Back to Journals » Drug Design, Development and Therapy » Volume 19
Enhancing Cartilage Repair in Osteoarthritis Using Platelet Lysates and Arthroscopic Microfracture
Authors Zhang H, Li D, Zheng W , Hua J, Chen Z , Xu W, Zhu J, Wang Y , Chen X, Chen H, Guo L, Yuan Q, Zhou L , Shan L
Received 13 November 2024
Accepted for publication 18 April 2025
Published 13 May 2025 Volume 2025:19 Pages 3827—3843
DOI https://doi.org/10.2147/DDDT.S502935
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Tuo Deng
Haiyan Zhang,1,* Dipeng Li,2,* Wei Zheng,3,* Jiaqing Hua,3,* Zuxiang Chen,4 Wenting Xu,4 Jianing Zhu,5 Yue Wang,3 Xiaotian Chen,3 Huixin Chen,3 Le Guo,3 Qiang Yuan,3 Li Zhou,4 Letian Shan1
1The Second Affiliated Hospital, Zhejiang Chinese Medical University, Hangzhou, Zhejiang, People’s Republic of China; 2Department of Orthopaedics, Hangzhou Ninth People’s Hospital, Hangzhou, Zhejiang, People’s Republic of China; 3College of Pharmaceutical Science, Zhejiang Chinese Medical University, Hangzhou, Zhejiang, People’s Republic of China; 4The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, Zhejiang, People’s Republic of China; 5The Second Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Letian Shan; Li Zhou, Email [email protected]; [email protected]
Background: Osteoarthritis (OA) is the most prevalent joint degenerative disease. MF is considered as a first-line treatment for OA. In the long term, the cartilage tissue regenerated after MF is fibrocartilage. In this study, we examine whether combined treatment of MF and Platelet lysate (PL) can inhibit promotion of cartilage repair and antifibrosis.
Methods: OA rat model established by the modified Hulth method. Rat PL injected into treated knee joints after MF surgery. The expression levels of metabolic and fibrosis molecules (Col2, Mmp13, Col1, Col3, α-SMA, and Ctgf) of chondrocytes were examined by immunohistochemistry. Cell immunofluorescence was used to assess bone marrow MSCs (BMSCs) proliferation. Transwell assays evaluated BMSCs migration, and qPCR and Western blot analyzed the mechanisms of PL. Moreover, a retrospective analysis was conducted to determine the clinical efficacy and safety of the combined treatment of MF and PL on OA patients.
Results: In vivo data showed that the combined treatment of MF and PL significantly alleviated joint pain, protected chondrocytes and inhibited synovial fibrosis on OA rats, as was confirmed by upregulation of Collagen II and downregulation of Mmp13, Col1, Col3, α-SMA, and Ctgf. Such anti-OA and antifibrosis effects of the combined treatment of MF and PL were superior to MF alone. In vitro data showed that PL induced cellular chondrogenic differentiation and migration of BMSCs, suggesting that PL facilitated stem cell homing to the cartilage injury sites and promoted cartilage repair and regeneration. Furthermore, the clinical data showed significant improvements of pain reduction and cartilage repair in OA patients.
Conclusion: This study demonstrated the anti-OA and antifibrosis effects of the combination of MF and PL, providing a promising synergistic therapeutic option for the treatment of OA.
Keywords: platelet lysate, microfracture, osteoarthritis, bone marrow mesenchymal stem cells, antifibrosis
Graphical Abstract:

Introduction
Osteoarthritis (OA) is the most prevalent joint degenerative disease worldwide and is primarily characterized by the deterioration of hyaline cartilage, loss of intact subchondral bone, and synovial inflammation.1–5 Inflammation is a key factor in the maintenance of OA and is positively correlated with pain of knee joints.6,7 At the global, approximately 500 million individuals are currently affected by OA worldwide, 22% of adults over the age of 40 have knee OA.1 The knee joint is the most commonly affected joint, accounting for 80% of global OA cases.8,9 Current treatments for OA include surgical interventions and pharmaceutical treatments. The oral administration of analgesia, non-steroidal anti-inflammatory drugs (NSAIDs), and selective inhibitors of cyclooxygenase 2 (COX2) are the most common pharmaceutical treatments, but they can only provide pain relief and symptom control, long-term NSAIDs use in patients may result in severe adverse effects.10,11 Surgical interventions can be divided into early intervention and end-stage intervention. Early surgical interventions include microfracture (MF), autologous chondrocyte implantation (ACI), autologous matrix-induced chondrogenesis (AMIC), and matrix-assisted autologous chondrocyte implantation (MACI).12 Compared with other early surgical strategies, MF has the advantages of less damage, simple operation and quick recovery. Total knee arthroplasty (TKA) is the ultimate treatment option for patients with advanced OA. However, postoperative complications such as infection and periprosthetic knee fractures may occur after surgery,13,14 which carries a heavy social and economic burden. Therefore, there is an urgent clinical need to develop new therapeutic strategies to treat OA.
Microfracture (MF) is an early surgical strategy for repairing osteochondral lesions and has received attention for its better efficacy in OA.2 The principle of MF treatment is to drill holes in the cartilage injury site, blood and bone marrow naturally leak out of the bone cavity and fill the injury site after a blood clot is formed in the injury site. The bone marrow mesenchymal stem cells (BMSCs) in the clot release growth factors and differentiate into fibrocartilage to replace the articular cartilage and improve the injury.15,16 MF is considered as a first-line treatment for the early cartilage repair of OA in addition to oral drugs because of its low cost, good short-term efficacy and easy operation.17 However, MF can only repair cartilage damage of small and limited size.18,19 The best repair defect size is about 1~2.5 cm2. In the long term, the cartilage tissue regenerated after MF is fibrocartilage. The most important biomarkers for fibrocartilage are collagen type I (Col1), collagen type III (Col3) and Alpha-smooth muscle actin (α-SMA).20,21 In the contrary, the biomarker for hyaline cartilage is collagen type II (Col2), SRY-related high-mobility group box 9 (Sox9), and aggrecan.22 It is difficult to obtain hyaline cartilage repair with high weight-bearing capacity and resistance to mechanical wear in microfracture surgery.23 In addition, knee OA (kOA) patients are predominantly elderly, and they release a low number of BMSCs after MF surgery, resulting in a weak self-repair and regenerative capacity of BMSCs.24 These disadvantages have limited the MF application in the clinic.
Platelet lysate (PL) is obtained by freeze-thaw lysis of platelet granules rich in growth factors. The main components of PL include platelet derived growth factor (PDGF), insulin-like growth factor (IGF), basic epidermal growth factor (EGF), fibroblast growth factor (FGF), hepatocyte growth factor (HGF) and transforming growth factor-β (TGF-β).25 PL is recognized for its ability to promote tissue growth, repair and healing.26,27 Previous studies have shown that PL can synergistically treat OA with mesenchymal stem cells (MSCs) including BMSCs, the combined treatment of PL and MSCs significantly reversed the OA pathological changes.28 Moreover, PL as an adjuvant for MSCs in treating OA, which promotes proliferation, cell cycle transition and migration of MSCs. Considering that combined treatment of PL and MSCs increase the expression of cartilage anabolic biomarkers Col2 and Sox9, we hypothesize that PL can inhibit the formation of fibrocartilage after MF.
The purpose of this study was to evaluate the promotion of cartilage repair and antifibrosis of MF and combined treatment of MF and PL on rat OA model through pain behavior test, cartilage histopathological and immunohistochemical analyses. We evaluated the migration and proliferation effects of PL on BMSCs by transwell and cellular immunofluorescence analysis. In addition, a retrospective study was carried out to confirm the clinical efficacy of combined treatment of MF and PL on OA patients. The novelty of this study lies in the combination of animal experiment and clinical data to study the therapeutic of MF and combined treatment of MF and PL, the evaluation of regulatory roles of PL towards pain and cartilage metabolism through an animal model of OA pain, demonstrating the promotion of cartilage repair and antifibrosis of combined treatment of MF and PL in clinic. This combination treatment approach helps address the limitations of current OA treatment strategies, potentially improving patient outcomes and reducing healthcare costs.
Methods
Reagents
Minimum essential medium-alpha modification (α-MEM) with Glutamax™-1 was purchased from Gibco (NY, United States). Trypsin (0.25%) was purchased from Thermo Fisher Scientific (MA, United States). Fetal bovine serum (FBS) was purchased from Gibco (NY, USA). Transwell chambers were purchased from Corning (NY, USA). TRIzol reagent and Real-time PCR kit were purchased from TaKaRa Biotechnology Co., Ltd. (Dalian, China). 2 × SYBR Green qPCR Master Mix (low ROX) kit was purchased from Bimake (TX, USA). The primary antibodies collagen type I (Col1, NB600-408), collagen type III (Col3, NB600-594), Aggrecan (NB100-74350), Fibronectin (NBP1-91258) and vascular endothelial growth factor (Vegf, NB100-664) were purchased from Novus Biologicals (CO, USA). Collagen type II (Col2, ab34712) was purchased from Abcam (MA, USA). SRY-related high-mobility group box 9 (Sox9, A2479) and connective tissue growth factors (Ctgf, A11067) were purchased from ABclonal (Wuhan, China). Alpha-smooth muscle actin (α-SMA, 19245), Vimentin (5741S) and proliferating cell nuclear antigen (PCNA, 13110) were purchased from Cell Signaling Technology (MA, USA). Matrix metallopeptidase 13 (Mmp13, 18165-1-AP) was purchased from Proteintech (IL, USA). Collagen type I (Col1, AF7001) was purchased from Affinity Biosciences (Jiangsu, China). β-Actin was purchased from Sigma-Aldrich (MO, USA). Mouse recombinant IGF-1 protein was purchased from Thermo Fisher Scientific (MA, United States). Rat recombinant HGF protein and rat IL-1β protein were purchased from Sino Biological (Beijing, China). Hematoxylin and eosin (H&E), Safranin O/Fast green (SO) and Toluidine blue (TB) staining kits were purchased from Sigma-Aldrich (MO, USA). Masson staining kit was purchased from Yuanye Technology Co., Ltd. (Shanghai, China). Phosphate-buffered saline (PBS) was purchased from Sangon Biotech (Shanghai, China).
Rats
All animal experimental procedures were performed according to the guidelines for the Care and Use of Laboratory Animals of the National Institutes of Health and were approved by the Medical Regulation and Ethics Committee of Zhejiang Chinese Medical University (Approval No. 20231120–25). Eight-week-old male Sprague Dawley (SD) rats weighing 280–300 g were purchased from Shanghai SLAC Laboratory Animal Co., Ltd, China. All rats were housed in pathogen-free cages with a 12-hour light/dark cycle and free access to food and water. To evaluate the in vivo efficacy of MF and PL, 32 rats were randomly divided into 4 groups: 1) normal control group (Sham); 2) OA model group (Model); 3) MF treated model group (MF); and,4) sequential MF and PL treated model group (MF+PL). 8 rats were in each group. After one week of acclimatization, kOA was surgically induced by the modified Hulth method.29 Briefly, a 1 cm longitudinal incision was made in the skin of the posterior medial aspect of the rat knee, the medial collateral ligament and the anterior cruciate ligament were severed, and the medial meniscus was removed. Then the incision was closed layer by layer after surgery. In the sham group, only the longitudinal incision was made in the skin of the medial knee joint, which was closed layer by layer after surgery. An intramuscular injection of 20,000 units of penicillin was given 2 hours after the surgery to prevent infection for 3 consecutive days. One month after OA modeling, rats in the MF group underwent MF surgery,30 and an MF hole was manually created by a 0.5 mm round drill in the femoral trochlear groove. While rats in the sham and model group only had the longitudinal incision in the skin of the medial knee joint, followed by incision closure. At three days post Sham MF or MF treatment, rats in the MF+PL group were intra-articularly injected with 50 μL of PL, while rats in the other three groups were intra-articularly injected with 50 μL of saline. Only one intra-articular injection of PL or saline was performed for the entire experiment. After pain behavior measurements, all rats were anesthetized and euthanized for the following experiments (Figure 1).
 |
Figure 1 Timetable and flowchart of rat modeling and therapy. |
Pain Behavior Assessment
At 1 month after the PL treatment, the mechanical withdrawal thresholds (MWTs) were measured thrice in all rats by the classical von Frey filament (Ugo Basile, Lombardy, Italy) pain evaluation method.31 After 30 min of adaptation, the von Frey filaments were placed perpendicularly against the mid-plantar surface of the hind paws of each rat for at least three times and held for 2 s. Starting from 4 grams, the number of grams of stimulation was gradually increased. The presence of foot lifting or licking 3 times out of 5 stimulations was regarded as a positive response, and the number of grams eliciting a positive response was recorded as the MWTs.
Histopathological and Immunohistochemical Analyses
After being sacrificed, the joints of each rat were fixed with 10% formalin for 48 h, followed by decalcification with 10% EDTA solution for 8 weeks. After that, each sample was embedded in paraffin, cut into 4 μm, and stained with Hematoxylin and eosin (H&E), Safranin O/Fast green (SO), Masson, and Toluidine blue (TB). The OA progression was assessed according to the scoring system of Mankin and OARSI.32,33 Synovitis score was used to quantify pathological changes in the synovium.34 The expression of Col1 (1:100), Col2 (1:200), Col3 (1:100), α-SMA (1:200), Ctgf (1:50) and Mmp13 (1:300) was detected by immunohistochemistry. Briefly, each slice underwent antigen retrieval (pH 6.0, Solarbio, Beijing, China) and was incubated with different primary antibodies (Col1, Col2, Col3, α-SMA, Ctgf, and Mmp13). Then incubated with corresponding secondary antibody and finally detection using 3.3′-diaminobenzidine (DAB). Col1, Col2, Col3, α-SMA, Ctgf, and Mmp13 expression was quantified by Image-Pro Plus 6.0 software (Media Cybernetics, MD, USA) under a light microscope (NIKON 80i, Tokyo, Japan). The data were expressed as the percentage of antigen-positive area to total area in the selected 6 fields.
Preparation of Primary Bone Marrow Stem Cells
Rat bone marrow mesenchymal stem cells (BMSCs) were isolated from 2-week-old SD rats as previously described.35 Briefly, the femur and tibia of rats were removed under sterile conditions and then washed three times with PBS solution. The bone marrow cavity was then rinsed with α-MEM supplemented with 10% FBS. The rinsate was then filtered through a 70 μm cell strainer (Corning, NY). After centrifugation at 1000 rpm for 10 minutes, the cell pellets were collected as BMSCs and cultured adherently in an incubator at 37°C, 5% CO2, using α-MEM supplemented with 10% FBS, and 3 to 5 generations of BMSCs were used for subsequent experiments.
Rat PL Extraction
Rat platelet lysate (PL) was prepared by lysing platelet concentrates of rat plasma according to the acknowledged method with modifications.36 Briefly, 10 mL of whole blood was collected from the heart of each rat in tubes containing sodium citrate (3% v/v) anticoagulant. After standing at 4°C for 2 h, the supernatant was collected by centrifugation at 190 g for 5 min, with the non-erythrocyte volume collected subsequently. The platelet concentrate was lysed by repeating frozen and thawed 3 times at −80°C and 37°C, followed by centrifugation at 2,000 × g for 10 min to remove remaining platelet fragments. The obtained supernatant containing PL was divided into aliquots and stored at −80°C before use.
Cellular Experimentation
To investigate the effects of PL on BMSCs, BMSCs were divided into two groups: normal control (NC) group and PL group. BMSCs in the NC group were cultured in α-MEM supplemented with 10% FBS, whereas the PL group in α-MEM containing 10% PL.
In order to study the effect of growth factors in PL on chondrocytes fibrosis, chondrocytes were divided into NC group, IL-1β group, HGF+IGF-1 group and PL group. The IL-1β group, HGF+IGF-1 group and PL group were modeled by pre-treating IL-1β (10 ng/mL) for 24 h for fibrosis modeling. Subsequently, the HGF+IGF-1 group was treated with physiological concentration HGF (505 pg/mL)37 and physiological concentration IGF-1 (56.2 pg/mL)28 for 24 h, the PL group was treated with 10% PL for 24 h.
Cell Immunofluorescence
BMSCs were seeded into coverslips within 24-well plates at a density of 5 × 104 cell/well. After 48 h, the culture medium was discarded and the coverslips were washed three times with PBS. Cells were fixed with 4% paraformaldehyde (Servicebio, Beijing, China) and washed three times with PBS. The fixed cells were permeabilized with 0.1% Triton X-100 (Beyotime Biotechnology, Shanghai, China) for 30 minutes at room temperature. After washing three times with PBS, cells were incubated in goat serum (ZSGQ-BIO, Beijing, China) for 1 h to block non-specific antibody binding, then incubated overnight at 4°C with primary antibody PCNA (1:400), followed by incubating with secondary antibody for 1 h at 4°C and DAPI staining in the absence of light. Three coverslips were carried out for each group, and PCNA positive cells in three randomly selected fields were imaged under a fluorescent microscope (CarlZeiss, Göttingen, Germany).
Transwell Assay
BMSCs were seeded at a density of 5×104 cell/well in the upper chamber of inserts in 24-well transwell chambers with 8 μm nitrocellulose pore filters. 600 μL α-MEM containing either 10% FBS (NC group) or 10% PL (PL group) were added into the lower chamber. After 15 h, the cells that passed through the membranes of the upper chambers were fixed with 4% paraformaldehyde and stained with 1% crystal violet dye solution (Beyotime Biotechnology, Shanghai, China). Images of each group were captured using a light microscope in different areas in three independent repeated experiments. The number of migrated BMSCs was calculated by manual counting on three random microscope fields.
Real-Time PCR (qPCR)
The qPCR method used in this study was the same as our previous study described.38 With β-Actin as the reference gene, relative mRNA expression was determined by 2−ΔΔCT method (Table 1).
 |
Table 1 Primer Sequences of Targeted Genes |
Western Blot Analysis
Total protein of BMSCs and chondrocytes were extracted with RIPA lysis buffer (Beyotime Biotechnology, Shanghai, China), quantified by BCA protein assay kit (Beyotime Biotechnology, Shanghai, China) and denatured. Sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and nitrocellulose membranes (Gottingen, Germany) were used to separate and transfer the targeted proteins. After blocking with 5% nonfat milk in Tris-buffered saline tween, the membranes were incubated with the following primary antibodies: β-Actin (1:40,000), Aggrecan (1:1000), Col2 (1:1500), Sox9 (1:1000), Fibronectin (1:1500), Vimentin (1:1000), Vegf (1:1000), Col1 (1:1000), Col3 (1:1000), α-SMA (1:1500). The membranes were then incubated with corresponding secondary antibody peroxidase-conjugated goat antirabbit/mouse IgG (ZSGQ-BIO, Beijing, China). Finally, the protein was visualized using ECL kit (Biosharp, Beijing, China) and analyzed using ImageQuant TL 7.0 analysis software (GE, United States).
Clinical Retrospective Study
This study complied with the Declaration of Helsinki. The Ethics Committee of Hangzhou Ninth People’s Hospital gave its approval to this study (Ethical number: 2021–04). The data of 33 patients with OA who have been treated with 5 mL patient autologous PL were collected. Immediately after arthroscopic microfracture surgery, each patient received only one PL treatment through intra-articular injection. For evaluating the clinical outcomes, visual analog scale (VAS), Lysholm score, HSS scores and magnetic resonance imaging (MRI) examinations were performed 1 week before (baseline) and 3 months after the administration. The inclusive criteria include: (1) meets the diagnostic criteria for kOA; (2) age ≥ 40 years; (3) MRI confirmed localized full thickness cartilage defects in the knee joint; (4) scheduled for arthroscopic examination; and (5) voluntarily agreed to participate in the study and provided signed informed consent. The exclusive criteria include: (1) X-ray confirmed varus/valgus deformity of the knee joint exceeding 5°; (2) combined varus/valgus deformity with flexion contracture; (3) joint instability caused by ligament injury, systemic arthropathy, or tibial lesions; (4) patients lost to follow-up during the study; (5) coagulation disorders or immune system diseases; (6) active infections, rheumatoid arthritis, or other systemic joint diseases; and (7) inability to tolerate surgery or anesthesia. All patients gave their written informed consent to this study.
Statistical Analysis
SPSS23.0 software (SPSS, IL, USA) was used for data analysis. All data in the article were expressed as mean ± standard error of the mean (SEM). Data from clinical retrospective study analyzed with Student’s t-test after confirming homogeneity of variances. One-way analysis of variance (ANOVA) followed by Tukey’s post hoc test was used for comparison among groups ≥3. Statistical differences were considered to be significant at p < 0.05.
Results
PL Attenuated Synovial Fibrosis in Osteoarthritic Rats
To investigate the in vivo effects of PL on synovial fibrosis, pathologic changes in the synovium were assessed on OA rats. HE and Masson staining showed obvious hyperplasia, angiogenesis, and collagen fiber deposition in the synovium after modeling, suggesting the presence of synovial inflammation and fibrosis in the model rats (Figure 2A and B). By contrast, the MF treatment reduced the synovial thickness and the amount of collagen fibers within the synovium. The additional treatment of PL not only ameliorated the hyperplastic and fibrotic phenotype of the synovium but also suppressed angiogenesis in the synovium (Figure 2A and B). Thus, the administration of PL could attenuate synovial fibrosis in OA rats.
PL Benefited Chondroprotection in Osteoarthritic Rats
To investigate the therapeutic effects of MF and PL on OA, a rat OA model was established by using the modified Hulth method. Histopathological staining results showed cartilage degeneration with chondrocytes and glycosaminoglycan loss, and the Mankin’s scores and OARSI scores were significantly increased (p < 0.01 vs sham) after modeling (Figure 3A, D and E). MF treatment (MF group) apparently improved the structural integrity of articular cartilage, increased the number of chondrocytes and the content of glycosaminoglycan, with significantly reduced Mankin’s scores and OASRI scores (p < 0.01 vs model) (Figure 3A, D and E). The sequential MF and PL treatment outperformed the single MF treatment in terms of chondrocytes and glycosaminoglycan production, with considerably lower Mankin’s scores and OASRI scores (p < 0.01 vs model) (Figure 3A, D and E). Immunohistochemical results showed that Col2 and Mmp13 were significantly altered in the model group (p < 0.01 vs sham) (Figure 3B). The expressions of Col2 and Mmp13 were dramatically restored to normal levels after the combined treatment of MF and PL (p < 0.01 vs model) (Figure 3F and G). The pain behavior evaluation showed rats in the model group had abnormal allodynia with significantly decreased MWTs (p < 0.01 vs sham) (Figure 3C). While after the administration of MF and PL, MWTs were significantly increased (p < 0.05 vs model) (Figure 3C). Taken together, the combined treatment of MF and PL exhibited better chondroprotective effects than MF alone in OA rats.
PL Inhibited Pathological Fibrocartilage Formation in OA Progression
To evaluate whether PL had an inhibitory effect on fibrocartilage formation caused by microfracture, several fibrocartilage markers were examined by immunohistochemical experiments. Immunohistochemical results showed that the expression of Col1, Col3, α-SMA, and Ctgf were significantly elevated in the MF group (p < 0.01 vs sham). After combined treatment of MF and PL, the expression of these markers was significantly restored to normal levels (p < 0.01 vs MF). Notably, despite the absence of MF treatment, the expression of Col1, Col3, and Ctgf was elevated in the model group (p < 0.05 vs sham) (Figure 4A–E). The above results revealed that MF did have a pro-fibrotic effect on rat cartilage, and PL inhibited the formation of fibrocartilage after the microfracture procedure.
PL Promoted Migration and Proliferation of BMSCs
To evaluate the pro-migratory and proliferative effects of PL on BMSCs, we performed transwell and cellular immunofluorescence assays. As shown in Figure 5A and B, the number of cells migrating in the PL group was significantly higher than that in the NC group (p < 0.05). Cellular immunofluorescence showed that PL promoted the expression of PCNA compared to the control group, indicating that PL had a significant effect on BMSCs proliferation (Figure 5C and D). The above results showed that PL could promote both migration and proliferation of BMSCs.
PL Regulated Chondrogenic Differentiation and Migration of BMSCs
To evaluate the chondrogenic differentiation and migration effects of PL on BMSCs, we performed qPCR and Western blotting assays. The qPCR results showed that the mRNA expression of chondrogenic differentiation markers (Aggrecan, Col2, Sox9) and migration markers (Fibronectin, Vimentin, Vegf) was significantly increased in BMSCs after 48 h of PL intervention (p < 0.01) (Figure 6A). Consistent with the qPCR results, Western blotting showed that PL significantly increased the expression of Aggrecan, Col2, Sox9, Fibronectin, Vimentin, and VEGF proteins in BMSCs (Figure 6B and C). Thus, the administration of PL effectively increased the expression of genes related to chondrogenic differentiation and migration in rat BMSCs.
PL Exerted Anti-Fibrotic Effects on Chondrocytes Mainly Through HGF and IGF-1
To investigate the antifibrotic potential of PL and its constituent growth factors (HGF and IGF-1), we performed qPCR and Western blotting assays. The qPCR results revealed that mRNA expression of cartilage fibrosis markers (Col1, Col3, and α-SMA) was significantly decreased in chondrocytes after 24 h treatment with HGF+IGF-1 or PL (p < 0.01) (Figure 7A). Consistent with these findings, Western blotting analysis demonstrated that both HGF+IGF-1 combination therapy and PL treatment markedly reduced Col1, Col3, and α-SMA protein levels (Figure 7B and C). Notably, the HGF+IGF-1 combination achieved effects comparable to PL treatment (Figure 7B and C). These results collectively indicate that HGF+IGF-1 recapitulates the antifibrotic activity of PL, suggesting these two factors are the primary functional components mediating PL’s effects.
Combined Treatment of MF and PL Relieved Symptoms in OA Patients
To confirm the clinical anti-OA efficacy of combined treatment of MF and PL, we further conducted a clinical retrospective study. Clinical data of recruited patients showed no significant difference in age between different genders among all 33 OA patients (Table 2). OA patients were evaluated for Kellgren-Lawrence grade (Table 3). MRI results showed varying degrees of improvement in articular cartilage after 3 months of combined treatment of MF and PL (Figure 8A). Compared with pre-treatment baseline, the VAS scores were significantly decreased (p < 0.01) (Figure 8B). The Lysholm scores and HSS scores were significantly increased after 3 months of treatment (p < 0.01) (Figure 8C and D), which indicated a significant improvement post-combined treatment of MF and PL.
 |
Table 2 Clinical Information of OA Patients Received Combined Treatment of MF and PL |
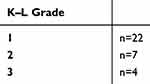 |
Table 3 Kellgren-Lawrence (K-L) Grade of OA Patients Received Combined Treatment of MF and PL |
Discussion
MF serves as the gold standard for the early treatment of OA in the clinic, but its efficacy remains controversial.39 A recent meta-analysis has demonstrated excellent short-term clinical outcomes after MF treatment (first 24 months), but the clinical durability of MF underwent functional decline over time.40 Imaging studies showed that MF treatment resulted in complete repair of cartilage damage in 18% to 95% of osteoarthritic patients, whereas 17% to 57% of the patients failed to have satisfactory outcomes.41 Suboptimal MF efficiency is due to the presence of an inflammatory microenvironment in the joint cavity and the decreased regenerative capacity of senescent stem cells.42–45 Besides, in damaged joint tissues, BMSCs tend to differentiate into fibrochondrocytes, which leads to the formation of fibrocartilage repair at the injury site.46 The present study evaluated the in vivo anti-OA effects of combined treatment of MF and PL on an OA rat model by the modified Hulth method and clinical OA patients and explored the cellular and molecular mode of action of PL on BMSCs. In vivo data showed that the combined treatment of MF and PL had multiple positive effects on OA by ameliorating joint pain, protecting chondrocytes, and inhibiting synovial fibrosis (Figures 2–4). The anti-OA effect of the combined treatment of MF and PL was superior to that of MF alone (p < 0.05), suggesting that the combined treatment of MF and PL had a synergistic effect on the treatment of OA (Figure 3). Moreover, PL application also improved MF-induced cartilage fibrosis (down-regulation of Col1, Col3, α-SMA and Ctgf) (Figure 4). In vitro data showed that PL could induce cellular chondrogenic differentiation and migration of BMSCs, suggesting that PL facilitated stem cell homing to the cartilage injury sites and promoted cartilage repair and regeneration (Figures 5 and 6). Based on the previous reports, we focused on HGF and IGF-1, evaluated their anti-fibrotic effects on chondrocytes, and compared them with PL. Results showed that the combination of HGF and IGF-1 exerted effects close to PL, indicating these two growth factors play a major role in PL (Figure 7). Consistently, the clinical retrospective study validated the anti-OA efficacy of the combined treatment of MF and PL (Figure 8). The main innovation and characteristic points of this study are: (1) both experimental and clinical determination of anti-OA efficacy and safety of the combined treatment of MF and PL; (2) the comparison of therapeutic effects between MF alone and the combined treatment of MF and PL; and (3) the application of PL in reducing MF-induced cartilage fibrosis and facilitating cartilage repair.
BMSCs are a subpopulation of non-hematopoietic cell-derived adult stem cells present in the bone marrow stroma with high proliferation, chemotactic migration and self-renewal abilities, and multidirectional differentiation ability under different induction conditions.24 Our results showed that PL could promote proliferation, migration and chondrogenic differentiation of BMSCs. Indeed, through interacting with tyrosine kinase receptors, human PL (hPL) has been found to increase the expressions of signal transducer and activator of transcription 3 (STAT3) and myelocytomatosis (MYC), both known as stimulators of cell proliferation.47 BMSCs cultured in expansion medium supplemented with hPL exhibited a higher proliferation rate than in the medium supplemented with FBS.48 Neutralization experiments have shown that inhibition of PDGF-BB and bFGF within PL reduced the proliferation rate of MSCs by approximately 20% and 50%, respectively.49 Besides, PL could promote the expression of high mobility group box-1 (HMGB1), which can induce cell proliferation and migration.50 Another study showed that PL could be used as an alternative to FBS for clinical-scale expansion of MSCs, and MSCs cultured in the presence of PL maintained their trilineage differentiation potential and immunomodulatory properties.51
PL contained various growth factors (eg, PDGF, TGF‐β, IGF‐1, EGF, HGF and FGF), which have been shown to play important roles in cell proliferation, cell migration, chondrogenic differentiation of MSCs, tissue regeneration and repair, including cartilage repair, wound healing, and anti-fibrotic therapy.28,36,52 For instance, PDGF-BB was reported to promote the recruitment and homing of MSCs and improve the adherent microenvironment, and therefore attenuated OA progression.53–55 TGF-β1 was shown to induce a SMAD3-dependent nuclear aggregation of β-catenin promoting the proliferation of BMSCs, while TGF-β2 and TGF-β3 showed superior capacity in inducing chondrogenic differentiation of BMSCs.56,57 Previous studies have reported that IGF1 could not only stimulate proliferation and chondrogenic differentiation of MSCs, but also enhance the paracrine activity of MSCs, which contributed to cartilage regeneration and repair.58,59 Our previous study showed that the proliferation rate of huc-MSCs treated with EGF was approaching to that PL, suggesting that EGF was a major contributor to the pro-proliferative effect of PL.28 Several studies have shown that FGF-2 could promote MSCs proliferation through the activation of PI3K-Akt, ERK1/2 and JNK signaling pathways.60,61 In addition, IGF-1 can inhibit cardiac fibrosis by targeting α-SMA, and HGF can inhibit peritoneal fibrosis and pulmonary fibrosis in mice.62–64 Our study found that the combination of HGF and IGF-1 exerted effects similar to those of PL, indicating these two growth factors were the main antifibrotic components in PL. Taken together, different combinations of recombinant growth factors may be incorporated with MF to improve its clinical outcome and generate high-quality cartilage.
We for the first time show the anti-OA and antifibrosis effects via the combination of MF and PL. The combined treatment of MF and PL significantly alleviated joint pain, protected chondrocytes and inhibited synovial fibrosis in OA rats, and PL induced cellular chondrogenic differentiation and migration of BMSCs, suggesting that PL facilitated stem cell homing to the cartilage injury sites and promoted cartilage repair and regeneration. The limitation of this study is that the anti-fibrosis mechanism of PL was not studied, and we only detected the fibrosis phenotype. The clinical data showed significant improvements in pain reduction and cartilage repair in OA patients. Our study provides new insights into the combined treatment of MF and PL for OA, and the findings can guide the different combinations of recombinant growth factors with MF to improve their clinical efficacy and produce high-quality cartilage.
Some limitations exist in this study. In this study, the efficacy of MF combined with PL therapy was assessed in this study primarily by clinical parameters. Meniscal damage and joint effusion in MRI images were not designated as primary endpoints. Building on these findings, future prospective investigations incorporating serial MRI assessments will be planned to systematically evaluate structural modifications in meniscal integrity and synovial fluid parameters after MF combined with PL treatment.
Conclusion
We for the first time show the anti-OA and antifibrosis effects via the combination of MF and PL. The combined treatment of MF and PL significantly alleviated joint pain, protected chondrocytes and inhibited synovial fibrosis on OA rats, and PL induced cellular chondrogenic differentiation and migration of BMSCs, suggesting that PL facilitated stem cell homing to the cartilage injury sites and promoted cartilage repair and regeneration. The clinical data showed significant improvements of pain reduction and cartilage repair in OA patients. The animal experiment, cell experiment and clinical retrospective study are closely linked, forming a logical process from preclinical investigation to mechanism understanding and then clinical verification. Together, the three parts provided a comprehensive and coherent narrative that highlights the central topic: the combined treatment of MF and PL represents a promising strategy to enhance OA cartilage repair and anti-fibrosis, supported by strong evidence at the molecular, preclinical, and clinical levels.
Abbreviations
MF, microfracture; OA, osteoarthritis; PL, platelet lysate; BMSCs, bone mesenchymal stem cells; Col1, collagen type I; Col3, collagen type III; α-SMA, alpha-smooth muscle actin; Col2, collagen type II; Sox9, sry-related high-mobility group box 9; Ctgf, connective tissue growth factors; Mmp13, matrix metallopeptidase 13; Vegf, vascular endothelial growth factor; PDGF, platelet derived growth factor; IGF, insulin-like growth factor; EGF, basic epidermal growth factor; FGF, fibroblast growth factor; HGF, hepatocyte growth factor; TGF-β, transforming growth factor-β.
Ethical Statement
All animal experimental procedures were performed according to the guidelines for the Care and Use of Laboratory Animals of the National Institutes of Health and were approved by the Medical Regulation and Ethics Committee of Zhejiang Chinese Medical University (Approval No. 20231120-25).
Acknowledgments
The graphical abstract was Created in BioRender. Zhang, H. (2025) https://BioRender.com/j77y800. We appreciate the great help from the Medical Research Center, Academy of Chinese Medical Sciences, Zhejiang Chinese Medical University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Natural Science Foundation of China (grant numbers 82274373 and 82474367), Zhejiang Provincial Key Research and Development Program (grant number 2021C03046), the Health and Family Planning Science and Technology Plan General Program of Hangzhou (grant number B20200382), Zhejiang Province Postdoctoral Scientific Research Merit-based Funding Project (grant number ZJ2022058), Zhejiang Chinese Medical University Scientific Research Project Fund (grant numbers 2022RCZXZK22, 2023JKZKTS29 and 2021JKZDZC05), the Natural Science Foundation of Zhejiang Province (grant number LGF22H060032), and the Talent Project under the University-Level Scientific Research Program of Zhejiang Chinese Medical University (grant number 2024RCZXZK56).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yao Q, Wu X, Tao C, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduction Target Ther. 2023;8(1):56. doi:10.1038/s41392-023-01330-w
2. Carneiro DC, Araújo LT, Santos GC, et al. Clinical Trials with Mesenchymal Stem Cell Therapies for Osteoarthritis: challenges in the Regeneration of Articular Cartilage. Int J mol Sci. 2023;24(12). doi:10.3390/ijms24129939
3. Wu Y, Li J, Zeng Y, et al. Exosomes rewire the cartilage microenvironment in osteoarthritis: from intercellular communication to therapeutic strategies. Int J Oral Sci. 2022;14(1):40. doi:10.1038/s41368-022-00187-z
4. Fan X, Ong LJY, Sun AR, Prasadam I. From polarity to pathology: decoding the role of cell orientation in osteoarthritis. J Orthopaedic Transl. 2024;49:62–73. doi:10.1016/j.jot.2024.09.004
5. Su S, Tian R, Jiao Y, et al. Ubiquitination and deubiquitination: implications for the pathogenesis and treatment of osteoarthritis. J Orthopaedic Transl. 2024;49:156–166.
6. Conaghan PG, Cook AD, Hamilton JA, Tak PP. Therapeutic options for targeting inflammatory osteoarthritis pain. Nat Rev Rheumatol. 2019;15(6):355–363. doi:10.1038/s41584-019-0221-y
7. Xie J, Huang Z, Yu X, Zhou L, Pei F. Clinical implications of macrophage dysfunction in the development of osteoarthritis of the knee. Cytokine Growth Factor Rev. 2019;46:36–44. doi:10.1016/j.cytogfr.2019.03.004
8. Xiang XN, Zhu SY, He HC, Yu X, Xu Y, He CQ. Mesenchymal stromal cell-based therapy for cartilage regeneration in knee osteoarthritis. Stem Cell Res Ther. 2022;13(1):14. doi:10.1186/s13287-021-02689-9
9. Jeyaraman M, Maffulli N, Gupta A. Stromal Vascular Fraction in Osteoarthritis of the Knee. Biomedicines. 2023;11(5). doi:10.3390/biomedicines11051460
10. Abramoff B, Caldera FE. Osteoarthritis: pathology, Diagnosis, and Treatment Options. Med Clin North Am. 2020;104(2):293–311. doi:10.1016/j.mcna.2019.10.007
11. Wang X, Wang D, Deng B, Yan L. Syringaresinol attenuates osteoarthritis via regulating the NF-κB pathway. Int Immunopharmacol. 2023;118:109982. doi:10.1016/j.intimp.2023.109982
12. Makris EA, Gomoll AH, Malizos KN, Hu JC, Athanasiou KA. Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol. 2015;11(1):21–34. doi:10.1038/nrrheum.2014.157
13. Bendich I, Zhang N, Barry JJ, Ward DT, Whooley MA, Kuo AC. Antibiotic-Laden Bone Cement Use and Revision Risk After Primary Total Knee Arthroplasty in U.S. Veterans. J Bone Joint Surg Am Vol. 2020;102(22):1939–1947. doi:10.2106/jbjs.20.00102
14. Risager SK, Viberg B, Abrahamsen CS, Arndt KB, Odgaard A, Lindberg-Larsen M. Patient-reported outcome 1 to 4 years after periprosthetic knee fracture: a nationwide cross-sectional matched study. Acta orthopaedica. 2025;96:209–216. doi:10.2340/17453674.2025.43083
15. Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthopaedics Related Res. 2001;2001(391 Suppl):S362–369. doi:10.1097/00003086-200110001-00033
16. Madry H, Gao L, Eichler H, Orth P, Cucchiarini M. Bone Marrow Aspirate Concentrate-Enhanced Marrow Stimulation of Chondral Defects. Stem Cells Int. 2017;2017:1609685. doi:10.1155/2017/1609685
17. Guo X, Ma Y, Min Y, et al. Progress and prospect of technical and regulatory challenges on tissue-engineered cartilage as therapeutic combination product. Bioact Mater. 2023;20:501–518. doi:10.1016/j.bioactmat.2022.06.015
18. Salzmann GM, Sah B, Südkamp NP, Niemeyer P. Clinical outcome following the first-line, single lesion microfracture at the knee joint. Archiv Orthopaed Trauma Surg. 2013;133(3):303–310. doi:10.1007/s00402-012-1660-y
19. Dekker TJ, Aman ZS, DePhillipo NN, Dickens JF, Anz AW, LaPrade RF. Chondral Lesions of the Knee: an Evidence-Based Approach. J Bone Joint Surg Am Vol. 2021;103(7):629–645. doi:10.2106/jbjs.20.01161
20. Hall AC. The Role of Chondrocyte Morphology and Volume in Controlling Phenotype-Implications for Osteoarthritis, Cartilage Repair, and Cartilage Engineering. Curr Rheumatol Rep. 2019;21(8):38. doi:10.1007/s11926-019-0837-6
21. Rim YA, Ju JH. The Role of Fibrosis in Osteoarthritis Progression. Life. 2020;11(1). doi:10.3390/life11010003
22. Sun Y, Wu Q, Dai K, You Y, Jiang W. Generating 3D-cultured organoids for pre-clinical modeling and treatment of degenerative joint disease. Signal Transduction Target Ther. 2021;6(1):380. doi:10.1038/s41392-021-00675-4
23. Kreuz PC, Steinwachs MR, Erggelet C, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006;14(11):1119–1125. doi:10.1016/j.joca.2006.05.003
24. Lin H, Sohn J, Shen H, Langhans MT, Tuan RS. Bone marrow mesenchymal stem cells: aging and tissue engineering applications to enhance bone healing. Biomaterials. 2019;203:96–110. doi:10.1016/j.biomaterials.2018.06.026
25. Szponder T, Latalski M, Danielewicz A, et al. Osteoarthritis: pathogenesis, Animal Models, and New Regenerative Therapies. J Clin Med. 2022;12(1). doi:10.3390/jcm12010005
26. Burnouf T, Goubran HA, Chen TM, Ou KL, El-Ekiaby M, Radosevic M. Blood-derived biomaterials and platelet growth factors in regenerative medicine. Blood Rev. 2013;27(2):77–89. doi:10.1016/j.blre.2013.02.001
27. Tang Q, Lim T, Wei XJ, et al. A free-standing multilayer film as a novel delivery carrier of platelet lysates for potential wound-dressing applications. Biomaterials. 2020;255:120138. doi:10.1016/j.biomaterials.2020.120138
28. Yan L, Zhou L, Yan B, et al. Growth factors-based beneficial effects of platelet lysate on umbilical cord-derived stem cells and their synergistic use in osteoarthritis treatment. Cell Death Dis. 2020;11(10):857. doi:10.1038/s41419-020-03045-0
29. Liang Y, Chen S, Yang Y, et al. Vasoactive intestinal peptide alleviates osteoarthritis effectively via inhibiting NF-κB signaling pathway. J Biomed Sci. 2018;25(1):25. doi:10.1186/s12929-018-0410-z
30. Xing L, Jiang Y, Gui J, et al. Microfracture combined with osteochondral paste implantation was more effective than microfracture alone for full-thickness cartilage repair. Knee Surgery Sports Traumatol Arthroscopy. 2013;21(8):1770–1776. doi:10.1007/s00167-012-2031-5
31. Zhang H, Bao R, Xu J, et al. Development and Evaluation of a Rat Model of Full-Thickness Cartilage Defects. J Visualized Experiment. 2023;2023(195). doi:10.3791/64475
32. Mankin HJ, Dorfman H, Lippiello L, Zarins A. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. II. Correlation of morphology with biochemical and metabolic data. J Bone Joint Surg Am Vol. 1971;53(3):523–537.
33. Glasson SS, Chambers MG, Van Den Berg WB, Little CB. The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the mouse. Osteoarthritis Cartilage. 2010;18(Suppl 3):S17–23. doi:10.1016/j.joca.2010.05.025
34. Krenn V, Morawietz L, Burmester GR, et al. Synovitis score: discrimination between chronic low-grade and high-grade synovitis. Histopathology. 2006;49(4):358–364. doi:10.1111/j.1365-2559.2006.02508.x
35. Li X, Zhang Y, Qi G. Evaluation of isolation methods and culture conditions for rat bone marrow mesenchymal stem cells. Cytotechnology. 2013;65(3):323–334. doi:10.1007/s10616-012-9497-3
36. Yan L, Zhou L, Xie D, et al. Chondroprotective effects of platelet lysate towards monoiodoacetate-induced arthritis by suppression of TNF-α-induced activation of NF-ĸB pathway in chondrocytes. Aging. 2019;11(9):2797–2811. doi:10.18632/aging.101952
37. Klatte-Schulz F, Schmidt T, Uckert M, et al. Comparative Analysis of Different Platelet Lysates and Platelet Rich Preparations to Stimulate Tendon Cell Biology: an In Vitro Study. Int J mol Sci. 2018;19(1). doi:10.3390/ijms19010212
38. Chen Z, Ge Y, Zhou L, et al. Pain relief and cartilage repair by Nanofat against osteoarthritis: preclinical and clinical evidence. Stem Cell Res Ther. 2021;12(1):477. doi:10.1186/s13287-021-02538-9
39. Cao H, Wang X, Chen M, et al. Childhood Cartilage ECM Enhances the Chondrogenesis of Endogenous Cells and Subchondral Bone Repair of the Unidirectional Collagen-dECM Scaffolds in Combination with Microfracture. ACS Appl Mater Interfaces. 2021;13(48):57043–57057. doi:10.1021/acsami.1c19447
40. Gou GH, Tseng FJ, Wang SH, et al. Autologous Chondrocyte Implantation Versus Microfracture in the Knee: a Meta-analysis and Systematic Review. Arthroscopy. 2020;36(1):289–303. doi:10.1016/j.arthro.2019.06.033
41. Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37(10):2053–2063. doi:10.1177/0363546508328414
42. Wang X, Cai Y, Wu C, et al. Conversion of senescent cartilage into a pro-chondrogenic microenvironment with antibody-functionalized copper sulfate nanoparticles for efficient osteoarthritis therapy. J Nanobiotechnol. 2023;21(1):258. doi:10.1186/s12951-023-02036-5
43. Li M, Yin H, Yan Z, et al. The immune microenvironment in cartilage injury and repair. Acta Biomater. 2022;140:23–42. doi:10.1016/j.actbio.2021.12.006
44. Fan M, Tong P, Yan L, et al. Detrimental alteration of mesenchymal stem cells by an articular inflammatory microenvironment results in deterioration of osteoarthritis. BMC Med. 2023;21(1):215. doi:10.1186/s12916-023-02923-6
45. Boulestreau J, Maumus M, Jorgensen C, Noël D. Extracellular vesicles from mesenchymal stromal cells: therapeutic perspectives for targeting senescence in osteoarthritis. Adv Drug Delivery Rev. 2021;175:113836. doi:10.1016/j.addr.2021.113836
46. Mustapich T, Schwartz J, Palacios P, Liang H, Sgaglione N, Grande DA. A Novel Strategy to Enhance Microfracture Treatment With Stromal Cell-Derived Factor-1 in a Rat Model. Front Cell Develop Biol. 2020;8:595932. doi:10.3389/fcell.2020.595932
47. Oeller M, Jaksch-Bogensperger H, Templin M, et al. Transcription Factors STAT3 and MYC Are Key Players of Human Platelet Lysate-Induced Cell Proliferation. Int J mol Sci. 2022;23(24). doi:10.3390/ijms232415782
48. Karadjian M, Senger AS, Essers C, et al. Human Platelet Lysate Can Replace Fetal Calf Serum as a Protein Source to Promote Expansion and Osteogenic Differentiation of Human Bone-Marrow-Derived Mesenchymal Stromal Cells. Cells. 2020;9(4). doi:10.3390/cells9040918
49. Fekete N, Gadelorge M, Fürst D, et al. Platelet lysate from whole blood-derived pooled platelet concentrates and apheresis-derived platelet concentrates for the isolation and expansion of human bone marrow mesenchymal stromal cells: production process, content and identification of active components. Cytotherapy. 2012;14(5):540–554. doi:10.3109/14653249.2012.655420
50. Romaldini A, Ulivi V, Nardini M, Mastrogiacomo M, Cancedda R, Descalzi F. Platelet Lysate Inhibits NF-κB Activation and Induces Proliferation and an Alert State in Quiescent Human Umbilical Vein Endothelial Cells Retaining Their Differentiation Capability. Cells. 2019;8(4). doi:10.3390/cells8040331
51. Astori G, Amati E, Bambi F, et al. Platelet lysate as a substitute for animal serum for the ex-vivo expansion of mesenchymal stem/stromal cells: present and future. Stem Cell Res Ther. 2016;7(1):93. doi:10.1186/s13287-016-0352-x
52. Xiao X, Xu J, Wang C, et al. Porcine platelet lysates exert the efficacy of chondroregeneration and SMAD2-mediated anti-chondrofibrosis on knee osteoarthritis. Int Immunopharmacol. 2024;128:111509. doi:10.1016/j.intimp.2024.111509
53. Li X, Li X, Yang J, et al. Living and Injectable Porous Hydrogel Microsphere with Paracrine Activity for Cartilage Regeneration. Small. 2023;19(17):e2207211. doi:10.1002/smll.202207211
54. Vainieri ML, Lolli A, Kops N, et al. Evaluation of biomimetic hyaluronic-based hydrogels with enhanced endogenous cell recruitment and cartilage matrix formation. Acta Biomater. 2020;101:293–303. doi:10.1016/j.actbio.2019.11.015
55. Hao L, Tianyuan Z, Zhen Y, et al. Biofabrication of cell-free dual drug-releasing biomimetic scaffolds for meniscal regeneration. Biofabrication. 2021;14(1). doi:10.1088/1758-5090/ac2cd7
56. Jian H, Shen X, Liu I, Semenov M, He X, Wang XF. Smad3-dependent nuclear translocation of beta-catenin is required for TGF-beta1-induced proliferation of bone marrow-derived adult human mesenchymal stem cells. Genes Dev. 2006;20(6):666–674. doi:10.1101/gad.1388806
57. Barry F, Boynton RE, Liu B, Murphy JM. Chondrogenic differentiation of mesenchymal stem cells from bone marrow: differentiation-dependent gene expression of matrix components. Exp Cell Res. 2001;268(2):189–200. doi:10.1006/excr.2001.5278
58. Xie M, Zhang Y, Xiong Z, et al. Generation of hyaline-like cartilage tissue from human mesenchymal stromal cells within the self-generated extracellular matrix. Acta Biomater. 2022;149:150–166. doi:10.1016/j.actbio.2022.06.040
59. Qazi TH, Mooney DJ, Duda GN, Geissler S. Niche-mimicking interactions in peptide-functionalized 3D hydrogels amplify mesenchymal stromal cell paracrine effects. Biomaterials. 2020;230:119639. doi:10.1016/j.biomaterials.2019.119639
60. Choi SC, Kim SJ, Choi JH, Park CY, Shim WJ, Lim DS. Fibroblast growth factor-2 and −4 promote the proliferation of bone marrow mesenchymal stem cells by the activation of the PI3K-Akt and ERK1/2 signaling pathways. Stem Cells Develop. 2008;17(4):725–736. doi:10.1089/scd.2007.0230
61. Ahn HJ, Lee WJ, Kwack K, Kwon YD. FGF2 stimulates the proliferation of human mesenchymal stem cells through the transient activation of JNK signaling. FEBS Lett. 2009;583(17):2922–2926. doi:10.1016/j.febslet.2009.07.056
62. Ock S, Ham W, Kang CW, Kang H, Lee WS, Kim J. IGF-1 protects against angiotensin II-induced cardiac fibrosis by targeting αSMA. Cell Death Dis. 2021;12(7):688. doi:10.1038/s41419-021-03965-5
63. Obata Y, Abe K, Miyazaki M, Koji T, Tabata Y, Nishino T. The Transfer of the Hepatocyte Growth Factor Gene by Macrophages Ameliorates the Progression of Peritoneal Fibrosis in Mice. Int J mol Sci. 2023;24(8). doi:10.3390/ijms24086951
64. Bao R, Wang Q, Yu M, et al. AAV9-HGF cooperating with TGF-beta/Smad inhibitor attenuates silicosis fibrosis via inhibiting ferroptosis. Biomed Pharmacothe. 2023;161:114537. doi:10.1016/j.biopha.2023.114537
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Network Analysis of Osteoarthritis Progression Using a Steiner Minimal Tree Algorithm
Xie Y, Shao F, Ji Y, Feng D, Wang L, Huang Z, Wu S, Sun F, Jiang H, Miyamoto A, Wang H, Zhang C
Journal of Inflammation Research 2024, 17:3201-3209
Published Date: 18 May 2024








