Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
Effects of Acupuncture Combined with Conventional Rehabilitation Training for Patients with Post-Stroke Dysphagia: A Randomized Controlled Trial
Authors Xu F, Zhang Y, Su X, Dai F , Ye Y, Ling M, Hu P, Cheng H
Received 7 March 2025
Accepted for publication 26 May 2025
Published 2 June 2025 Volume 2025:18 Pages 3139—3152
DOI https://doi.org/10.2147/JMDH.S526827
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Fangyuan Xu,1,* Yiting Zhang,2,* Xingxing Su,2 Fan Dai,1 Yu Ye,3 Meijuan Ling,3 Peijia Hu,4 Hongliang Cheng2
1The First Clinical Medical School, Anhui University of Chinese Medicine, Hefei, 230031, People’s Republic of China; 2Department of Neurology, The Second Affiliated Hospital of Anhui University of Chinese Medicine, Hefei, 230061, People’s Republic of China; 3The Second Clinical Medical School, Anhui University of Chinese Medicine, Hefei, 230031, People’s Republic of China; 4Department of Endocrinology, The Second Affiliated Hospital of Anhui University of Chinese Medicine, Hefei, 230061, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongliang Cheng, Department of Neurology, The Second Affiliated Hospital of Anhui University of Chinese Medicine, No. 300 Shouchun Road, Luyang District, Hefei, Anhui, 230061, People’s Republic of China, Email [email protected] Peijia Hu, Department of Endocrinology, The Second Affiliated Hospital of Anhui University of Chinese Medicine, No. 300 Shouchun Road, Luyang District, Hefei, Anhui, 230061, People’s Republic of China, Email [email protected]
Objective: Stroke is a significant global public health challenge. Evidence suggests that acupuncture contributes to the treatment and rehabilitation of post-stroke dysphagia (PSD), effectively improving swallowing function and enhancing patients’ quality of life. This study aimed to examine the effects of acupuncture combined with conventional rehabilitation training (CRT) on swallowing function, neurotransmitter levels, nutritional status, and swallowing-related quality of life in patients with PSD.
Methods: Following screening, 90 patients with PSD were randomly assigned to either the intervention group (receiving acupuncture combined with CRT) or the control group (receiving CRT only). Both groups underwent treatment six times per week for four weeks. Primary outcome measures included the standardized swallowing assessment (SSA), the modified Mann assessment of swallowing ability (MMASA), the water swallowing test (WST), and 5-hydroxytryptamine (5-HT) levels. Secondary outcomes assessed swallowing-related quality of life and nutritional indicators.
Results: Compared with baseline data, both groups showed improvements after 2 and 4 weeks of treatment, with reductions in SSA scores and increases in MMASA, hemoglobin (HB), albumin (ALB), serum total protein (STP), swallowing quality of life questionnaire (SWAL-QoL) scores, and WST performance. And the intervention group exhibited significantly greater improvements than the control group at the fourth week. Notably, the 5-HT levels in the intervention group were significantly higher than those in the control group after 4 weeks (362.44± 88.63 vs 310.16± 86.79, P = 0.006).
Conclusion: A 4-week course of acupuncture combined with CRT demonstrated significant benefits in enhancing swallowing function, neurotransmitter levels, nutritional status, and quality of life in patients with PSD.
Keywords: acupuncture, rehabilitation training, post-stroke dysphagia, clinical trial, swallowing function
Introduction
Stroke is a major cause of mortality and disability, posing a significant public health threat.1 Swallowing is a fundamental physiological activity involving the coordinated action of multiple muscle groups and nerves to transport food or liquids from the mouth to the stomach.2 Dysphagia, a common complication following stroke, manifests as impaired swallowing function due to motor neuron damage and dysfunction of the oral and pharyngeal muscles.3 Owing to variations in diagnostic methods and stroke locations, the prevalence of post-stroke dysphagia (PSD) ranges from 37% to 78%.4,5 While spontaneous recovery or improvement in PSD may occur within the first few weeks post-stroke, research indicates that 74.5% of PSD patients experience persistent swallowing dysfunction at discharge, and 50.9% continue to suffer from dysphagia one month after stroke.5 PSD can lead to complications such as aspiration pneumonia, malnutrition, and dehydration, which can prolong the rehabilitation process, increase healthcare costs, and adversely affect patient prognosis and quality of life. Therefore, proactive interventions are essential to prevent further progression of PSD.
Guidelines issued by the European Stroke Organization and the European Society for Dysphagia in 2021 suggest that acupuncture may aid in restoring swallowing function in patients with PSD.6 Evidence indicates that acupuncture significantly contributes to the treatment and rehabilitation of PSD, improving swallowing function and enhancing patients’ quality of life.7,8 Although the mechanism by which acupuncture benefits PSD remains complex and requires further elucidation, swallowing function involves the coordinated activity of multiple brain regions. The therapeutic effects of acupuncture on PSD may be attributed to its modulatory effects on both central and peripheral neural pathways involved in swallowing. Specifically, acupuncture has been reported to activate the cortical swallowing centers, subcortical structures, and brainstem nuclei, as well as to stimulate peripheral nerves and the specific muscle groups responsible for swallowing function.9,10 Electroacupuncture has been shown to increase local blood perfusion and enhance neuronal activity in the primary sensory cortex.11 Research suggests that the motor cortex-parabrachial nuclei-nucleus tractus solitarii (NTS) neural circuit plays a role in regulating swallowing. Electroacupuncture at the Lianquan (RN 23) acupoint has been found to modulate this circuit, aiding in PSD recovery.12 Additionally, acupuncture may stimulate the swallowing-related muscle groups and the peripheral terminals of the glossopharyngeal nerve, thereby facilitating the recovery of the swallowing reflex arc. It manifested as increased hyoid bone displacement, shortened pharyngeal transit time, and overall improvement in dysphagia symptoms.13 Rehabilitation training supports swallowing recovery by promoting neuroplasticity.14 The neural networks involved in swallowing can be activated through frequent exercises or external stimulation, which may help enhance the activity of intact neurons and strengthen the connectivity and efficiency of information transmission.15 Acupuncture combined with conventional rehabilitation training (CRT) exerts a synergistic effect in the treatment of PSD. A meta-analysis has demonstrated that acupuncture combined with swallowing training yields superior outcomes compared to swallowing training alone.16 Both combined therapy and rehabilitation training alone have been shown to increase the mean amplitude of electromyographic activity in the submental and sublingual muscle groups, shorten average swallowing duration, and improve patients’ quality of life. Nevertheless, the combined approach has demonstrated significantly greater therapeutic efficacy.17
Neurotransmitters play a critical role in mediating signal transmission between neurons and are essential for the recovery process in PSD patients.15 5-Hydroxytryptamine (5-HT), a monoamine neurotransmitter, is involved in the complex sensorimotor circuits that regulate the swallowing process.18 The brainstem motor nuclei that innervate the swallowing muscles receive serotonergic input from the NTS and other brain regions, thereby facilitating the coordination of swallowing movements.19 Studies have shown that 5-HT deficiency, compared with control conditions, can lead to reduced licking behavior during the oral phase and impaired swallowing speed during the pharyngeal phase.20 Additionally, other research has emphasized the excitatory role of 5-HT in both reflexive and automatic swallowing.21 Therefore, this study uses a combined intervention of acupuncture and CRT to evaluate its effect on improving swallowing function, 5-HT levels, nutritional status, and quality of life in PSD patients.
Materials and Methods
Study Design
Between January 2022 and April 2024, recruitment was conducted through posters and online announcements in the neurology department at the Second Affiliated Hospital of Anhui University of Chinese Medicine. The research protocol received approval from the hospital’s ethics review committee (2021-zj-40) and was registered in the Chinese Clinical Trial Registry (ChiCTR2100052028). All participants provided written informed consent.
Participants
Stroke diagnosis was based on the 2018 Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke in China and Diagnostic Points for Various Cerebrovascular Diseases, utilizing CT, MRI, and related examinations. Swallowing disorders were defined according to the 2017 Chinese Expert Consensus on the Assessment and Treatment of Dysphagia, with symptoms including difficulty swallowing, coughing during swallowing, prolonged retention of food or saliva in the mouth, or outflow from the nasal cavity or mouth, as well as unclear articulation and hoarseness.
Inclusion criteria were as follows: (1) meeting the above diagnostic criteria; (2) stable vital signs after conventional treatment and a disease course of less than 3 months; (3) clinical manifestations of dysphagia, such as coughing while eating or drinking; and (4) consent to participate in the study and signing of the informed consent form. Exclusion criteria included: (1) large-area cerebral infarction or severe cerebral hemorrhage; (2) true bulbar paralysis; (3) severe cognitive impairment; (4) severe multiple organ dysfunction syndrome; and (5) inability to complete the prescribed course of acupuncture and rehabilitation treatment.
Sample Size
Sample size calculation was performed using PASS software. Preliminary clinical observations indicated an effective rate of 90% in the treatment group and 65% in the control group. With a power (1-β) of 0.8 and an alpha level (α) of 0.05, PASS analysis determined that 40 patients would be required in each group. Accounting for a potential 10% dropout rate, the final sample size was adjusted to 90 patients.
Randomization and Grouping
A total of 90 patients were enrolled in this study and randomly assigned in a 1:1 ratio to either the intervention group (n = 45) or the control group (n = 45). The randomization sequence was generated using SPSS 26.0. After eligibility screening, each patient was assigned a unique random number based on the sequence. The corresponding treatment allocations were placed in sequentially numbered, opaque, sealed envelopes prepared by an independent research assistant not involved in patient enrollment or outcome assessment, thereby ensuring allocation concealment. Experienced clinical operators opened the envelopes in sequence and administered the assigned treatments accordingly. To minimize measurement bias, outcome assessors were blinded to the group allocation throughout the study.
Intervention Protocols
The control group received CRT, which consisted of the following four components: (1) Cold stimulation training: Cold cotton swabs are used to stimulate the throat and base of the tongue, with patients instructed to swallow gently; (2) Tongue Movement Exercises: Patients perform horizontal, backward, and lateral tongue movements, using a spoon or tongue depressor to provide resistance for these exercises; (3) Shaker Exercise: Patients lie flat on a bed, lift their head as high as possible without raising their shoulders off the surface, and look at their feet. This position is held for 1 minute, followed by a 1-minute rest after the head returns to its original position; (4) Mendelsohn Maneuver Training: For patients able to lift their throat, they are instructed to press their tongue against the hard palate, hold their breath for 2–3 seconds while swallowing, and place their index and middle fingers on the thyroid and cricoid cartilages to feel the upward movement of the throat. For patients unable to lift their throat, the operator assists by pushing the throat upward to facilitate swallowing. Rehabilitation training was conducted for 40 minutes per session, six consecutive days per week, with Sunday designated as a rest day. Treatment effectiveness is evaluated after 2 and 4 weeks.
The intervention group received acupuncture treatment in addition to CRT. Acupoint selection was based on established principles derived from previous data mining analyses22,23 and clinical practice. The acupoints applied included Fengfu (DU 16), Lianquan (RN 23), Tiantu (RN 22), Fengchi (GB 20), Wangu (GB 12), and Yifeng (SJ 17). The 0.3 mm*40 mm acupuncture needles were inserted 30 mm at the GB 20, GB 12, DU 16, and SJ 17 acupoints, directed toward the posterior pharynx. For the RN 23 acupoint, the needle was inserted 15–20 mm toward the root of the tongue. At the RN 22 acupoint, a 0.3 mm *50 mm needle was inserted directly to a depth of 5 mm, then angled downward and gently twisted to a depth of 40 mm along the posterior edge of the sternal manubrium. De qi sensations, characterized by soreness, numbness, distension, or heaviness, were initially elicited through 30 seconds of twirling manipulation. To sustain the de qi sensation, manual twirling was repeated every 10 minutes during the 30-minute needle retention period. Each acupuncture session lasted 30 minutes and was administered six consecutive days per week. Treatment effectiveness was assessed after 2 and 4 weeks.
Outcomes
Primary Outcomes
(1) Standardized swallowing assessment (SSA)24,25
Changes in swallowing function (SSA) were evaluated at three intervals: before treatment and at 2 and 4 weeks post-treatment. The assessment followed a three-step protocol. In the first step, a clinical examination was conducted to evaluate parameters including consciousness, head and trunk control, breathing, lip closure, soft palate movement, laryngeal function, pharyngeal reflex, and spontaneous cough, with a score range of 8 to 23 points. In the second step, patients were instructed to swallow 5 mL of water three times, observing responses such as throat movement, repeated swallowing, wheezing during swallowing, and post-swallowing laryngeal function, with scores ranging from 5 to 11 points. If two or more of the three swallowing attempts appeared normal, the patient proceeded to the third step. In the third step, patients need to drink 60 mL of water to observe whether they could complete the task without complications, including coughing, choking, voice quality changes, or aspiration. Scores for this step range from 5 to 12 points. The total SSA score ranging from 18 to 46 reflects swallowing function, with higher scores indicating poorer function.
(2) Water swallowing test (WST)26,27
The patient sits upright and drinks 30 mL of warm water, while the time taken to finish and any instances of coughing during the process are observed. The grading criteria are as follows: Grade I: The patient swallows the water smoothly in a single attempt. Grade II: The patient swallows the water in two attempts without choking or coughing. Grade III: The patient swallows the water in a single attempt but experiences choking or coughing. Grade IV: The patient requires more than two attempts to swallow with occurrences of choking or coughing. Grade V: The patient coughs frequently and is unable to complete the swallowing process.
(3) Modified Mann assessment of swallowing ability (MMASA)28
MMASA was used to assess swallowing function. This assessment consists of 12 key items, including evaluations of articulation disorders, tongue muscle movement, pharyngeal reflex, cough reflex, and soft palate function. The MMASA provides a total score out of 100 points, with higher scores indicating better swallowing function.
(4) Neurotransmitter: 5-HT level
Venous blood samples (5 mL) were collected from fasting patients both before treatment and four weeks post-treatment. The samples were centrifuged at 3000 rpm for 10 minutes to isolate the serum, which was then analyzed for 5-HT levels using enzyme-linked immunosorbent assay (ELISA) kits.
Secondary Outcomes
(1) Swallowing quality of life questionnaire (SWAL-QoL)29
The scale comprises 44 items across 11 dimensions, including appetite, food selection, meal duration, symptom frequency, psychological burden, fear, communication ability, mental health, fatigue, sleep, and social interaction. It provides a comprehensive assessment of quality of life for patients with swallowing disorders. Each item is rated on a 5-point scale, from 1 (poor) to 5 (good). Patients self-assess their condition, with lower scores indicating a more severe swallowing disorder and reduced quality of life.
(2) Nutritional indicators
Hemoglobin (Hb), albumin (ALB), and serum total protein (STP) levels were measured before and after treatment. Blood samples were collected from fasting patients, centrifuged to separate the serum, and then analyzed using a fully automated biochemical analyzer to determine Hb, ALB, and STP levels.
Statistical Analysis
Statistical analyses were performed using SPSS version 26. Quantitative data following a normal distribution are presented as mean ± standard deviation (SD). Intragroup comparisons were conducted using the paired sample t-test, while intergroup comparisons employed the independent sample t-test. For non-normally distributed data, expressed as median and interquartile range [M (P25, P75)], the Mann-Whitney U-test was applied. Categorical data are reported as frequencies or percentages and analyzed using the chi-square test. Ranked data were assessed with the Wilcoxon rank sum test. Statistical significance was set at P < 0.05.
Results
Baseline Characteristics
A total of 122 patients were assessed for eligibility, of whom 13 declined participation, 16 did not meet inclusion criteria, and 3 presented with severe comorbidities. Consequently, 90 patients with PSD were enrolled and randomly assigned to two groups (n = 45 per group). A detailed flowchart of the study design is provided in Figure 1. Table 1 presents the demographic characteristics, history of stroke-related conditions, and stroke type distribution of the participants. The mean age of the intervention group was 61.71 ± 5.91 years, and that of the control group was 60.02 ± 6.76 years. No statistically significant differences were observed between the two groups in terms of age, sex, BMI, smoking status, alcohol use, medical history, or stroke type (all P > 0.05).
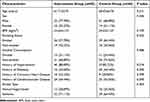 |
Table 1 Baseline Characteristics of Included Participants |
Primary Outcomes
The SSA and MMASA indicators were used to assess the improvement in PSD patients after 2 and 4 weeks of treatment (Figure 2A and B). Prior to treatment, no significant differences were observed between the two groups in SSA and MMASA scores (P = 0.137 and P = 0.292, respectively). Following treatment, the SSA scores in the intervention group significantly decreased at the second and fourth weeks compared to the control group, indicating a superior effect of acupuncture combined with CRT in enhancing swallowing ability. In addition, both groups showed decreased SSA scores at weeks 2 and 4 relative to baseline (Table 2). For the MMASA score, the intervention group’s scores increased from baseline (68.09 ± 5.41) to 2 weeks post-treatment (73.60 ± 4.84) and further at 4 weeks (76.22 ± 4.67), demonstrating that acupuncture combined with CRT could improve MMASA scores at weeks 2 and 4. Notably, the score increase was faster in the second week and then gradually slowed by the fourth week. Compared to the control group, the intervention group showed statistically significant differences in MMASA scores at both week 2 and 4 (P = 0.024 and P = 0.009, respectively).
 |
Table 2 Comparison of SSA, MMASA, and SWAL-QoL Before and After Treatment in Two Groups |
Table 3 and Figure 3 illustrate WST changes at baseline, week 2, and week 4 in both groups. WST results improved significantly in both groups by week 2, with further improvements by week 4. At week 4, the intervention group showed a significant improvement in WST compared to the control group (P = 0.02), whereas no significant difference was observed at week 2 (P = 0.114). After 4 weeks of acupuncture combined with CRT, 26 out of 45 patients were graded as level I or II, indicating notable recovery in swallowing function. Table 4 and Figure 4 indicate that 5-HT levels increased significantly in both groups after 4 weeks of treatment, with a more substantial increase observed in the acupuncture plus CRT group than in the CRT group (P = 0.006).
 |
Table 3 Comparison of WST Before and After Treatment in Two Groups |
 |
Table 4 Comparison of 5-HT Levels Before and After Treatment in Two Groups |
 |
Figure 3 The visualized diagram of WST before and after treatment in two groups. Abbreviation: WST, water swallowing test. |
 |
Figure 4 The bar chart of 5-HT levels before and after treatment in two groups. *P<0.05 vs Baseline, #P<0.05 vs Control group. Abbreviation: 5-HT, 5-hydroxytryptamine. |
Secondary Outcomes
Quality of life and nutritional status were assessed as secondary outcomes in this study. As shown in Table 2 and Figure 2C, dysphagia-related quality of life significantly improved in both groups after 2 and 4 weeks of treatment, with acupuncture combined with CRT demonstrating a greater effect on enhancing quality of life. Table 5 and Figure 2D–F illustrate changes in nutritional indicators (Hb, ALB, and STP) for both groups. When compared with baseline data, Hb, ALB, and STP levels increased significantly in each group at weeks 2 and 4. At week 4, statistically significant differences were observed between two groups in Hb (135.91 ± 13.14 vs 129.96 ± 11.36, P = 0.024), ALB (42.56 ± 3.69 vs 40.64 ± 2.50, P = 0.005), and STP (69.61 ± 4.33 vs 67.59 ± 4.12, P = 0.026) levels.
 |
Table 5 Comparison of Hb, ALB, and STP Before and After Treatment in Two Groups |
Adverse Events
No serious adverse events were observed in either group. Two patients reported mild pain at the acupuncture site, which resolved spontaneously, and two patients developed hematomas that resolved with compression.
Discussion
This study investigates the effects of acupuncture combined with CRT on PSD across four dimensions: swallowing function, neurotransmitter levels, nutritional status, and quality of life. SSA and WST are widely used screening tools for dysphagia, and MMASA offers further evaluation of swallowing function changes. Our findings reveal that acupuncture combined with CRT significantly improved SSA and MMASA scores at weeks 2 and 4 compared to CRT alone. Additionally, after four weeks of treatment, acupuncture demonstrated a cumulative effect, significantly enhancing WST outcomes. Cerebral ischemia can lead to neuronal membrane depolarization and synaptosomal mitochondrial dysfunction, resulting in abnormal neurotransmitter release.30,31 5-HT, a key neurotransmitter in swallowing regulation, may facilitate swallowing through an excitatory neuronal network.21,32 A clinical study reported that acupuncture treatment enhanced blood 5-HT levels compared to rehabilitation training alone, as measured by high-performance liquid chromatography.33 The 5-HT1A receptors are densely distributed in the NTS and play a critical role in regulating the medullary reflex pathways involved in swallowing.34,35 Animal studies have shown that electroacupuncture at the Fengfu (DU 16) and Lianquan (RN 23) acupoints significantly increases the expression of 5-HT1A.36 Furthermore, our clinical study demonstrated that after four weeks of acupuncture combined with rehabilitation training, 5-HT levels in PSD patients increased significantly, potentially contributing to improved swallowing function.
Patients with PSD are at high risk for malnutrition due to inadequate intake of fluids and food.37 The prevalence of malnutrition following acute stroke varies widely, from 6.1% to 62%, depending on the assessment methods, evaluation timing, and patient characteristics.37–39 Malnutrition may be present at hospital admission or develop as the disease progresses, increasing mortality risk and negatively impacting patient prognosis.39–41 This study therefore examined the potential benefits of combining acupuncture with CRT on nutritional indicators. Previous research has associated low Hb levels with poor functional recovery and difficulty swallowing in stroke patients undergoing rehabilitation.42 ALB and STP are commonly used to monitor nutritional status. Our results showed that acupuncture combined with CRT led to increased Hb, ALB, and STP levels, particularly after 4 weeks of treatment. Additionally, dysphagia introduces considerable challenges and can severely impact quality of life. SWAL-QoL scores in two groups improved significantly at weeks 2 and 4 compared to baseline, with greater improvements observed in the group receiving acupuncture combined with CRT compared to CRT alone.
Swallowing rehabilitation exercises play a key role in restoring swallowing function and improving prognosis in patients with dysphagia.43,44 Research has shown that a sensorimotor interaction exists between oral sensory input and pharyngeal motor pathways in cortical areas, with cold oral stimulation significantly enhancing pharyngeal cortical excitability.45 The Shaker exercise, or head lift exercise, strengthens the digastric, genioglossus, and mandibular hyoid muscles, thereby increasing the opening width of the upper esophageal sphincter (UES).46,47 Evidence indicates that the Shaker exercise effectively enhances hyoid movement and reduces aspiration risk.48 The Mendelsohn maneuver improves the coordination of anterior and upper hyoid movement and optimizes the relationship between the average width of the UES opening and the hyoid maximum elevation (HME). Furthermore, as HME increases, both the penetration-aspiration scale and the dysphagia outcome and severity scale show marked improvement.49
The 2016 Guidelines for Adult Stroke Rehabilitation and Recovery recommend acupuncture as a beneficial alternative approach for treating dysphagia.50 Studies have shown that acupuncture, when combined with rehabilitation training, can significantly enhance patients’ swallowing function, daily living activities, and quality of life,16 findings that align with our study results. Specifically, nape acupuncture combined with rehabilitation has been found to improve brain hemodynamics and regulate neurotrophin levels. In selecting acupoints, Lianquan (RN 23) emerged as a commonly used acupoint based on data mining. Key acupoints such as Fengchi (GB 20), Lianquan (RN 23), and Wangu (GB 12) are in close proximity to the hypoglossal, vagus, and glossopharyngeal nerves. Stimulating these acupoints enhances sensory nerve input, promoting nerve function recovery. Additionally, acupuncture at Fengchi (GB 20), Fengfu (DU 16), and Yifeng (SJ 17) has been shown to enhance cerebral blood flow, which aids in regulating swallowing function.51 Deep needling at the Tiantu (RN 22) acupoint directly affects the pharyngeal muscles, facilitating the formation of the swallowing neural pathway and accelerating the recovery of swallowing muscle strength.52
Our study demonstrated the superiority of acupuncture combined with CRT over CRT alone in the recovery of PSD. Nevertheless, the underlying mechanisms of acupuncture’s effects on PSD remain to be clarified. Several factors may contribute to its therapeutic effects. First, the initiation of voluntary swallowing requires normal cortical function.53,54 Acupuncture stimulation may transmit afferent signals to the cerebral cortex or medulla oblongata, thereby promoting cortical activation, enhancing regional brain function, and facilitating neuroplasticity. These effects may help initiate and complete the swallowing process more effectively, ultimately improving swallowing function in patients with PSD.55 Second, acupuncture promotes the release of peripheral neurotransmitters, such as 5-HT, which modulate the excitability of primary afferent sensory neurons.36,56 It also increases local blood supply and improves cerebral circulation. Finally, acupuncture helps activate peripheral nerves involved in swallowing, enhances pharyngeal muscle coordination, and restores the swallowing reflex.
This study has several limitations. First, due to practical constraints, we did not use fiberoptic endoscopic evaluation of swallowing (FEES) or videofluoroscopic swallowing study (VFSS) to assess changes in swallowing function before and after treatment in PSD patients. Additionally, we did not compare treatment outcomes by stroke type, which could provide insights into differential responses. Follow-up assessments were not conducted, primarily due to patients’ post-stroke motor dysfunction and older age, which limited the evaluation of long-term efficacy. Due to the inherent procedural differences between acupuncture and CRT, patient blinding was not feasible. As a result, participants’ awareness of their treatment allocation may have introduced expectancy bias, potentially affecting the objectivity of outcome assessments. Moreover, this study did not include a sham acupuncture control group. Finally, as all participants were recruited from a single hospital, the generalizability of the findings may be restricted.
To address the above limitations, future research should incorporate large-scale, multi-center, and rigorously designed clinical studies with follow-up evaluations to assess long-term treatment efficacy. The application of FEES or VFSS would provide more objective assessments of swallowing function. Incorporating a sham acupuncture control group could better control for placebo effects and patient expectancy bias. Stratifying analyses by stroke type may further enhance the clinical applicability of the findings. Furthermore, investigating neurotrophic factors and inflammatory markers could facilitate a more comprehensive exploration of the recovery mechanisms underlying PSD.
Conclusion
This study found that a 4-week course of acupuncture combined with CRT significantly improved swallowing function, 5-HT levels, nutritional status, and quality of life in PSD patients compared to CRT alone. These findings suggest that the combined therapeutic approach may offer meaningful clinical benefits in promoting functional recovery. Given its safety, minimal invasiveness, and complementary role, acupuncture presents practical advantages when integrated into conventional PSD rehabilitation strategies. Further research is warranted to validate these benefits and support evidence-based clinical decision-making and broader implementation.
Clinical Registration
This study was registered in the Chinese Clinical Trial Registry (ChiCTR2100052028)
Data Sharing Statement
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the ethics committee of the Second Affiliated Hospital of Anhui University of Chinese Medicine (2021-zj-40). This study was performed in accordance with the declaration of Helsinki. All patients have signed an informed consent statement.
Acknowledgments
We express our sincere appreciation to all participants in this study.
Funding
This study was supported by Anhui Clinical Medical Research Translational Project (202304295107020123).
Disclosure
The authors declare that they have no conflicts of interest regarding this work.
References
1. Chen X, Zheng J, Wang J, et al. Global burden and cross-country inequalities in stroke and subtypes attributable to diet from 1990 to 2019. BMC Public Health. 2024;24(1):1813. doi:10.1186/s12889-024-19337-5
2. Sasegbon A, Cheng I, Hamdy S. The neurorehabilitation of post-stroke dysphagia: physiology and pathophysiology. J Physiol. 2024;603(3):617–634. doi:10.1113/JP285564.
3. Chen J, Chen J, Wang Y, et al. Transition experiences of patients with post stroke dysphagia and family caregivers: a longitudinal, qualitative study. PLoS One. 2024;19(6):e0304325. doi:10.1371/journal.pone.0304325
4. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–2763. doi:10.1161/01.STR.0000190056.76543.eb
5. Song W, Wu M, Wang H, Pang R, Zhu L. Prevalence, risk factors, and outcomes of dysphagia after stroke: a systematic review and meta-analysis. Front Neurol. 2024;15:1403610. doi:10.3389/fneur.2024.1403610
6. Dziewas R, Michou E, Trapl-Grundschober M, et al. European stroke organisation and European society for swallowing disorders guideline for the diagnosis and treatment of post-stroke dysphagia. Eur Stroke J. 2021;6(3):LXXXIX–CXV. doi:10.1177/23969873211039721
7. Guo H, Pan X, Zheng Y, et al. Current state of research on acupuncture for the treatment of post-stroke dysphagia: a scoping review. Front Neurosci. 2024;18:1391576. doi:10.3389/fnins.2024.1391576
8. Zhu H, Deng X, Luan G, Zhang Y, Wu Y. Comparison of efficacy of non-pharmacological intervention for post-stroke dysphagia: a systematic review and Bayesian network meta-analysis. BMC Neurosci. 2023;24(1):53. doi:10.1186/s12868-023-00825-0
9. Zhang J, Wu M, Li X, et al. Effect of acupuncture on dysphagia after stroke: a meta-analysis and trial sequential analysis of randomized controlled trials. Cerebrovasc Dis. 2025; 1–25. doi:10.1159/000544743
10. Ke Z, Liu W, Xiong Z, et al. Neural mechanism analysis of electroacupuncture in the treatment of post-stroke dysphagia. J Liaoning Univ Tradit Chin Med. 2024;26(3):51–55. doi:10.13194/j.issn.1673-842x.2024.03.012
11. Yuan S, Qiu B, Liang Y, et al. Role of TRPV1 in electroacupuncture-mediated signal to the primary sensory cortex during regulation of the swallowing function. CNS Neurosci Ther. 2024;30(3):e14457. doi:10.1111/cns.14457
12. Yao L, Ye Q, Liu Y, et al. Electroacupuncture improves swallowing function in a post-stroke dysphagia mouse model by activating the motor cortex inputs to the nucleus tractus solitarii through the parabrachial nuclei. Nat Commun. 2023;14(1):810. doi:10.1038/s41467-023-36448-6
13. Liang X, Yan L, Zhang Y, et al. Lateral needling at lianquan (CV 23) for post-stroke dysphagia: a randomized controlled trial. Zhongguo Zhen Jiu. 2022;42(7):717–720. doi:10.13703/j.0255-2930.20210712-k0003
14. Choy J, Pourkazemi F, Anderson C, et al. Dosages of swallowing exercises in stroke rehabilitation: a systematic review. Eur Arch Otorhinolaryngol. 2023;280(3):1017–1045. doi:10.1007/s00405-022-07735-7
15. Li X, Wu M, Zhang J, et al. Post-stroke dysphagia: neurological regulation and recovery strategies. Biosci Trends. 2025;19(1):31–52. doi:10.5582/bst.2025.01029
16. Li L, Deng K. Acupuncture combined with swallowing training for poststroke dysphagia: a meta-analysis of randomised controlled trials. Acupunct Med. 2019;37(2):81–90. doi:10.1136/acupmed-2016-011305
17. Xu J, Liu J, Peng Y. Tongnao Huoluo Liyan acupuncture combined with rehabilitation training for post-stroke dysphagia: a randomized controlled trial. Zhongguo Zhen Jiu. 2025;45(4):435–441. doi:10.13703/j.0255-2930.20240327-k0004
18. Kessler JP, Jean A. Inhibition of the swallowing reflex by local application of serotonergic agents into the nucleus of the solitary tract. Eur J Pharmacol. 1985;118(1–2):77–85. doi:10.1016/0014-2999(85)90665-x
19. Sood S, Liu X, Liu H, et al. 5-HT at hypoglossal motor nucleus and respiratory control of genioglossus muscle in anesthetized rats. Respir Physiol Neurobiol. 2003;138(2–3):205–221. doi:10.1016/j.resp.2003.07.001
20. Haney MM, Sinnott J, Osman KL, et al. Mice lacking brain-derived serotonin have altered swallowing function. Otolaryngol Head Neck Surg. 2019;161(3):468–471. doi:10.1177/0194599819846109
21. Hashim MA, Bieger D. Excitatory action of 5-HT on deglutitive substrates in the rat solitary complex. Brain Res Bull. 1987;18(3):355–363. doi:10.1016/0361-9230(87)90013-x
22. Yang S, Gao R, Lu Y. Law of acupoint selection in acupuncture treatment on dysphagia after stroke. J Emerg Tradit Chin Med. 2018;27(6):979–981. doi:10.3969/j.issn.1004-745X.2018.06.011
23. Wang S, Zhang H, Liu H, et al. Literature research of acupoint selection rules in acupuncture treatment of dysphagia after stroke. J Tradit Chin Med. 2017;58(16):1412–1415. doi:10.13288/j.11-2166/r.2017.16.016
24. Liang Y, Lin J, Wang H, et al. Evaluating the efficacy of vitalstim electrical stimulation combined with swallowing function training for treating dysphagia following an acute stroke. Clinics. 2021:
25. Wang X, Huang G, Wang D, et al. Effects of cerebellar repetitive transcranial magnetic stimulation on stroke rehabilitation: a systematic review and meta-analysis. Brain Res Bull. 2025;225:111341. doi:10.1016/j.brainresbull.2025.111341
26. McCarty EB, Chao TN. Dysphagia and swallowing disorders. Med Clin North Am. 2021;105(5):939–954. doi:10.1016/j.mcna.2021.05.013
27. Wu Y, Zhang Z, Li Q, et al. Clinical study on the efficacy of postural control combined with electroacupuncture in treating dysphagia after stroke. Front Neurol. 2024;15:1296758. doi:10.3389/fneur.2024.1296758
28. Antonios N, Carnaby-Mann G, Crary M, et al. Analysis of a physician tool for evaluating dysphagia on an inpatient stroke unit: the modified Mann assessment of swallowing ability. J Stroke Cerebrovasc Dis. 2010;19(1):49–57. doi:10.1016/j.jstrokecerebrovasdis.2009.03.007
29. McHorney CA, Robbins J, Lomax K, et al. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. 2002;17(2):97–114. doi:10.1007/s00455-001-0109-1
30. Mayor D, Tymianski M. Neurotransmitters in the mediation of cerebral ischemic injury. Neuropharmacology. 2018;134(Pt B):178–188. doi:10.1016/j.neuropharm.2017.11.050
31. Sood A, Mehrotra A, Dhawan DK, Sandhir R. Neuroprotective effects of Withania somnifera on ischemic stroke are mediated via anti-inflammatory response and modulation of neurotransmitter levels. Neurochem Int. 2024;180:105867. doi:10.1016/j.neuint.2024.105867
32. Bieger D. Role of bulbar serotonergic neurotransmission in the initiation of swallowing in the rat. Neuropharmacology. 1981;20(11):1073–1083. doi:10.1016/0028-3908(81)90099-x
33. Bai L, Cheng H, Hu P, et al. Effect of acupuncture on post-stroke dysphagia: a randomized controlled trial. Front Neurol. 2024;15:1391226. doi:10.3389/fneur.2024.1391226
34. Thor KB, Blitz-Siebert A, Helke CJ. Autoradiographic localization of 5HT1 binding sites in autonomic areas of the rat dorsomedial medulla oblongata. Synapse. 1992;10(3):217–227. doi:10.1002/syn.890100305
35. Manaker S, Verderame HM. Organization of serotonin 1A and 1B receptors in the nucleus of the solitary tract. J Comp Neurol. 1990;301(4):535–553. doi:10.1002/cne.903010405
36. You H, Hu S, Ye QP, et al. Role of 5-HT1A in the nucleus of the solitary tract in the regulation of swallowing activities evoked by electroacupuncture in anesthetized rats. Neurosci Lett. 2018;687:308–312. doi:10.1016/j.neulet.2018.06.018
37. Sabbouh T, Torbey MT. Malnutrition in stroke patients: risk factors, assessment, and management. Neurocrit Care. 2018;29(3):374–384. doi:10.1007/s12028-017-0436-1
38. Chai J, Chu FCS, Chow TW, Shum NC. Prevalence of malnutrition and its risk factors in stroke patients residing in an infirmary. Singapore Med J. 2008;49(4):290–296.
39. Foley NC, Martin RE, Salter KL, Teasell RW. A review of the relationship between dysphagia and malnutrition following stroke. J Rehabil Med. 2009;41(9):707–713. doi:10.2340/16501977-0415
40. Lamb CA, Parr J, Lamb EIM, Warren MD. Adult malnutrition screening, prevalence and management in a United Kingdom hospital: cross-sectional study. Br J Nutr. 2009;102(4):571–575. doi:10.1017/S0007114509236038
41. Gomes F, Emery PW, Weekes CE. Risk of malnutrition is an independent predictor of mortality, length of hospital stay, and hospitalization costs in stroke patients. J Stroke Cerebrovasc Dis. 2016;25(4):799–806. doi:10.1016/j.jstrokecerebrovasdis.2015.12.017
42. Yoshimura Y, Wakabayashi H, Nagano F, Bise T, Shimazu S, Shiraishi A. Low hemoglobin levels are associated with sarcopenia, dysphagia, and adverse rehabilitation outcomes after stroke. J Stroke Cerebrovasc Dis. 2020;29(12):105405. doi:10.1016/j.jstrokecerebrovasdis.2020.105405
43. Jamil A, Imtiaz M, Muhammad A, et al. Evidence based therapeutic and assessment techniques to rehabilitate post stroke dysphagia patients-A systematic review. Eur Arch Otorhinolaryngol. 2024;282(1):1–10. doi:10.1007/s00405-024-08874-9
44. Xu F, Bai L, Dai Z, Cheng H. Research hotspots and trends in post-stroke dysphagia: a bibliometric analysis. Front Neurosci. 2023;17:1275748. doi:10.3389/fnins.2023.1275748
45. Magara J, Watanabe M, Tsujimura T, Hamdy S, Inoue M. Cold thermal oral stimulation produces immediate excitability in human pharyngeal motor cortex. Neurogastroenterol Motil. 2018;30(10):e13384. doi:10.1111/nmo.13384
46. Mepani R, Antonik S, Massey B, et al. Augmentation of deglutitive thyrohyoid muscle shortening by the shaker exercise. Dysphagia. 2009;24(1):26–31. doi:10.1007/s00455-008-9167-y
47. Easterling C. Does an exercise aimed at improving swallow function have an effect on vocal function in the healthy elderly?. Dysphagia. 2008;23(3):317–326. doi:10.1007/s00455-008-9158-z
48. Park JS, Hwang NK, Oh DH, Chang MY. Effect of head lift exercise on kinematic motion of the hyolaryngeal complex and aspiration in patients with dysphagic stroke. J Oral Rehabil. 2017;44(5):385–391. doi:10.1111/joor.12492
49. McCullough GH, Kim Y. Effects of the Mendelsohn maneuver on extent of hyoid movement and UES opening post-stroke. Dysphagia. 2013;28(4):511–519. doi:10.1007/s00455-013-9461-1
50. Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2016;47(6):e98–e169. doi:10.1161/STR.0000000000000098
51. Yu J, Zhu Y, Mao JH, Yuan JH, Xu YL, Huang JX. Scalp-nape acupuncture as adjuvant therapy for pharyngeal dysphagia of stroke at recovery stage: a randomized controlled trial. Zhongguo Zhen Jiu. 2022;42(5):481–485. doi:10.13703/j.0255-2930.20210620-k0003
52. Yuan Y, Cai XH, Chen F, et al. Clinical trials of acupuncture treatment of post-stroke dysphagia by deep acupuncture of Tiantu (CV22) in combination with swallowing rehabilitation training. Zhen Ci Yan Jiu. 2019;44(1):47–50. doi:10.13702/j.1000-0607.170788
53. Jean A. Brain stem control of swallowing: neuronal network and cellular mechanisms. Physiol Rev. 2001;81(2):929–969. doi:10.1152/physrev.2001.81.2.929
54. Kamarunas E, Mulheren R, Palmore K, Ludlow C. Timing of cortical activation during spontaneous swallowing. Exp Brain Res. 2018;236(2):475–484. doi:10.1007/s00221-017-5139-5
55. Fu X, Li H, Yang W, et al. Electroacupuncture at HT5 + GB20 promotes brain remodeling and significantly improves swallowing function in patients with stroke. Front Neurosci. 2023;17:1274419. doi:10.3389/fnins.2023.1274419
56. Cui S, Yao S, Wu C, et al. Electroacupuncture involved in motor cortex and hypoglossal neural control to improve voluntary swallowing of poststroke dysphagia mice. Neural Plast. 2020;2020:8857543. doi:10.1155/2020/8857543
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



