnets on chronic Knee Pain and Physical Function” a double-blind study. Alter-Ther-Health-Med. 2002;8(4):50–55.
31. Adey WR. Physiological signaling across cell membranes and cooperative influences of extremely low frequency electromagnetic fields. In: Frohlich H, editor. Biological Coherence and Response to External Stimuli. New york, NY: Springer-Verlag; 1989: 148–170.
32. Holcomb RR, Parker RA, Harrison MS. Biomagentics in the treatment of human pain-past, present, future. Environ Med. 1991;8:24–30.
33. Bassett CAL, Mitchell SN, Gaston SR. Pulsing electromagnetic field treatment in ununited fractures and failed arthrodeses. J Am Med Assoc. 1982;247:623. doi:10.1001/jama.1982.03320300027017
34. Winberger A, Nyska A, Giler S. Treatment of experimental inflammatory synovitis with continuous magnetic field. Ist J Med Sci. 1996;32:1197–1201.
35. Rubin CT, Danahue HJ, Rubin JE, Mc Leod KT. Optimization of electric field parameters for the control of bone remodeling: Exploitation of an indigenous mechanism for the prevention of osteopenia. J Bone Miner Res. 1993;8:573–581. doi:10.1002/jbmr.5650081327
36. Sullivan MS, Saraf LD, Riddle DL. The relationship lumbar flexion to disability in patents with low back pain. Phys Ther. 2000;80(3):240–250. doi:10.1093/ptj/80.3.240
37. Weintraub MI. Magnetic Fields, Environmental Health Criteria. Geneva: World Health Organization; 1999.
38. Van Nguen J, Marks R. Pulsed electromagnetic fields for treating osteoarthritis. Physiotherapy. 2002;88(8):458–470. doi:10.1016/S0031-9406(05)60848-6
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

