Back to Journals » Infection and Drug Resistance » Volume 18
Evaluating the Performance of Two Rapid Immunochromatographic Techniques for Detecting Carbapenemase in Carbapenem-Resistant Enterobacterales Clinical Isolates
Authors Liu P, Qin M, Zhao C , Yi S, Ye M, Liao K, Deng J, Chen Y
Received 20 November 2024
Accepted for publication 6 March 2025
Published 13 March 2025 Volume 2025:18 Pages 1415—1424
DOI https://doi.org/10.2147/IDR.S506021
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandip Patil
Pingjuan Liu,1,* Mengling Qin,2,* Chenfeng Zhao,1,* Siting Yi,3 Mengmin Ye,3 Kang Liao,1 Jiankai Deng,1 Yili Chen1
1Department of Laboratory Medicine, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, Guangdong, 510080, People’s Republic of China; 2Department of Laboratory Medicine, Hainan West Central Hospital, Hainan, 571700, People’s Republic of China; 3Department of Laboratory Medicine, The East Division of The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, Guangdong, 510080, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yili Chen; Jiankai Deng, Department of Laboratory Medicine, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, 510080, People’s Republic of China, Email [email protected]; [email protected]
Introduction: The rapid and accurate identification of carbapenemases in Enterobacterales isolates is of paramount importance for the selection of effective antibiotics and the control of hospital-acquired infections.
Methods: This study aimed to evaluate the performance of two immunochromatographic methods, NG-Test Carba 5 (Carba 5) and Goldstream Carbapenem-resistant K.N.I.V.O. Detection K-Set (K-Set) for detecting five major carbapenemase (KPC, NDM, IMP, OXA-48-like, and VIM). Carbapenemase genes were confirmed by PCR.
Results: In this study, a total of 245 carbapenem-resistant Enterobacterales (CRE) isolates were encompassed, with an overwhelming 96.7% of these strains exhibiting the ability to produce carbapenemase. A total of 58.2% of Klebsiella pneumoniae strains that produce KPC carbapenemase were the most prevalent among carbapenem-resistant Enterobacteriaceae (CRE). NDM-producing Klebsiella pneumoniae accounted for 30.4%. Importantly, NDM-type carbapenemase emerges as the predominant form in Escherichia coli and Enterobacter cloacae strains, accounting for 46 (93.9%) and 20 (83.3%) cases, respectively. The performance of the two methods in carbapenemase detection has demonstrated remarkable outcomes, exhibiting overall specificity and sensitivity exceeding 99%. Specifically, the K-Set accurately detected a unique KPC-carbapenemase in K. pneumoniae, whereas Carba 5 was unable to identify it. This was due to the presence of a novel blaKPC gene, which harbored a specific point mutation (A to G) at nucleotide position 787, differentiating it from the blaKPC-33 gene.
Conclusion: These two methods, characterized by their simplicity, rapidity, and accuracy, are ideally suited for detecting carbapenemases in routine microbiology laboratories. They serve as a vital foundation for the rational selection of antibiotics in clinical practice.
Keywords: carbapenem-resistant Enterobacterales, CRE, carbapenemase gene, rapid immunochromatographic
Introduction
Carbapenem-resistant Enterobacterales (CRE) are designated as urgent and serious threats by the Centers for Disease Control and Prevention (CDC) of the United States.1 In recent years, CRE has emerged as a significant challenge in the field of global public health, posing substantial difficulties and challenges to clinical treatment, particularly carbapenem-resistant Klebsiella pneumoniae (CRKP) and Escherichia coli.2 They can cause urinary tract infections, respiratory tract infection, bloodstream infection, meningitis, malignant external otitis, intra-abdominal infection, and wound infections.3,4 It is worth noting that CRE infections are becoming a severe problem due to limited availability of effective treatment options and poor prognosis. We previously reported that the mortality associated with carbapenem-resistant K. pneumoniae bloodstream infections (CRKP-BSI) was significantly higher (48.3%) in elderly patients.5 Generally, carbapenemases include Klebsiella pneumoniae carbapenemase (KPC), imipenemase (IMP), New Delhi metallo-β-lactamase (NDM), Verona integron-encoded metallo-β-lactamase (VIM), and oxacillinase (OXA)-48-like enzymes.6,7 Currently, it has been reported that blaKPC is the predominant gene for K. pneumoniae and blaNDM is the predominant gene for E. coli in China.3,8 Therefore, rapid and accurate identification of carbapenemases is of upmost importance, not only conducive to epidemic control and clinical decision-making but also helping to rapidly optimize antibiotic treatment.9–12
Phenotypic confirmation tests recommended by the Clinical and Laboratory Standards Institute (CLSI) guidelines, such as the modified carbapenem inactivation test, have been developed for the detection of carbapenemase.13 This phenotypic method for the detection of carbapenemases is generally effective, but it is time-consuming and cannot accurately classify the enzymes produced.14 Gene detection methods are considered the gold standard, such as traditional PCR and Xpert Carba-R, which can directly identify carbapenemase genes with high sensitivity and specificity.3,15 However, PCR-based methods may require expensive instruments and reagents, which limits their application in many laboratories. In addition, this method may fail to detect new or rare types of carbapenemase genes.14,16 As rapid immunochromatographic methods, Carba 5 and K-Set are recently developed, featuring simple experimental procedures and short turn-around times (TATs). They are promising methods for the rapid detection of carbapenemases.17,18 However, the distribution of bacterial epidemiology and drug resistance varies greatly across different regions. For Guangdong Province in southern China, data on the carbapenemase genes are very limited, and t few evaluation studies on the rapid detection of carbapenemases have been conducted thus far.
In this study, we collected clinical CRE strains from multiple centers in Guangdong Province to compare the performance of two immunochromatographic methods, Carba 5 and K-Set, in detecting five major carbapenemases (KPC, NDM, IMP, OXA-48-like, and VIM). The purpose of this study is to provide a wealth of information for laboratories to choose the detection methods of carbapenemase.
Materials and Methods
Clinical Bacterial Isolates
This multicenter clinical study was conducted at eight tertiary general hospitals in Guangdong, China, during the period from January 2018 to December 2021. In total, 245 isolates of Enterobacteriaceae showing carbapenem resistance were included in the retrospective analysis. According to the Clinical and Laboratory Standards Institute (CLSI) M100 Edition 34, carbapenem resistance was defined as a minimum inhibitory concentration (MIC) of ≥4 mg/L for meropenem or imipenem, or ≥2 mg/L for ertapenem. Both of them were designed to identify the five major carbapenemases (KPC, NDM, IMP, OXA-48-like, and VIM). Isolates were stored at −80°C, incubated overnight on Columbia agar with 5% sheep blood (Autobio, Zhengzhou) and incubated at 35±2°C in 5% CO2. All bacterial species were subcultured twice prior to testing to ensure the purity of the strains and were identified by MALDI-TOF MS (VITEK® MS, Bio Mérieux). Two ATCC prototype isolates, K. pneumoniae BAA-1706 and BAA-1705, were used as quality controls in each run.
Targeted PCR
All isolates included were screened for the presence of carbapenemase genes using targeted PCR, gene names and corresponding primer sequence references19 including blaKPC, blaNDM, blaIMP, blaVIM, and blaOXA−48. DNA, used as a template in PCR, was extracted by boiling. The primers used to amplify specific carbapenemase genes in this study are shown in Table 1.
 |
Table 1 Primer Sequence and Fragment Length of the Carbapenemase Gene |
NG-Test CARBA 5 Assay (“CARBA 5”)
According to the manufacturer’s instructions, five drops of extraction buffer were added, and then a full loop (1 µL) of bacterial colonies from a culture plate was mixed. Containing the strain for 10 min, 5 drops of the diluted sample were dispensed into the Carba 5 sample test strip. The results were observed with the naked eye after 15 min of incubation at room temperature.
Goldstream Carbapenem-Resistant K.N.I.V.O. Detection K-Set (“K-Set”)
Goldstream carbapenem-resistant K.N.I.V.O. Detection K-Set (Beijing Gold Mountainriver Tech Development Co, Ltd) is a rapid test based on immunochromatography. A single colony bacterial isolate was added to 10 drops of lysis solution, and then 50 µL of the mixture was added onto the cassette after mixing, according to the reagent instructions. The results were interpreted after 10 minutes.
Whole-Genome Sequencing and Bioinformatics Analysis
Genomic DNA of the selected isolates was extracted using a DNA extraction kit (Magen, Guangzhou, China), and 150 bp paired-end reads were obtained using an Illumina NextSeq 550 system (Illumina, San Diego, CA, USA). For whole-genome sequencing (WGS) data, at least 100-fold coverage of original reads was obtained, and the assembly draft of the sequences was generated by SPAdes.20
Data Analysis
Taking the results from targeted PCR as the reference standard, the performance of Carba 5 and K-Set was compared by analyzing the sensitivity and specificity. Statistical analysis was conducted using the SPSS 20.0 software. The comparison of rates was conducted using a chi square test, with P<0.05 indicating statistical significance. Simultaneously conducting kappa value consistency analysis, with P<0.01, it is considered that the consistency between the two methods is statistically significant. Kappa value ≥0.75 indicates good consistency; Kappa values ranging from 0.40 to <0.75 indicate moderate consistency; Kappa value <0.40 indicates poor consistency.
Results
Carbapenemase Gene Detection Results
A total of 245 non-replicative CRE isolates were collected in this study, including 70.2% (172/245) strains of K. pneumoniae, 20.0% (49/245) E. coli strains, and 9.8% (24/245) E. cloacae strains. Almost all K. pneumoniae (96.5% against Imipenem, 98.2% against Meropenem) have a MIC ≥ 16 mg/L; The MIC values of E. coli against these two antibiotics are also relatively high, with 87.8% and 91.8% of E. coli strains having MIC ≥ 16 mg/L against Imipenem and Meropenem, respectively. 54.2% of E. cloacae had a MIC ≥ 16 mg/L against Imipenem, and 66.7% had a MIC ≥ 16 mg/L against Meropenem. Characteristics of CREs antimicrobial resistance to carbapenems are detailed in Table 2.
 |
Table 2 Characteristics of CREs Antimicrobial Resistance to Carbapenems |
Among 245 CRE strains, 96.7% (237/245) produced carbapenemase, 60.8% (149/245) of which carried blaKPC, 31.8% (78/245) carried blaNDM, 0.8% (2/245) had blaIMP, 0.4% (1/245) had blaOXA-48-like, and 2.8% (7/245) had multiple genes detected (1 with blaKPC-blaNDM, 1 with blaOXA-48-like-blaIMP, and 5 with blaNDM-blaIMP), as shown in Table 3.
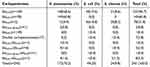 |
Table 3 Types of Carbapenemase Genes Detected by PCR Among the 245 Solates of Enterobacteriaceae |
Consistency Evaluation of CARBA 5 for Carbapenemase Genotype Detection Results
The consistency between CARBA 5 and PCR methods for the detection of five types of carbapenemases is shown in Table 4. Among the 245 CRE screening positive samples, CARBA 5 reagent detected 236 cases of producing carbapenemases and 9 cases of not producing carbapenemases. Some positive results are shown in Figure 1. Among them, one case of CARBA 5 detection with non-producing carbapenemases did not match the PCR method, with a positive consistency rate of 99.58% (236/237). The total agreement rate of the two methods for the detection of five carbapenems was 99.59% (244/245). Kappa consistency test: The kappa value for KPC was 0.990 (P<0.001), while the kappa values for NDM, IMP, and OXA-48 like were all 1 (P<0.001); The kappa values for the simultaneous production of two carbapenems, NDM+IMP, KPC+NDM, and OXA-48-like+NDM, were all 1 (P=0.008). The CARBA 5 detection method and PCR method have high consistency and accuracy in detecting different types of carbapenemase genes, whether it is single gene or multi-gene detection.
 |
Table 4 CARBA 5 and Agreement Evaluation of PCR Results for Carbapenemase Isolates (n) |
 |
Figure 1 Positive results shown by Carba 5. Left: OXA-48-like positive, middle: KPC positive, right: NDM and IMP positive. |
Consistency Evaluation of K-Set for Carbapenemase Genotype Detection Results
The consistency between K-Set and PCR methods for the detection of five carbapenemases is shown in Table 5. Among the 245 CRE screening positive samples, the K-Set reagent detected 237 cases of carbapenemase production and 8 cases of non-production, with a positive consistency rate of 100% (237/237). Some positive results are shown in Figure 2. The total agreement rate of the two methods for the detection of five carbapenems was 100% (245/245). Kappa consistency test: The kappa values for KPC, NDM, IMP, and OXA-48 like were all 1 (P<0.001); The kappa values for the simultaneous production of two carbapenems, NDM+IMP, KPC+NDM, and OXA-48-like+NDM, were all 1 (P=0.008). The K-Set and PCR detection methods have high consistency and accuracy in detecting different types of carbapenemase genes, whether it is single gene or multi-gene detection.
 |
Table 5 K-Set and Agreement Evaluation of PCR Results for Carbapenemase Isolates (n) |
 |
Figure 2 Positive results shown by K-Set. From left to right, it represents IMP, NDM, OXA-48, and KPC positivity, respectively. |
Discovery and Sequencing Results of a K. pneumonia Strain Producing blaKPC-145
Specifically, one KPC-carbapenemase of K. pneumonia was accurately detected by the K-Set but failed to be detected by Carba 5. Whole genome sequencing confirmed that this K. pneumonia isolate (CZHKP-07) harbored a novel blaKPC gene with a point mutation (A to G) at nucleotide position 787 compared with the blaKPC-33 gene. This mutation resulted in the amino acid substitution of threonine to alanine (T263A), assigned by GenBank as blaKPC-145 (accession number: OP626310).
Discussion
The emergence and spread of carbapenemase-producing Enterobacteriaceae (CPE) undoubtedly pose a significant public health challenge because CPE is often resistant to multiple antibiotics and has limited treatment options.1,3,6,21 The production of carbapenemase is the primary mechanism of carbapenem resistance. Other mechanisms, such as overproduction or broad-spectrum of AmpC β-lactamase can also contribute to the lack of outer membrane protein and the overproduction of some efflux pumps, thus conferring carbapenem resistance.22 Previous studies have indicated that CPE is the predominant type of CRE, with prevalence rates ranging from 77.3% to 91.3%.23–26 Therefore, the rapid detection and identification of CPE are essential to enable physicians to quickly implement appropriate infection control measures, rapidly adapt antibiotic treatment, and optimize care strategies and outcomes.
In terms of treatment, the choice of drugs to treat CRE infection depends on specific carbapenemases.27 For KPC and OXA-48-like enzymes, ceftazidime-avibactam can be the preferred agent.26,28,29 If Enterobacterales isolates produce NDMs (or any other metallo-β-lactamase), the preferred antibiotic is ceftazidime avibactam combined with aztreonam.30,31 Therefore, given the distinctive features of different carbapenemases, rapid and reliable discrimination between these carbapenemases will provide valuable information for appropriate treatment.
In this study, 96.7% (237/245) of clinical CRE were carbapenemase-producing Enterobacterales strains, indicating that carbapenemase production is the prominent mechanism of CRE in Guangdong, China. A total of 58.2% of K. pneumoniae producing KPC carbapenemase was the most common CRE. NDM-producing K. pneumoniae accounted for 30.4%. Significantly, NDM-type is the primary carbapenemase among E. coli and E. cloacae strains, accounting for 46 (93.9%) and 20 (83.3%), respectively. In Chinese adults, KPC is reported as the most predominant carbapenemase (81%) of CP-kpn, while NDM-kpn is more prevalent in infants and neonates (61%~87.2%).32–34 A study found that NDM accounted for 73.8% of Enterobacter cloacae carbapenemases, far lower than our research results, indicating that CPE has different molecular and epidemiological characteristics in different geographical regions.35 Therefore, it is very important to monitor and master the characteristics of enzyme production of strains in each region. Moreover, carbapenemase coproducing strains pose an important diagnostic challenge. It is worth noting that in our study, seven isolates coproduced two types of carbapenemases, including NDM+IMP (n=5), KPC+NDM (n=1) and OXA-48 like+IMP, n=1), which were also accurately identified by the two methods. Considering that strains producing multiple carbapenemases at the same time are increasingly common, for example, in Guangdong, we need to pay special attention to the simultaneous carrying of NDM+IMP.
Carba 5 and K-Set are two commercial immunological enzyme detection reagents for the detection of five major carbapenemases (KPC, NDM, VIM, IMP, and OXA-48). Carba 5 is a multiplex immunochromatographic test that can detect the five major carbapenemases simultaneously in a single test cassette. K-Set is a monoplex immunochromatographic test that can detect the five major carbapenemases separately or simultaneously. In addition to being easy to use, they also showed results in 15 minutes. Our research shows that, compared with the PCR method, K-Set is very suitable for identifying five major carbapenemases, with a sensitivity and specificity of 100%. Another study has also shown that this kit could classify almost all carbapenemase-producing strains within its detection range due to its high sensitivity (99.28%) and specificity (100%).21 In the study results of Mustafa Sadek, the sensitivity and specificity of K-Set for detecting the 5 major carbapenemases were 100% and 98.8%, respectively, which are almost consistent with the results in the present study.36 The sensitivity of 99.6% and the specificity of 100% obtained by Carba 5 in this study also confirmed that it is a relatively accurate method for detecting carbapenemase, which is consistent with other studies.17 A multicenter study in the United States showed that Carba 5 has 100% sensitivity and specificity in detecting five major carbapenemase families.37
Recently, various KPC variants resistant to ceftazidime-avibactam have emerged in clinical settings. The most critical phenotypic features of KPC variants are their resistance to ceftazidime-avibactam and their restoration of susceptibility to meropenem or imipenem. The most common resistance mechanism is the expression of KPC variants characterized by single amino acid substitutions in the Ω-loop region, leading to the lateral flow immunoassays, and main phenotypic carbapenemase detection methods fail to detect these variants with diminished carbapenemase activity.38–42 Currently, it has been documented that Carba 5 has poor diagnostic ability for detecting various KPC variants with mutations in Ω-loops, such as KPC-33, KPC-31 and KPC-203 variant.43,44 KPC-33, a new subtype of KPC, has been detected in several regions and countries and is easily overlooked due to the inconspicuous characteristics of carbapenem resistance.38,41 In our study, we also identified a KPC variant, called KPC-145. Whole genome sequencing confirmed that this K. pneumoniae isolate (CZHKP-07) harbored a novel blaKPC gene with a point mutation (A to G) at nucleotide position 787 compared with the blaKPC-33 gene. This mutation resulted in the amino acid substitution of threonine to alanine (T263A), assigned by GenBank as blaKPC-145 (accession number: OP626310). However, this KPC variant was accurately detected by K-Set but failed to be detected by Carba 5. It is believed that K-Set has a certain ability to detect KPC variants, but we will need more data to confirm this hypothesis in the future. Phenotype detection methods are the most widely used and cost-effective approaches for detecting carbapenemases in clinical microbiology laboratories. However, failure to identify isolates producing KPC enzymes may promote their widespread dissemination in healthcare settings. Thus, clinical laboratories must find appropriate detection methods to identify these strains and should constantly improve existing detection methods to better detect new KPC mutations.
The study has several limitations that should be acknowledged. Firstly, the collection of isolates may contain clones that were not identified or accounted for, which could introduce bias in our analysis and interpretation of the data. Then, not all carbapenemases were subjected to molecular characterization. Future studies should consider incorporating these molecular approaches to provide a more comprehensive understanding of the strains and resistance mechanisms involved.
Conclusions
It is important to highlight that both Carba 5 and K-Set are simple, rapid and accurate methods with high specificity and sensitivity for detecting CRE carbapenemase, which still have extensive application value in clinical practice in China. Therefore, the most appropriate carbapenemase detection method should be selected according to the actual situation of the laboratory and the epidemiological background of carbapenemase.
Data Sharing Statement
The sequence of blaKPC-145 has been deposited into GenBank under accession no. OP626310.
Ethical Approval and Informed Consent Statement
This report was approved by the Clinical Research and Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University. It was a purely retrospective study that did not involve patients during data collection, and informed consent was not needed. All the bacterial isolates in this study were isolated prior to this study for routine hospital laboratory procedure. The authors stated that all methods of this study were carried out in accordance with the Declaration of Helsinki.
Acknowledgments
We thank Prof Yu Guangchao, Clinical Laboratory Center of the First Affiliated Hospital of Jinan University, Prof Liang Jiayin, Department of Clinical Laboratory of the Third Affiliated Hospital of Sun Yat-sen University, Prof Lu Jinghui, Department of Clinical Laboratory of the First Affiliated Hospital of Guangdong Pharmaceutical University, Prof Sun Hengbiao, Department of Clinical Laboratory of the Third Affiliated Hospital of Southern Medical University, Prof Wu Kuihai, Department of Clinical Laboratory of the First People’s Hospital of Foshan City, Guangdong Province, Jinsong Wu, Professor of Shenzhen People’s Hospital of the Second Clinical Medical College of Jinan University, and Liu Xiaoqiang, Professor of Clinical Laboratory of the Second Affiliated Hospital of Sun Yat-sen University for providing experimental strains for this study.
Funding
This work was supported by National Natural Science Foundation of China (82302599) and Guangdong Natural Science Foundation (2023A1515011252).
Disclosure
The authors declare no conflicts of interest. This paper has been uploaded to ResearchSquare as a preprint: https://www.researchsquare.com/article/rs-2454925/v1
References
1. CDC’s Antibiotic Resistance Threats in the United States, 2019. Available Online: Https://Www.Cdc.Gov/Drugresistance/Biggest-Threats.Html.
2. Jin X, Zhang H, Wu S, et al. Multicenter evaluation of xpert carba-R assay for detection and identification of the carbapenemase genes in rectal swabs and clinical isolates. J. Mol. Diagn. JMD. 2021;23:111–119. doi:10.1016/j.jmoldx.2020.10.017
3. Cai Z, Tao J, Jia T, et al. Multicenter evaluation of the xpert carba-R assay for detection and identification of carbapenemase genes in sputum specimens. J. Clin. Microbiol. 2020;58:e00644–20. doi:10.1128/JCM.00644-20
4. Abdeta A, Bitew A, Fentaw S, et al. Phenotypic characterization of carbapenem non-susceptible gram-negative bacilli isolated from clinical specimens. PLoS One. 2021;16:e0256556. doi:10.1371/journal.pone.0256556
5. Chen Y, Chen Y, Liu P, et al. Risk factors and mortality for elderly patients with bloodstream infection of carbapenem resistance Klebsiella pneumoniae: a 10-year longitudinal study. BMC Geriatr. 2022;22:573. doi:10.1186/s12877-022-03275-1
6. Bonomo RA, Burd EM, Conly J, et al. Carbapenemase-producing organisms: a global scourge. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;66:1290–1297. doi:10.1093/cid/cix893
7. Corcione S, Lupia T, Maraolo AE, Mornese Pinna S, Gentile I, De Rosa FG. Carbapenem-sparing strategy: carbapenemase, treatment, and stewardship. Curr Opin Infect Dis. 2019;32:663–673. doi:10.1097/QCO.0000000000000598
8. Zhang Z, Wang D, Li Y, Liu Y, Qin X. Comparison of the performance of phenotypic methods for the detection of carbapenem-resistant Enterobacteriaceae (CRE) in clinical practice. Front Cell Infect Microbiol. 2022;12:849564. doi:10.3389/fcimb.2022.849564
9. Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;72:e169–e183. doi:10.1093/cid/ciaa1478
10. Doi Y. Treatment options for carbapenem-resistant gram-negative bacterial infections. Clin Infect Dis Off Publ Infect Dis Soc Am. 2019;69:S565–S575. doi:10.1093/cid/ciz830
11. Humphries RM, McKinnell JA. Continuing challenges for the clinical laboratory for detection of carbapenem-resistant Enterobacteriaceae. J Clin Microbiol. 2015;53:3712–3714. doi:10.1128/JCM.02668-15
12. Hong JS, Yoon E-J, Lee H, Jeong SH, Lee K. Clonal dissemination of pseudomonas aeruginosa sequence type 235 isolates carrying BlaIMP-6 and emergence of BlaGES-24 and BlaIMP-10 on novel genomic islands PAGI-15 and −16 in South Korea. Antimicrob Agents Chemother. 2016;60:7216–7223. doi:10.1128/AAC.01601-16
13. Mathers AJ, Carroll J, Sifri CD, Hazen KC. Modified Hodge test versus indirect carbapenemase test: prospective evaluation of a phenotypic assay for detection of Klebsiella pneumoniae carbapenemase (KPC) in Enterobacteriaceae. J Clin Microbiol. 2013;51:1291–1293. doi:10.1128/JCM.03240-12
14. Tamma PD, Simner PJ. Phenotypic detection of carbapenemase-producing organisms from clinical isolates. J Clin Microbiol. 2018;56:e01140–18. doi:10.1128/JCM.01140-18
15. Baeza LL, Pfennigwerth N, Greissl C, et al. Comparison of five methods for detection of carbapenemases in Enterobacterales with proposal of a new algorithm. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2019;25:
16. Pierce VM, Simner PJ, Lonsway DR, et al. Modified carbapenem inactivation method for phenotypic detection of carbapenemase production among Enterobacteriaceae. J Clin Microbiol. 2017;55:2321–2333. doi:10.1128/JCM.00193-17
17. Zhu Y, Jia P, Li X, et al. Carbapenemase detection by NG-test CARBA 5-a rapid immunochromatographic assay in carbapenem-resistant Enterobacterales diagnosis. Ann Transl Med. 2021;9:769. doi:10.21037/atm-20-8216
18. Zhang A, Wang X, Liang X, et al. Performance evaluation of diagnostic assays for detection and classification of carbapenemase-producing organisms. Antibiot Basel Switz. 2021;10:1457. doi:10.3390/antibiotics10121457
19. Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes[J]. Diagnostic Microbiol Infectious Dis. 2011;70(1):119–123. doi:10.1016/j.diagmicrobio.2010.12.002
20. Bankevich A, Nurk S, Antipov D, et al. SPAdes: a new genome assembly algorithm and its applications to single cell sequencing[J]. J Computational Biol. 2012;19(5):455–477. doi:10.1089/cmb.2012.0021
21. Roca I, Akova M, Baquero F, et al. The global threat of antimicrobial resistance: science for intervention. New Microbes New Infect. 2015;6:22–29. doi:10.1016/j.nmni.2015.02.007
22. Iovleva A, Doi Y. Carbapenem-Resistant Enterobacteriaceae. Clin Lab Med. 2017;37:303–315. doi:10.1016/j.cll.2017.01.005
23. Teixeira P, Pinto N, Henriques I, Tacão M. KPC-3-, GES-5-, and VIM-1-producing Enterobacterales isolated from urban ponds. Int J Environ Res Public Health. 2022;19:5848. doi:10.3390/ijerph19105848
24. Segagni Lusignani L, Presterl E, Zatorska B, Van den Nest M, Diab-Elschahawi M. Infection control and risk factors for acquisition of carbapenemase-producing Enterobacteriaceae. A 5 year (2011-2016) case‒control study. Antimicrob Resist Infect Control. 2020;9:18. doi:10.1186/s13756-019-0668-2
25. Arum N, Ghafur A, Kazi M, et al. Prevalence of fecal carriage of carbapenemase producing Enterobacteriaceae in healthy Indian subjects from the community. Ind J Med Microbiol. 2022;40:374–377. doi:10.1016/j.ijmmb.2022.05.010
26. Zou C, Wei J, Shan B, Chen X, Wang D, Niu S. In vitro activity of ceftazidime-avibactam and aztreonam-avibactam against carbapenem-resistant Enterobacteriaceae isolates collected from three secondary hospitals in southwest china between 2018 and 2019. Infect Drug Resist. 2020;13:3563–3568. doi:10.2147/IDR.S273989
27. Tamma PD, Hsu AJ. Defining the role of novel β-lactam agents that target carbapenem-resistant gram-negative organisms. J Pediatr Infect Dis Soc. 2019;8:251–260. doi:10.1093/jpids/piz002
28. de Jonge BLM, Karlowsky JA, Kazmierczak KM, Biedenbach DJ, Sahm DF, Nichols WW. In vitro susceptibility to ceftazidime-avibactam of carbapenem-nonsusceptible Enterobacteriaceae isolates collected during the INFORM global surveillance study (2012 to 2014). Antimicrob Agents Chemother. 2016;60:3163–3169. doi:10.1128/AAC.03042-15
29. Castanheira M, Doyle TB, Collingsworth TD, Sader HS, Mendes RE. Increasing frequency of OXA-48-producing Enterobacterales worldwide and activity of ceftazidime/avibactam, meropenem/vaborbactam and comparators against these isolates. J Antimicrob Chemother. 2021;76:3125–3134. doi:10.1093/jac/dkab306
30. Shaw E, Rombauts A, Tubau F, et al. Clinical outcomes after combination treatment with ceftazidime/avibactam and aztreonam for NDM-1/OXA-48/CTX-M-15-producing Klebsiella pneumoniae infection. J Antimicrob Chemother. 2018;73:1104–1106. doi:10.1093/jac/dkx496
31. Falcone M, Daikos GL, Tiseo G, et al. Efficacy of ceftazidime-avibactam plus aztreonam in patients with bloodstream infections caused by metallo-β-lactamase-producing Enterobacterales. Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;72:1871–1878. doi:10.1093/cid/ciaa586
32. Wang M, Earley M, Chen L, et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Klebsiella pneumoniae complex among patients from different global regions (CRACKLE-2): a prospective, multicenter, cohort study. Lancet Infect Dis. 2022;22:401–412. doi:10.1016/S1473-3099(21)00399-6
33. Berglund B, Hoang NTB, Lundberg L, et al. Clonal spread of carbapenem-resistant Klebsiella pneumoniae among patients at admission and discharge at a Vietnamese neonatal intensive care unit. Antimicrob Resist Infect Control. 2021;10:162. doi:10.1186/s13756-021-01033-3
34. Yin D, Zhang L, Wang A, et al. Clinical and molecular epidemiologic characteristics of carbapenem-resistant Klebsiella pneumoniae infection/colonization among neonates in China. J Hosp Infect. 2018;100:21–28. doi:10.1016/j.jhin.2018.05.005
35. Rasheed JK, Kitchel B, Zhu W, et al. New delhi metallo-β-lactamase-producing Enterobacteriaceae, United States. Emerg Infect Dis. 2013;19:870–878. doi:10.3201/eid1906.121515
36. Sadek M, Bouvier M, Kerbol A, Poirel L, Nordmann P. Evaluation of novel immunological rapid test (K.N.I.V.O. Detection K-Set) for rapid detection of carbapenemase producers in multidrug-resistant gram negatives. Diagn Microbiol Infect Dis. 2022;104:115761. doi:10.1016/j.diagmicrobio.2022.115761
37. Jenkins S, Ledeboer NA, Westblade LF, et al. Evaluation of NG-test carba 5 for rapid phenotypic detection and differentiation of five common carbapenemase families: results of a multicenter clinical evaluation. J Clin Microbiol. 2020;58:e00344–20. doi:10.1128/JCM.00344-20
38. Shi Q, Yin D, Han R, et al. Emergence and recovery of ceftazidime-avibactam resistance in BlaKPC-33-harboring Klebsiella pneumoniae sequence type 11 isolates in China. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71:S436–S439. doi:10.1093/cid/ciaa1521
39. Oueslati S, Iorga BI, Tlili L, et al. Unraveling Ceftazidime/Avibactam resistance of KPC-28, a KPC-2 variant lacking carbapenemase activity. J Antimicrob Chemother. 2019;74:2239–2246. doi:10.1093/jac/dkz209
40. Lebreton F, Corey BW, McElheny CL, et al. Characterization of KPC-82, a KPC-2 variant conferring resistance to ceftazidime-avibactam in a carbapenem-nonsusceptible clinical isolate of citrobacter koseri. Antimicrob Agents Chemother. 2021;65:e0015021. doi:10.1128/AAC.00150-21
41. Venditti C, Butera O, Meledandri M, et al. Molecular analysis of clinical isolates of ceftazidime-avibactam-resistant Klebsiella pneumoniae. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2021;27:
42. Bianco G, Boattini M, Comini S, et al. Implementation of chromatic super CAZ/AVI® medium for active surveillance of ceftazidime-avibactam resistance: preventing the loop from becoming a spiral. Eur J Clin Microbiol Infect Dis. 2022;41:1165–1171. doi:10.1007/s10096-022-04480-x
43. Ding L, Shi Q, Han R, et al. Comparison of four carbapenemase detection methods for BlaKPC-2 variants. Microbiol Spectr. 2021;9:e00954–21. doi:10.1128/Spectrum.00954-21
44. Bianco G, Boattini M, Iannaccone M, et al. Carbapenemase detection testing in the era of ceftazidime/avibactam-resistant KPC-producing Enterobacterales: a 2-year experience[J]. J Global Antimicrobial Resistance. 2021;24:411–414. doi:10.1016/j.jgar.2021.02.008
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

