Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Effects of Physical Activity, VO2max, and Visfatin on Relationship Between BMI and Chronic Inflammation
Authors Su L , Wu S, Fu J, Sun S
Received 11 April 2024
Accepted for publication 14 November 2024
Published 26 November 2024 Volume 2024:17 Pages 4489—4500
DOI https://doi.org/10.2147/DMSO.S473266
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Liqiang Su,1,2 Shouzhi Wu,3 Jinmei Fu,4 Shunli Sun4
1Physical Education of College, Jiangxi Normal University, Nanchang City, Jiangxi Province, People’s Republic of China; 2School of Physical Education and Sport Science, Fujian Normal University, Fuzhou City, Fujian Province, People’s Republic of China; 3School of Public Foundation, Wannan Medical College, Wuhu City, Anhui Province, People’s Republic of China; 4Jiangxi Sports Science Medical Center, Nanchang City, Jiangxi Province, People’s Republic of China
Correspondence: Liqiang Su; Shouzhi Wu, Email [email protected]; [email protected]
Purpose: This study aims to explore the relationship between BMI and chronic inflammation and to investigate the interaction and mediation of physical activity (PA), cardiopulmonary function, and visfatin.
Methods: A total of 119 participants were included in the study, 60 in the obesity group, 30 in the normal weight group, and 29 in the overweight group. PA, VO2max, visfatin, high-sensitivity C-reactive protein (hs-CRP), and four blood lipid indices (TC, TG, HDLC, LDLC) were analyzed. Regression analysis was used to understand the effect of BMI on chronic inflammation. Covariate analysis was conducted to screen effective covariates affecting BMI to predict chronic inflammation and test the interaction and intermediary role of effective covariates.
Results: The increase in BMI could aggravate chronic inflammation. PA, VO2max, and visfatin had interactive effects on BMI affecting chronic inflammation, and visfatin played an intermediary role in BMI affecting chronic inflammation. The effect value of BMI on chronic inflammation in terms of low PA was 3.5 times higher than that of high PA, that of low VO2max was 2.8 times higher than that of high VO2max, and that of high visfatin was 3.65 times higher than that of low visfatin. Approximately 19.35% of the effect was mediated by visfatin.
Conclusion: An increase in BMI can aggravate chronic inflammation. Increases in PA and VO2max can alleviate chronic inflammation, and visfatin plays a positive mediating role.
Keywords: obesity, chronic inflammation, physical activity, VO2max, visfatin
Introduction
Obesity and related metabolic diseases, tumors, and other diseases have increased dramatically worldwide;1,2 these diseases will not only reduce the quality of life of individuals but also bring a huge burden to families and society. Obesity has become a research focus of scholars. A study found that the process of individuals from normal weight to obesity was accompanied by intensification of chronic inflammation.3 Chronic inflammation always occurs without clinical symptoms and induces many diseases.4 To identify the risk and prognosis of obesity-related diseases, scholars use indicators, such as TNF-α and hs-CRP, as well as the intermediate or end products of chronic inflammatory reaction.5 Chronic inflammation was found to be positively correlated with obesity.6 It varies among people with similar BMI. In addition to BMI, many factors can affect chronic inflammation. Energy accumulation is closely related to BMI and chronic inflammation.7 Therefore, we can identify the risk factors of chronic inflammation from multiple perspectives and explore the regulatory role of energy accumulation (PA, cardiopulmonary function, fat factor, etc.) in the relationship between BMI and chronic inflammation.
Epidemiological studies show that decreased PA is associated with increased chronic inflammation.8–10 Conversely, increased PA can alleviate chronic inflammation.11,12 Cardiopulmonary function is negatively correlated with chronic inflammation.13,14 Improvement of cardiopulmonary function can alleviate the aggravation of chronic inflammation.12 Although an increase in BMI can aggravate the accumulation of chronic inflammation,3 greater PA and cardiopulmonary function can alleviate it. However, during the development of obesity from normal weight, with the increase of BMI, the regulatory effect of different PA and cardiopulmonary function on chronic inflammation remains unclear.
Studies on the regulation of chronic inflammation show that the degree of adipose tissue accumulation is significantly related to the amount of visfatin secreted by fat.15–17 In obese people, chronic inflammation is significantly positively correlated with the level of circulating visfatin.17 As such, visfatin can drive chronic inflammation.18,19 Although current epidemiology literature indicates that visfatin affects chronic inflammation15,19, the specific effects of different concentrations of visfatin have not been reported yet in the process of BMI increasing and developing into obesity. However, individual energy accumulation factors (PA, cardiopulmonary function, adipokine, etc.) vary greatly, and these variations may change the degree of chronic inflammation. Therefore, learning that these factors can regulate chronic inflammation in the process of increasing BMI has an important guiding role in the prevention of obesity and its related diseases.
This study aimed to clarify the regulatory effect of PA, cardiorespiratory function and visfatin on the process of increasing BMI and developing into obesity.
Material and Methods
Participants and Recruitment
From May 2020 to July 2020, adult participants for weight loss and fitness evaluation were recruited at Yangzhou Lipan Weight Loss Training Camp in Yangzhou City. The inclusion criteria were as follows: BMI of the normal weight group: 18.5–23.9, super recombinant BMI: 24–27.9, and BMI of the obesity group: ≥ 28. The exclusion criteria included the following: inflammatory events, infectious diseases, long-term medication, hypertension, diabetes, professional sports training, and sports contraindications. In the training camp, health files were established for volunteers who participated in the training and mastered their health awareness, behavior, and PA before entering the camp. This study was ethically approved by Fujian Normal University Ethics Committee. The clinical trial registration number is ChiCTR2200058959. The participants signed an informed consent form.
This study used “multivariate regression analysis model with added covariates” in G-power 3.1.9.2 software to estimate sample size.20,21 R2 was used to measure the amount of effect.22 According to Cohen (1998), 23 R2 = 0.13 indicates medium test efficiency. For the intermediary effect analysis as an example (R2=0.13), the calculated regression model effect size f2 is 0.15, the α error is 0.05, the power (1-βerror) is 0.9, and the total sample size is 108. The sample size estimates required by other statistical analysis methods are similar. In the present study, 140 volunteers were collected, and the data of each volunteer were checked according to the exclusion criteria. A total of 21 volunteers were excluded (7 individuals with long-term medication use, 4 with hypertension, 3 with diabetes, 3 with a history of professional training, and 4 with sports injuries). Finally, 119 volunteers were included, which satisfied the need of statistical analysis to achieve medium test efficiency.
Outcome Measures
PA was measured using International PA Questionnaire (short version). The PA questionnaire consists of three main components: basic information (including name, gender, age, height, and weight), health history (covering physical examination status, disease history, medication use, and sports injury history), and physical activity assessment. The physical activity section adopts the International Physical Activity Questionnaire (IPAQ-Short Form), which has been validated for reliability and validity in Chinese populations. The questionnaire functions to evaluate total physical activity levels by calculating exercise volume using metabolic equivalent tasks (MET), providing scores in MET min/week. This calculation incorporates different intensity levels of activity, where total physical activity equals the sum of vigorous activity (8.0 MET), moderate activity (4.0 MET), and light activity (3.3 MET), each multiplied by its respective duration and frequency.
Height was measured using an instrument with an accuracy of 0.1 cm. Weight was measured on an empty stomach in the morning (unit: kg).
A VO2max test was conducted. The 20-meter round trip is a load method used to evaluate cardiopulmonary function.24 Maximum oxygen consumption (VO2max) was evaluated by the level completed by the tester (unit: mL/kg/min).
TC, TG, HDLC, LDLC, visfatin, and hs-CRP were measured. Blood was collected from the volunteers on an empty stomach from 7:00 to 8:00 in the morning the next day when they entered the camp to participate in training and fasted after 22:00 the day before. About 5 mL of blood was drawn from the elbow vein of negative-pressure blood collection vessel containing separating gel accelerator. Visfatin was measured in Wuhan Eliot Biotechnology Co., Ltd. TC, TG, HDLC, LDLC, and hs-CRP was measured in Nanjing Aidikang Medical Laboratory.
Statistical Analysis
Quantitative data were expressed by mean ± standard deviation. Qualitative data were evaluated by frequency (percentage). The regression analysis results were presented by β (95% confidence interval). Data were processed and analyzed by statistical packages R (the R Foundation, version 3.1.2) and Empower (R). P < 0.05 indicates that the difference is statistically significant, and P < 0.01 means the difference is very statistically significant.
Chi square test was used for comparison of gender differences. The differences in these variables (age, height, weight, BMI, hs-CRP, TC, TG, HDLC, LDLC, Visfatin, PA, VO2max) between different groups were compared using one-way ANOVA if the data followed a normal distribution, and the Kruskal-Wallis rank sum test was employed if the data did not follow a normal distribution.
The pairwise correlation between these variables (hs-CRP, BMI, PA, VO2max, Visfatin) was analyzed using Pearson’s correlation coefficient.
The regulation of PA, VO2max, and visfatin in the impact of BMI on chronic inflammation was analyzed using the interaction effect approach. Chronic inflammation was set as the dependent variable, and BMI as the independent variable. The PA, VO2max, and visfatin variables were divided into three equal parts based on their data magnitudes (eg, dividing visfatin into three equal groups based on concentration levels: high, medium, and low concentration groups) to serve as effect modifiers in the interaction. Age and gender were included as adjusted variables.
It is generally believed that indicators serving as mediators are often endogenous substances within the body. In this study, visfatin was treated as a potential mediator, and a mediation analysis was conducted to examine its role in the effect of BMI on chronic inflammation.
Results
Study Population Characteristics
As shown in Table 1, among the 119 volunteers, 60 were in the obesity group, 29 were in the overweight group, and 30 were in the normal weight group. The average age was 28.30 ± 6.80 years, and the average height was 169.27 ± 8.25 cm. No significant difference was found in age and height among groups. Body weight, BMI, TC, TG, LDLC, visfatin, PA, VO2max, and hs-CRP were significantly different among the three groups (P < 0.01).
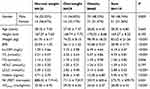 |
Table 1 Characteristics of Participants with Different BMI |
Correlation Among Hs-CRP, BMI, PA, VO2max, Visfatin
Correlation coefficients among hs-CRP, BMI, PA, VO2max, and visfatin were calculated. hs-CRP and BMI had the largest correlation coefficient and had significant correlation with PA, VO2max, and visfatin (Table 2). Chronic inflammation is closely related to BMI, while PA, VO2max, and visfatin may affect the relationship between BMI and chronic inflammation.
 |
Table 2 Correlation Coefficient Among Indicators |
Interaction Between PA and BMI on Chronic Inflammation
According to the effect of different physical activities on chronic inflammation of BMI (Table 3, Model 2), the effect of lower the PA subgroup (42.6–105.5) is 0.59, the effect of the medium PA subgroup (115.2–600.3) is 0.42, and the effect of the higher PA subgroup (602.4–2923.2) is 0.18. In the lower PA group, every increase in BMI can be accompanied by an increase of 0.59mg/L in hs-CRP; in the higher PA subgroup, every increase in BMI can be accompanied by an increase of 0.18mg/L in hs-CRP. This result shows that greater PA can reduce the effect of BMI on inflammation. Hence, PA and BMI have a significant interaction effect on chronic inflammation (P = 0.0231).
 |
Table 3 Hierarchical Regression and Interaction Test of Each Covariate (PA, VO2max, Visfatin) |
Interaction Between Cardiopulmonary Function and BMI on Chronic Inflammation
From the perspective of the effect of VO2max and BMI on chronic inflammation (Table 3, Model 2), the effect level of the lower VO2max subgroup (21.3–24.0) is 0.71, that of the medium VO2max subgroup (24.1–27.8) is 0.32, and that of the higher VO2max subgroup (27.9–40.9) is 0.27. In the lower VO2max subgroup, every increase in BMI can be accompanied by an increase of 0.71 mg/L in hs-CRP; in the higher VO2max subgroup, every increase in BMI can be accompanied by an increase of 0.27 mg/L in hs-CRP. This result shows that a high VO2max level can reduce the effect of BMI on inflammation. VO2max and BMI have a significant interaction effect on chronic inflammation (P = 0.0113).
Effect of Visfatin and BMI on Chronic Inflammation
Interaction Between Visfatin and BMI on Chronic Inflammation
According to the effect of different concentrations of visfatin and BMI on chronic inflammation (Table 3, Model 2), the effect of low concentration (1.6–5.8) is 0.17, that of medium concentration (6.1–11.2) is 0.54, and that of high concentration (11.4–28.3) is 0.62. In the low concentration subgroup, each increase in BMI can be accompanied by an increase in hs-CRP of 0.17 mg/L; in the high concentration subgroup, each increase in BMI can be accompanied by an increase in hs-CRP of 0.62 mg/L. This result shows that a high concentration of visfatin can cause BMI to have a greater effect on inflammation. A significant interaction effect was found between visfatin and BMI on chronic inflammation (P = 0.0082).
Mediation of Visfatin in the Influence of BMI on Chronic Inflammation
Table 4 shows that whether gender and age are adjusted or not has little effect on the mediating role of visfatin. Based on model 2 with gender and age adjustment, BMI can significantly affect hs-CRP, with the total effect value c of 0.4506 (P < 0.05). The direct effect value c’ played by BMI is 0.3634 (P < 0.05), visfatin plays a significant mediating role, and the mediating effect value a * b is 0.0872 (P < 0.05). The effect of BMI on hs-CRP is 19.35% mediated by visfatin.
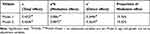 |
Table 4 Mediation of Visfatin in the Influence of BMI on Hs-CRP |
Discussion
Obesity is a Risk Factor for Chronic Inflammation
Obesity-related chronic inflammation increases the risk of cardiovascular diseases. hs-CRP can widely and diffusely reflect the scope and status of chronic inflammation and can be used as a biological marker to evaluate chronic inflammation.5,25–27 Different levels of obesity can lead to different chronic inflammatory states. This study shows that there is a significant difference in the concentration of hs-CRP in the serum of the normal weight group, the super recombinant, and the obese group (Table 1). This finding is consistent with results from large epidemiological studies such as the Framingham Heart Study, which also reported a clear gradient in hs-CRP levels across weight categories, with the highest levels observed in obese individuals.28 Our results further support the notion that hs-CRP is a reliable marker for obesity-related chronic inflammation and cardiovascular risk. Chronic inflammation is the main cause of obesity-induced diseases. Clarifying the relationship between chronic inflammation and many cardiovascular risk factors has a positive role in promoting obesity health.
Relationship Between Obesity and Chronic Inflammation is Influenced by PA, VO2max, and Visfatin
Obesity is the result of induction of multiple risk factors that have certain correlations. The decrease in body energy consumption associated with the decline of PA can induce obesity and lead to the decline of heart and lung functions. Fat tissue accumulation associated with obesity may induce inflammation through visfatin. This study shows that chronic inflammation, obesity degree, PA, cardiorespiratory function, and visfatin are all correlated, and the correlation coefficient between chronic inflammation and BMI is the largest. Hence, chronic inflammation has a greater correlation with BMI, while PA, VO2max, and visfatin may affect the correlation between BMI and chronic inflammation. Since chronic inflammation plays a major role in obesity-induced cardiovascular diseases and visfatin, PA, and cardiorespiratory function are closely related to obesity, clarifying the regulatory roles of PA, cardiorespiratory function, and visfatin is of great significance for the health education of obese people. The effect of PA on serum visfatin levels is controversial. Some studies indicate that regular PA can lower serum visfatin levels, which may be related to a reduction in adipose tissue inflammation and an improvement in metabolic health.29 However, other research suggests that short-term high-intensity exercise may cause a temporary increase in serum visfatin levels, likely due to exercise-induced inflammatory responses and adipose tissue stress.30 Therefore, the specific impact of PA on visfatin may depend on the type, intensity, and duration of the exercise. The impact of PA on visfatin appears to be contingent upon the type, intensity, and duration of the exercise.
Interaction Between PA and BMI on Chronic Inflammation
In this study, three groups were divided according to the size of PA. A significant interaction was found between PA and BMI on chronic inflammation. The decrease in PA increases the accumulation of chronic inflammation caused by BMI.
The ACSM Exercise Testing and Exercise Prescription Guide defines sedentary and sedentary behavior as not participating in moderate PA at least 3 days a week and no less than 30 minutes a day for more than 3 months. Sedentary behavior refers to the behavior of sitting or lying in a conscious state, which consumes no more than 1.5 MET of energy.31,32 In our study, the PA level of the low PA subgroup is 42.6–105.5 MET min/week, which belongs to the category of sedentary and low activity. At this level of PA, the increase in BMI has a higher proinflammatory effect, which may be an important reason for the induction of many diseases. Sedentary inactivity of more than 7 hours a day is associated with increased mortality.33 The PA of people engaged in leisure sports was reduced to less than 5000 steps/day. On the fifth day, the blood flow regulating vascular diastolic function was significantly reduced.34,35 These results show that low PA does great harm to health. This study extends this phenomenon from the perspective of the relationship between low PA and chronic inflammation. Low PA can harm health by affecting chronic inflammation. In addition, this study not only clarified the level of effect of BMI of different PA groups on chronic inflammation but also identified that the effect of increasing BMI of low PA groups on chronic inflammation is 3.5 times that of high PA groups (Table 3, Figure 1). Hence, low PA has a greater proinflammatory effect on the process of increasing BMI, while high PA can alleviate chronic inflammation.
From the perspective of health acquisition, increased PA can improve the oxidative energy supply capacity of the body, reduce oxidative stress, and improve lipid metabolism and cardiopulmonary function. These health benefits are closely related to reducing the accumulation of chronic inflammation. The improvement of lipid metabolism disorder can reduce the ability of LDLC to cause immune cells to migrate to vascular endothelial cells, thereby alleviating the proinflammatory reaction.36 Improvement of oxidative stress can lead to the improvement of oxidative stress signal pathways, and many of which are also signal pathways of inflammatory reaction. The results found that increasing PA cannot only improve lipid metabolism and cardiopulmonary function but also play a good anti-inflammatory role. For obese people, if the weight loss effect is not ideal within a certain period, then increasing the PA can still reduce the negative impact of chronic inflammation on health, thereby reducing the risk of related diseases.
Interaction Between Cardiopulmonary Function and BMI on Chronic Inflammation
In this study, a significant interaction was found between cardiopulmonary function and BMI on chronic inflammation, and the interaction effect was not affected by age and gender (Table 3). Cardiopulmonary function is an important manifestation of physical function improvement and the basis of resistance to many diseases. According to the report of New England Medical Journal, cardiopulmonary function has a stronger predictive effect on mortality, and every reduction in the level of cardiopulmonary function by 1 MET increases the risk of death by 12%.37 Cardiopulmonary function is of great significance to health, and chronic inflammation is an important channel for cardiopulmonary function to affect health. The results showed that hs-CRP, a marker of chronic inflammation, was negatively correlated with VO2max. A study on adults aged 20–34 years found that the level of cardiopulmonary function was significantly negatively correlated with chronic inflammation markers, namely, CRP and IL-6; the results also showed that VO2max was negatively correlated with chronic inflammation in the elderly.13,14 In addition, people with a high baseline level of CRP, an inflammatory marker, may reduce the improvement of cardiopulmonary function brought by exercise training38. These results show that the decline of heart and lung function can promote the aggravation of chronic inflammation, consistent with the present work.
Low cardiopulmonary function leads to the reduction of blood supply and oxygen supply of the heart, promote the hypoxia of tissues, damage the mitochondrial function, increase the oxidative stress, and activate pro-inflammatory pathways leading to chronic inflammation.39 Low external cardiopulmonary function can affect chronic inflammation by changing the methylation of apoptosis-related spot-like protein (ASC).40 These results link cardiopulmonary function with chronic inflammation from a mechanistic point of view. The present study investigated the regulatory effect of cardiopulmonary function on the relationship between BMI and chronic inflammation. Weak cardiopulmonary function can aggravate the accumulation of chronic inflammation, while good cardiopulmonary function can alleviate it.
Furthermore, muscle mass plays a crucial role in the context of chronic inflammation. Studies have shown that muscle tissue itself can produce anti-inflammatory factors, such as IL-10 and IL-1RA, which help inhibit inflammatory responses.41 Therefore, even in cases of high BMI, individuals with greater muscle mass may experience mitigated levels of chronic inflammation, suggesting that BMI alone may not suffice for a comprehensive risk assessment.
Moreover, the relationship between physical activity and muscle mass is interconnected. High levels of physical activity are typically associated with increased muscle mass, which not only enhances basal metabolic rate but also improves cardiopulmonary function by promoting better oxygen and nutrient transport.42 This enhancement can further reduce oxidative stress and activate inflammatory pathways, thereby lowering the risk of chronic inflammation. Thus, the benefits of physical activity extend beyond fat reduction; they also include muscle mass improvement, which indirectly influences chronic inflammation.
As noted earlier, good cardiopulmonary function can alleviate chronic inflammation. It is plausible that the increase in muscle mass from high physical activity also modulates chronic inflammation by further improving cardiopulmonary function. Therefore, individuals with high BMI but high physical activity levels may not face as severe chronic inflammation risks, possibly due to the protective effects tied to their muscle mass.
Based on these considerations, a comprehensive assessment strategy for chronic inflammation should account for body composition, rather than relying solely on BMI. For instance, individuals with high BMI but a high level of physical activity may require a different risk evaluation for chronic inflammation which incorporates muscle mass and additional biomarkers such as adiponectin and leptin. Future research should delve into how increasing muscle mass can optimize the benefits of physical activity on chronic inflammation, potentially leading to novel strategies for preventing and treating chronic inflammation.
Effect of Visfatin on Chronic Inflammation in Patients with BMI
Interaction Between Visfatin and BMI on Chronic Inflammation
As an important factor of fat secretion, visfatin is closely related to chronic inflammation. The results show that visfatin is significantly and positively correlated to hs-CRP, a marker of chronic inflammation (Table 3). Derosa G et al43 showed that visfatin is associated with obesity-related chronic inflammation. A meta-analysis of Lee YH44 reported the positive correlation between visfatin and chronic inflammatory marker CRP in rheumatoid individuals. However, the regulatory effect of different concentrations of visfatin on chronic inflammation in the process of increasing BMI has not been reported yet. This study not only found a significant positive correlation between BMI and visfatin but also quantified the interaction effect of visfatin on obesity-induced chronic inflammation. In the high-concentration visfatin group, the effect of visfatin regulating BMI on hs-CRP was affected by age and sex to some extent. In general, a high concentration of visfatin can aggravate the effect of chronic inflammation induced by BMI, thereby limiting the production of visfatin and reducing the aggravation of obesity-related chronic inflammation. In terms of visfatin source, animal experiments show that visceral fat secretes visfatin more specifically than subcutaneous fat.45 Studies show that visfatin is positively correlated with visceral fat.46 In the present study, visfatin is highly correlated with visceral fat (Table 3), suggesting that the proinflammatory effect of visceral fat may be related to the proinflammatory effect of visfatin in addition to the proinflammatory factor secreted by the fat itself.35 Given the complexity of the human internal environment and the multiplicity of the functions of visfatin, whether the proinflammatory effect of visfatin directly mediates chronic inflammation in the human body remains unknown.
Mediating Role of Visfatin in the Influence of BMI on Chronic Inflammation
In this study, visfatin played a significant positive mediating role in chronic inflammation caused by increased BMI, and the mediating role of visfatin is not affected by age and sex (Table 4). In 1994, visfatin was initially considered to be an immune-regulating cytokine.47 In 2005, it was found to be highly specifically expressed in adipose tissues.48 Visfatin is related to the activation of many inflammatory pathways, such as NF-κB. Mitogen-activated protein kinase (MAPK), phosphatidylinositol 3 kinase (PI3).19 Extensive research suggests that visfatin can also be regulated through the JAK2/STAT3 signaling pathway, which plays a crucial role in mediating inflammatory responses. Activation of the JAK2/STAT3 pathway by visfatin has been shown to enhance the expression of various pro-inflammatory cytokines, further exacerbating chronic inflammation. This signaling pathway promotes the transcription of inflammatory genes in response to visfatin signaling, contributing to the inflammatory processes associated with obesity and metabolic syndrome.49 Visfatin can regulate a variety of inflammatory genes in peripheral blood monocytes and stimulate the release of inflammatory mediators. In addition, visfatin can upregulate extracellular matrix proteins in preadipocytes, such as osteopontin, collagen VI, MMP-2, and MMP-9 and increase adipose tissue fibrosis,19 which is an important way to cause inflammation.50 Studies at the cytological level show that visfatin can promote inflammation and is related to chronic inflammation. Katsogiannos P et al found that the levels of visfatin and inflammatory markers in the obese group were significantly higher than those in the normal-weight group.51 Owczarek AJ reported that the variations in visfatin level in obese people could be related to obesity-related inflammatory markers hs-CRP and IL-6.17 Karbaschian Z et al found that the level of lipoproteins in peripheral blood was significantly correlated with the concentration of hs-CRP.52 These studies show that visfatin in the population is related to chronic inflammation but not directly related to the relationship between visfatin and chronic inflammation in the process of BMI increase. Visfatin plays an intermediary role of approximately 19.35% in chronic inflammation caused by BMI increase (Table 4). The results suggest that visfatin may become a candidate target for obese people to improve chronic inflammation; it can be reduced through exercise, diet, or drugs to resist related diseases induced by chronic inflammation.
This study highlights the clinical value of addressing the relationship between BMI and chronic inflammation. Improving physical activity and cardiorespiratory fitness, while targeting metabolic regulators like visfatin, can effectively reduce chronic inflammation exacerbated by higher BMI. Early intervention in overweight and obese patients, focusing on these modifiable factors, is crucial for preventing inflammatory diseases.
Conclusion
Variations in PA, cardiorespiratory function, and visfatin can regulate the influence of BMI on chronic inflammation. Increased PA and oxygen uptake and decreased visfatin can alleviate chronic inflammation caused by increased BMI. When the degree of obesity is difficult to improve, obesity-related chronic inflammation can be alleviated by increasing PA, improving heart and lung function, and reducing visfatin to reduce disease risk and increase health benefits.
Abbreviations
PA, physical activity; hs-CRP, high-sensitivity C-reactive protein; MET, metabolic equivalent tasks; ASC, apoptosis-related spot-like protein; MAPK, Mitogen-activated protein kinase; PI3K, Mitogen-activated protein kinase.
Data Sharing Statement
For data requests, please contact the corresponding author.
Ethical Approval and Consent to Participate
The trial was ethically approved by Fujian Normal University Ethics Committee with clinical trial registration number ChiCTR2200058959. All methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki). The participants signed an informed consent form.
Acknowledgments
This work was supported by Major Research Project in Humanities and Social Sciences in Anhui Province Universities (2023AH040235). The authors would like to thank all the participants for their valuable contribution.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kim MS, Kim WJ, Khera AV, et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J. 2021;42(34):3388–3403. doi:10.1093/eurheartj/ehab454
2. Quan M, Xun P, Wu H, et al. Effects of interrupting prolonged sitting on postprandial glycemia and insulin responses: a network meta-analysis. J Sport Health Sci. 2021;10(4):419–429. doi:10.1016/j.jshs.2020.12.006
3. Simoes E, Correia-Lima J, Sardas L, et al. Sex dimorphism in inflammatory response to obesity in childhood. Int J Obes Lond. 2021;45(4):879–887. doi:10.1038/s41366-021-00753-1
4. Karczewski J, Śledzińska E, Baturo A, et al. Obesity and inflammation. Eur Cytokine Netw. 2018;29(3):83–94. doi:10.1684/ecn.2018.0415
5. Setty BNY, Betal SG, Miller RE, et al. Relationship of Omega-3 fatty acids DHA and EPA with the inflammatory biomarker hs-CRP in children with sickle cell anemia. Prostaglandins Leukot Essent Fatty Acids. 2019;146:11–18. doi:10.1016/j.plefa.2019.05.004
6. Kenđel Jovanović G, Mrakovcic-Sutic I, Pavičić Žeželj S, Šuša B, Rahelić D, Klobučar Majanović S. The efficacy of an energy-restricted anti-inflammatory diet for the management of obesity in younger adults. Nutrients. 2020;12(11):3583. doi:10.3390/nu12113583
7. Xu B, Zhou L, Chen Q, et al. Role of VEGFR2 in mediating endoplasmic reticulum stress under glucose deprivation and determining cell death, oxidative stress, and inflammatory factor expression. Front Cell Dev Biol. 2021;9:631413. doi:10.3389/fcell.2021.631413
8. Ford E. Does Exercise Reduce Inflammation? Physical Activity and C-Reactive Protein Among U.S. Adults. Epidemiology. Vol. 13. Cambridge, Mass, 2002;561–568.
9. Mora S, Lee I-M, Buring JE, Ridker PM. Association of physical activity and body mass index with novel and traditional cardiovascular biomarkers in women. JAMA. 2006;295(12):1412–1419. doi:10.1001/jama.295.12.1412
10. Chen J, Xu L, He Q, Wu S, Hu D, Lu K. Correlation between ideal cardiovascular health metrics and plasma hs-CRP levels in a North China population: one four-year follow-up study. Int J Gen Med. 2020;13:617–625. doi:10.2147/IJGM.S266602
11. Fuentes GC, Castañer O, Warnberg J, et al. Prospective association of physical activity and inflammatory biomarkers in older adults from the PREDIMED-Plus study with overweight or obesity and metabolic syndrome. Clin Nutr. 2020;39(10):3092–3098. doi:10.1016/j.clnu.2020.01.015
12. Li FH, Sun L, Zhu M, et al. Beneficial alterations in body composition, physical performance, oxidative stress, inflammatory markers, and adipocytokines induced by long-term high-intensity interval training in an aged rat model. Exp Gerontol. 2018;113:150–162. doi:10.1016/j.exger.2018.10.006
13. Rosado-Pérez J, Mendoza-Núñez VM. Relationship between aerobic capacity with oxidative stress and inflammation biomarkers in the blood of older Mexican urban-dwelling population. Dose Response. 2018;16(2):1559325818773000. doi:10.1177/1559325818773000
14. Blumenthal JA, Smith PJ, Mabe S, et al. Lifestyle and neurocognition in older adults with cardiovascular risk factors and cognitive impairment. Psychosom Med. 2017;79(6):719–727. doi:10.1097/PSY.0000000000000474
15. Singh M, Benencia F. Inflammatory processes in obesity: focus on endothelial dysfunction and the role of adipokines as inflammatory mediators. Int Rev Immunol. 2019;38(4):157–171. doi:10.1080/08830185.2019.1638921
16. Jamurtas AZ, Stavropoulos-Kalinoglou A, Koutsias S, Koutedakis Y, Fatouros I. Adiponectin, resistin, and visfatin in childhood obesity and exercise. Pediatr Exerc Sci. 2015;27(4):454–462. doi:10.1123/pes.2014-0072
17. Owczarek AJ, Olszanecka-Glinianowicz M, Kocełak P, et al. The relationship between circulating visfatin/nicotinamide phosphoribosyltransferase, obesity, inflammation and lipids profile in elderly population, determined by structural equation modeling. Scand J Clin Lab Invest. 2016;76(8):632–640. doi:10.1080/00365513.2016.1230884
18. Pham D-V, Park P-H. Recent insights on modulation of inflammasomes by adipokines: a critical event for the pathogenesis of obesity and metabolism-associated diseases. Arch. Pharmacal Res. 2020;43(10):997–1016. doi:10.1007/s12272-020-01274-7
19. Dakroub A, An S, Younis N, et al. Visfatin: a possible role in cardiovasculo-metabolic disorders. Cells. 2020;9(11):2444. doi:10.3390/cells9112444
20. Muller K. Statistical power analysis for the behavioral sciences. Technometrics. 1989;31(4):499–500. doi:10.1080/00401706.1989.10488618
21. Gauss T, Ageron FX, Devaud ML, et al. Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. 2019;154(12):1117–1124. doi:10.1001/jamasurg.2019.3475
22. Correll J, Mellinger C, McClelland GH, Judd CM. Avoid Cohen’s ‘Small’, ‘Medium’, and ‘Large’ for power analysis. Trends Cognit Sci. 2020;24(3):200–207. doi:10.1016/j.tics.2019.12.009
23. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New Jersey: L. Erlbaum Associates; 1988.
24. Cavar M, Marsic T, Corluka M, et al. Effects of 6 weeks of different high-intensity interval and moderate continuous training on aerobic and anaerobic performance. J Strength Cond Res. 2019;33(1):44–56. doi:10.1519/JSC.0000000000002798
25. Unamuno X, Gómez-Ambrosi J, Ramírez B, et al. Dermatopontin, A novel adipokine promoting adipose tissue extracellular matrix remodelling and inflammation in obesity. J Clin Med. 2020;9(4):1069. doi:10.3390/jcm9041069
26. Porter Starr KN, Orenduff M, McDonald SR, et al. Influence of weight reduction and enhanced protein intake on biomarkers of inflammation in older adults with obesity. J Nutr Gerontol Geriatr. 2019;38(1):33–49. doi:10.1080/21551197.2018.1564200
27. Yan P, Xu Y, Zhang Z, et al. Decreased plasma neuregulin 4 levels are associated with peripheral neuropathy in Chinese patients with newly diagnosed type 2 diabetes: a cross-sectional study. Cytokine. 2019;113:356–364. doi:10.1016/j.cyto.2018.10.007
28. Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162(16):1867–1872. doi:10.1001/archinte.162.16.1867
29. Tok Ö, Kişioğlu SV, Ersöz H, Kahveci B, Göktaş Z. Effects of increased physical activity and/or weight loss diet on serum myokine and adipokine levels in overweight adults with impaired glucose metabolism. J Diabetes Complications. 2021;35(5):107892. doi:10.1016/j.jdiacomp.2021.107892
30. Ghanbari-Niaki A, Saghebjoo M, Soltani R, Kirwan JP. Plasma visfatin is increased after high-intensity exercise. Ann Nutr Metab. 2010;57(1):3–8. doi:10.1159/000313936
31. Tremblay M. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi:10.1139/h2012-124
32. Viir R, Veraksits A. Discussion of “letter to the editor: standardized use of the terms sedentary and sedentary behaviours” - sitting and reclining are different states. Appl Physiol Nutr Metab. 2012;37(6):1256–1257. doi:10.1139/h2012-123
33. Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8(11):e80000. doi:10.1371/journal.pone.0080000
34. Boyle LJ, Credeur DP, Jenkins NT, et al. Impact of reduced daily physical activity on conduit artery flow-mediated dilation and circulating endothelial microparticles. J Appl Physiol (1985). 2013;115(10):1519–1525. doi:10.1152/japplphysiol.00837.2013
35. Narici M, De Vito G, Franchi M, et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur J Sport Sci. 2020;21:1–22.
36. Joyner MJ, Green DJ. Exercise protects the cardiovascular system: effects beyond traditional risk factors. J Physiol. 2009;587(Pt 23):5551–5558. doi:10.1113/jphysiol.2009.179432
37. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793–801. doi:10.1056/NEJMoa011858
38. Chen CY, Liao YH, Chou CC, Sung YC, Tsai SC. Initial systemic inflammatory state perturbs exercise training adaptations in elite Taekwondo athletes. PLoS One. 2017;12(4):e0176140. doi:10.1371/journal.pone.0176140
39. Dirks ML, Miotto PM, Goossens GH, et al. Short-term bed rest-induced insulin resistance cannot be explained by increased mitochondrial H2O2 emission. J Physiol. 2020;598(1):123–137. doi:10.1113/JP278920
40. Butts B, Butler J, Dunbar SB, Corwin EJ, Gary RA. ASC Methylation and Interleukin-1β are associated with aerobic capacity in heart failure. Med Sci Sports Exerc. 2017;49(6):1072–1078. doi:10.1249/MSS.0000000000001200
41. Cordingley DM, Cornish SM, Candow DG. Anti-inflammatory and anti-catabolic effects of creatine supplementation: a brief review. Nutrients. 2022;14(3):544. doi:10.3390/nu14030544
42. Do Nascimento DM, Machado KC, Bock PM, et al. Functional training improves peak oxygen consumption and quality of life of individuals with heart failure: a randomized clinical trial. BMC Cardiovasc Disord. 2023;23(1):381. doi:10.1186/s12872-023-03404-7
43. Derosa G, Catena G, Gaudio G, D’Angelo A, Maffioli P. Adipose tissue dysfunction and metabolic disorders: is it possible to predict who will develop type 2 diabetes mellitus? Role of markErs in the progreSsion of dIabeteS in obese paTIeNts (The RESISTIN trial). Cytokine. 2020;127:154947. doi:10.1016/j.cyto.2019.154947
44. Lee YH, Bae SC. Circulating adiponectin and visfatin levels in rheumatoid arthritis and their correlation with disease activity: a meta-analysis. Int J Rheum Dis. 2018;21(3):664–672. doi:10.1111/1756-185X.13038
45. Fain JN, Sacks HS, Buehrer B, et al. Identification of omentin mRNA in human epicardial adipose tissue: comparison to omentin in subcutaneous, internal mammary artery periadventitial and visceral abdominal depots. Int J Obes Lond. 2008;32(5):810–815. doi:10.1038/sj.ijo.0803790
46. Kim HJ, Park SY, Choi YJ, Han SJ, Lee KW, Kim DJ. Differential significance of plasma visfatin concentrations according to adiposity in children and adolescents. Horm Res Paediatr. 2013;79(4):208–213. doi:10.1159/000348848
47. Samal B, Sun Y, Stearns G, Xie C, Suggs S, McNiece I. Cloning and characterization of the cDNA encoding a novel human pre-B-cell colony-enhancing factor. Mol Cell Biol. 1994;14(2):1431. doi:10.1128/mcb.14.2.1431-1437.1994
48. Fukuhara A, Matsuda M, Nishizawa M, et al. Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science. 2005;307(5708):426–430. doi:10.1126/science.1097243
49. Heo YJ, Choi SE, Jeon JY, et al. Visfatin induces inflammation and insulin resistance via the NF-κB and STAT3 signaling pathways in hepatocytes. J Diabetes Res. 2019;2019:4021623. doi:10.1155/2019/4021623
50. Zhu Q, Scherer PE. Immunologic and endocrine functions of adipose tissue: implications for kidney disease. Nat Rev Nephrol. 2018;14(2):105–120. doi:10.1038/nrneph.2017.157
51. Katsogiannos P, Kamble PG, Pereira MJ, et al. Changes in circulating cytokines and adipokines after RYGB in patients with and without type 2 diabetes. Obesity (Silver Spring). 2021;29(3):535–542. doi:10.1002/oby.23093
52. Karbaschian Z, Hosseinzadeh-Attar MJ, Giahi L, et al. Portal and systemic levels of visfatin in morbidly obese subjects undergoing bariatric surgery. Endocrine. 2013;44(1):114–118. doi:10.1007/s12020-012-9821-x
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


