Back to Journals » Infection and Drug Resistance » Volume 18
Epidemiology and Molecular Drug-Resistance Patterns of Tuberculosis in Non-Elderly Patients in Luoyang, China, 2019-2023
Authors Wang Z, Xu L, Guo T, Liu J, Jin J, Zhang Q, Jiang T, Zhao Z, Xue Y
Received 7 March 2025
Accepted for publication 30 May 2025
Published 24 June 2025 Volume 2025:18 Pages 3087—3101
DOI https://doi.org/10.2147/IDR.S524300
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Oliver Planz
Zhenzhen Wang,1,2,* Liyang Xu,2,3,* Tengfei Guo,1 Jinwei Liu,1 Junrong Jin,1 Qing Zhang,1 Tao Jiang,1 Zhanqin Zhao,4 Yun Xue2
1The First Affiliated Hospital, and College of Clinical Medicine of Henan University of Science and Technology, Luoyang, Henan, People’s Republic of China; 2School of Medical Technology and Engineering, Henan University of Science and Technology, Luoyang, Henan, People’s Republic of China; 3Luoyang Center for Disease Control and Prevention, Luoyang, Henan, People’s Republic of China; 4Animal Science and Technology, Henan University of Science and Technology, Luoyang, Henan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yun Xue, School of Medical Technology and Engineering, Henan University of Science and Technology, No. 24 Jinghua Road, Jianxi District, Luoyang, Henan, People’s Republic of China, Tel +8613633799373, Email [email protected]
Purpose: Existing data offer limited guidance on TB control strategies for the non-elderly population, hampering effective epidemic management. This study aimed to analyze TB transmission and molecular resistance profiles among non-elderly patients (< 60 years) in Luoyang City.
Patients and Methods: From 2019– 2023, 24,706 non-duplicate sputum samples from 10 TB-designated hospitals were tested for Mycobacterium tuberculosis complex (MTBC) via IS6110-targeted real-time PCR. MTBC-positive specimens underwent multicolor melting curve analysis (MMCA) to assess resistance to isoniazid (INH), rifampin (RFP), streptomycin (SM), and ethambutol (EMB). Age-stratified analyses were performed to compare drug-resistant TB (DR-TB) prevalence between elderly and non-elderly groups, with multivariate regression identifying resistance risk factors in non-elderly patients.
Results: Non-elderly individuals exhibited significantly higher TB (17.54% vs 15.26%) and DR-TB (26.82% vs 21.62%) rates than the elderly (all, P < 0.001). Among non-elderly patients, males, retreatment cases, main urban residents and smear-positive groups had significantly elevated MTBC detection rates. The predominant resistance patterns of multidrug-resistant tuberculosis (MDR-TB) and poly-resistant tuberculosis (PDR-TB) were MDR4 (INH + RFP + EMB + SM) and PDR2 (INH + SM), with detection rates of 5.52% (142) and 2.33% (60), respectively. MTBC positive rate peaked at 30– 34 years (23.10%), while the resistance rate peaked at 35– 39 years. After adjusting for the effects of smear results and diagnosis year, the multivariate regression analysis model indicated that male sex, retreatment, and the main urban area were high-risk factors for TB resistance in non-elderly cases.
Conclusion: The non-elderly population demonstrates a significantly higher burden of both TB detection and resistance, particularly among males, retreatment cases, and main urban patients. The emergence of complex drug resistance patterns, combined with a distinct trend of younger age at infection, highlights the critical need for targeted interventions tailored to specific epidemiological and resistance profiles of MTBC-infected populations.
Keywords: TB, non-elderly, dissemination, molecular resistance
Introduction
TB remains a major respiratory infectious disease and persistent public health threat. As of 2022, an estimated 10.6 million new cases of TB (95% UI: 9.9–11.4 million) and around 1.3 million (95% UI: 1.18–1.43 million) TB-related deaths.1 Despite a gradual decline in incidence, China still bears a heavy TB burden.2 In 2022, the incidence rate was 52 per 100,000, far from the 33 per 100,000 target set by the WHO’s “End TB Strategy” for 2025, highlighting the urgency of enhanced control efforts.3 China’s TB epidemiology exhibits marked complexity due to vast geographic disparities, uneven economic development, and heterogeneous population dynamics.4 The COVID-19 pandemic has substantially exacerbated this complex scenario. Multiple factors including diagnostic delays, treatment interruptions, immunological interactions between the diseases, and socioeconomic determinants have significantly altered TB epidemiological characteristics.5
Distinct age groups exhibit differences in TB epidemiological characteristics, clinical phenotypes, and sociobehavioral factors.6 Elderly patients, affected by immunosenescence and polypharmacy, need integrated interventions combining TB and comorbidity management.7 In contrast, non-elderly individuals often struggle with treatment adherence due to occupational/academic pressures, drug tolerance, and lack of psychosocial support.8–11 Therefore, the implementation of age-stratified precision prevention and development of differentiated control measures tailored to the specific needs of each age group are essential for effectively reducing TB transmission and associated public health burdens.
In recent years, Luoyang’s accelerating urbanization and tourism growth have intensified population mobility - a recognized TB transmission amplifier.12 Despite the implementation of a centralized TB diagnosis and treatment model locally, significant differences exist between elderly and non-elderly patients regarding epidemiological features, social behavioral patterns, and drug resistance risks.13 Since 2022, systematic analyses of the region’s TB epidemiology and drug resistance patterns have revealed that TB transmission and drug-resistant TB are predominantly concentrated in the non-elderly population (<60 years).14,15 Nevertheless, key aspects of TB in this groups—including transmission characteristics, drug resistance distribution, nd risk factors — remain poorly understood. This limitations in TB surveillance data hinder accurate assessment of the disease burden in non-elderly populations and obscure a deeper understanding of TB and drug resistance risks in this group.
This study aims to comprehensively delineate the TB epidemic among Luoyang’s non-elderly population, generating evidence to guide the design of context-specific control measures tailored to the region’s socioeconomic and healthcare landscape. The findings will also inform post-pandemic TB control strategies and enhance the evidence base for public health interventions against TB.
Materials and Methods
Study Area
Luoyang is an important industrial and tourist city in central China. Its main urban area encompasses six administrative regions, while nine county and township areas — Luanchuan, Luoning, Mengjin, Ruyang, Song, Xin’an, Yanshi, Yichuan, and Yiyang counties — fall under its jurisdiction. The city covers a total area of 15,230 square kilometers. By the end of 2023, its resident population was 7.0779 million, among which 5.662 million were under the age of 60.16
Study Design and Data Collection
We conducted a systematic retrospective analysis of the molecular epidemiology and drug-resistance patterns among non-elderly TB patients in Luoyang, China from January 2019 to December 2023., The sputum samples were collected from 24,706 patients at 10 designated TB medical institutions in Luoyang City (including one municipal-level in the main urban area and nine county-level in the county and township areas under its jurisdiction). The samples were then sent to Luoyang Infectious Disease Hospital for fluorescent real-time PCR testing to identify MTBC strains and assess their resistance to first-line anti-TB drugs. The results were stratified by age, with 9,545 elderly cases (≥ 60 years) and 15,161 non-elderly cases (< 60 years). The study aimed to further elucidate the tuberculosis prevalence among local non-elderly populations by comparing transmission dynamics and resistance patterns between the two age groups.
According to the relevant provisions of the Law of the People’s Republic of China on the Protection of the Rights and Interests of the Elderly, non-elderly and elderly people refer to groups under the age of 60 (<60 years) and 60 years or older(≥60 years), respectively.17 Information such as the gender, age, and history of TB treatment was collected by trained medical personnel from the electronic medical records (EMRs) and TB reporting system.
Laboratory Methods
Strain Identification
According to the requirements of the experiment, the sputum samples of patients treated in designated TB hospitals were collected, and were sent to the laboratory by special personnel and special vehicles.18 After checking the sample numbers, acid staining and microscopic examination were carried out to determine the quality of sputum samples.19 When recording the results of acid-fast staining, for unqualified specimens, we arranged for the patient to collect the sputum specimen again after further professional guidance. For qualified sputum specimens, the nucleic acid extraction and real-time fluorescence PCR analysis were carried out in strict accordance with the instructions of commercial reagents (Zhishan, Xiamen), and the MTBC-specific insertion sequence 6110 (IS6110) was detected to confirm whether the isolate was an MTBC member.
Molecular Susceptibility Testing
For the specimens with a positive identification of MTBC strains, the MMCA technique is performed to determine the molecular mutation mechanisms underlying their resistance to the first-line anti-TB drugs. The INH resistance (INH-R) detection region focused on mutations in the ahpC promoter (−44 to −30 and −15 to 3 sites), inhA94 codon, inhA promoter (−17 to −8 sites), and katG315 codon. The detection region for RFP resistance (RFP-R) focuses on the mutation status within the region of 27 amino acid codons (81 base pairs, the rifampicin resistance-determining region) from the codon 507–533 of the rpoB gene. The EMB resistance (EMB-R) detection region were mutations at codon embB306, embB378, embB406, and embB497. The SM resistance (SM-R) detection regions were mutations at codons 43 and 88 of the gene rpsL, as well as the codons 513–517 and 905–908 of the gene rrs. The drug resistance detection is carried out in accordance with the standard operating procedures of the commercial kit instructions (Zhishan, Xiamen), and the quality control operations are performed as required.
Quality Control
The experimental operations, data analysis, and the execution of quality procedures are all carried out by two professional personnel. This laboratory is regularly evaluated by the national reference laboratory. The positive control is a plasmid containing the wild-type amplified target gene (the natural, non-mutated form of the gene). The negative control is a solution containing no target gene (Tris, EDTA·2H2O sodium, and Triton X-100). Negative/positive quality control was established for each batch of experiments to assess the experimental quality and ensure the reliability of the experimental results.
Inclusion and Exclusion Criteria
Inclusion criteria: Sputum specimens were collected from non-elderly patients (including TB-confirmed and TB-suspected cases) at designated tuberculosis hospitals between 2019 and 2023.20 Prior to analysis, duplicate cases were excluded through cross-referencing demographic data (including name, gender, date of birth, TB treatment history, and geographic origin). Furthermore, sputum specimens failing to meet quality standards - including those with volume <1 mL, excessively watery consistency, or visible contaminants (eg, food particles or pigmentation) - were excluded based on acid-fast staining criteria (specimens containing ≥10 squamous epithelial cells or ≤25 white blood cells per low-power field were considered inadequate).21
Statistical Analysis
Pearson’s chi-square test and Fisher’s exact test were used to determine the distribution differences of MTBC positivity and drug resistance between the non-elderly and elderly groups. The age distribution trend charts of local MTBC dissemination and different drug-resistance types were mapped. Then, variables potentially associated with drug-resistance outcomes were included in a multivariate logistic regression model to identify the risk factors for TB drug resistance in the non-elderly group. The odds ratio and the 95% confidence interval were used as relevant measures, and a p-value less than 0.05 was considered statistically significant. All analyses were conducted using STATA/SE 15.1.
Results
Patients’ Characteristics
A total of 24,706 non-replicate samples were included in this study. The number of samples in the non-elderly group (<60 years) was 1.46 times that of the elderly group (≥60 years), with 14,673 samples in the non-elderly group and 10,033 samples in the elderly group. Among the non-elderly group, there were more males (66.47% vs 33.53%), newly diagnosed patients (96.23% vs 3.77%), individuals from county and township areas (81.11% vs 18.89%), and smear-negative cases (86.04% vs 13.96%). The distribution characteristics of the elderly group in terms of gender, treatment history, and regional origin were similar to those of the non-elderly group (Table 1).
 |
Table 1 Clinical and Demographic Characteristics of Participating Numbers |
Epidemiological Characteristics of MTBC
The detection rate of MTBC was significantly higher in the non-elderly group than in the elderly group (17.54% vs 15.26%, P < 0.001). The differences in the positive rate of MTBC between the non-elderly and the elderly were also observed in subgroups of males, females, new patients, county and township area cases, smear-negative patients, and smear-positive patients (19.16% vs 16.46%, P < 0.001; 14.31% vs 12.58%, P = 0.028; 16.33% vs 14.04%, P < 0.001; 13.21% vs 11.34%, P < 0.001; 6.98% vs 6.06%, P = 0.008; 82.62% vs 78.14%, P = 0.001). While in the main urban area, the detection rate of MTBC is higher among the elderly population (39.83% vs 31.82%, P < 0.001).
In the non-elderly population, the detection rate of MTBC showed a downward trend, with a statistically significant difference between 2019 and 2023 (25.01% vs 17.69%, P < 0.001). And, the males, retreatment patients, main urban cases, and smear-positive patients had higher MTBC detection rates (19.16% vs 14.31%, P < 0.001; 48.28% vs 16.33%, P < 0.001; 31.82% vs 13.21%, P < 0.001; 82.62% vs 6.98%, P < 0.001). The characteristics of population distribution related to MTBC dissemination in the elderly population were highly consistent with those of the overall non-elderly population (Table 2).
 |
Table 2 Differences in MTBC Detection Between Elderly and Non-Elderly |
Drug-Resistance Patterns
Among the non-elderly population, 26.82% (690) were DR-TB cases. The detection rates of resistance to first-line anti-TB drugs from high to low were INH (19.70%) > SM (18.42%) > RFP (14.81%) > EMB (7.66%). The detection rate of mono-resistant tuberculosis (MR-TB) was 10.30% (265), with MR-TB(SM) and MR-TB(INH) having high detection rates, accounting for 4.28% and 4.35%, respectively. The detection rates of different resistance patterns of MDR from high to low were MDR4 (INH + RFP + EMB + SM) at 5.52%, MDR3 (INH + RFP + SM) at 4.47%, MDR1 (INH + RFP) at 1.98%, MDR2 (INH + RFP + EMB) at 0.54%. While, PDR2 (INH + SM) had the highest detection rate among the PDR, reaching 2.33% (60). The detection rates of INH-R, RFP-R, SM-R, MR, and MDR in non-elderly TB patients were higher compared with those in elderly TB patients (19.70% vs 14.89%, P < 0.001; 14.81% vs 9.60%, P < 0.001; 18.42% vs 15.41%, P = 0.014; 10.30% vs 8.36%, P = 0.041; 12.51% vs 7.51%, P < 0.001). However, the differences in the detection rates of various patterns of MR and MDR2 (INH + RFP + EMB) were not significant between the two groups. The PDR had a higher detection rate in the older population (5.75% vs 4.00%, P = 0.010), but this difference was only significant in the detection of PDR6 (0.72% vs 0.16%, P = 0.006) (Table 3).
 |
Table 3 Drug Resistance Patterns of MTBC Between Elderly and Non-Elderly |
MTBC Positive and Drug Resistance Age Distribution Trends
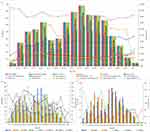
The median age of the MTBC positive group was 53.5 years (IQR: 34, 66). The highest overall detection rate of MTBC was observed in the 30–34 age group (23.10%), followed by the 20–24 age group (22.84%).In the overall population and each subgroup classified by variables (county and townships, main urban, males, new cases, previously treated cases, smear-positive, smear-negative), the age range with the highest absolute number of MTBC detections was 55–59 years old, with case numbers being 440, 261, 179, 364, 391, 149, 293, and 147 respectively. However, for females, the age range with the highest number of detections was 30–34 years old, with 123 cases. The peak MTBC detection rates in county and township areas, among males, and in the overall population were observed in the 30–34 age group, reaching 17.64%, 22.98%, and 23.10% respectively. Among the female, new patient, and smear-negative case groups, the highest MTBC detection rates were in the ≥ 90 age group (27.27%, 22.64%, and 10.23% respectively). However, the detection rates were also notably high in the 20–24 age group, at 24.12%, 21.81%, and 10.24% respectively. The MTBC detection rate peaked at 48.25% in the main urban area group at 80–84 years of age, 67.74% in the retreatment group at 35–39 years of age, and the overall detection rate was high in the smear-positive group, peaking at 94.44% at < 15 years of age (Figure 1A). The median ages of INH-R, RFP-R, EMB-R, and SM-R were 52 years (IQR: 34, 63), 49 years (IQR: 32, 61), 51 years (IQR: 32, 61), and 50 years (IQR: 33, 64), respectively. The highest resistance rates of INH, RFP and SM were all concentrated in the age group of 35–39 years, at 27.51%, 21.69% and 25.93%, respectively. The age range of peak EMB-R rate was 20–24 years old (11.95%), while there was also a high detection rate (11.64%) at 35–39 years (Figure 1B). The median ages of MR, MDR and PDR were 53 years (IQR: 35, 64), 48 years (IQR: 32, 61), and 57 years (IQR: 36, 70) respectively. The highest detection rates of them were concentrated in the age groups of 50–54 years, 35–39 years, and 60–64 years respectively, at 11.93%, 18.82%, and 6.97% respectively (Figure 1C). Note: In the analysis of drug resistance patterns in different subgroups stratified by age category, the groups aged under 15 years and over 91 years were not included in the statistics due to the small number of drug-resistant cases.
Risk Factor Analysis for Resistance Outcome
In the multivariable logistic regression model, after accounting for the effects of sputum smear and detection year, males had 1.655 times (95% CI: 1.300, 2.107), 1.795 times (95% CI: 1.356, 2.377), 1.413 times (95% CI: 1.112, 1.795), 1.428 times (95% CI: 1.051, 1.941), and 1.702 times (95% CI: 1.263, 2.294) higher odds than females for INH-R, RFP-R, SM-R, MR and MDR, respectively. Individuals with a history of TB treatment had 1.531 times (95% CI: 1.137, 2.060), 2.112 times (95% CI: 1.547, 2.882), 1.854 times (95% CI: 1.242, 2.768), 2.030 times (95% CI: 1.521, 2.708), and 2.034 times (95% CI: 1.463, 2.827) higher odds than new patients with INH-R, RFP-R, EMB-R, SM-R and MDR, respectively. Main urban residents had 1.685 times (95% CI: 1.376, 2.062), 1.553 times (95% CI: 1.237, 1.951), 1.633 times (95% CI: 1.205, 2.212), 1.577 times (95% CI: 1.280, 1.942), 1.562 times (95% CI: 1.120, 2.032), 1.542 times (95% CI: 1.209, 1.968), and 1.528 times (95% CI: 1.020, 2.290) higher odds than those in county and township areas of being diagnosed with INH-R, RFP-R, EMB-R, SM-R, MR, MDR and PDR, respectively (Table 4).
 |
Table 4 The Model of Multinomial Logistic Regression for the First-Line Anti-TB Drugs |
Resistance Rate Differences During Different Stages of the COVID-19 Pandemic (2019, 2020 - 2022, 2023)
We divided the diagnosis years into three stages: “pre-COVID-19”, “mid-COVID-19”, and “post-COVID-19”, corresponding to 2019, 2020–2022, and 2023 respectively. During the study period, the rate of TB resistance showed a downward trend. The significant declines were mainly observed between the “pre-COVID-19” and “mid-COVID-19” stages, and between the “pre-COVID-19” and “post-COVID-19” stages. Notably, the difference in the detection rate of SM-R was only evident between the “pre-COVID-19” and “post-COVID-19” stages (21.87% vs 15.11%, P = 0.007). However, when considering the resistance rate of INH-R alone, there was no statistically significant difference among the three stages. In addition, the detection rate of MR showed an upward trend and the most significant difference was between the “pre-COVID-19” and “mid-COVID-19” stages (7.66% vs 11.52%, P = 0.006). There was no statistically significant difference in all resistance pattern detection rates between the “mid-COVID-19” and “post-COVID-19” stages (Table 5).
 |
Table 5 Changes and Differences in the Detection Rate of Drug-Resistant Tuberculosis at Different Stages of COVID-19 (2019, 2020–2022, 2023) |
Discussion
TB is generally thought to threaten the elderly seriously because of physical decline, chronic diseases, malnutrition, and potential drug side-effects.22–24 However, the heterogeneous distribution of the transmission of TB and the resistance patterns is one of the main reasons for the challenges faced in TB management.25 The 2024 global TB report revealed that young and middle-aged adults (15–44 years) account for 53% of all pulmonary TB cases, and this age group comprises over 50% of newly diagnosed multidrug-resistant/rifampicin-resistant TB (MDR/RR-TB) cases annually.26 Dong et al showed that the risk of TB in people aged 20–24 years was similar to that in people aged 70–74 years.6 The detection of DR-TB in Qinghai Province was mainly concentrated among those aged 30–59 years.27 In Anhui, the group aged 41–60 had a higher resistance detection rate.28 In the Taiwan region, those over 65 years old are a high-burden group for MDR-TB.29 Study in Tianjin highlighted age (specifically, the patient group aged 40–59) as one of the crucial factors influencing the development of DR-TB.30 While, regions such as Ethiopia, Nigeria, Sudan, and Uganda exhibit a higher prevalence of TB among individuals aged 35–54 years.31 Our data suggests that local non-elderly have higher rates of TB detection and resistance. The local people aged 55–59 years accounted for a relatively high proportion of TB cases. However, the highest incidence of TB was in younger people aged 30–34 years. Under different variables, the highest incidence of TB was in people under 40 years old. Similarly, the first-line anti-TB drug resistance also exhibits similar characteristics, with the peak resistance rate concentrated between the ages of 20–34 years. Nowadays, non-elderly people are the main force in social construction. They are active in academia or profession and often gather in densely populated areas, which increases their chances of exposure to TB.32 In addition, some people in specific living environments, such as miners, livestock practitioners and other specific occupational groups, have an increased susceptibility to MTBC due to long-term exposure to high-dust and microbially contaminated environments.33 Furthermore, the detection rate of elderly TB is often atypical, making it prone to misdiagnosis and missed diagnosis, which affects the detection rate. Notably, the detection rate of TB in the elderly population in the main local urban area was significantly higher than that in the non-elderly. Now, China has entered a deeply aging society. The main urban area has attracted a large number of elderly people due to better medical resource allocation and relatively more economic opportunities, which has increased the burden of TB among the elderly.
Although the impact of gender on TB incidence is controversial, global data in 2022 showed that 55% of TB cases were males, and in China, 65% of new cases were males over 14 years old.1 A domestic study reported pulmonary TB in 84.4% of males, more than twice the rate in females.34 Globally, the male-to-female ratio of TB incidence generally ranges from 1.2 to 4.9.35 Our data show that the transmission of TB is more severe among non-elderly males, and the resistance situation is also more prominent. Males play important roles in society, which makes them socialize frequently and leads to a prevalence of unhealthy lifestyles such as tobacco dependence and excessive alcohol consumption among them.26 Some males have low health literacy, lack sufficient knowledge of TB prevention and control, and lack the awareness of active prevention and early screening.36 As a result, it is difficult to diagnose and intervene in a timely manner after MTBC infection. These factors significantly increase the risk of DR-TB infection. In addition, new evidence suggests that, apart from biological susceptibility and genetic polymorphism may also play a key potential role in the occurrence and development of TB in males.37–39 Carry out gender-sensitive health education, such as disseminating “cough screening” messages through male-frequented channels (eg, gas station broadcasts, sports venue posters) while avoiding stigmatizing language. Collaborative efforts with enterprises should be established to conduct on-site screening in male-dominated industries (transportation, construction) for early TB detection.40 Integrate smoking cessation/moderate alcohol consumption interventions, such as incorporating referral services for Nicotine Replacement Therapy (NRT) during the diagnosis and treatment of TB.41 Provide financial incentives (eg, transportation subsidies) to improve participation, so as to narrow the gender gap in TB detection.42
The dense population, high mobility, fast-paced life, and high psychological stress in main urban areas, along with rapid urbanization bringing in new migrants and industrial and traffic pollution weakening the body’s resistance, which are the main reasons for the relatively high TB burden in the main urban areas.43,44 In addition, combined with the comprehensive surveillance and reporting system that can detect and report TB in a timely manner, contribute to the high DR-TB detection rate in main urban areas.45 The WHO 2024 report highlights that 82% of global TB cases in the post-pandemic era occur in urban areas, a phenomenon exacerbated by healthcare access disruptions during the pandemic.46,47 Our data corroborate this finding, showing a 2.41 times higher detection rate in urban core areas compared to rural townships (31.82% vs 13.21%). Strengthen active screening in areas with concentrated floating populations in the main urban area (eg, via mobile X-ray units) and improved healthcare accessibility (eg, evening clinics) to reduce diagnostic delays would help mitigate transmission risks in high-density urban environments.48 Such measures could potentially interrupt community transmission chains and reduce the overall urban TB burden. Implementing customized health education programs tailored to urban living conditions, including promoting proper ventilation in enclosed living spaces and enhancing the capacity for preventive measures to reduce new cases, is also a highly effective measure.
For retreatment patients, delayed detection of drug-resistant strains, irregular and prolonged treatment, and adverse reactions resulting from drug interactions are the main obstacles to effectively managing this group.49 Targeted interventions can disrupt the chains of drug-resistance transmission caused by retreatment cases. Rapid molecular testing (such as GeneXpert) should be performed on all retreatment cases whenever possible to rule out drug resistance, thereby avoiding empirical medication use.50 For retreatment cases exhibiting complex drug resistance patterns, comprehensive drug susceptibility testing should be performed to develop personalized treatment regimens. The implementation of a combined “Directly Observed Treatment (DOT) with Concurrent Household Contact Screening” approach is recommended to optimize treatment supervision. Complementary social support measures, including nutritional supplementation and peer support programs utilizing successfully treated patients as educators, should be incorporated to minimize treatment discontinuation rates. Furthermore, establishing lifelong management for retreatment cases and maintaining long-term follow-up of close contacts are essential components of an effective drug-resistant TB control strategy.51,52
Compared with single drug resistance, the combined resistance patterns of anti-TB drugs were more serious in this area and vary by age. Among non-elderly TB cases, the detection rates of DR-TB and MDR-TB, accounting for 26.82% and 12.51% respectively, were higher than those in Shandong Province and the national baseline.35,53 The high drug resistance burden among young people poses a great challenge to local anti-TB cause. Young adults have insufficient knowledge of TB and poor treatment compliance. They often decline regular treatment because they experience only mild symptoms, which leads to a protracted illness.54,55 Therefore, enhancing their awareness of the importance of standardized treatment, detecting latent TB in this demographic as early as possible, and implementing the full-course supervised chemotherapy strategy are of great significance for the prevention and treatment of DR-TB.
After a long period of unremitting struggle against TB, the overall resistance rate of TB is showing a downward trend, which is a positive result at this stage of this long-term battle against TB. However, the COVID-19 pandemic has made the outcome of TB treatment uncertain. It is reported that the COVID-19 pandemic has offset the progress made in the global fight against TB over the years.56 Studies have shown that although the extensive spatial isolation measures during the COVID-19 pandemic have had a certain positive effect on the prevention and control of TB, their effectiveness cannot offset the negative impact caused by insufficient diagnosis.5 In 2021, the number of global TB deaths reached 1.6 million, marking the first increase in the global TB death toll since 2005.57 In 2023, the number of reported cases reached 8.2 million, hitting a historical peak since the establishment of the monitoring system in 1995.36 The conservative modeling by the TB/COVID-19 Global Research Group predicts that the TB mortality rate may increase by 20% within the next five years.58 Specifically, this impact is also clearly evident at the local level. Compared with the situation before the COVID-19 pandemic (in 2019), the decline in the detection rate and resistance rate of MTBC in the local area during the COVID-19 pandemic (from 2020 to 2022) requires a more objective and rational view. Of course, the significant decline in the rates of TB detection and resistance are the core indicators for measuring the effectiveness of anti-TB work, and they intuitively confirm the scientificity and effectiveness of the current prevention and control strategies. This achievement not only demonstrates the coordinated efforts of multi-dimensional measures such as the innovation of rapid diagnostic technologies, public health education for all, and the guarantee of medical insurance policies, but also provides a successful example that can be used for reference prevention and treatment of TB.59,60 Also, the impact of TB diagnosis and under-reporting at this stage on the actual data should be fully considered.61 In fact, the detection rate of MTBC has increased somewhat after the epidemic (2023) compared to the epidemic period (2020–2022). Although the detection rate of drug resistance still showed a downward trend, the detection rate of different TB resistance patterns did not decrease significantly. All these constantly remind us that after the COVID-19 pandemic, we should strengthen the monitoring and management of TB, improve diagnostic technology, allocate medical resources appropriately, and ensure the supply of anti-TB drugs. Implementing these measures will help offset or reverse the impact of COVID-19 on TB prevention and control, get the anti-TB cause back on track, and thus successfully achieve the “End TB Strategy” by 2035.62 His remains the focus of current TB control.
Our study has some limitations. Firstly, the subjects selected for the experiment were mostly high-risk groups who visited the designated TB medical institutions either on their own initiative or were referred after other medical treatments. Due to the non-mandatory nature of the selection, some groups may not have been fully monitored, which led to certain biases in the research data on TB among local high-risk groups. Secondly, although the quality screening of the experimental samples was very strict, most of the specimens were from patients’ self-expectorated sputum, lacking supervision throughout the whole process. As a result, some samples were not collected at the appropriate time and were affected by factors such as medication, resulting in the failure to detect the TB strains and drug-resistant loci in a timely manner. Despite these limitations, our study can still reflect the characteristics of TB spread and resistance across the entire city, including the main urban area and its subordinate county and township areas. This is of great significance for revealing the epidemiological characteristics of TB among high-risk groups. Meanwhile, our data cover the three periods before, during, and after the COVID-19 pandemic, which can help us better understand the prevalence of TB during the outbreaks of other infectious respiratory diseases and provide a reference for formulating more effective anti-TB plans in response to similar situations in the future.
Conclusion
This study revealed that TB prevalence and drug resistance among non-elderly (<60) were concerning in Luoyang, China, from 2019 to 2023. Among this population, males, the main urban patients, and retreatment cases showed higher TB detection rates and resistance risks. Despite the TB incidence overall decline, the trend of younger cases requires attention. The MTBC detection peak occurred in the 30–34 age group, while peak INH/RFP resistance and MDR-TB rates all clustered in the 35–39 cohort. Therefore, precise and targeted screening strategies is the focus of effective TB management. Active case-finding systems should be prioritized in male-dominated workplaces and urban migrant communities, ensuring to cover patients and close contacts. Directly observed therapy (DOT) combined with social support measures should be enforced for retreatment cases to reduce treatment interruptions and improve completion rates. The COVID-19 pandemic hindered the expected decline in the local TB detection and resistance rates. Thus, improving the post-pandemic monitoring system, establishing a dynamic TB resistance databases, and regularly screening high-risk populations are essential to address pandemic-related monitoring gaps. Overall, age- and risk-stratified prevention strategies are crucial. Surveillance high-risk groups to track resistant strains, and enhanced molecular resistance monitoring, will aid in developing effective drug resistance control programs and advancing TB prevention efforts.
Data Sharing Statement
Data can be made available through contact with the corresponding author.
Ethics Statement
This study was approved by the Ethics Review Committee of The First Affiliated Hospital and Clinical Medical College, Henan University of Science and Technology (Approval Registration Number - 2022/03/B070). The patients’ information was anonymized before the data analysis. This study was conducted in accordance with the Declaration of Helsinki. Considering the retrospective nature of the study and the anonymous data used for analysis, the ethics committee waived the requirement for informed consent forms.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Nature Science Foundation of China (32072899), Henan Science and Technology Development Plan (212102310741) and Joint construction project of Henan Province (LHGJ20200589).
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization. Global Tuberculosis Report 2023. Geneva: World Health Organization; 2023.
2. Zhu S, Xia L, Yu S, et al. The burden and challenges of tuberculosis in China: findings from the Global Burden of Disease Study 2015. Sci Rep. 2017;7(1):1746. doi:10.1038/s41598-017-15024-1
3. Wang XY, Jiang ML, Pang YJ, et al. Current status of tuberculosis burden in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2024;45(6):857–864. doi:10.3760/cma.j.cn112338-20240311-00111
4. Long Q, Qu Y, Lucas H. Drug-resistant tuberculosis control in China: progress and challenges. Infect Dis Poverty. 2016;5(1):9. doi:10.1186/s40249-016-0103-3
5. Liu Y, Sun R, Zhang H, et al. Trends and predictions of tuberculosis notification in mainland China during and after the COVID-19 pandemic. J Infect. 2023;87(6):e100–e103. doi:10.1016/j.jinf.2023.08.001
6. Dong Z, Wang QQ, Yu SC, et al. Age-period-cohort analysis of pulmonary tuberculosis reported incidence, China, 2006-2020. Infect Dis Poverty. 2022;11(1):85. doi:10.1186/s40249-022-01009-4
7. Han TT, Liu GZ, Chen QQ, et al. Interpretation of Framework for collaborative action on tuberculosis and comorbidities. Chin J Antituberc. 2023;45(1):25–30. doi:10.19982/j.issn.1000-6621.20220464
8. Liu X, Zhang L, Xu J, et al. Drug resistance and epidemiological characteristics of Mycobacterium tuberculosis in northern Zhejiang from 2018 to 2022. Adv Clin Med. 2023;13(11):18499–18506. doi:10.12677/ACM.2023.13112600
9. Wang X, Su B, Chen P, et al. Subspecies distribution and drug-resistance characteristics of Mycobacterium abscessus complex clinical isolates in South China. Microbiol Spectrum. 2025:
10. Gai X, Chi H, Li R, et al. Tuberculosis in infertility and in vitro fertilization-embryo transfer. Chinese Med J. 2024;137(20):2404–2411. doi:10.1097/CM9.0000000000003255
11. Cervantes J. Tuberculosis: digging deep in the soul of humanity. Respir Med. 2016;119:20–22. doi:10.1016/j.rmed.2016.08.009
12. Yang C, Lu L, Warren JL, et al. Internal migration and transmission dynamics of tuberculosis in Shanghai, China: an epidemiological, spatial, genomic analysis. Lancet Infect Dis. 2018;18(7):788–795. doi:10.1016/S1473-3099(18)30218-4
13. Hu DM, Xu CH, Zhao YL, et al. Analysis of the Epidemiological Characteristics of Pulmonary Tuberculosis among the Floating Population in China from 2018 to 2021. Trop Dis Parasitol. 2023;21(2):78–81. doi:10.3969/j.issn.1672-2302.2023.02.004
14. Wang Z, Guo T, Jiang T, et al. Regional distribution of Mycobacterium tuberculosis infection and resistance to rifampicin and isoniazid as determined by high-resolution melt analysis. BMC Infect Dis. 2022;22(1):812. doi:10.1186/s12879-022-07792-7
15. Wang Z, Guo T, Xu L, et al. Analysis of molecular resistance and associated risk factors in tuberculosis. BMC Infect Dis. 2025;25(1):216. PMID:39948442. doi:10.1186/s12879-025-10615-0
16. Luoyang Bureau of Statistics, Luoyang Survey Team of the National Bureau of Statistics. Statistical bulletin on the national economic and social development of Luoyang in 2023. Available from: https://www.ly.gov.cn/2024/05-09/144763.html.
17. National People’s Congress of China. Law of the People’s Republic of China on the protection of the rights and interests of the elderly; 2021. Available from: https://www.gov.cn/guoqing/2021-10/29/content_5647622.htm.
18. Ministry of Health of China. Regulations on the administration of the transport of highly pathogenic microbial strains/viruses or samples capable of infecting humans; 2006. Available from: https://www.gov.cn/gongbao/content/2006/content_453197.htm.
19. Basra D, Matee MIN, Mcnerney R. Quality assessment of sputum smear microscopy for detection of acid fast bacilli in peripheral health care facilities in Dar es Salaam, Tanzania. East Afr Med J. 2006;83(6):306–310. doi:10.4314/eamj.v83i6.9437
20. National Health Commission of China. Diagnostic criteria for pulmonary tuberculosis (WS 288-2017). Electron J Emerg Infect Dis. 2018;3(1):59–61.
21. Shang H, Wang YS, Shen ZY, et al. National Clinical Laboratory Procedures.
22. Caraux-Paz P, Diamantis S, de Wazières B, et al. Tuberculosis in the elderly. J Clin Med. 2021;10(24):5888. doi:10.3390/jcm10245888
23. Byng-Maddick R, Noursadeghi M. Does tuberculosis threaten our ageing populations? BMC Infect Dis. 2016;16:119. doi:10.1186/s12879-016-1451-0
24. Ye ZT, Ren F, Wang H, et al. Treatment outcomes and influencing factors in elderly patients with multidrug/rifampicin-resistant pulmonary tuberculosis: a national multicenter, retrospective cohort study. Chin J Antituberc. 2024;46(9):1023–1029. doi:10.19982/j.issn.1000-6621.20240215
25. Song YY, Li T, Xia H, et al. Analysis of the epidemiological characteristics of national reported pulmonary tuberculosis incidence, 1997-2023. Chin J Antituberc. 2024;46(10):10. doi:10.19982/j.issn.1000-6621.20240382
26. World Health Organization. Global Tuberculosis Report 2024. Geneva: World Health Organization; 2024. Available from: https://www.who.int/publications/i/item/9789240101531.
27. Liu MR, Wang YQ, Gao MQ, et al. A case-control study on the risk factors of multidrug-resistant pulmonary tuberculosis in Qinghai Province. J Clin Pulm Med. 2015;20(4):592–595.
28. Xu DF, Wang Q, Li Z, et al. Resistance analysis of the first and second line anti-TB drugs in 420 clinical Mycobacteria tuberculosis isolates from Anhui Province. Chin J Zoonoses. 2014;30(1):54–57. doi:10.3969/cjz.j.issn.1002-2694.2014.01.012
29. Chuang PH, Wu MH, Fan SY, et al. Population-based drug resistance surveillance of multidrug-resistant tuberculosis in Taiwan, 2007-2014. PLoS One. 2016;11(11):e0165222. doi:10.1371/journal.pone.0165222
30. Zhao H, Wang ZR, Ju HF, et al. Epidemiological characteristics of drug-resistance and influencing factors in pulmonary tuberculosis patients in Tianjin, 2020. Dis Surveill. 2023;38(1):57–63. doi:10.3784/jbjc.202206210286
31. Abuaku B, Tan H, Li X, et al. Treatment default and death among tuberculosis patients in Hunan, China. Scand J Infect Dis. 2010;42(4):281–287. doi:10.3109/00365540903493723
32. Technical Guidance Group of the Fifth National TB Epidemiological Survey. The fifth national tuberculosis epidemiological survey in 2010. Chin J Antituberc. 2012;34(8):485–508.
33. Chen XG. Occupational exposure and protective measures for medical staff dealing with tuberculosis. Guide Chin Med. 2011;9(31):2. doi:10.3969/j.issn.1671-8194.2011.31.360
34. Li T, Li J, Du X, et al. Age-specific pulmonary tuberculosis notification rates - China, 2008-2018. China CDC Weekly. 2022;4(38):841–846. doi:10.46234/ccdcw2022.176
35. An Q, Song W, Liu J, et al. Primary drug-resistance pattern and trend in elderly tuberculosis patients in Shandong, China, from 2004 to 2019. Infect Drug Resist. 2020;13:4133–4145. doi:10.2147/IDR.S277203
36. Guo J, Feng YP, Liu ZD, et al. Analysis of factors influencing patient delay by patients with pulmonary tuberculosis in Lishui City, Zhejiang Province. BMC Pulm Med. 2023;23(1):264. doi:10.1186/s12890-023-02554-w
37. Lönnroth K, Jaramillo E, Williams BG, et al. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc sci med. 2009;68(12):2240–2246. doi:10.1016/j.socscimed.2009.03.041
38. Akalu TY, Clements ACA, Wolde HF, et al. Economic burden of multidrug-resistant tuberculosis on patients and households: a global systematic review and meta-analysis. Sci Rep. 2023;13(1):22361. doi:10.1038/s41598-023-47094-9
39. Fountain AJ, Waller NJE, Cheung CY, et al. Verapamil and its metabolite norverapamil inhibit the Mycobacterium tuberculosis MmpS5L5 efflux pump to increase bedaquiline activity. Proc Natl Acad Sci. 2025;122(16):e2426827122. doi:10.1073/pnas.2426827122
40. Vissandjee B, Mourid A, Greenaway CA, et al. Searching for sex- and gender-sensitive tuberculosis research in public health: finding a needle in a haystack. Int J Women’s Health. 2016;8:731–742. doi:10.2147/IJWH.S119757
41. Khan MT, Zaheer S, Amar W, et al. Effect of smoking cessation interventions on abstinence and tuberculosis treatment outcomes among newly diagnosed patients: a randomized controlled trial. Microbiol Spectrum. 2024;12(4):e0387823. doi:10.1128/spectrum.03878-23
42. Lee CY, Chi MJ, Yang SL, et al. Using financial incentives to improve the care of tuberculosis patients. Am J Manag Care. 2015;21(1):e35–e42. PMID:25880266.
43. Sriboonchitta S. Does urbanization increase the risk of emerging infectious diseases in China? A spatial econometric analysis. Sustainability. 2022;14(1):165. doi:10.3390/su14010165
44. Woldesemayat EM. Tuberculosis in migrants is among the challenges of tuberculosis control in high-income countries. Risk Manage Healthcare Policy. 2021;14:2965–2970. doi:10.2147/RMHP.S314777
45. Ding XY, Mao WH, Lu W, et al. Impact of multiple policy interventions on the screening and diagnosis of drug-resistant tuberculosis patients: a cascade analysis on six prefectures in China. Infect Diseases Poverty. 2021;10(1):8. doi:10.1186/s40249-021-00793-9
46. Shah T, Shah Z, Yasmeen N, et al. Pathogenesis of SARS-CoV-2 and Mycobacterium tuberculosis Coinfection. Front Immunol. 2022;13:909011. doi:10.3389/fimmu.2022.909011
47. Goig GA, Windels EM, Loiseau C, et al. Ecology, global diversity and evolutionary mechanisms in the Mycobacterium tuberculosis complex. Nat Rev Microbiol. 2025. doi:10.1038/s41579-025-01159-w
48. Ardizzoni E, Mulders W, De Diego Fuertes M, et al. Phenotypic and genotypic resistance to bedaquiline in patients with multi-drug-resistant tuberculosis: experiences from Armenia. Antimicrob Agents Chemother. 2025;69(9):e0183924. doi:10.1128/aac.01839-24
49. Gunther G. Multidrug-resistant and extensively drug-resistant tuberculosis: a review of current concepts and future challenges. Clin Med. 2014;14(3):279–285. doi:10.7861/clinmedicine.14-3-279
50. Serajian M, Testagrose C, Prosperi M, et al. A comparative study of antibiotic resistance patterns in Mycobacterium tuberculosis. Sci Rep. 2025;15(1):5104. doi:10.1038/s41598-025-89087-w
51. Wen S, Yin J, Sun Q. Impacts of social support on the treatment outcomes of drug-resistant tuberculosis: a systematic review and meta-analysis. BMJ Open. 2020;10(10):e036985. doi:10.1136/bmjopen-2020-036985
52. Ministry of Health of the People’s Republic of China. Report on the Baseline Survey of Tuberculosis Drug Resistance in China. Beijing: People’s Medical Publishing House; 2010.
53. Leo B, Retnowulan H. Complicated case of multidrug-resistant tuberculosis with multiple comorbidities, successfully treated after several treatment modifications. Clin Med Insights Circ Respir Pulm Med. 2022;16:11795484221142468. doi:10.1177/11795484221142468
54. Chida N, Ansari Z, Hussain H, et al. Determinants of default from tuberculosis treatment among patients with drug-susceptible tuberculosis in Karachi, Pakistan: a mixed methods study. PLoS One. 2015;10(11):e0142384. doi:10.1371/journal.pone.0142384
55. Guo P, Qiao W, Sun Y, et al. Telemedicine technologies and tuberculosis management: a randomized controlled trial. Telemed J E Health. 2019;26(9):1150–1156. doi:10.1089/tmj.2019.0190
56. Dheda K, Perumal T, Moultrie H, et al. The intersecting pandemics of tuberculosis and COVID-19: population-level and patient-level impact, clinical presentation, and corrective interventions. Lancet Respir Med. 2022;10(6):603–622. doi:10.1016/S2213-2600(22)00092-3
57. World Health Organization. Global Tuberculosis Report 2022. Geneva: World Health Organization; 2022:2.
58. TB/COVID-19 Global Study Group. Tuberculosis and COVID-19 co-infection: description of the global cohort. Eur Respir J. 2022;59(3):2102538.
59. Zafar Ullah AN, Shrestha S, Malik AA, et al. Holistic approach to tuberculosis detection, treatment and prevention: emerging evidence and strategies from the field. Trop Med Infect Dis. 2022;7(3):36. doi:10.3390/tropicalmed7030036
60. Uys PW, Warren R, van Helden PD, et al. Potential of rapid diagnosis for controlling drug-susceptible and drug-resistant tuberculosis in communities where Mycobacterium tuberculosis infections are highly prevalent. J Clin Microbiol. 2009;47(5):1484–1490. doi:10.1128/JCM.02289-08
61. Pai M, Kasaeva T, Swaminathan S. Covid-19’s devastating effect on tuberculosis care - A path to recovery. N Engl J Med. 2022;386(16):1490–1493. doi:10.1056/NEJMp2118145
62. John C. Realizing the World Health Organization’s End TB Strategy (2016⁻2035): how can social approaches to tuberculosis elimination contribute to progress in Asia and the Pacific? Trop Med Infect Dis. 2019;4(1). doi:10.3390/tropicalmed4010028
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.