Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Enhanced Recovery After Surgery (ERAS) Rehabilitation Protocols Significantly Improve Postoperative Pain and Recovery in Ankle Fracture Surgery
Authors Yang Q, Yang H, Zhao J, Ren L
Received 16 January 2025
Accepted for publication 20 April 2025
Published 5 June 2025 Volume 2025:21 Pages 841—850
DOI https://doi.org/10.2147/TCRM.S517790
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Qian Yang, Huan Yang, JunYan Zhao, Lei Ren
Dazhou Central Hospital, Dazhou, Sichuan, 635000, People’s Republic of China
Correspondence: Lei Ren, Dazhou Central Hospital, No. 61 Tongchuan North Road, Tongchuan District, Dazhou, Sichuan, 635000, People’s Republic of China, Email [email protected]
Background: Enhanced Recovery After Surgery (ERAS) principles have gained widespread recognition for optimizing recovery across various surgical specialties. Effective management of postoperative pain plays a pivotal role in facilitating early rehabilitation and enhancing patient outcomes, particularly in ankle fracture surgery. This study investigated the effectiveness of rehabilitation therapies rooted in ERAS protocols in alleviating postoperative wound pain and improving recovery for patients undergoing ankle fracture surgery.
Methods: A total of 376 patients who underwent ankle fracture surgery between December 2022 and December 2023 were included in this retrospective analysis. Of these, 190 patients received ERAS-guided rehabilitation, while 186 underwent standard rehabilitation care. The ERAS program encompassed tailored interventions such as multimodal pain control, prompt mobilization, and personalized physical therapy regimens. Pain intensity was evaluated using the Visual Analog Scale (VAS) at 24 hours, 48 hours, and 7 days postoperatively. Additional metrics, including the duration of hospital stay, complication rates, and patient satisfaction, were also assessed.
Results: Patients in the ERAS group experienced significantly lower VAS scores than the standard care group at 24 hours (4.2 ± 1.1 vs 5.6 ± 1.4, P< 0.001), 48 hours (3.1 ± 0.9 vs 4.4 ± 1.2, P< 0.001), and 7 days post-surgery (2.0 ± 0.7 vs 3.1 ± 0.9, P< 0.001). Furthermore, those receiving ERAS care had a shorter average hospital stay (5.1 ± 1.6 days vs 6.7 ± 2.1 days, P< 0.001) and reported higher levels of satisfaction (92.1% vs 78.4%, P< 0.001). However, there were no statistically significant differences in overall complication rates between the two groups (3.7% vs 4.3%, P=0.712).
Conclusion: Rehabilitation therapies incorporating ERAS principles demonstrate substantial benefits in reducing postoperative wound pain and expediting recovery in ankle fracture surgery patients. These findings underscore the value of integrating ERAS-driven protocols into clinical practice to enhance patient experiences and postoperative outcomes.
Keywords: ankle fracture surgery, enhanced recovery after surgery ERAS, multimodal pain management, postoperative rehabilitation, patient satisfaction
Introduction
Ankle fracture surgery is a common orthopedic procedure that is crucial for restoring joint stability and function in trauma patients.1–3 Despite advancements in surgical techniques, postoperative wound pain remains a major challenge, often delaying recovery and negatively impacting patient outcomes. Efficient pain control plays a crucial role in facilitating early mobilization, minimizing complications, and ensuring successful recovery. Ankle injuries, particularly fractures, are common and often lead to significant biomechanical changes due to the disruption of joint stability and function. These injuries can result in chronic pain, instability, and difficulty performing activities of daily living. Rehabilitation plays a key role in restoring joint mobility, muscle strength, and proprioception. Techniques such as early mobilization, proprioceptive training, and strengthening exercises are commonly employed to restore function and reduce the risk of long-term complications like post-traumatic osteoarthritis. Originally designed for colorectal procedures, Enhanced Recovery After Surgery (ERAS) principles have been widely adopted in diverse surgical fields, including orthopedics, for their effectiveness in overcoming postoperative challenges and enhancing recovery outcomes. Despite advancements in surgical techniques, such as open reduction and internal fixation (ORIF) for ankle fractures, postoperative pain management remains a significant challenge. Early interventions, such as those incorporated in ERAS protocols, have shown promise in optimizing recovery through multimodal pain management and early rehabilitation, contributing to faster recovery and improved functional outcomes.4–8
ERAS principles adopt a comprehensive, multidisciplinary approach that integrates preoperative education, multimodal analgesia, early mobilization, and individualized rehabilitation plans.9–11 These strategies aim to minimize surgical stress, promote recovery, and enhance patient satisfaction. Existing evidence highlights the benefits of ERAS protocols in surgical care. For example, Ripollés-Melchor et al12 reported that ERAS protocols significantly reduced postoperative complications and shortened hospital stays in orthopedic surgeries, and improved adherence to ERAS plans was associated with fewer postoperative complications. Similarly, Ljungqvist and Kehlet emphasized that reducing surgical stress and systemic inflammation is a key factor in the success of ERAS,9 while early mobilization within ERAS protocols, as highlighted by Tazreean et al13 reduces the risk of postoperative complications, accelerates recovery, and improves pain management.
In the field of orthopedic surgery, the application of ERAS protocols in procedures such as ankle fracture repairs has shown promising prospects but remains underexplored. Li et al14 in a multicenter study comparing the outcomes of ERAS protocols with traditional pathways in patients with ankle fractures and distal radius fractures, demonstrated that ERAS-based perioperative programs are associated with higher satisfaction, reduced bed rest durations, and shorter hospital stays without increasing the incidence of complications or compromising functional outcomes. Additionally, Yao et al15 emphasized the short-term postoperative benefits of ERAS protocols in ankle fracture patients, noting improvements in healthcare quality and efficiency. While these studies provide valuable insights into the benefits of ERAS, few have specifically evaluated their impact on postoperative wound pain in ankle fracture surgeries.
The successful implementation of ERAS protocols largely depends on perioperative nursing care, which plays a critical role in promoting patient education, managing postoperative pain, and ensuring adherence to rehabilitation plans. Auyong et al suggested that individualized nursing interventions can optimize patient compliance with ERAS protocols, thereby improving clinical outcomes. However, inconsistent nursing practices and a lack of standardized protocols, as Ripollés-Melchor et al pointed out, may undermine the effectiveness of ERAS interventions, leading to variability in patient outcomes.
Despite the growing evidence supporting the application of ERAS in orthopedic care, a significant gap remains in tailored rehabilitation protocols for managing postoperative pain in ankle fracture surgeries. Bridging this gap is essential for refining pain management approaches and enhancing the recovery pathways for these patients. This study aims to evaluate the impact of ERAS-aligned rehabilitation therapies on postoperative wound pain in patients undergoing ankle fracture surgery. By assessing outcomes such as pain scores, hospital stays, and patient satisfaction, this research seeks to provide evidence-based insights into improving rehabilitation protocols and enhancing perioperative care in orthopedic surgery.
Materials and Methods
Patient Selection Study Design and Participants
This retrospective cohort study evaluated the impact of rehabilitation therapies aligned with Enhanced Recovery After Surgery (ERAS) principles on postoperative wound pain in patients undergoing ankle fracture surgery. Patients aged ≥18 who underwent ankle fracture surgery between December 2022 and December 2023 were included. Postoperative outcomes, including pain scores, mobilization milestones, complications, and patient satisfaction, were assessed during the first 7 days following surgery, which served as the short-term follow-up period. Data were collected from electronic medical records and verified independently by two researchers. Inclusion criteria were as follows: (1) Patients aged ≥18; (2) Underwent primary ankle fracture surgery. Exclusion criteria included: (1) Revision ankle fracture surgeries; (2) Significant comorbidities potentially influencing outcomes (eg, severe cardiovascular or renal diseases); (3) Refusal to participate in postoperative rehabilitation protocols. The study adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Dazhou Central Hospital. Written informed consent was obtained from all participants.
ERAS-Based Perioperative Nursing Interventions
Patients in the ERAS group received targeted rehabilitation interventions aligned with ERAS principles:
Preoperative Education
Preoperative education sessions were structured to provide patients with comprehensive information regarding their surgery and recovery. These sessions aimed to prepare patients psychologically and physically for the surgery and postoperative rehabilitation. The key components of the preoperative education included in Supplementary Table 1.
We implemented a multimodal analgesia protocol to manage postoperative pain. This approach combined several strategies:Regional Anesthesia: Nerve blocks were administered during surgery to target pain at its source; Non-Opioid Analgesics: Acetaminophen and NSAIDs were used routinely to control mild to moderate pain; Opioids: Opioids were used sparingly, only for breakthrough pain, to minimize the risk of opioid dependence and adverse effects; Early Mobilization: Mobilization was initiated within 24 hours of surgery, with patients engaging in structured physical therapy. This involved ankle pumps, early weight-bearing exercises, and progressive walking under the supervision of a physiotherapist.
The inclusion of early mobilization has been supported by numerous studies,16 including Tazreean et al13 which highlighted the role of early physical activity in reducing the risk of postoperative complications and accelerating recovery.
Nutritional Support
Nutritional support was an essential component of the ERAS protocol, emphasizing early postoperative nutrition. Protein-rich meals were introduced within 24 hours to support tissue healing and overall recovery. Nutritional education focused on the importance of balanced meals, including easily digestible options that promote wound healing and immune function.17
Monitoring and Complication Prevention
Nurses proactively monitored for complications, including infections and deep vein thrombosis (DVT). Preventive measures, such as compression stockings and anticoagulants, were implemented according to protocol.
Standard Care and Differences Between ERAS and Standard Care Protocol
The standard care group received conventional postoperative care, which included:General Pain Management: Primarily opioid-based analgesia, with minimal use of non-opioid analgesics; Basic Mobilization: Mobilization commenced on the second or third postoperative day, depending on the patient’s condition. Exercise instructions were limited to ankle pumps performed once daily without progression or individualization; Dietary Guidelines: Nutritional support was provided after the return of bowel function, and patients were encouraged to consume standard meals.
The key difference between the ERAS and standard care groups was the tailored and proactive rehabilitation plan in the ERAS group, which included:Personalized Exercises: The ERAS group followed a customized rehabilitation program, including early ankle range-of-motion exercises, progressive weight-bearing activities, and mobility training within 24 hours post-surgery; Early and Structured Mobilization: ERAS patients began walking with assistance and participated in supervised physiotherapy sessions from the first day after surgery. In contrast, the standard care group followed a less structured and delayed rehabilitation approach, which lacked the same degree of personalization and early intervention.
Data Collection and Outcome Measures
Clinical data were collected retrospectively from electronic medical records and verified independently by two researchers. Primary outcomes included:Postoperative wound pain assessed by the Visual Analog Scale (VAS) at 24 hours, 48 hours, and 7 days; Length of hospital stay; Patient satisfaction scores. Secondary outcomes included:Readmission rates within 30 days; Recovery milestones, such as time to independent ambulation; Postoperative complication rates.
Postoperative Complications
Circulatory System: Monitoring of blood pressure and cardiovascular events; Coagulation System: Assessment of DVT and clotting profiles; Urinary System: Evaluation of urine output and infections; Digestive System: Observation of gastrointestinal complications and bowel function.
Power Analysis
A post-hoc power analysis was conducted using the primary outcome measure (VAS score at 24 hours) to confirm the adequacy of the sample size. Based on the observed effect size (Cohen’s d = 1.10), a total sample size of 376 (190 in ERAS group, 186 in standard care group) achieves a power of 0.99 with a two-sided alpha level of 0.05. This indicates that the study was adequately powered to detect statistically significant differences between groups.
Data Analysis
Patient characteristics and clinical outcomes were summarized using descriptive statistics. For continuous variables, including VAS scores and hospital stay durations, comparisons were performed using t-tests or Mann-Whitney U-tests as appropriate. Categorical variables, such as complication rates, were analyzed using chi-square tests or Fisher’s exact tests. To account for potential confounders like age, gender, and comorbidities, multivariable regression analysis was applied. Statistical evaluations were carried out with SPSS software (version 25.0, IBM, Armonk, NY, USA), with significance set at P<0.05. Data visualizations were generated using R (version 4.0.5) and GraphPad Prism (version 8.0).
Results
The inclusion and exclusion criteria are detailed in Figure 1. A total of 376 patients undergoing ankle fracture surgery were included in this study, with 190 patients receiving ERAS-based rehabilitation and 186 receiving standard care. Baseline characteristics, including gender distribution, age, BMI, and ASA classification, were comparable between the two groups (P > 0.05). Similarly, the distribution of fracture types (bimalleolar, unimalleolar, and trimalleolar) and comorbidities, such as diabetes mellitus and hypertension, showed no statistically significant differences. Although the prevalence of open fractures and fractures caused by traffic accidents was slightly higher in the ERAS group, these differences were not significant (Table 1).
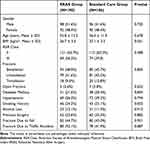 |
Table 1 Baseline Characteristics of Patients Undergoing Ankle Fracture Surgery Across ERAS-Based and Standard Care Groups |
 |
Figure 1 Inclusion and exclusion table for patients undergoing total knee arthroplasty. |
Postoperative complications occurred less frequently in the ERAS group compared to the standard care group. Specifically, rates of postoperative infection (1.6% vs 6.5%, P=0.011), deep vein thrombosis (3.2% vs 8.6%, P=0.016), and delayed wound healing (0.8% vs 5.4%, P=0.009) were significantly lower in the ERAS group. Other complications, such as wound dehiscence, respiratory complications, and cardiovascular events, did not differ significantly between groups (Table 2).
 |
Table 2 Postoperative Complications Among Patients Receiving ERAS-Based Rehabilitation Versus Standard Care |
Logistic regression analyses identified ERAS-based rehabilitation (OR=3.412, 95% CI: 2.529–4.602, P<0.001) and early mobilization within 24 hours (OR=2.593, 95% CI: 1.983–3.462, P<0.001) as independent predictors of shorter hospital stays. Factors such as gender, age, BMI, and fracture type were not significantly associated with the duration of hospital stay in multivariate analyses (Table 3).
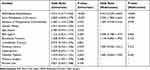 |
Table 3 Predictors of Shorter Hospital Stay Following Ankle Fracture Surgery |
Clinical recovery outcomes showed significant improvement in the ERAS group. The time to achieve first ambulation was notably shorter (20.4 ± 5.7 hours vs 42.8 ± 6.9 hours, P<0.001), and patients reached independent walking earlier (3.6 ± 1.1 days vs 5.9 ± 1.4 days, P<0.001). Pain levels, as measured by the Visual Analog Scale (VAS), were consistently lower in the ERAS group at all measured intervals: 24 hours, 48 hours, and 7 days postoperatively (P<0.001). Additionally, patient satisfaction ratings were significantly higher in the ERAS group (92.4% vs 76.8%, P<0.001), and the duration of hospital stay was reduced (5.1 ± 1.6 days vs 6.7 ± 2.1 days, P<0.001) (Table 4).
 |
Table 4 Clinical Recovery Outcomes |
Quality of life and functional recovery outcomes also favored the ERAS group. Participants scored higher on the physical and mental health components of the Short Form-36 (SF-36) survey (P<0.001) and demonstrated superior results in the EuroQol-5D (EQ-5D) index and EQ Visual Analog Scale (EQ-VAS). Furthermore, a larger proportion of ERAS patients returned to work or resumed daily routines (81.6% vs 68.7%, P=0.039) and reported greater participation in social activities (78.9% vs 65.4%, P=0.028). The ability to perform activities of daily living (ADLs) independently was also markedly better in the ERAS group (89.5% vs 75.8%, P=0.014) (Table 5).
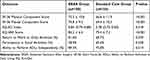 |
Table 5 Patient-Reported Outcomes Comparing ERAS and Standard Care Groups |
Discussion
Ankle fracture surgery is a commonly performed orthopedic procedure critical for restoring joint stability and function in trauma patients.2,18,19 Despite advancements in surgical techniques, postoperative wound pain remains a major challenge, often delaying recovery and negatively affecting patient outcomes. Effective pain management is crucial for promoting early mobilization, reducing complications, and achieving optimal recovery.16,20,21 This study demonstrates that applying ERAS principles in the rehabilitation of ankle fracture patients leads to significantly improved postoperative outcomes. These benefits include reduced pain intensity, earlier mobilization, shorter hospital stays, and increased patient satisfaction. These findings are consistent with ERAS implementations in other orthopedic procedures and underscore the importance of a structured, multimodal perioperative approach tailored to trauma patients.
One of the most significant findings of our study is the reduction in postoperative complications in the ERAS group, including lower rates of postoperative infection, deep vein thrombosis, and delayed wound healing. These reductions emphasize the efficacy of ERAS protocols in minimizing perioperative risks. Morrell et al22 reported similar findings, demonstrating that ERAS protocols reduce complication rates and promote functional recovery in orthopedic surgery. Similarly, Zhang et al23 found that it can significantly shorten LOS, reduce transfusion rates, and decrease 30-day postoperative mortality. The superior outcomes observed in our study may be attributed to key components of ERAS protocols, including early mobilization, multimodal pain management, and preoperative education. These strategies likely contributed to improved pain control, enhanced circulation, and better overall recovery.
In addition to fewer complications, patients in the ERAS group achieved faster recovery milestones and had shorter hospital stays. Compared to standard care, the ERAS group’s hospital stays were reduced by an average of 1.6 days (5.1 ± 1.6 days vs 6.7 ± 2.1 days, P<0.001). Early mobilization within 24 hours and individualized rehabilitation plans likely accelerated functional recovery. These findings align with research by Zhu et al7 who demonstrated that ERAS protocols significantly reduce hospital stays and associated healthcare costs across various surgical fields. Shorter hospital stays also alleviate psychological and emotional burdens on patients and their families, further highlighting the holistic benefits of ERAS-based care.24,25 An important consideration in the management of ankle fractures is the risk of long-term complications, particularly post-traumatic osteoarthritis. This condition may develop due to residual joint incongruity, instability, or chronic inflammation, and can substantially affect patients’ long-term mobility and quality of life. In severe cases, especially when conservative treatments fail, ankle arthrodesis (joint fusion) may be required to relieve pain and restore function. As noted by Biz et al, post-traumatic osteoarthritis remains a common sequela in complex ankle fractures and is a leading indication for surgical fusion procedures.26 While surgical solutions like arthrodesis address severe structural outcomes, non-invasive interventions such as taping can offer functional benefits during earlier phases of recovery. Beyond standard rehabilitation protocols, the application of functional taping during the recovery phase has shown potential benefits in improving proprioception, neuromuscular control, and ankle joint stability. Taping may assist in reducing reinjury risk, supporting the joint during early mobilization, and enhancing confidence in movement. According to newly research, incorporating taping into physical therapy regimens yielded improved dynamic balance and ankle function in individuals recovering from ankle trauma.27
Our study also emphasizes significant improvements in patient-reported outcomes. Patients in the ERAS group reported higher scores in the physical and mental components of the SF-36, along with better overall health as measured by the EQ-5D index. Choi et al28 found that ERAS protocols significantly reduced the use of opioids and antiemetics, improved long-term pain management and functional recovery after orthopedic surgery, and decreased the incidence of complications in patients undergoing spinal fusion. Furthermore, a larger proportion of patients in the ERAS group resumed work or daily activities during the follow-up period, reflecting the comprehensive advantages of ERAS-based rehabilitation. These findings underscore the importance of integrating patient-centered strategies, such as individualized rehabilitation and education, into perioperative care to optimize functional recovery and satisfaction.
To further enhance the effectiveness and clinical applicability of ERAS protocols in ankle fracture surgery, recent studies have emphasized the importance of integrating structured physiotherapy interventions into both the preoperative and early postoperative phases of care. One promising approach is preoperative physiotherapy, or “prehabilitation”, which focuses on improving ankle joint mobility, strengthening periarticular muscles, and addressing patients’ psychological preparedness for surgery. These interventions have been shown to reduce surgical stress, support better neuromuscular control, and accelerate postoperative recovery. In the early postoperative stage, ERAS protocols may benefit from more standardized and personalized rehabilitation plans that adapt to individual patient needs. Evidence-based physiotherapy guidelines recommend a phased progression of rehabilitation that includes ankle range-of-motion training, proprioceptive exercises, isometric muscle activation, and gradual weight-bearing, beginning as early as 24 hours after surgery. Such protocols have been associated with improved circulation, reduced risk of complications such as deep vein thrombosis, and earlier achievement of functional milestones. Moreover, integrating standardized rehabilitation frameworks—as suggested in the current literature—can enhance interprofessional collaboration between surgeons, physiotherapists, and nursing staff, while ensuring consistency in clinical delivery. These refinements may help optimize functional outcomes, improve quality of life, and further reduce the length of hospital stay. As the field continues to evolve, embedding these physiotherapy-driven strategies into ERAS models may represent a critical next step in advancing recovery pathways for orthopedic trauma patients.1,29
While ERAS protocols have demonstrated success in colorectal, spine, and joint replacement surgeries, limited research has evaluated their use in acute orthopedic trauma, particularly ankle fractures. Our study addresses this gap by demonstrating that ERAS-based rehabilitation can be safely and effectively applied in ankle fracture surgery. This extends the clinical relevance of ERAS beyond elective procedures to include urgent fracture repair, suggesting that the principles of early mobilization, multimodal analgesia, and structured education may improve outcomes even in non-elective orthopedic populations. As trauma surgery continues to evolve, adapting ERAS protocols to these scenarios offers a meaningful step toward standardized, patient-centered care.
Despite these encouraging findings, our study has certain limitations. First, the retrospective nature of the research restricts the ability to draw definitive causal inferences between ERAS interventions and improved outcomes. Second, being conducted at a single institution, the study’s results may not be broadly generalizable. Future investigations should prioritize multicenter, prospective designs to confirm these findings and assess their relevance across varied healthcare environments. Demographic and geographic differences, such as variations in healthcare access and population characteristics, may influence the effectiveness of ERAS protocols. Further exploration of these factors is essential to refine care protocols and expand the applicability of ERAS-based rehabilitation in ankle fracture surgery. Finally, the lack of standardized protocols for implementing ERAS-based interventions remains a challenge. Our findings highlight the need for evidence-based guidelines to ensure consistent and effective application of ERAS principles. Standardized protocols could further optimize recovery, improve patient outcomes, and ensure uniformity in clinical practice.
Conclusion
In conclusion, this study demonstrates that ERAS-aligned rehabilitation significantly improves postoperative outcomes in ankle fracture surgery patients, including reductions in wound pain (VAS scores), shortened time to ambulation and independent walking, improved quality of life (SF-36, EQ-5D), and higher patient satisfaction. While ERAS principles are well-established, their specific application to ankle fracture surgery remains limited in current literature. Our findings suggest that adapting ERAS protocols to orthopedic trauma care is both feasible and beneficial, offering valuable clinical guidance for improving recovery in this underrepresented patient population.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participation
Written informed consent was obtained from all participants. This research was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Dazhou Central Hospital.
Acknowledgments
Thanks to the nurses in the department for their help with the project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Chen B, Ye Z, Wu J, Wang G, Yu T. The effect of early weight-bearing and later weight-bearing rehabilitation interventions on outcomes after ankle fracture surgery: a systematic review and meta-analysis of randomised controlled trials. J Foot Ankle Res. 2024;17(2):e12011. doi:10.1002/jfa2.12011
2. Lin CW, Donkers NA, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. 2012;11:Cd005595. doi:10.1002/14651858.CD005595.pub3
3. Pflüger P, Braun KF, Mair O, Kirchhoff C, Biberthaler P, Crönlein M. Current management of trimalleolar ankle fractures. EFORT Open Rev. 2021;6(8):692–703. doi:10.1302/2058-5241.6.200138
4. Ljungqvist O, de Boer HD, Balfour A, et al. Opportunities and challenges for the next phase of enhanced recovery after surgery: a review. JAMA Surgery. 2021;156(8):775–784. doi:10.1001/jamasurg.2021.0586
5. Smith TW, Wang X, Singer MA, Godellas CV, Vaince FT. Enhanced recovery after surgery: a clinical review of implementation across multiple surgical subspecialties. Am J Surg. 2020;219(3):530–534. doi:10.1016/j.amjsurg.2019.11.009
6. Wainwright TW, Immins T, Middleton RG. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract Res Clin Anaesth. 2016;30(1):91–102. doi:10.1016/j.bpa.2015.11.001
7. Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. 2017;93(1106):736–742. doi:10.1136/postgradmedj-2017-134991
8. Biz C, Angelini A, Zamperetti M, et al. Medium-long-term radiographic and clinical outcomes after surgical treatment of intra-articular tibial pilon fractures by three different techniques. Biomed Res Int. 2018;2018:6054021. doi:10.1155/2018/6054021
9. Ljungqvist O. ERAS--enhanced recovery after surgery: moving evidence-based perioperative care to practice. JPEN J Parenter Enteral Nutr. 2014;38(5):559–566. doi:10.1177/0148607114523451
10. Ljungqvist O, Hubner M. Enhanced recovery after surgery-ERAS-principles, practice and feasibility in the elderly. Aging Clin Exp Res. 2018;30(3):249–252. doi:10.1007/s40520-018-0905-1
11. Vannucci J, Costi S, Matricardi A, Scarnecchia E, Droghetti A. VATS group ERAS registry. J Thoracic Dis. 2018;10(Suppl 4):S571–S577. doi:10.21037/jtd.2018.02.56
12. Ripollés-Melchor J, Abad-Motos A, Díez-Remesal Y, et al. Association between use of enhanced recovery after surgery protocol and postoperative complications in total hip and knee arthroplasty in the postoperative outcomes within enhanced recovery after surgery protocol in elective total hip and knee arthroplasty study (POWER2). JAMA Surgery. 2020;155(4):e196024. doi:10.1001/jamasurg.2019.6024
13. Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. 2022;11(2):121–129. doi:10.2217/cer-2021-0258
14. Li T, Sun ZJ, Zhou Y, et al. Perioperative protocol of ankle fracture and distal radius fracture based on enhanced recovery after surgery program: a multicenter prospective clinical controlled study. Pain Res Manag. 2022;2022(3458056):1–8. doi:10.1155/2022/3458056
15. Yao YC, Liou JY, Wang HY, Chou PH, Lin HH, Wang ST. Benefits of early recovery after surgery (ERAS) protocols on perioperative outcomes in patients undergoing elective lumbar spinal fusion: a prospective study. Spine J. 2025. doi:10.1016/j.spinee.2025.01.023
16. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surgery. 2017;152(7):691–697. doi:10.1001/jamasurg.2017.0898
17. Hübner M, Kusamura S, Villeneuve L, et al. Guidelines for perioperative care in cytoreductive surgery (CRS) with or without hyperthermic IntraPEritoneal chemotherapy (HIPEC): enhanced recovery after surgery (ERAS®) society recommendations - part I: preoperative and intraoperative management. Eur J Surg Oncol. 2020;46(12):2292–2310. doi:10.1016/j.ejso.2020.07.041
18. Tengberg PT, Ban I. Treatment of ankle fractures. Ugeskrift Laeger. 2018;180(41):V11170883.
19. Winge R, Bayer L, Gottlieb H, Ryge C. Compression therapy after ankle fracture surgery: a systematic review. Eur J Trauma Emerg Surg. 2017;43(4):451–459. doi:10.1007/s00068-017-0801-y
20. Hübner M, Kusamura S, Villeneuve L, et al. Guidelines for perioperative care in cytoreductive surgery (CRS) with or without hyperthermic intraperitoneal chemotherapy (HIPEC): enhanced recovery after surgery (ERAS®) society recommendations - part II: postoperative management and special considerations. Eur J Surg Oncol. 2020;46(12):2311–2323. doi:10.1016/j.ejso.2020.08.006
21. Rawal N. Intrathecal opioids for the management of post-operative pain. Best Pract Res Clin Anaesth. 2023;37(2):123–132. doi:10.1016/j.bpa.2023.01.001
22. Morrell AT, Layon DR, Scott MJ, Kates SL, Golladay GJ, Patel NK. Enhanced recovery after primary total hip and knee arthroplasty: a systematic review. J Bone Joint Surg Am Vol. 2021;103(20):1938–1947. doi:10.2106/JBJS.20.02169
23. Zhang Q, Chen Y, Li Y, et al. Enhanced recovery after surgery in patients after Hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. 2024;100(1181):159–173. doi:10.1093/postmj/qgad125
24. Gonella F, Massucco P, Perotti S, et al. Prehab, ERAS, rehab: a patient care continuum around colo-rectal surgery: prehabilitation combined with ERAS and rehabilitation to reduce morbidity and hospital stay. Eur J Surg Oncol. 2024;50(12):108688. doi:10.1016/j.ejso.2024.108688
25. Schneider S, Armbrust R, Spies C, du Bois A, Sehouli J. Prehabilitation programs and ERAS protocols in gynecological oncology: a comprehensive review. Arch Gynecol Obstetrics. 2020;301(2):315–326. doi:10.1007/s00404-019-05321-7
26. Biz C, Hoxhaj B, Aldegheri R, Iacobellis C. Minimally invasive surgery for tibiotalocalcaneal arthrodesis using a retrograde intramedullary nail: preliminary results of an innovative modified technique. J Foot Ankle Surg. 2016;55(6):1130–1138. doi:10.1053/j.jfas.2016.06.002
27. Biz C, Nicoletti P, Tomasin M, Bragazzi NL, Di Rubbo G, Ruggieri P. Is kinesio taping effective for sport performance and ankle function of athletes with chronic ankle instability (CAI)? A systematic review and meta-analysis. Medicina. 2022;58(5):620. doi:10.3390/medicina58050620
28. Choi JU, Kee TH, Lee DH, Hwang CJ, Park S, Cho JH. Enhanced recovery after surgery protocols in one- or two-level posterior lumbar fusion: improving postoperative outcomes. J Clin Med. 2024;13(20):6285. doi:10.3390/jcm13206285
29. Lewis SR, Pritchard MW, Parker R, et al. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. 2024;9(9):Cd005595. doi:10.1002/14651858.CD005595.pub4
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

