Back to Journals » Drug Design, Development and Therapy » Volume 19
Establishing the Median and 95% Effective Doses of Oliceridine for Immediate Post-Surgical Analgesia Following Laparoscopic Cholecystectomy: A Double-Blind, Sequential Dose-Finding Study
Authors Cao X, Xiao H, Yan H, Wei Y, Wen Q, Zhang Z, Xu G, Xu B, Chen J, Li X
Received 8 November 2024
Accepted for publication 19 March 2025
Published 8 April 2025 Volume 2025:19 Pages 2737—2747
DOI https://doi.org/10.2147/DDDT.S505079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Tin Wui Wong
Xianghua Cao,1,2,* Huiling Xiao,1,2,* Haoran Yan,1,2,* Yujiao Wei,1,2 Qiting Wen,1,2 Zhijian Zhang,1,2 Guizhen Xu,1,2 Binbin Xu,1,2 Jian Chen,1,2 Xueping Li1,2
1Department of Anesthesiology, Dongguan Tungwah Hospital, Dongguan, People’s Republic of China; 2Dongguan Key Laboratory of Anesthesia and Enhanced Recovery after Surgery, Guangdong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xueping Li, Email [email protected]
Background: This investigation aimed to establish the optimal dosing parameters of oliceridine for postoperative pain control in laparoscopic cholecystectomy (LC) procedures. Using Dixon and Massey’s up-and-down sequential allocation method, the median effective dose (ED50) and the dose required for 95% effective dose (ED95) were determined, alongside an evaluation of the agent’s safety profile.
Methods: In this prospective trial, 82 participants scheduled for LC were enrolled and randomly assigned to receive either oliceridine or saline (control). Prior to surgical incision, the intervention group received varying doses of intravenous oliceridine, while control subjects received equivalent volumes of saline solution. Post-surgical pain management involved standardized multimodal analgesic protocols for both cohorts. Baseline demographic data was documented for all participants. Pain evaluations using the 11-point verbal numeric rating scale (NRS) at 15 min, 30 min, and 2h post-extubation. Using Dixon’s up-and-down methodology, the ED50 and ED95 were determined. Hemodynamic variables were tracked and pain levels quantified throughout the procedure. The study protocol included monitoring post-anesthetic recovery characteristics and documenting adverse effects.
Results: Probability unit regression analysis indicated that the ED50 of oliceridine for the prevention of early postoperative pain was calculated to be 18.45 μg/kg (95% CI: 16.85– 19.82 μg/kg), while the ED95 was determined to be 22.39 μg/kg (95% CI: 20.75– 26.98 μg/kg). Statistical analysis showed comparable rates of adverse events between study groups (p > 0.05). Additional analyses demonstrated similar outcomes between oliceridine and control cohorts regarding hemodynamic stability, and adverse effect profiles. Pain management satisfaction assessment at 24 hours post-LC revealed high approval rates in the oliceridine group, with 90% of patients (36/40, p=0.31) and 97.5% of surgeons (39/40, p=0.03) expressing satisfaction, regardless of administered dose.
Conclusion: Our findings establish that for early postoperative pain management, oliceridine demonstrates optimal therapeutic efficacy at an ED50 of 18.45 ug/kg, with the ED95 determined to be 22.39 ug/kg.
Keywords: laparoscopic cholecystectomy, postoperative pain, oliceridine, ED50, ED95
Introduction
Laparoscopic cholecystectomy (LC) is the preferred surgical approach for gallbladder disorders, providing the benefits of minimal invasiveness and enhanced recovery.1,2 The immediate post-LC pain response includes surgical site discomfort, internal organ pain3–7, and increased pain sensitivity after opioid administration.8–13 This complex pain profile may induce physiological instability, impacting metabolic and cardiovascular parameters and potentially prolonging recovery periods and hospital stays.14–17 However, managing acute post-surgical discomfort remains a significant challenge.
Despite therapeutic advances, managing acute post-surgical pain effectively remains challenging, with suboptimal control potentially leading to adverse outcomes and chronic pain.18–20 While opioids are traditionally the mainstay for moderate-to-severe pain management,21 their use often results in undesirable effects such as respiratory suppression, drowsiness, gastrointestinal disturbances, and pruritic reactions.20,22,23 Effective post-surgical pain control through comprehensive, multifaceted analgesic strategies represents a cornerstone of Enhanced Recovery After Surgery (ERAS) protocols.24 Oliceridine offers a novel approach in pain management as a selective mu-opioid receptor modulator. Research indicates that G-protein signaling mediates analgesic effects, whereas β-arrestin pathways are associated with adverse reactions, suggesting a potential for an improved therapeutic range compared to traditional opioids,20,25–28 making it a valuable option in multimodal pain management strategies. Existing clinical evidence29 suggests that oliceridine is effective in pain control while reducing the incidence of nausea and vomiting—a common concern in post-operative care. Research indicates that20,30 initiating oliceridine at a lower dose with the option for titration can optimize pain management while minimizing side effects. Despite the promising evidence, there remains a notable research gap regarding the optimal dosing of oliceridine specifically in LC. Currently, clinical guidelines do not provide specific recommendations for oliceridine usage in this context, and further studies are needed to elucidate the most effective dosing strategies and to assess the long-term outcomes associated with oliceridine compared to traditional opioids in LC patients.
By employing the sequential allocation methodology developed by Dixon and Massey,7,31,32 this study evaluated the median dose (ED50) and the effective dose at 95% (ED95) of oliceridine for managing postoperative pain during LC procedures. Furthermore, the investigation examined the therapeutic safety profile and clinical efficacy of this analgesic approach.
Materials and Methods
Recruitment of Patients
This investigation was approved by the Dongguan Tungwah Hospital Ethics Committee (DHKY-2023-071-01) and registered with the Chinese Clinical Trial Registry (ChiCTR2400083033) on April 15, 2024. Between May and October 2024, 106 participants were enrolled for elective LC at Dongguan Tungwah Hospital. The study protocol adhered to the Declaration of Helsinki guidelines and CONSORT 2010 reporting standards.33 A designated anesthesiologist screened and enrolled eligible participants, obtaining documented informed consent from all subjects or their authorized representatives.
Randomization and Blinding
Either an initial dose of oliceridine (30 µg/kg) or an equivalent amount of saline as a control was given to patients at random in a 1:1 ratio. Before the trial started, an assistant sequentially numbered the opaque, sealed envelopes with the randomization codes, which were created using computerized random number techniques (SPSS 25 Inc., Chicago, IL). An impartial researcher who was not involved in the subsequent study protocols managed the randomization process.
An anesthesia nurse who had received extensive training on the protocol prepared the study drugs while remaining blind to the treatment allocations. As required by the investigation, oliceridine and saline were both diluted in identical 10 mL syringes. An attending anesthesiologist administered the anesthesia without knowing the prescribed treatment in order to preserve blinding. Additionally, patients were not informed of the precise drugs they were prescribed. Another independent anesthesiologist, who was oblivious to the group assignments, collected the data. Additionally, throughout the study, the treatment assignments for patients, surgeons, and data analyzers were kept secret.
Subjects
Participants eligible for this study were adults between the ages of 18 and 60, with a Body Mass Index (BMI) less than 30 kg/m2, an ASA physical status of I–II, and scheduled for LC under general anesthesia at Dongguan Tungwah Hospital. Exclusion criteria included known allergies to opioids or local anesthetics, abnormal coagulation profiles, recent analgesic use or substance dependency, psychiatric or neurological disorders within the past two weeks, significant organ system impairment, or necessity for conversion to an open surgical approach.
Pharmacological Intervention
In the treatment arm, subjects were administered pre-incisional intravenous oliceridine, produced by Jiangsu Nhwa Pharmaceutical Co., Ltd. The comparison group received an equivalent volume of saline. Dixon’s up-down method was utilized to define the ED50 and ED95 dosages. An initial dose of 30 ug/kg was chosen based on institutional insights and literature,20 with doses varying from 10 to 50 ug/kg in 5 ug/kg increments (10–15-20-25-30-35-40-45-50 ug/kg).
Pain levels were assessed using a 11-point verbal numeric rating scale (NRS),34 with 0 indicating no pain and 10 representing the maximum imaginable pain. The criteria for determining “effective” analgesia: no requirement for rescue analgesic drugs and NRS scores ≤3 during the initial 2-hour post-extubation period (measured at 15 min, 30 min, and 2 h). The criteria for determining “ineffective” analgesia: either requirement for rescue analgesic drugs or NRS scores >3 during any time point within 2 hours after extubation (measured at 15 min, 30 min, and 2 h).
Dose adjustments for subsequent participants were guided by sequential allocation. The protocol required a dose increase for the next participant if their predecessor registered NRS >3 at any assessment point or required tramadol for rescue analgesia. Conversely, effective pain control, indicated by NRS ≤3 without the need for rescue analgesia, triggered a reduction in dose for the subsequent participant. Participants who did not meet the study criteria were replaced to preserve the integrity of the randomization and dose adjustment protocol.
Anesthetic Management
Before surgery, patients underwent IV catheterization in the preoperative area and were then transferred to the operating suite. Vital parameters such as SPO2, HR, and NIBP were continuously monitored at five-minute intervals. Preoperative preparation included the administration of 40 mg of intravenous paracetamol sodium and supplemental oxygen through a mask. Standardized anesthetic protocols were applied across both study groups. Anesthesia induction involved midazolam (0.05 mg/kg), propofol (2 mg/kg), sufentanil (0.3 ug/kg), and rocuronium (0.6 mg/kg). After placing a double-lumen laryngeal mask, subjects in the intervention group received predetermined doses of oliceridine intravenously, while those in the control group were given volume-matched saline. Anesthesia was maintained with propofol (3–5 mg/kg/h), sevoflurane (1–1.5%), and remifentanil (0.1ug/kg/min), keeping narcotrend values between 40–60.
Signs of inadequate anesthesia were identified by patient movements or swallowing, lacrimation or diaphoresis, or hemodynamic changes exceeding 20% of baseline for more than one minute, and narcotrend values rising above 60. Adjustments in anesthetic depth included stepwise changes in propofol (±1 mg/kg/h), remifentanil (±0.05 ug/kg/min), and sevoflurane (±0.5%). Hemodynamic parameters were maintained within ±20% of baseline values. Muscle relaxation was discontinued 30 minutes before the end of surgery. At wound closure, administration of remifentanil and propofol was stopped, and the area was infiltrated with 0.5% ropivacaine with 20mL. Patients were then transferred to the PACU where residual sedation and neuromuscular blockade were reversed using flumazenil and sugammadex. The use of flumazenil was included as a precautionary measure to ensure consistent and safe recovery from midazolam-induced sedation, and minimize potential delays in awakening.
Outcomes Assessment
Baseline characteristics and operative parameters included documentation of patient characteristics and operative metrics such as age, gender, BMI, ASA status (I/II), surgical duration, and doses of intraoperative medications (sufentanil, remifentanil, and propofol). The primary endpoint was to establish oliceridine’s ED50 and ED95 for early post-surgical pain prevention. Secondary endpoints included cardiovascular monitoring, parameters assessed during the recovery phase, pain evaluations, and adverse events. Cardiovascular monitoring involved measurements of mean arterial pressure (MAP) and heart rate (HR) at three crucial time points: T0 (pre-anesthetic baseline), T1 (initial surgical incision), and T2 (gallbladder dissection phase). Parameters assessed during the recovery phase included the time from surgery completion to extubation, and pain evaluations using the NRS at 15 min, 30 min, and 2h post-extubation. This phase also monitored the need for rescue analgesia or muscle relaxant reversal, and PACU medication administration, especially opioids, along with adverse event monitoring (postoperative nausea and vomiting, pruritus, and surgeon-patient satisfaction).
A research nurse, blinded to treatment allocation, performed standardized assessments of patients at 15 min, 30 min, and 2h post-extubation, evaluating pain intensity via NRS (0–10), nausea and vomiting severity (none/light/medium/severe), pruritus intensity (none/light/medium/severe), and overall satisfaction with pain management on a 5-point scale (satisfied/slightly satisfied/neutral/slightly unhappy/dissatisfied).
Sample Size
Based on the sample size termination criteria associated with the sequential allocation method, previous literature and initial experimental studies suggest that involving 20 to 40 patients can provide stable estimates for the ED50 and ED90 parameters.7,35–37 The aim of this study is to explore the ED50 and ED95 doses of oliceridine for alleviating immediate postoperative pain after LC before skin incision. To account for an anticipated dropout rate of 10% due to participants not completing the study, we enrolled a total of 106 patients, ultimately including 79 in our analysis.
Statistical Analyses
Statistical analyses were conducted using multiple platforms: SPSS 25.0, Free Statistics (v1.9), and GraphPad Prism 10. For continuous variables with a normal distribution, means ± SD were reported, and Student’s t-tests were employed. For non-normally distributed data, medians with interquartile ranges were presented, and Mann–Whitney U-tests were utilized. Categorical data were expressed as frequencies and percentages, with either Chi-square or Fisher’s exact tests applied as needed. Probit analysis via probability unit regression was used to determine oliceridine’s ED50 and ED95, along with 95% confidence intervals, by evaluating the binary outcomes (‘effective’ vs ‘ineffective’) obtained through sequential up-and-down allocation.7,36,38,39
Results
During the study period (May-October 2024), 106 eligible patients underwent LC. After randomization, 41 participants were allocated to each study arm—oliceridine intervention and saline control. Recruitment was halted upon reaching the predetermined sample size, with the final analysis including 79 subjects (40 in the oliceridine arm, 39 in the control arm; Figure 1). Comparative analysis showed no statistically significant differences in baseline characteristics between the groups (p > 0.05), including demographic factors (age, gender, BMI), ASA classification, procedural duration, and anesthetic requirements (sufentanil, remifentanil, propofol), with details presented in Table 1 and Table 2.
 |
Table 1 Demographic Data of Patients |
 |
Table 2 Intraoperative Information |
 |
Figure 1 The consort flowchart. |
The up-and-down sequential analysis, shown in Figure 2, identified the distribution of effective and ineffective responses. Probability unit regression analysis, illustrated in Figure 3, established that oliceridine had a ED50 of 18.45 ug/kg (95% CI: 16.85–19.82 ug/kg) for early postoperative pain prevention. The ED95 was calculated to be 22.39 ug/kg (95% CI: 20.75–26.98 ug/kg).
 |
Figure 3 Dose-response curve of oliceridine for preventing early postoperative pain in patients undergoing laparoscopic cholecystectomy. |
Analysis of hemodynamic parameters indicated stability between the groups, with no significant differences in MAP at measurement intervals T1 and T2 (p > 0.05). Similarly, HR measurements were statistically equivalent across both groups at these times (p > 0.05) (Figure 4).
Table 2 details the post-anesthetic recovery metrics for all participants, showing comparable awakening intervals between the intervention and control groups, with no statistically significant differences. Twenty-four hours after LC, supplemental tramadol for breakthrough pain was required by 53.8% (21/39) of patients in the control group and 40% (16/40) of patients in the intervention group (p=0.22, Table 3). Table 3 displays the analysis of post-surgical complications, revealing minimal adverse effects in both cohorts. There were no instances of respiratory depression observed in either group. The oliceridine-treated cohort reported one case of mild pruritus and the control group three cases of mild nausea and vomiting, none of which required supplementary medication. No serious adverse reactions were recorded during the study.
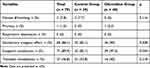 |
Table 3 Adverse Events and Surgeon-Patient Satisfaction |
Patient satisfaction assessments conducted 24 hours post-LC showed comparable satisfaction rates between groups, with 82.1% (32/39) in the control group and 90% (36/40) in the oliceridine group reporting satisfactory pain management (p=0.31, Table 3). Surgeon evaluations indicated a statistically significant higher satisfaction rate in the oliceridine group (97.5%; 39/40) compared to the control group (82.1%; 32/39) (p=0.03, Table 3).
Discussion
Utilizing a prospective, double-blinded, randomized sequential allocation design with up-down methodology, it was determined that the ED50 of oliceridine for preventing post-surgical pain in LC cases is 18.45 ug/kg (95% CI: 16.85–19.82 ug/kg). The ED95 was calculated as 22.39 ug/kg (95% CI: 20.75–26.98 ug/kg). Comparative analyses between the treatment and control groups revealed no statistically significant differences in opioid consumption patterns, patient’s satisfaction metrics, hemodynamic responses during critical surgical phases (skin incision and gallbladder bed dissection), or adverse event profiles in both frequency and intensity. Surgeon-patient’s evaluation indicated a statistically significant higher satisfaction rate in the oliceridine group.
LC is recognized as the preferred intervention for symptomatic gallstone disease, particularly in cases presenting with acute abdominal pain.40 Post-surgical pain management is challenging due to factors such as complex neural innervation patterns, thermal injury from electrocautery, trauma from surgical incision, and paradoxical pain sensitization induced by opioid medications.7,36,40 Contemporary pain management strategies emphasize a multimodal approach, targeting various pain pathways with complementary analgesic combinations to optimize pain control while minimizing the doses of individual drugs and their associated adverse effects.24,41–43 Currently, opioid and non-opioid analgesics are the main drugs used to prevent pain during and after surgery. Even while opioids have undeniable therapeutic benefits in the treatment of pain, their usage can occasionally be limited by a number of unfavorable side effects, including opioid dependence, tolerance, constipation, itching, or respiratory depression.7 Clinicians have highlighted the need for the development of effective opioid’s analgesics with improved safety profiles and reduced adverse reactions, as a critical unmet need in acute surgical pain management.44
Oliceridine introduces a novel approach to opioid receptor targeting through biased agonism, selectively enhancing G-protein signaling while minimizing β-arrestin pathway activation.20,26,45–47 This mechanism could potentially offer a broader therapeutic range than traditional opioids and reduce opioid-related adverse events while maintaining analgesic efficacy. Soergel and colleagues48,49 conducted a randomized crossover trial involving 30 healthy participants to compare three oliceridine doses (1.5, 3, and 4.5 mg IV) against 10 mg IV morphine and placebo. The higher doses of oliceridine demonstrated a superior analgesic onset with a 75-second latency compared to morphine. Viscusi’s50 team assessed oliceridine in patients undergoing bunionectomy with a popliteal sciatic nerve block, revealing that peak pain relief occurred within 5 minutes for 2 mg and 3 mg doses, markedly quicker than morphine’s onset of over 20 minutes. Singla et al51 study explored postoperative pain management in 200 abdominoplasty patients using PCA, which allowed for individualized analgesic titration while monitoring adverse effects. Our research builds on these methods by determining oliceridine’s ED50 for post-LC pain using a sequential allocation methodology. This novel finding is clinically significant, providing anesthesiologists with evidence-based guidance for integrating oliceridine into multimodal analgesic protocols.
Oliceridine acts at the µ (MOP) receptor and signals via G-protein and arrestin pathways, with the former believed to underlie its analgesic effects and the latter its side effects.20 Viscusi et al50 found that oliceridine doses of 0.1 and 0.35 mg present a lower risk of respiratory depression compared to morphine, as demonstrated in a placebo-controlled randomized trial. Singla et al51 observed no difference in safety and tolerability between 1 mg oliceridine and placebo in 401 abdominoplasty patients. Bergese et al52 reported that with cumulative oliceridine doses stratified into >4-8, >8-16, >16-36, >36 mg, the occurrence rates were 31% for nausea, 15% for constipation, 10% for vomiting, and 3% for serious events. Our study corroborates these findings, showing no difference in the incidence of nausea, vomiting, or pruritus between groups at the 50% effective dose, with no increase in respiratory depression.
None of the participants in this study developed severe hypotension requiring intervention with inotropic agents or vasopressors. The most significant reduction in systolic blood pressure (SBP) was observed 5 minutes after the propofol bolus injection. This investigation confirms that administering a single intravenous dose of oliceridine prior to surgical incision does not lead to clinically significant hemodynamic instability. We have further funded that the ED50 (18.45 µg/kg) and ED95 (22.39 µg/kg) of oliceridine for early postoperative pain management in LC. These dose-response parameters provide anesthesiologists with evidence-based guidance for integrating oliceridine into multimodal analgesic regimens. Specifically, the ED50 value can be used as a starting point for dose titration, while the ED95 offers a target dose for achieving effective pain control in 95% of patients based on the background of multimodal analgesia and enhanced recovery after surgery. The narrow therapeutic window between the ED50 and ED95 suggests that oliceridine has a predictable dose-response relationship, which may reduce the risk of under- or over-dosing in clinical practice. This is particularly relevant in day-case surgeries or ERAS pathways, where rapid and effective pain relief is essential for early mobilization and discharge. Our findings are consistent with those of Bergese et al52 who reported that oliceridine provided effective analgesia with a favorable safety profile in patients undergoing various surgical procedures.
This study’s strength resides in its comprehensive evaluation of the dose-response relationship of intravenous oliceridine for managing early postoperative pain in patients undergoing LC. By incorporating a detailed dose-response curve, this research offers valuable insights that can assist healthcare providers in clinical decision-making. Our findings introduce new evidence that supports the application of oliceridine within LC populations, specifically when used in a multimodal analgesia protocol. Several limitations warrant consideration when interpreting our findings. The study design employed an up-down allocation methodology to determine sample size instead of traditional power calculations. Additionally, comparisons of pain assessment between groups were challenging due to the variable dosing protocol used in the oliceridine cohort. The investigation was limited to immediate post-surgical pain management (2 hours after extubation), excluding the evaluation of oliceridine’s long-term analgesic efficacy. Since this center used a single-dose of oliceridine before skin incision to observe the pain within 2 hours after surgery, and did not observe the patients’ pain for a long time or the pain in the shoulder area, we look forward to conducting a prospective cohort study in the future to observe the analgesic effect and duration of oliceridine.
Conclusion
This investigation established the optimal dosing parameters for oliceridine in managing early postoperative pain, with an ED50 of 18.45 µg/kg and an ED95 of 22.39 µg/kg. Administered during surgery, oliceridine effectively attenuated nociceptive responses while ensuring normal emergence from anesthesia and maintaining a robust safety profile. These findings provide anesthesiologists with evidence-based guidance for integrating oliceridine into multimodal analgesic protocols, particularly in the context of LC and ERAS pathways. Further research will help to fully elucidate its potential benefits and optimize its use in a broader range of surgical contexts.
Data Sharing Statement
Data related to this study can be obtained by contacting the corresponding author if reasonable.
Ethics Approval and Consent to Participate
This study was approved by The Ethics Committee of Dongguan Tungwah hospital (DHKY-2023-071-01) and written informed consent was obtained from all subjects participating in the study.
Funding
This work was supported by Guangdong Medical Association (GDMA-2023-396-004).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Aloraini A, Alanezi T, AlShahwan N. Subtotal laparoscopic cholecystectomy versus open total cholecystectomy for the difficult gallbladder: a systematic review and meta-analysis. Curr Prob Surg. 2024;61(11):101607. doi:10.1016/j.cpsurg.2024.101607
2. on behalf of the SAGES Safe Cholecystectomy Task Force, Pucher PH, Brunt LM, Davies N, et al. Outcome trends and safety measures after 30 years of laparoscopic cholecystectomy: a systematic review and pooled data analysis. Surg Endosc. 2018;32(5):2175–2183. doi:10.1007/s00464-017-5974-2.
3. Hilvering B, Draaisma WA, Van Der Bilt JDW, Valk RM, Kofman KE, Consten ECJ. Randomized clinical trial of combined preincisional infiltration and intraperitoneal instillation of levobupivacaine for postoperative pain after laparoscopic cholecystectomy. Br J Surg. 2011;98(6):784–789. doi:10.1002/bjs.7435
4. Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. J British Surg. 2000;87(3):273–284. doi:10.1046/j.1365-2168.2000.01374.x
5. Mitra S, Khandelwal P, Roberts K, Kumar S, Vadivelu N. Pain relief in laparoscopic cholecystectomy—a review of the current options. Pain Pract. 2012;12(6):485–496. doi:10.1111/j.1533-2500.2011.00513.x
6. Hang L, Shao D, Sun W. The ED50 and ED95 of ketamine for prevention of postoperative hyperalgesia after remifentanil-based anaesthesia in patients undergoing laparoscopic cholecystectomy. Swiss Med Wkly. 2011. doi:10.4414/smw.2011.13195
7. Xu Z, Lang Y, Xu X, Deng L, Song H, Yin D. The ED50 and ED95 of esketamine for preventing early postoperative pain in patients undergoing laparoscopic cholecystectomy: a prospective, double-blinded trial. BMC Anesthesiol. 2023;23(1):385. doi:10.1186/s12871-023-02357-w
8. Koponen ME, Forget P. Pharmacological interventions for opioid-induced hyperalgesia: a scoping review of preclinical trials. JCM. 2022;11(23):7060. doi:10.3390/jcm11237060
9. Tompkins DA, Campbell CM. Opioid-induced hyperalgesia: clinically relevant or extraneous research phenomenon? Curr Pain Headache Rep. 2011;15(2):129–136. doi:10.1007/s11916-010-0171-1
10. Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14(2;3):145–161. doi:10.36076/ppj.2011/14/145
11. Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014;112(6):991–1004. doi:10.1093/bja/aeu137
12. Koo C-H, Yoon S, Kim B-R, et al. Intraoperative naloxone reduces remifentanil-induced postoperative hyperalgesia but not pain: a randomized controlled trial. Br J Anaesth. 2017;119(6):1161–1168. doi:10.1093/bja/aex253
13. Angst MS, Koppert W, Pahl I, Clark DJ, Schmelz M. Short-term infusion of the μ-opioid agonist remifentanil in humans causes hyperalgesia during withdrawal. Pain. 2003;106(1):49–57. doi:10.1016/S0304-3959(03)00276-8
14. Rekatsina M, Paladini A, Piroli A, Zis P, Pergolizzi JV, Varrassi G. Pathophysiologic approach to pain therapy for complex pain entities: a narrative review. Pain Ther. 2020;9(1):7–21. doi:10.1007/s40122-019-00147-2
15. Chadwick A, Frazier A, Khan TW, Young E. Understanding the psychological, physiological, and genetic factors affecting precision pain medicine: a narrative review. JPR. 2021;14:3145–3161. doi:10.2147/JPR.S320863
16. Apfelbaum JL, Chen C, Mehta SS, Gan ATJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesthesia Analg. 2003;97(2):534–540. doi:10.1213/01.ANE.0000068822.10113.9E
17. Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. JPR. 2017;10:2287–2298. doi:10.2147/JPR.S144066
18. Santa Cruz Mercado LA, Liu R, Bharadwaj KM, et al. Association of intraoperative opioid administration with postoperative pain and opioid use. JAMA Surg. 2023;158(8):854. doi:10.1001/jamasurg.2023.2009
19. Espitalier F, Idrissi M, Fortier A, et al. Impact of Nociception Level (NOL) index intraoperative guidance of fentanyl administration on opioid consumption, postoperative pain scores and recovery in patients undergoing gynecological laparoscopic surgery. A randomized controlled trial. J Clin Anesthesia. 2021;75:110497. doi:10.1016/j.jclinane.2021.110497
20. Daksla N, Wang A, Jin Z, Gupta A, Bergese SD. Oliceridine for the ma nagement of moderate to severe acute postoperative pain: a narrative review. DDDT. 2023;17:875–886. doi:10.2147/DDDT.S372612
21. Lovich-Sapola J, Smith CE, Brandt CP. Postoperative pain control. Surgical Clinic North Am. 2015;95(2):301–318. doi:10.1016/j.suc.2014.10.002
22. Dahan A, Aarts L, Smith TW. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112(1):226–238. doi:10.1097/ALN.0b013e3181c38c25
23. Volkow ND, Blanco C. The changing opioid crisis: development, challenges and opportunities. mol Psychiatry. 2021;26(1):218–233. doi:10.1038/s41380-020-0661-4
24. Tan M, Law LS-C, Gan TJ. Optimizing pain management to facilitate enhanced recovery after surgery pathways. Can J Anesth/J Can Anesth. 2015;62(2):203–218. doi:10.1007/s12630-014-0275-x
25. Azzam AAH, Lambert DG. Preclinical discovery and development of oliceridine (Olinvyk®) for the treatment of post-operative pain. Expert Opin Drug Discov. 2022;17(3):215–223. doi:10.1080/17460441.2022.2008903
26. Kaye AD, Edinoff AN, Babin KC, et al. Pharmacological advances in opioid therapy: a review of the role of oliceridine in pain management. Pain Ther. 2021;10(2):1003–1012. doi:10.1007/s40122-021-00313-5
27. Viscusi ER. A critical review of oliceridine injection as an IV opioid analgesic for the management of severe acute pain. Expert Rev Neurotherapeutics. 2022;22(6):419–426. doi:10.1080/14737175.2022.2072731
28. Tan HS, Habib AS. Safety evaluation of oliceridine for the management of postoperative moderate-to-severe acute pain. Expert Opin Drug Saf. 2021;20(11):1291–1298. doi:10.1080/14740338.2021.1965989
29. Bergese S, Berkowitz R, Rider P, et al. Low incidence of postoperative respiratory depression with oliceridine compared to morphine: a retrospective chart analysis. Pain Res Managmnt Edited by Ablin J. 2020;2020:1–10.
30. Niu J, Hu W, Lu Y, Tang H. Efficacy and safety of oliceridine treatment in patients with postoperative pain: a systematic review and meta-analysis of randomized controlled trials. Expert Rev Clin Pharmacol. 2023;16(6):589–599. doi:10.1080/17512433.2023.2213889
31. Khatoon F, Kocarev M, Fernando R, et al. Optimal infusion rate of norepinephrine for prevention of spinal hypotension for cesarean delivery: a randomized controlled trial, using up-down sequential allocation. Anesthesia Analg. 2024. doi:10.1213/ANE.0000000000007231
32. Mazoit JX, Van Elstraete AC, Tirault M. Tirault M: Dixon and Massey’s method: the starting dose. Anesthesia Analg. 2009;108(1):378–379. doi:10.1213/ane.0b013e31818d4abd
33. Schulz KF, Altman DG, Moher D, the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8(1):18. doi:10.1186/1741-7015-8-18
34. Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, same or different? Are visual analog scale values and numerical rating scale equally viable tools for assessing patients after microdiscectomy? Pain Res Managmnt Edited by Taiar R. 2022;2022:1–6.
35. Cao X, Gui Q, Wei Y, et al. The 50% effective dose of hydromorphone and morphine for epidural analgesia in the hemorrhoidectomy: a double-blind, sequential dose-finding study. BMC Anesthesiology. 2024;24(1). doi:10.1186/s12871-024-02420-0.
36. Huang X-D, Chen J-B, Dong X-Y, Wang W-L, Zhou J, Zhou Z-F. The impact of fentanyl on the effective dose of remimazolam-induced sedation in elderly female patients: an up-and-down sequential allocation trial. DDDT. 2024;18:3729–3737. doi:10.2147/DDDT.S473662
37. Pace NL, Stylianou MP, Warltier DC. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007;107(1):144–152. doi:10.1097/01.anes.0000267514.42592.2a
38. Dixon WJ. Staircase bioassay: the up-and-down method. Neurosci Biobehav Rev. 1991;15(1):47–50. doi:10.1016/S0149-7634(05)80090-9
39. Wang S, Li Y, Chen F, Liu H-C, Pan L, Shangguan W. Comparison of the ED50 of ciprofol combined with or without fentanyl for laryngeal mask airway insertion in children: a prospective, randomized, open-label, dose-response trial. DDDT. 2024;18:4471–4480. doi:10.2147/DDDT.S466603
40. Kim SS, Donahue TR. Laparoscopic cholecystectomy. JAMA. 2018;319(17):1834. doi:10.1001/jama.2018.3438
41. Rosero EB, Joshi GP. Preemptive, preventive, multimodal analgesia: what do they really mean? Plastic and Reconstruct Surg. 2014;134:85S–93S. doi:10.1097/PRS.0000000000000671
42. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691. doi:10.1001/jamasurg.2017.0898
43. Geng Z, Wang B, Zhang Y, et al. Preemptive multimodal analgesia for gynecologic oncology patients undergoing laparotomy: a randomized controlled trial. Front Med. 2024;11:1427548. doi:10.3389/fmed.2024.1427548
44. Gan TJ, Epstein RS, Leone-Perkins ML, Salimi T, Iqbal SU, Whang PG. Practice patterns and treatment challenges in acute postoperative pain management: a survey of practicing physicians. Pain Ther. 2018;7(2):205–216. doi:10.1007/s40122-018-0106-9
45. Beard TL, Michalsky C, Candiotti KA, et al. Oliceridine is associated with reduced risk of vomiting and need for rescue antiemetics compared to morphine: exploratory analysis from two phase 3 randomized placebo and active controlled trials. Pain Ther. 2021;10(1):401–413. doi:10.1007/s40122-020-00216-x
46. Brzezinski M, Hammer GB, Candiotti KA, et al. Low incidence of opioid-induced respiratory depression observed with oliceridine regardless of age or body mass index: exploratory analysis from a phase 3 open-label trial in postsurgical pain. Pain Ther. 2021;10(1):457–473. doi:10.1007/s40122-020-00232-x
47. Hammer GB, Khanna AK, Michalsky C, et al. Oliceridine exhibits improved tolerability compared to morphine at equianalgesic conditions: exploratory analysis from two phase 3 randomized placebo and active controlled trials. Pain Ther. 2021;10(2):1343–1353. doi:10.1007/s40122-021-00299-0
48. Soergel DG, Subach RA, Burnham N, et al. Biased agonism of the μ-opioid receptor by TRV130 increases analgesia and reduces on-target adverse effects versus morphine: a randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Pain. 2014;155(9):1829–1835. doi:10.1016/j.pain.2014.06.011
49. Soergel DG, Ann Subach R, Sadler B, et al. First clinical experience with TRV130: pharmacokinetics and pharmacodynamics in healthy volunteers. J Clin Pharm. 2014;54:351–357.
50. Viscusi ER, Webster L, Kuss M, et al. A randomized, Phase 2 study investigating TRV130, a biased ligand of the μ-opioid receptor, for the intravenous treatment of acute pain. Pain. 2016;157(1):264–272. doi:10.1097/j.pain.0000000000000363
51. Singla N, Minkowitz H, Soergel D, et al. A randomized, Phase IIb study investigating oliceridine (TRV130), a novel µ-receptor G-protein pathway selective (µ-GPS) modulator, for the management of moderate to severe acute pain following abdominoplasty. JPR. 2017;10:2413–2424. doi:10.2147/JPR.S137952
52. Bergese SD, Brzezinski M, Hammer GB, et al. ATHENA: a phase 3, ope n-label study of the safety and effectiveness of oliceridine (TRV130), A G-protein selective agonist at the μ-opioid receptor, in patients with moderate to severe acute pain requiring parenteral opioid therapy. JPR. 2019;12:3113–3126. doi:10.2147/JPR.S217563
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Effective Doses of Nalbuphine Combined with Propofol in Painless Hysteroscopy
Zhong W, Chen C, Tang W
International Journal of General Medicine 2022, 15:5609-5614
Published Date: 11 June 2022
RETRACTED ARTICLE: Effective Doses of Oliceridine Combined with Propofol for Painless Hysteroscopy: A Prospective Dose-Finding Study
Gao L, Tan A, Wang Z, Wei L, Wang X
International Journal of General Medicine 2025, 18:2651-2657
Published Date: 21 May 2025



