Back to Journals » Journal of Pain Research » Volume 18
Efficacy and Temporal Dynamics of Genicular Nerve Block in Primary and Secondary Knee Osteoarthritis for Pain and Function: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Authors Li Z , Bai Y , Liu C, Gu Y
Received 11 February 2025
Accepted for publication 10 June 2025
Published 17 June 2025 Volume 2025:18 Pages 3037—3048
DOI https://doi.org/10.2147/JPR.S518315
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor King Hei Stanley Lam
Ziqing Li,1 Yang Bai,2 Cheng Liu,2 Yanglin Gu1
1Nanjing Medical University Affiliated Wuxi No.2 People’s Hospital, Jiangsu, People’s Republic of China; 2Jiangnan University Affiliated Wuxi No.2 People’s Hospital, Jiangsu, People’s Republic of China
Correspondence: Yanglin Gu, Nanjing Medical University Affiliated Wuxi No.2 People’s Hospital, Email [email protected]
Purpose: Genicular nerve block (GNB) has emerged as a promising intervention for knee osteoarthritis (KOA), yet its comparative efficacy remains incompletely understood. The purpose of this review was to assess the effectiveness of GNB in reducing pain and improving function for primary or secondary KOA.
Methods: We conducted systematic searches of PubMed, Web of Science, and Embase up to October 9, 2024, for randomized controlled trials comparing GNB with other therapies. The data were analyzed using Review Manager (RevMan) 5.4, and study quality was assessed using the Cochrane risk of bias tool.
Results: This study included six RCTs involving a total of 420 participants. Results revealed that GNB significantly reduced pain (SMD = 1.00, 95% CI: 0.48– 1.52, p=0.0002) and improved function (SMD = 1.07, 95% CI: 0.37– 1.77, p=0.003) compared to other interventions. Subgroup analyses showed that GNB provided better pain relief at 2 weeks (SMD=1.21; 95% CI: 0.09– 2.33; P=0.03) and greater functional improvement at 12 weeks (SMD=1.13; 95% CI: 0.10– 2.16; P=0.03).
Conclusion: This review suggested GNB as an effective intervention for KOA management, with distinct temporal patterns for pain relief and functional improvement.
Keywords: knee pain, genicular nerve block, knee osteoarthritis, meta-analysis
Introduction
Osteoarthritis (OA) represents one of the most significant challenges in global musculoskeletal health, ranking as the 11th leading cause of disability worldwide in the 2010 Global Burden of Disease Study.1 As populations continue to age, its burden on healthcare systems intensifies exponentially. Knee osteoarthritis (KOA), a predominant manifestation of OA, not only significantly impairs individual mobility and quality of life but also imposes substantial socioeconomic costs across healthcare systems globally.2
The hallmark symptom of KOA - chronic knee pain - precipitates a cascade of adverse effects, including functional limitations, sleep disturbances, fatigue, psychological distress and progressive loss of independence.3 Current therapeutic approaches for KOA encompass both conservative and surgical interventions. Conservative management includes patient education, structured exercise programs, weight management, and pharmacological interventions such as paracetamol, NSAIDs, corticosteroids, botulinum neurotoxin, hyaluronic acid supplementation and laser therapy.4–7 However, when conservative management proves inadequate, a significant proportion of patients ultimately require total knee arthroplasty.8 The efficacy of conventional conservative therapies in achieving sustained pain relief and functional improvement remains controversial, while total knee arthroplasty carries inherent surgical risks and substantial financial burden.9
Given these limitations, genicular nerve block (GNB), a minimally invasive procedure, has shown considerable promise in providing durable pain relief and functional improvement in KOA patients, positioning it as a potentially superior alternative.
GNB functions through precise interruption of pain signal transmission via selective blockade of the superior medial (SMGN), superior lateral (SLGN), and inferior medial genicular nerves (IMGN).10 Growing clinical evidence supports its efficacy in alleviating pain and enhancing function in KOA patients.11 Furthermore, GNB has demonstrated utility as a diagnostic tool preceding radiofrequency ablation procedures,12,13 and has shown effectiveness in reducing post-operative pain and opioid consumption following total knee arthroplasty.13–16
While previous meta-analyses have examined GNB in KOA management,17 their scope was primarily limited to pre-post intervention comparisons due to the paucity of comparative studies. To address these limitations, this study conducted a comprehensive review and meta-analysis of recent RCTs to evaluate the comparative efficacy of GNB in managing primary and secondary KOA.
Methods
Study Design
This systematic review and meta-analysis was designed to evaluate the comparative effectiveness of GNB in managing KOA. The study protocol was developed in accordance with the methodological standards outlined in the Cochrane Handbook for Systematic Reviews of Interventions and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines.18 To ensure methodological transparency and minimize reporting bias, the protocol was prospectively registered in PROSPERO (No.: CRD42024603966).
Search Strategy
YB and CL conducted a comprehensive search of PubMed, Web of Science (WOS), and Embase databases until October 9, 2024. Search terms included combinations of “genicular nerve block” with “osteoarthritis” or “arthritis” without language restrictions to ensure inclusivity. No language restrictions were applied during the initial search to maximize coverage. Reference lists of included studies and relevant review articles were manually screened to identify additional eligible studies. The detailed search strategy, including specific terms and combinations, is documented in Additional Table 1.
Inclusion and Exclusion Criteria
Inclusion criteria were: (1) randomized controlled trials (RCTs) comparing GNB with other therapies for primary or secondary KOA; (2) reporting pain and function outcomes with a minimum follow-up of 2 months; (3) studies published in English with full-text availability.
Exclusion criteria included: (1) observational or non-RCT studies; (2) interventions combined with other treatments; (3) studies with insufficient data for meta-analysis; (4) unpublished or non-peer-reviewed articles.
Data Extraction and Quality Assessment
Two authors independently extracted data using a predefined template, including study characteristics (author, year, country, disease, intervention, control group), baseline patient demographics, outcome measures, follow-up periods). The outcome measure of interest in this study encompassed Visual Analog Scale (VAS), Western Ontario and McMaster University’s Index of Arthritis (WOMAC), Lysholm score and Oxford knee score (OKS) at 2, 4, 8, and 12 weeks. Secondary outcomes was adverse effect. A third reviewer reviewed included literature and performed verification to ensure and minimize errors during the extraction stage.
Risk of bias for each included study was assessed independently by two reviewers using the Cochrane Risk of Bias 2.0 tool. Domains evaluated included randomization process, allocation concealment, blinding of participants and outcome assessors, incomplete outcome data, and selective reporting. Studies with high risk of bias in more than two domains were considered low quality.
Statistical Analysis
Meta-analyses were conducted using Review Manager (RevMan) software version 5.4. For continuous outcomes, standardized mean differences (SMD) and 95% confidence intervals (CI) were calculated. Heterogeneity was assessed using the I² statistic, with thresholds of 25%, 50%, and 75% representing low, moderate, and high heterogeneity, respectively. A random-effects model was applied for I² > 50%, while a fixed-effects model was used otherwise. Subgroup analyses were performed based on follow-up durations (eg, 2, 4, 8, and 12 weeks) to explore potential sources of heterogeneity. Sensitivity analyses were conducted by sequentially excluding each study to evaluate the robustness of results. Publication bias was not formally assessed due to the limited number of studies (<10 per pooled analysis).19 Alternative approaches such as Egger’s test or trim-and-fill were considered, but their applicability was limited in this context. Thus, any interpretation should be cautious.
Result
Search Results
Our systematic literature search initially identified 174 potentially relevant articles across the selected databases (Figure 1). After removing 44 duplicate records, we screened the titles and abstracts of 130 articles. Of these, 111 articles were excluded as they did not meet our predefined eligibility criteria, leaving 19 articles for full-text review. Following detailed assessment of the full texts, 13 articles were further excluded for the following reasons: non-randomized study design (n=5), inadequate follow-up duration (n=3), combined interventions (n=3), and insufficient outcome data (n=2). Ultimately, six randomized controlled trials meeting all inclusion criteria were included in our meta-analysis. The included studies comprised a total of 420 participants and represented diverse geographical locations. Four studies focused on KOA,20–23 while two studies involved rheumatoid arthritis (RA),24 and juvenile idiopathic arthritis (JIA),25 respectively (Table 1).
 |
Table 1 General characteristics of the included studies |
 |
Figure 1 Flowchart. PRISMA flowchart presenting the summary of searches carried out in the literature. GNB indicates Genicular nerve block. Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.18 |
Influence on Pain Outcomes
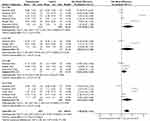
The pooled analysis of six studies using VAS demonstrated that GNB achieved superior pain relief compared to control treatments, with a standardized mean difference (SMD) of 1.00 (95% CI: 0.48–1.52, p=0.0002; Figure 2). Given the substantial heterogeneity observed across studies (I² > 50%), conducted subgroup analyses based on follow-up periods to better understand the temporal pattern of pain relief.
The temporal analysis demonstrated that GNB provided maximal pain relief at 2 weeks post-intervention (SMD=1.21; 95% CI: 0.09–2.33; p=0.03; Figure 2), although the effects were not statistically significant at longer follow-up intervals (4, 8, and 12 weeks; Table 2).
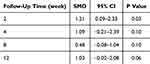 |
Table 2 Effects of Subgroup Analysis of Pain by Follow-up Time |
Notably, when we excluded the study by Ahlawat et al,23 which compared GNB with saphenous nerve block, the overall treatment effect became more pronounced (SMD=1.37; 95% CI: 0.78–1.96; P<0.00001; Figure 3) and significant differences were observed at all follow-up times (Table 3). This sensitivity analysis not only demonstrated the robustness of our findings but also revealed that the choice of comparator intervention might influence the relative effectiveness of GNB.
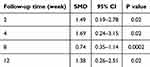 |
Table 3 Effects of Subgroup Analysis of Pain by Follow-up Time with Removing One Study |
Function Outcomes
Functional improvement was systematically evaluated across all six included studies using validated assessment tools. Three studies used WOMAC, two studies used Lysholm score, and one studies used OKS. Due to the varied assessment timelines across studies, with only two studies reporting outcomes at 4 and 8 weeks, we focused our analysis on the 2-week and 12-week time points to ensure robust statistical comparison.
Notably, the functional improvements were most substantial at 12 weeks post-treatment (SMD=1.13; 95% CI: 0.10–2.16; p=0.03; Figure 4). In contrast, at 2 weeks, the improvements were not statistically significant (SMD=1.02; 95% CI: −0.03 to 2.08; p=0.06; Figure 4), suggesting the benefits of GNB in function might develop more fully over time.
Risk of Bias and Sensitivity Analysis
Details of the risk of bias assessment for the six studies can be obtained in Figures 5 and 6. The assessment identified potential limitations in two studies regarding randomization procedures and allocation concealment documentation.20,23 Additionally, two studies were classified as having a higher risk of bias due to their single-blind design.21,23 The remaining four studies demonstrated low risk of bias across all assessed domains. To evaluate the robustness of our findings, we performed a thorough sensitivity analysis by sequentially excluding each study from the meta-analysis. The consistency of our findings across these methodological assessments and sensitivity analyses provides strong support for the validity of our conclusions, despite the identified limitations in some included studies.
 |
Figure 5 Summary in risk of bias. Risk of bias graph of included studies (Green, Low Risk of Bias; Yellow, Unclear Risk of Bias; Red, High Risk of Bias). |
 |
Figure 6 Summary in risk of bias. Risk of bias graph of included studies (Green, Low Risk of Bias; Yellow, Unclear Risk of Bias; Red, High Risk of Bias). |
Discussion
Our comprehensive meta-analysis demonstrates that GNB offers significant improvements in pain and functional outcomes for KOA patients when compared to other therapeutic interventions. Subgroup analyses reveals a distinct pattern in the therapeutic response to GNB. The intervention demonstrates robust immediate efficacy, with peak pain relief occurring within the first two weeks post-treatment. This initial response, while significant, shows a gradual diminution over time, consistent with the known pharmacological properties of local anesthetics. While the observed pattern of functional improvement follows a different trajectory, with patients experiencing progressive enhancement in functional capabilities over time.
Prior meta-analyses conducted by Vilchez-Cavazos et al17 included five trials, three used GNB in both intervention and control groups, one combined GNB with intra-articular steroids, and only one provided a true comparison with standard corticosteroid injection. Thus their analysis could only examine pre- and post-intervention changes. Our study addresses this critical gap by incorporating direct comparisons between GNB and diverse therapeutic alternatives.
The individualized approach to GNB administration and its technical considerations warrant detailed examination. In a notable study,23 researchers implemented a responsive treatment protocol where repeat blocks were administered when pain relief was inadequate (VAS>4). Although the GNB group required more frequent repeat interventions, this approach yielded superior long-term pain relief and functional improvement compared to other trials in our analysis. This indicated that repeated blocks may provide longer-lasting relief or better outcomes for patients who experience insufficient pain relief from a single block, possibly due to variability in the response to the initial treatment.
Technical aspects of GNB administration have been extensively investigated. Kim et al conducted a trial to compare the efficacy of GNB with or without corticosteroids.26 Their findings revealed the VAS scores were significantly lower at both 2 (P < 0.001) and 4 (P < 0.001) weeks and mean OKS decreased more significantly at 4 weeks after GNB with corticosteroids treatment, however, this significant difference could only sustained for 1–2 weeks. Considering that corticosteroids may cause local or systemic adverse effects, the addition of corticosteroid therapy might not provide significant benefits to GNB with a local anesthetic alone. A subsequent study,27 comparing imaging guidance methods found that while ultrasound and fluoroscopy - guided techniques demonstrated comparable effectiveness, ultrasound guidance offered the distinct advantage of real-time visualization of soft tissues (nerves, muscles, vessels, etc), potentially enhancing procedural safety and precision. In addition, neither the patients nor clinicians are exposed to radiation during an ultrasound-guided procedure.
The evolution of GNB techniques has been informed by both anatomical studies and clinical trials. Several cadaveric studies have established reliable anatomical landmarks for GNB administration,28–30 demonstrating the feasibility of landmark-guided approaches. However, comparative studies have increasingly favored ultrasound guidance. While Cankurtaran et al found both ultrasound - guided and blind techniques were effective in relieving pain and improving muscle strength, however, GNB with ultrasound guidance could help to detect concomitant pathology and significantly relieve pain during the injection (P = 0.01).10 A subsequent retrospective cohort study,31 reported that ultrasound-guided GNB was more advantageous in reducing WOMAC and Numeric Rating Scale (NRS) scores compared with blind technique, the difference achieving statistical significance at six weeks after treatment (p =0.026). The integration of ultrasound guidance with percutaneous peripheral nerve stimulation, as described by Ferreira-Dos-Santos may further enhance the precision of nerve identification and improve procedural outcomes.32 Ghai et al compared ultrasound guided pulsed radiofrequency (PRF) of genicular nerve with GNB,33 result showed that both PRF and GNB provided comparable pain relief. However, compared to GNB, geniculate nerve PRF required more time and equipment.
Fonkoue et al compared classical anatomical targets for GNB (SMGN, SLGN, IMGN) with revised targets, including the fibular nerve and infrapatellar branch of the saphenous nerve.34 While the revised targets showed greater reduction in NRS mean score and higher proportion of patients achieving more than 50% knee pain reduction, however, these differences were statistically significant only at 1-hour post intervention. Kesikburun et al found that blocking only the SMGN and IMGN was sufficient in most KOA patients,35 as the medial compartment is typically the most affected in KOA.36 And it has been suggested that only these two knee nerves are involved in clinically significant knee pain associated with medial compartment KOA.35
While GNB is generally well-tolerated, some studies report adverse effects, including local pain, hypoesthesia, and swelling. These side effects, although mild and self-limiting in most cases, should be considered when deciding on GNB as a treatment option.24,25,37 Interestingly, no adverse effects were observed in other studies, highlighting the variability in patient responses and the need for careful patient monitoring.21,22,33
Implications for Clinical Practice
As a minimally invasive operation, GNB not only supports a non-pharmacological approach to pain management but also reduces dependence on painkillers that can cause side effects. Due to the simplicity, GNB can reduce the financial pressure on patients in poor areas and greatly improve the quality of KOA management in hospitals with backward medical conditions. In addition, given its immediate analgesic and long-term functional improvement effects, GNB can be a powerful alternative therapy for patients who cannot tolerate surgery.
The temporal pattern of GNB treatment response suggests that regular maintenance interventions may be required by clinical practitioners to sustain therapeutic benefits of pain relief. In the functional management of KOA, GNB can be used as an adjunctive therapy to other therapies such as hyaluronic acid injections, platelet rich plasma injections to enhance efficacy of functional improvement.
Limitations
Our study’s limitations warrant careful consideration when interpreting the findings. The relatively modest scope of our analysis, encompassing six studies with a total of 420 participants, potentially constrains the broad applicability of our conclusions. This limitation in sample size, while sufficient for identifying significant treatment effects, may not fully capture the diversity of patient responses across different clinical contexts. The inconsistent reporting of adverse events across the included studies precluded a comprehensive safety assessment, leaving important questions about risk profiles incompletely addressed. Methodological heterogeneity presented another significant challenge. The variations in patient characteristics, treatment protocols, and operator expertise across studies introduced considerable variability in our findings. While our statistical approaches accounted for this heterogeneity, it underscores the need for standardization in future research protocols. Additionally, the overall quality of available evidence, though adequate for preliminary conclusions, highlights the necessity for more rigorous, large-scale clinical trials to definitively establish the role of GNB in KOA management.
Conclusion
This review indicates that GNB can reduce pain and improve function in patients with KOA compared with other interventions. The treatment exhibits unique temporal patterns, with optimal pain relief occurring within two weeks post-intervention and peak functional improvements at 12 weeks. Future research should consider exploring the effect of repeat blocks on patients with KOA compared with other therapies, while expanding the sample size and conducting longer follow-up periods.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Wuxi Municipal “Double Hundred” Young and Middle-aged Top Talent Training Fund for Medicine and Health (BJ2020037).
Disclosure
The authors declare no conflict of interest.
References
1. Cross M, Smith E, Hoy D, et al. The global burden of Hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi:10.1136/annrheumdis-2013-204763
2. Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107(9):152–162. doi:10.3238/arztebl.2010.0152
3. Hawker GA. Osteoarthritis is a serious disease. Clin Exp Rheumatol. 2019;37 Suppl 120(5):3–6.
4. Pesare E, Vicenti G, Kon E, et al. Italian orthopaedic and traumatology society (SIOT) position statement on the non-surgical management of knee osteoarthritis. J Orthop Traumatol. 2023;24(1):47. doi:10.1186/s10195-023-00729-z
5. Kan HS, Chan PK, Chiu KY, et al. Non-surgical treatment of knee osteoarthritis. Hong Kong Med J. 2019;25(2):127–133. doi:10.12809/hkmj187600
6. Poenaru D, Sandulescu MI, Cinteza D. Pain modulation in chronic musculoskeletal disorders: botulinum toxin, a descriptive analysis. Biomedicines. 2023;11(7):1888. doi:10.3390/biomedicines11071888
7. Poenaru D, Sandulescu MI, Potcovaru CG, et al. High-intensity laser therapy in pain management of knee osteoarthritis. Biomedicines. 2024;12(8):1679. doi:10.3390/biomedicines12081679
8. Gress K, Charipova K, An D, et al. Treatment recommendations for chronic knee osteoarthritis. Best Pract Res Clin Anaesthesiol. 2020;34(3):369–382. doi:10.1016/j.bpa.2020.06.006
9. Moldovan F, Gligor A, Moldovan L, et al. An Investigation for future practice of elective hip and knee arthroplasties during COVID-19 in Romania. Medicina. 2023;59(2):314. doi:10.3390/medicina59020314
10. Cankurtaran D, Karaahmet OZ, Yildiz SY, et al. Comparing the effectiveness of ultrasound guided versus blind genicular nerve block on pain, muscle strength with isokinetic device, physical function and quality of life in chronic knee osteoarthritis: a prospective randomized controlled study. Korean J Pain. 2020;33(3):258–266. doi:10.3344/kjp.2020.33.3.258
11. Lebleu J, Fonkoue L, Bandolo E, et al. Lower limb kinematics improvement after genicular nerve blockade in patients with knee osteoarthritis: a milestone study using inertial sensors. BMC Musculoskelet Disord. 2020;21(1):822. doi:10.1186/s12891-020-03836-8
12. Yildiz G, Perdecioglu GRG, Yuruk D, et al. Comparison of the efficacy of genicular nerve phenol neurolysis and radiofrequency ablation for pain management in patients with knee osteoarthritis. Korean J Pain. 2023;36(4):450–457. doi:10.3344/kjp.23200
13. Wong PK, Kokabi N, Guo Y, et al. Safety and efficacy comparison of three- vs four-needle technique in the management of moderate to severe osteoarthritis of the knee using cooled radiofrequency ablation. Skeletal Radiol. 2021;50(4):739–750. doi:10.1007/s00256-020-03619-1
14. Pietrantoni P, Cuñat T, Nuevo-Gayoso M, et al. Ultrasound-guided genicular nerves block: an analgesic alternative to local infiltration analgesia for total knee arthroplasty: a noninferiority, matched cohort study. Eur J Anaesthesiol. 2021;38(Suppl 2):S130–s137. doi:10.1097/EJA.0000000000001546
15. Rambhia M, Chen A, Kumar AH, et al. Ultrasound-guided genicular nerve blocks following total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2021;46(10):862–866. doi:10.1136/rapm-2021-102667
16. Eid GM, Shaban SES, Mostafa TA. Comparison of ultrasound-guided genicular nerve block and knee periarticular infiltration for postoperative pain and functional outcomes in knee arthroplasty - A randomised trial. Indian J Anaesth. 2023;67(10):885–892. doi:10.4103/ija.ija_449_23
17. Vilchez-Cavazos F, Gamboa Alonso AA, Simental-Mendía M, et al. Genicular nerve block for knee osteoarthritis: a systematic review and meta-analysis of randomized clinical trials. Clin J Pain. 2024;40(10):618–624. doi:10.1097/AJP.0000000000001240
18. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
19. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10(10):Ed000142. doi:10.1002/14651858.ED000142
20. Ragab AR, Hegab S, Elnemr R, et al. Intra-articular corticosteroid injection and genicular nerve block under ultrasound guidance in pain control of knee osteoarthritis. Egypt J Radiol Nucl Med. 2021;52(1). doi:10.1186/s43055-021-00577-z.
21. Güler T, Yurdakul FG, Önder ME, et al. Ultrasound-guided genicular nerve block versus physical therapy for chronic knee osteoarthritis: a prospective randomised study. Rheumatol Int. 2022;42(4):591–600. doi:10.1007/s00296-022-05101-8
22. Shanahan EM, Robinson L, Lyne S, et al. Genicular nerve block for pain management in patients with knee osteoarthritis: a randomized placebo-controlled trial. Arthritis Rheumatol. 2023;75(2):201–209. doi:10.1002/art.42384
23. Ahlawat MS, Taxak S, Dahiya A, Zokarkar A, Laller A, Yadav T. A study to compare efficacy of ultrasound guided saphenous versus genicular nerve block in osteoarthritis knee pain. Int J Scientific Res Dental Med Sci. 2024;6(2):60–68.
24. Elsaman AM, Maaty A, Hamed A. Genicular nerve block in rheumatoid arthritis: a randomized clinical trial. Clin Rheumatol. 2021;40(11):4501–4509. doi:10.1007/s10067-021-05821-5
25. Radwan A, Ohrndorf S, Aly H, et al. Genicular nerve block in juvenile idiopathic arthritis: a randomized clinical trial. Clin Rheumatol. 2023;42(3):879–888. doi:10.1007/s10067-022-06389-4
26. Kim DH, Choi -S-S, Yoon S-H, et al. Ultrasound-guided genicular nerve block for knee osteoarthritis: a double-blind, randomized controlled trial of local anesthetic alone or in combination with corticosteroid. Pain Physician. 2018;21(1):41–52.
27. Kim DH, Lee M-S, Lee S, et al. A prospective randomized comparison of the efficacy of ultrasound- vs fluoroscopy-guided genicular nerve block for chronic knee osteoarthritis. Pain Physician. 2019;22(2):139–146.
28. Kim J, Kim JY, Shin HY, et al. Investigation of the existence of and a block technique for the inferior lateral genicular nerve: cadaveric study. Korean J Pain. 2023;36(3):328–334. doi:10.3344/kjp.23112
29. Yasar E, Kesikburun S, Kılıç C, et al. Accuracy of ultrasound-guided genicular nerve block: a cadaveric study. Pain Physician. 2015;18(5):E899–904.
30. Sutaria RG, Lee SW, Kim SY, et al. Localization of the lateral retinacular nerve for diagnostic and therapeutic nerve block for lateral knee pain: a cadaveric study. Pm r. 2017;9(2):149–153. doi:10.1016/j.pmrj.2016.06.017
31. Singh S, Singh S, Nachimuthu M, et al. Effectiveness of ultrasound-guided versus anatomical landmark-guided genicular nerve block to treat chronic knee osteoarthritis: a retrospective cohort study. Oman Med J. 2023;38(5):e550. doi:10.5001/omj.2023.103
32. Ferreira-Dos-Santos G, Hurdle M-FB, Gupta S, et al. Revisiting the genicular nerve block: an up-to-date guide utilizing ultrasound guidance and peripheral nerve stimulation - anatomy description and technique standardization. Pain Physician. 2021;24(2):E177–e183.
33. Ghai B, Kumar M, Makkar JK, et al. Comparison of ultrasound guided pulsed radiofrequency of genicular nerve with local anesthetic and steroid block for management of osteoarthritis knee pain. Korean J Pain. 2022;35(2):183–190. doi:10.3344/kjp.2022.35.2.183
34. Fonkoue L, Steyaert A, Kouame J-EK, et al. A comparison of genicular nerve blockade with corticosteroids using either classical anatomical targets vs revised targets for pain and function in knee osteoarthritis: a double-blind, randomized controlled trial. Pain Med. 2021;22(5):1116–1126. doi:10.1093/pm/pnab014
35. Kesikburun S, Yasar E, Uran A, Adiguzel E, Yilmaz B. Ultrasound-guided genicular nerve pulsed radiofrequency treatment for painful knee osteoarthritis: a preliminary report. Pain Physician. 2016;19(5):E751–9. doi:10.36076/ppj/2019.19.E751
36. Wise BL, Niu J, Yang M, et al. Patterns of compartment involvement in tibiofemoral osteoarthritis in men and women and in whites and African Americans. Arthritis Care Res. 2012;64(6):847–852. doi:10.1002/acr.21606
37. Elashmawy MM, Shabana AAH, Elsaid TO, et al. Ultrasound-guided genicular nerve block versus alcoholic neurolysis for treatment of advanced knee osteoarthritis patients. Egyptian Rheumatol. 2022;44(4):307–311. doi:10.1016/j.ejr.2022.04.002
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Influence of Knee Osteoarthritis Severity, Knee Pain, and Depression on Physical Function: A Cross-Sectional Study
Sonobe T, Otani K, Sekiguchi M, Otoshi K, Nikaido T, Konno S, Matsumoto Y
Clinical Interventions in Aging 2024, 19:1653-1662
Published Date: 5 October 2024
Effectiveness of Combination of Thunder Fire Moxibustion with Other Forms of Traditional Chinese Medicine for Osteoarthritis Knee: A Meta-Analysis
Wei W, Qin Y, Lin J
Journal of Pain Research 2025, 18:3087-3099
Published Date: 21 June 2025