Back to Journals » Infection and Drug Resistance » Volume 18
Etiological Factors and Development of a Predictive Model for Urinary Tract Infections in Cervical Cancer Patients Undergoing Intensity-Modulated Radiotherapy
Authors Yao Y, Tao L, Ma L, Fan Y, Zheng D, Wang J, Chen W
Received 26 November 2024
Accepted for publication 4 March 2025
Published 29 March 2025 Volume 2025:18 Pages 1637—1645
DOI https://doi.org/10.2147/IDR.S508574
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Oliver Planz
Ying Yao,1,* Lijun Tao,1,* Li Ma,2 Yuhan Fan,3 Dongju Zheng,2 Jian Wang,1 Wen Chen1
1Department of Pharmacy, People’s Hospital of Ningxia Hui Autonomous Region, Ningxia Medical University, Yinchuan, Ningxia, People’s Republic of China; 2Department of Radiotherapy, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, Ningxia, People’s Republic of China; 3Department of Preparation Center, Ningxia Medical University General Hospital, Yinchuan, Ningxia, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wen Chen, Department of Pharmacy, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, Ningxia, People’s Republic of China, Tel +86 19995350858, Email [email protected]
Objective: To investigate the distribution characteristics of pathogenic bacteria causing urinary tract infections in cervical cancer patients undergoing intensity-modulated radiotherapy (IMRT). Furthermore, to explore the risk factors and predictive factors associated with urinary tract infections, and to establish a personalized risk prediction model.
Methods: A retrospective study analyzed 160 cervical cancer patients undergoing intensity-modulated radiotherapy at the People’s Hospital of Ningxia Hui Autonomous Region from 2020 to 2023. The clinical characteristics of the participants were collected, and in combination with microbiological culture results, the distribution and drug resistance of pathogens causing urinary tract infections were analyzed. Using logistic regression and multivariable logistic analysis, we established a predictive model that includes clinical variables.
Results: Urinary specimens were collected and analyzed from 52 patients with urinary tract infections. The incidence of urinary tract infections in cervical cancer patients after radiotherapy in this study was approximately 32.5%, with the predominant pathogens identified as E. coli, E. faecalis, E. faecium, and P. mirabilis. Invasive procedures (OR 4.202, 95% CI:1.003– 17.608; P=0.050), history of ureteral stent insertion (OR 7.260, 95% CI:2.026– 26.016; P=0.002), Concurrent chemotherapy (OR 2.587, 95% CI:1.010– 6.623; P=0.048), and low serum albumin levels (OR 0.842, 95% CI:0.745– 0.951; P=0.006) were identified as four key factors in the final predictive model. The calibration curve indicated a consistent alignment between the predicted probabilities from the nomogram model and the actual observed outcomes. With an AUC of 0.804 (95% CI: 0.727– 0.881) for the ROC curve, the nomogram prediction model demonstrated strong predictive performance.
Conclusion: E. coli remains the most common pathogen causing urinary tract infections in cervical cancer patients with IMRT. The history of ureteral stent insertion, invasive procedures, concurrent chemotherapy, and serum albumin levels have been identified as independent risk factors of urinary tract infections in cervical cancer IMRT patients. The nomogram prediction model based on these factors can serve as a reference for clinicians to help prevent urinary tract infections.
Keywords: cervical cancer, urinary tract infections, IMRT, nomogram, model
Introduction
Worldwide, cervical cancer ranks as the fourth most common cancer in women.1 Radiation therapy (RT) plays a crucial role in treating cervical cancer, helping to lower the risk of local recurrence and improve overall patient survival.2,3 With advances in RT, high-conformal radiation coverage of the target volumes can be achieved while reducing the radiation dose to adjacent tissues through intensity-modulated radiotherapy (IMRT).4 Numerous clinical studies and dosimetric5 have shown that IMRT results in reduced acute radiation toxicity compared to traditional radiation therapy, while still achieving outstanding local control.
However, when radiation therapy is delivered to pelvic organs, involvement of the healthy parts of the bladder is inevitable Regardless of the type of radiation therapy chosen, genitourinary (GU) toxicity is still a significant complication associated with pelvic radiation therapy.6 Early studies estimated that between 23% and 80% of patients experienced symptoms of acute or early GU toxicity.7
There have also been reports of an association between urinary tract infection (UTI) and pelvic radiation therapy. Bialis et al8 demonstrated a 39% (22 out of 56) rate of UTI in patients receiving conventional pelvic radiation for cervical cancer. Subsequent investigations looked at the rate of UTI in those treated for gynecologic malignancies alone, showing UTI occurred in 40% of patients receiving brachytherapy9 and 33% of patients receiving brachytherapy plus External Beam Radiation Therapy(EBRT).10
UTI affect the quality of life of cervical cancer patients on one hand, and lead to intolerance or discontinuation of radiotherapy on the other, thereby severely impacting the treatment outcomes. How to predict UTI and mitigate adverse reactions is a key focus in the radiotherapy of cervical cancer. To date, no predictive models for urinary tract infections in cervical cancer IMRT patients have been reported, which is worth further exploration.
Therefore, we analyzed the incidence of urinary tract infections and the distribution of pathogens in cervical cancer patients following radiotherapy at People’s Hospital of Ningxia Hui Autonomous Region. Simultaneously, we established a nomogram to predict the risk of urinary tract infections in cervical cancer IMRT patients. It would allow practitioners to estimate the risk of infection, which could help prevent and control UTI in cervical cancer IMRT patients, thus improving patient prognosis and reducing healthcare costs.
Methods
Study Design and Patients
This retrospective cohort study included cervical cancer patients who received IMRT at the People’s Hospital of Ningxia Hui Autonomous Region from January 2020 to December 2023. The inclusion criteria were as follows: (I) primary cervical cancer confirmed by pathology; (II) Cervical cancer patients with first UTI after radiotherapy; (III)complete medical records. The exclusion criteria were: (I)urinary tract malformations;(II)ureteral invasion; (III)a prior UTI before treatment;(IV) immune system diseases, or Long-term use of immunosuppressants; Repeated bacterial colonies in the same patient were excluded. Based on the inclusion and exclusion criteria, this study included clinical data from a total of 160 patients. UTI diagnoses were adjudicated by physicians based on the standardized definition outlined in the evidence-based guidelines for the diagnosis and treatment of urinary tract infections.11
Microbiologic Studies
The susceptibility of the main pathogenic strains isolated from urine to commonly used antimicrobial agents, including penicillins, cephalosporins, carbapenems, aminoglycosides, tetracyclines, macrolides, quinolones, and glycopeptides, was determined using the Kirby-Bauer (K-B) and the MIC method. The antimicrobial susceptibility results were evaluated according to the CLSI standards.12
Data Collection and Establishment of the Model
Based on the factors mentioned in previous similar studies, we collected a total of 11 risk factors: age, comorbid conditions (such as diabetes mellitus and hypertension), stage of cervical cancer, ECOG score, invasive urological procedures (such as intubation or catheterization), concurrent chemotherapy, history of ureteral stent insertion, laboratory test results (eg, albumin levels), planning target volume (PTV) and Bladder dose-volume histogram(DVH). The pathogenic microorganisms and antimicrobial susceptibility results were also documented. The data were extracted from the hospital’s information system. Patients with urinary tract infections were classified into the infection group (n=52), while those without infections were placed in the control group (n=108).
Statistical Analysis
Data were analyzed with the use of SPSS version 21.0 and R software (version 4.1.1). Qualitative data are presented as percentages (%), while categorical variables are expressed as counts and corresponding percentages (%). Continuous variables were tested for normality using the Kolmogorov–Smirnov test. Normally distributed data are presented as the mean ± standard deviation and were analyzed using a t-test. Nonnormally distributed data are expressed as medians (interquartile ranges), and were assessed using the Mann–Whitney U-test.
Investigate the predictive factors in a multivariate logistic regression model based on variables with a p<0.05 in univariate analysis, and report the odds ratios (OR) and 95% confidence intervals (CI). When OR<1, it indicates that the exposure is associated with a decreased risk of UTI. If OR>1, it shows that the exposure is linked to an increased risk of UTI. And OR close to 1 suggests that there is no substantial statistical association between the exposure and UTI risk. P≤0.05 were considered statistically significant. The variance inflation factor (VIF) was less than 5, indicating that there was no multicollinearity among the independent variables. Variables with p≤0.05 in regression analysis were selected to establish a risk prediction model for urinary tract infections in cervical cancer patients using the nomogram method. The predictive model was evaluated on three criteria: discriminatory capacity, calibration ability, and clinical effectiveness. The ROC curve was used to test the predictive ability of the risk prediction model for UTI. The calibration curve and Hosmer-Lemeshow test were used to evaluate its calibration ability. DCA was used to evaluate clinical efficacy.
Results
UTI Incidence and Pathogen Distribution in Cervical Cancer IMRT Patients
Of the 52 urine cultures included in this study, 61 samples were collected during the first episode of bacteriuria. The most common isolates were Escherichia coli (E. coli) (49.18%), Enterococcus faecalis (E. faecalis) (9.84%), Enterococcus faecium (E. faecium) (8.20%), and Proteus mirabilis (P. mirabilis) (8.20%). Detailed information can be found in Table 1.
 |
Table 1 Classification and Constituent Ratio of Pathogens |
Resistance of the Main Pathogens to Commonly Used Antibiotics
Of the 30 E. coli isolates, 76.67% were resistant to ciprofloxacin, and 66.67% were resistant to ceftriaxone. The majority of E. coli and P. mirabilis, 26.67% and 60.0% respectively, were resistant to minocycline (Table 2). The majority of E. faecium and E. faecalis, 100.00% and 50.00% respectively, were resistant to levofloxacin. Among the most common Gram-negative, 70.0% (21/30) of E. coli isolates tested positive for extended-spectrum beta-lactamase (ESBLs), thus exhibiting multidrug resistance.
 |
Table 2 Antimicrobial Resistance of Common Pathogens (%) |
Results of Univariate and Multivariate Analysis
The initial logistic regression analysis of 11 potential variables identified six predictors, including stage of cervical cancer, concurrent chemotherapy, invasive procedures, history of ureteral stent insertion, Serum albumin, and PTV (as shown in the Table 3). Subsequently, the multivariate logistic regression refined these into four independent predictors significantly associated with the development of UTI: History of ureteral stent insertion (OR 7.260, 95% CI:2.026–26.016; P=0.002), invasive operation (OR 4.202, 95% CI:1.003–17.608; P=0.050), concurrent chemotherapy (OR 2.587, 95% CI:1.010–6.623; P=0.048), and Serum albumin (OR 0.842, 95% CI:0.745–0.951; P =0.006) (Table 4).
 |
Table 3 Univariate Analysis of UTI in Cervical Cancer IMRT Patients |
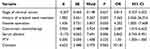 |
Table 4 Multivariate Logistic Analysis of UTI in Cervical Cancer IMRT Patients |
Predictive Model Construction and Validation
Based on these four independent predictors, we developed a nomogram for individualized assessment of UTI risk. The model’s formula integrated the weighted contributions of each predictor: logistic (risk score)=5.31+2.15×history of ureteral stent insertion+1.31×invasive operation+1.06×concurrent chemotherapy-0.18×serum albumin. The higher total scores calculated from the sum of the appointed points for each prognostic indicator in the nomogram, the higher the risk of infection (Figure 1).
The AUC was used to evaluate the discriminatory capacity of the predictive model, and the nomogram demonstrated good accuracy in estimating the risk of UTI. The AUC of ROC was 0.804 (95% CI 0.727–0.881) (Figure 2A). The predicted probability curve of the model was close to the actual curve, and its distribution was not far from the ideal curve, suggesting that the model for predicting infection had good consistency, which was confirmed by the Hosmer-Lemeshow test (P= 0.522)(Figure 2B). Decision curve analysis, as shown in Figure 3, indicates that within the specific probability threshold range of 0.1–0.9, using this model may lead to greater net benefits compared to the “All” and “None” strategies.
Discussion
In this study, we propose a valuable clinical tool to predict the possibility of urinary tract infection in Cervical cancer radiotherapy patients. Our study is the first to develop a nomogram with four features to predict UTI risk in cervical cancer patients with radiotherapy. History of ureteral stent insertion, invasive procedures, serum albumin and concurrent chemotherapy into a nomogram could help forecast the risk of UTI for these patients. This tool enables physicians to systematically assess individual risk factors and predict UTI likelihood, supporting more personalized and preventive therapeutic strategies.
Several studies10,13,14 have investigated the risk factors for UTI in IMRT patients. Previously identified risk factors for UTI include clinical stage and invasive procedures. Other risk factors include concurrent chemotherapy, diabetes, and ureteral stent insertion. In addition to these factors, we also included other factors, such as serum albumin levels. Albumin is the most abundant plasma protein and is closely related to combining and transporting inflammatory mediators and regulating inflammatory response.15,16 Wang Jing et al proved that with the decrease of hypoproteinemia level, it was positively associated with the occurrence of sepsis and septic shock.17 Our study showed that radiotherapy patients with higher serum albumin levels were associated with a 15.8% lower risk of urinary tract infection (OR=0.842).The findings from our study further indicated that when patients experienced hypoproteinaemia at the time of radiotherapy, clinicist should have recognized this as a marker of diminished immune function and a heightened risk for developing UTIs. The current analysis showed an OR of 2.587 for concurrent chemotherapy exposure by UTI patients versus controls, supporting the findings of previous studies.18,19
Ureteral stent, as an allogeneic implant, is prone to forming a urinary regulatory membrane.20 This regulatory membrane can facilitate bacterioplankton adherence through electrostatic interactions and bacterial adhesins, contributing to bacterial colonization within the urinary tract, potentially leading to infections.21 In this study, among 25 patients with ureteral stent placement, bacteria were detected in the urine in 20 patients. Consistent with other studies,22,23 the risk of urinary tract infection in patients with ureteral stent placement is 7.26 times higher than that in patients without ureteral stent placement. Our study results indicate that there is a significant difference in the incidence of UTI between patients who have undergone invasive procedures and those who have not (P=0.050, OR=4.202, 95% CI 1.003–17.608). This difference may be related to the disruption of the normal physiological and immune environment of the urethra caused by invasive procedures.24 Additionally, invasive procedures may also impede the natural flushing action of urine on urinary tract bacteria,25 thereby increasing the risk of infection. Among radiotherapy patients, there are no significant association between PTV, Bladder DVH and the incidence of urinary tract infections.
In addition to developing a predictive model, bacterial cultures and antibiotic resistance profiles were analyzed in cervical cancer patients undergoing radiotherapy to assess urinary tract infections.
The microorganisms most frequently isolated in our study were E. coli. E. coli surface P26 and type I pili27 and adhesin adhesion to the surface of urethral epithelial cells, become the prerequisite for E coli urinary tract infection.28 E. faecium is the most detected Gram-positive coccus among the pathogens, second only to E. coli, and its resistance rate to penicillin and levofloxacin exceeded 50%. Hola et al29 reported that E. coli and E. faecalis were the most common pathogenic bacteria associated with uropathogenic biofilms.
This study has several limitations that may impact the generalizability of our findings. Firstly, it is retrospective in nature, relies on data from a single tertiary hospital cohort, and may be subject to selection bias. Finally, since this study was limited to inpatients, the incidence of urinary tract infections in patients followed up outside the hospital was not included. Moreover, there was insufficient information on patients’comprehensive radiological data, such as the total radiation dose, dose per fraction,30 which could be relevant to UTI development. Further studies are needed to investigate the relationship between UTI in radiotherapy patients and these variables.
In conclusion, the incidence of urinary tract infections in cervical cancer patients after radiotherapy in this study was approximately 32.5%. Our findings indicate that E. coli, P. mirabilis, E. faecalis and E. faecium are the predominant pathogens. We have developed and validated a novel nomogram incorporating four clinical parameters that effectively predicts UTI in cervical cancer IMRT patients. This model, with its excellent calibration performance and outstanding performance in actual clinical applications, is expected to become a powerful tool for clinicians to predict risks. It represents an important step forward in the early identification and management of the risk of urinary tract infections in cervical cancer patients undergoing radiotherapy. However, further validation through external testing is still needed to confirm its effectiveness.
Ethical Approval
The study was approved by the ethical committee of the People’s Hospital of Ningxia Hui Autonomous Region (Approval number 2024-LL-174). This study was conducted in accordance with the principles of the Declaration of Helsinki. The patient information were anonymized and de-identified before analysis. The requirement for informed consent was waived by the Medical Ethics Committee of the People’s Hospital of Ningxia Hui Autonomous Region due to the study’s retrospective nature.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Natural Science Foundation of Ningxia, China (grant no. 2022AAC03528, 2023AAC03479), Ningxia Hui Autonomous Region Health Commission Research Program (2023-NWKYP-007).
Disclosure
The authors declare no competing interests.
References
1. Buskwofie A, David-West G, Clare CA. A review of cervical cancer: incidence and disparities. J Natl Med Assoc. 2020;112(2):229–232. doi:10.1016/j.jnma.2020.03.002
2. Li F, Guo H, Qiu H, et al. Urological complications after radical hysterectomy with postoperative radiotherapy and radiotherapy alone for cervical cancer. Medicine. 2018;97(13):e0173. doi:10.1097/MD.0000000000010173
3. Chargari C, Peignaux K, Escande A, et al. Radiotherapy of cervical cancer. Cancer Radiother. 2022;26(1–2):298–308. doi:10.1016/j.canrad.2021.11.009
4. Huang CM, Huang MY, Tsai HL, et al. A retrospective comparison of outcome and toxicity of preoperative image-guided intensity-modulated radiotherapy versus conventional pelvic radiotherapy for locally advanced rectal carcinoma. J Radiat Res. 2017;58(2):247–259. doi:10.1093/jrr/rrw098
5. Cordoba A, Nickers P, Tresch E, et al. Safety of adjuvant intensity-modulated postoperative radiation therapy in endometrial cancer: clinical data and dosimetric parameters according to the International Commission on Radiation Units (ICRU) 83 report. Rep Pract Oncol Radiother. 2015;20(5):385–392. doi:10.1016/j.rpor.2015.06.002
6. Zuppone S, Bresolin A, Spinelli AE, et al. Pre-clinical research on bladder toxicity after radiotherapy for pelvic cancers: state-of-the art and challenges. Front Oncol. 2020;22(10):527121. doi:10.3389/fonc.2020.527121
7. Marks LB, Carroll PR, Dugan TC, et al. The response of the urinary bladder, urethra, and ureter to radiation and chemotherapy. Int J Radiat Oncol Biol Phys. 1995;31(5):1257–1280. doi:10.1016/0360-3016(94)00431-J
8. Bialas I, Bessell EM, Sokal M, et al. A prospective study of urinary tract infection during pelvic radiotherapy. Radiother Oncol. 1989;16(4):305–309. doi:10.1016/0167-8140(89)90043-1
9. Prasad KN, Pradhan S, Datta NR. Urinary tract infection in patients of gynecological malignancies undergoing external pelvic radiotherapy. Gynecol Oncol. 1995;57(3):380–382. doi:10.1006/gyno.1995.1158
10. Widholm O, Mattsson T. Urinary tract infections in association with radiation therapy for gynecological cancer. Acta Obstet Gynecol Scand. 1972;51(3):247–250. doi:10.3109/00016347209156854
11. Nephrology Group, Paediatrics Society, Chinese Medical Association. Evidence-based guideline on diagnosis and treatment of urinary tract infection (2016). Chin J Pediatr. 2017;55:898–901.
12. CLSI. M100 performance standards for antimicrobial susceptibility testing, 34th edn. 2024. Available from: http://em100.edaptivedocs.net/dashboard.aspx.
13. Boothe D, Patel SH, Stessin A, et al. Comparing the rates of urinary tract infections among patients receiving adjuvant pelvic intensity modulated radiation therapy, 3-dimensional conformal radiation therapy, and brachytherapy for newly diagnosed endometrial cancer. Pract Radiat Oncol. 2013;3(4):269–274. doi:10.1016/j.prro.2012.12.002
14. Wang F, Wang X, Shi Y, et al. Development of a risk nomogram predicting urinary tract infection in patients with indwelling urinary catheter after radical surgery for cervical cancer. Prog Urol. 2023;33(10):492–502. doi:10.1016/j.purol.2023.08.017
15. Hayama T, Ozawa T, Tsukamoto M, et al. Predicting overall survival using preoperative nutritional and inflammation status for colorectal cancer. In Vivo. 2022;36(1):450–457. doi:10.21873/invivo.12724
16. Visser M, Kritchevsky SB, Newman AB, et al. Lower serum albumin concentration and change in muscle mass: the health, aging and body composition study. Am J Clin Nutr. 2005;82(3):531–537. doi:10.1093/ajcn.82.3.531
17. Wiedermann CJ. Hypoalbuminemia as surrogate and culprit of infections. Int J mol Sci. 2021;22(9):4496. doi:10.3390/ijms22094496
18. Millner R, Becknell B. Urinary tract infections. Pediatr Clin North Am. 2019;66(1):1–13. doi:10.1016/j.pcl.2018.08.002
19. Kostakopoulos NA, Karakousis ND, Moschotzopoulos D. Frailty associated urinary tract infections (FaUTIs). J Frailty Sarcopenia Falls. 2021;6(01):9–13. doi:10.22540/JFSF-06-009
20. Scotland KB, Lo J, Grgic T, et al. Ureteral stent-associated infection and sepsis: pathogenesis and prevention: a review. Biofouling. 2019;35(1):117–127. doi:10.1080/08927014.2018.1562549
21. Ozgur BC, Ekici M, Yuceturk CN, et al. Bacterial colonization of double J stents and bacteriuria frequency. Kaohsiung J Med Sci. 2013;29(12):658–661. doi:10.1016/j.kjms.2013.01.017
22. Riedl CR, Plas E, Hubner WA, et al. Bacterial colonization of ureteral stents. Eur Urol. 1999;36(1):53–59. doi:10.1159/000019927
23. Altunal N, Willke A, Hamzaoğlu O. Ureteral stent infections: a prospective study. Braz J Infect Dis. 2017;21(3):361–364. doi:10.1016/j.bjid.2016.12.004
24. Cortese YJ, Wagner VE, Tierney M, et al. Review of catheter-associated urinary tract infections and in vitro urinary tract models. J Healthc Eng. 2018;2018:2986742. doi:10.1155/2018/2986742
25. Mengatto MF, Castro BGR, Nobrega L, et al. Early removal of indwelling urinary catheter after radical surgery for early-stage cervical cancer-A cohort study. J Surg Oncol. 2020;122(7):1498–1505. doi:10.1002/jso.26167
26. Mortezaei N, Epler CR, Shao PP, et al. Structure and function of enterotoxigenic Escherichia coli fimbriae from differing assembly pathways. Mol Microbiol. 2015;95(1):116–126. doi:10.1111/mmi.12847
27. Spaulding CN, Schreiber HL, Zheng W, et al. Functional role of the type 1 pilus rod structure in mediating host-pathogen interactions. Elife. 2018;18(7):e31662. doi:10.7554/eLife.31662
28. Wurpel DJ, Beatson SA, Totsika M, et al. Chaperone-usher fimbriae of Escherichia coli. PLoS One. 2013;8(1):e52835. doi:10.1371/journal.pone.0052835
29. Holá V, Ruzicka F, Horka M. Microbial diversity in biofilm infections of the urinary tract with the use of sonication techniques. FEMS Immunol Med Microbiol. 2010;59(3):525–528. doi:10.1111/j.1574-695X.2010.00703.x
30. Ma JL, Hennessey DB, Newell BP, et al. Radiotherapy-related complications presenting to a urology department: a more common problem than previously thought? BJU Int. 2018;121(3):28–32. doi:10.1111/bju.14145
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




