Back to Journals » Journal of Pain Research » Volume 18
Evolution of the Quality of Life of Long-Term Fibromyalgia Users of Millimeter Wave-Based Neuromodulation: A Real-World Retrospective Study
Authors Minier L, Zanini P, Chipon E, Gonon-Demoulian R, Treillet E, Crouzier D
Received 6 November 2024
Accepted for publication 25 February 2025
Published 10 March 2025 Volume 2025:18 Pages 1143—1157
DOI https://doi.org/10.2147/JPR.S498935
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Dawood Sayed
Laure Minier,1 Paolo Zanini,1 Emilie Chipon,1 Raphaël Gonon-Demoulian,2 Erwan Treillet,3,4 David Crouzier1
1Medical Research, Remedee Labs, Montbonnot Saint-Martin, France; 2Pain, Psychosomatics and Functional Disease Department, Montpellier University hospital, Montpellier, France; 3Pain Management and Palliative Care Unit, APHP Lariboisière Hospital, Paris, France; 4Pain Management, Colmar Civil Hospital, Colmar, France
Correspondence: Emilie Chipon, Remedee Labs, 99 chemin de l’étoile, 38330, Montbonnot Saint-Martin, France, Email [email protected]
Purpose: Fibromyalgia (FM) is a widespread pain condition, associated with other symptoms such as fatigue, sleep disorders, stiffness, and mood disturbances. It significantly impacts patients’ quality of life (QoL) and poses a substantial challenge due to the lack of a definitive cure. This study aimed to report real-world data on the long-term use (18 months) of a millimeter (MMW)-based neuromodulation device and tracking application, and its effects on various health dimensions in a self-declared FM population.
Methods: This retrospective study was based on data including daily MMW wristband use and health parameters assessed at baseline (D0) and tracked weekly (pain, stiffness and fatigue) or quarterly (QoL, quality of sleep and impression of change). The primary inclusion criteria were a self-reported diagnosis of FM and consistent device usage for a minimum of 18 months.
Results: The inclusion criteria were met by 185 users. There was a reduction in the Fibromyalgia Impact Questionnaire (FIQ) scores, with an average reduction of 27% after the first three months (M3), indicating improved QoL, and stabilization thereafter. Similar improvements were observed in sleep quality, stiffness and fatigue. In contrast, pain intensity showed a continuous decline throughout the 18-month period.
Conclusion: The significant improvements in QoL, pain intensity, and sleep quality, maintained over time, underline the MMW device’s ability to provide sustained relief and enhance daily lives of people with FM.
Keywords: fibromyalgia, millimeter-waves, neuromodulation, quality of life, pain
Introduction
Fibromyalgia (FM) is a widespread pain condition, associated with other symptoms such as fatigue, sleep disorders, stiffness, mood disturbances, cognitive dysfunction, headaches, paresthesia, irritable bowel syndrome.1,2 FM arises from altered nociception without clear evidence of tissue or somatosensory damage.3 Based on the modified American College Rheumatology (ACR) 2016 criteria, prevalence has been estimated to be 3.4%.4
Because there is currently no cure for FM,5 the European Alliance of Associations for Rheumatology (EULAR) advises to focus on symptom mitigation and quality of life (QoL) improvement,6 and recommends non-pharmacological interventions as first line treatments.
Non-pharmacological interventions are advised as the first line of treatments and combining these therapies appears to be the most effective strategy for symptom management.7 For example, physical activity,6 Cognitive Behavioral Therapy,6 spa therapy,8,9 acupuncture,10 and meditative movement therapies such as Tai Chi, Qigong, and Yoga11 are recommended by the EULAR. Their benefits are thought to rely, at least in part, on the release of endogenous opioids.12–14 Millimeter waves (MMW) are electromagnetic radiation with frequencies ranging from 30 to 300 GHz, which corresponds to Extremely High Frequency (EHF). Exposure of the peripheral nervous system to MMW has also been shown to result in the central release of endorphins and other neurotransmitters,15 leading to hypoalgesic effects16 and modulation of the parasympathetic activities.17 In addition to benefits in pain reduction observed in post-surgical,18 neuropathic,19 and joint20 pain, MMW could be used to improve dimensions such as sleep and stress regulation.21
The field of digital health and wellness is rapidly expanding, fueled by ongoing technological advancements. Digital approaches can provide knowledge and information to patients at any time and any place and thereby help bridge the gap in program availability and practitioner follow-up for patients.22 In addition, digital solutions can help patients track their use of a device, and monitor the evolution of their symptoms to appreciate the changes through time.23 A Cochrane review described the effects of digital interventions as “largely positive” in enhancing chronic patients’ knowledge, sense of social support, and clinical outcomes, compared to those not using such methods.24 In particular, technology-assisted interventions have proven effective in improving self-management of chronic pain in adults.25
On these grounds, a subscription package including a MMW emitting device and a smartphone application was put on the market in an offer intended to improve the QoL of people suffering from bodily discomforts (pain, stiffness, fatigue) and sleep difficulties. These symptoms being frequently reported in FM, a great number of users happened to be FM patients seeking relief for their various symptoms. Prospects could subscribe online to this offer and pay a monthly fee giving access to the use of a wristband and a smartphone application allowing users both to track their wristband use and to record the evolution of their symptoms. Since the launch of the offer, numerous FM users kept using the MMW device for more than 18 months. The longitudinal research on FM patients’ outcomes and/or prolonged use of a given therapy being rather limited.26 The purpose of this retrospective study is to document the improvement in QoL and of FM symptoms (pain, stiffness, fatigue, quality of sleep) in MMW-based neuromodulation users, and to analyze their long-term (18 months) evolution through data collected in the course of their program.
Methods
Data Source and Study Population
The source for this retrospective study was a database belonging to the MMW wristband manufacturer (Remedee Well, Remedee Labs, Montbonnot-Saint-Martin, FRANCE) and collecting users’ device logs and self-reported clinical parameters. Data are uploaded to the database through the smartphone application “Rewell” (available on AppleStore and Playstore only in France). Wristband data require synchronization from the device to the application and clinical parameters require users to voluntarily fill in questionnaires. The analyses were run on an anonymized copy of the data collected between the 1st of October 2021 and the 20th of March 2024 and extracted on the 23th of April 2024. This corresponds to the data of users who subscribed between the 1st of October 2021 and the 20th of September 2022.
To be included in this study, users had to (1) be adults aged ≥18 years old, (2) self-declared as FM patient, (3) be subscribed to the offer for at least 18-months, (4) still be subscribed to the offer at the time of data extraction (to inform users and collect their consent) and (5) were given the opportunity to answer the quarterly questionnaires throughout the 18 months (if users took part in an additional program, they followed a different assessment regimen). At the offer subscription and in the documentation provided in the app, it is mentioned to the users to not stop actual medication without the advice of their doctor.
The present study complies with the Declaration of Helsinki and with French law on studies not involving the human person. It is part of a simplified procedure with 1) compliance with the “Reference Methodology for the processing of personal data in the context of research not involving the human person, studies and evaluations in the field of health (MR-004)” and 2) registration on the Health Data Hub under reference 17121115 (https://www.health-data-hub.fr/projets). The approval of the Scientific and Ethical Committee for Health Research, Studies and Assessments (In French: Comité Ethique et Scientifique pour les Recherches, les Etudes et les Evaluations dans le domaine de la Santé (CESREES)) is not required for this simplified procedure. In compliance with MR004, prior to data extraction, users were individually sent a letter informing them about the study, with details of how they could object to the use of their data if necessary. After this information letter was sent, they were given a period of one month in which to express their opposition if necessary.
Description of the Device and Device Functioning
The MMW emitting wristband contains two microelectronic components that can generate and amplify 61.2 GHz radiations. Its technology has been tested for innocuity in a clinical trial.17 It can be activated for sessions that last 30 minutes and during which radiations are transmitted through the antennas towards the inner part of the patient’s wrist. The waves penetrate the superficial layer of the skin and stimulate its nerve endings. The wave emission automatically stops at the end of a session.
Standard recommendation to users is to perform 3 sessions per day, every day, including one in the hour before bedtime to facilitate sleep onset and increase sleep quality. Additional sessions, up to a total of 6 sessions/per day, may be added if desired. Sessions are recorded in an internal memory and their logs can be synchronized with the smartphone application.
Description of the Application
At subscription, users were asked the main reason(s) for which they wanted to use MMW-based neuromodulation and if they had any identified pathologies that could deteriorate the evolution of their QoL. Through a smartphone application, users had the possibility to track both the use of their device and the evolution of their discomforts. To track the evolution of their discomforts, users had the possibility to fill in questionnaires measuring their QoL, quality of sleep and intensity of various common bodily discomforts (pain intensity and diffusion, stiffness, fatigue) just after the app onboarding and then periodically (ie weekly and quarterly). After completion, their received a report summarizing their answers. The smartphone application also included educative information about the device’s principle of action and training to use the device correctly. Users could ask for assistance in case of lack of understanding or technical issues.
Outcome Measures
Primary Outcomes: QoL Evolution
When users declared having FM, their QoL was measured with a French version of the Fibromyalgia Impact Questionnaire.27 It assesses the impact of FM on the current overall health status. Its total score ranges from 0 to 100, with higher scores indicating greater impact. Bennett et al28 identified scores <39 as representing a mild impact; ≥ 39 to < 59 a moderate impact, and ≥ 59 to 100 a severe impact of FM on QoL. Moreover, a reduction of the FIQ total score ≥14% from baseline measure (D0) is considered as the minimal clinically important difference (MCID).28 Users could fill in a FIQ at day 0 of their program (D0) and then every 3 months (M3, M6, M9, M12, M15 and M18).
Sleep Quality
Sleep quality was assessed with a custom-made questionnaire including perceived sleep quality, sleep onset, sleep duration, sleep efficiency, sleep disturbances, sleep medicine, and difficulties to stay awake during daytime. Scores ranged from 0 to 21 with higher scores indicating worse sleep quality. Users could fill in this questionnaire at D0 and then every 3 months (M3, M6, M9, M12, M15 and M18).
Impression of Change
The impression of change was assessed with the Patient Global Impression of Change (PGIC29). It involves 7 categories to qualify one’s perception of change since initiation of a treatment (1-very much worse, 2-much worse, 3-little worse, 4-unchanged, 5-little improved, 6-much improved, 7-very much improved). Users were offered to fill in this questionnaire every 3 months, from 3 months after initiation of use (M3, M6, M9, M12, M15 and M18).
Pain
At D0 and every week from the 4th week of device use, users could report their pain intensity on a Visual Analogical Scale (VAS, 0: no pain, 100: maximal pain) for 19 body parts (right and left jaws, neck, right and left shoulders, right and left arms, right and left forearms/hands, right and left hips/buttocks, right and left tights, right and left shin/foot, high back, low back, chest, abdomen). The Pain intensity value was average across the body parts with non-null values (ie painful body parts) and pain intensity improvement relative to baseline was computed for each user. Dworkin et al30 ‘s consensus defines improvements of 10–20% decrease as minimally important, ≥30% decrease as moderately important and ≥50% as substantial. A percentage of Pain diffusion was also computed, such that: pain diffusion = (number of the body parts with a non-null value/19)*100.
Stiffness and Fatigue
At D0 and every week from the 4th week of device use, users could report their level of stiffness and fatigue on two VAS (0: no stiffness or fatigue, 100: maximal stiffness or fatigue).
Adherence
Sessions performed by users could be synchronized from their device to their smartphone application. User were described as “adherent” if they performed ≥2 sessions per day, for 80% of a given period (ex: per trimester).
Seasonal Effect
It is commonly reported by patients that symptoms are worse during winter as opposed to summer, but results from the literature are rather incongruent on the matter (see, for example Abeler et al31). Here, taking advantage of our long-term data recording and in order to feed the literature on the topic, we investigated the so-called seasonal effect by testing the difference between FIQ total scores at D0, depending on the season of reporting.
Statistical Analyses
Demographics at D0, evolution in QoL, quality of sleep, bodily discomforts (pain, fatigue, stiffness) and device usage were described using means and standard deviations, medians and quartiles, proportions (effectives and percentages) when appropriate. A one-way ANOVA was used to test for seasonality effect on FIQ total scores at D0 (summer vs fall vs winter vs spring).
Results
Amongst the 1125 FM users aged ≥18 years old (criteria 1–2) who started using the MMW device (initiation of subscription) in the study period, 388 (34.5%) were still subscribed 18 months after initialization (criterion 3). Amongst those, users who unsubscribed after 18 months of subscription but before data extraction (lack of consent, criterion 4) or chose to follow a digital educational program in addition to using their MMW device and followed a different assessment regimen (criterion 5) were excluded from the sample. Finally, the study was composed of 185 users.
Table 1 displays the baseline demographics of the cohort of users. The population was mostly constituted of women (94.6%), of a mean age of 52.1 (SD= 12.1) years old. The duration of pathology ranged from 0 to 64 years, with median duration of 14 years. Most users did not declare having another pathology than FM. When they did, migraine and osteoarthritis were the most common comorbidities reported.
 |
Table 1 Baseline Characteristics |
Primary Outcomes
The primary outcome of our study was the quarterly improvements in QoL during the 18 months of use of the MMW device. The completion rate of the quarterly FIQ questionnaires decreased throughout time, such that D0=100% (185/185), M3=93% (172/185), M6=83.8% (155/185), M9=74.1% (137/185), M12=74.6% (138/185), M15=72.4% (134/185) and M18=64.3% (119/185). We analyzed the evolution of the mean FIQ total scores along the time (M3, M6, M9, M12, M15, M18). Amongst the 185 users in our cohort, 9 users completed the FIQ only at D0, and were therefore removed from the analyses regarding QoL. Figure 1A represents the evolution of the mean FIQ total scores from D0 to M18. While the mean FIQ total score at D0 was 63.2 (SD=14.6), it reduced by 27% after 3 months (M3) and then stayed stable along the time, up to 18 months. Figure 1B represents the evolution of the distributions of users into FIQ severity categories “mild” “moderate”, and “severe” from D0 to M18. At D0, 62.5% of the users were in the “severe” category, while only 5.7% were in the mild category. After 3 months, a minority of users (22.1%) remained in the severe category, while the rest is shared out equivalently in the moderate and mild categories. Figure 1C displays the proportion of users reaching the MCID compared to D0 for each of the trimesters up to M18. It shows that in between M3 and M18, a minimum of 65.2% (M6) to a maximum of 73.7% (M9) reached the MCID (ie a reduction of the FIQ total score from D0 ≥14%).
 |
Figure 1 FIQ total score evolution with time. (A) Mean FIQ total score. The grey area represents the standard deviation from the mean. (B) Distribution of users into FIQ severity categories “mild”: score <39, “moderate”: score ≥39 and <59 and “severe”: score ≥59.28 (C) Proportions of users reaching the MCID (ie FIQ reduction from D0 ≥14%28). |
Secondary Outcomes
Quality of Sleep
Completion rates of the sleep questionnaire were similar to those of the FIQ: D0=100% (185/185), M3=91.4% (169/185), M6=83.8% (155/185), M9=74.1% (137/185), M12=73.5% (136/185), M15=72.4% (134/185) and M18=64.3% (119/185). Ten users filled in the D0 questionnaire only and therefore were removed from the analyses. Figure 2 displays the mean sleep score evolution across the 175 remaining users. In a way analogous to the QoL, the quality of sleep reduced by 21% from D0 (m=12.15, SD=3.89) to M3 (m=9.64, SD=3.92) and then remained stable up to 18 months.
 |
Figure 2 Quality of sleep evolution with time. The grey area represents the standard deviation from the mean. |
Impression of Change
Impression of change was measured every quarter from M3. Completion rates were M3=98.4% (182/185), M6=89.2% (165/185), M9=78.9% (146/185), M12=80% (148/185), M15=77.8% (144/185) and M18=70.3% (130/185). Figure 3 displays the evolution of the quarterly distributions across the 7 categories of the PGIC.29 Proportions of much and very much improved progressed such that: M3: 32.7%, M6: 35.7%, M9: 43.7%, M12: 42.3%, M15: 40.6%, M18: 37%.
 |
Figure 3 Impression of change evolution with time. |
Bodily Discomforts (Pain Intensity, Pain Diffusion, Fatigue, Stiffness)
Every week, from week 4, users could fill in a questionnaire assessing the intensity of their pain, fatigue and stiffness. Figure 4 displays the numbers of questionnaires that were filled out depending on users’ program week.
 |
Figure 4 Number of users answering the weekly questionnaire. |
Figure 5A represents the evolution of mean pain intensity as reported by users who filled out the weekly questionnaire, for every week between week 4 and week 72. At D0 the mean pain intensity across users was 56.7 (SD=15.6) and declined steadily up to week 72 to reach a mean of 35.4 (SD=16.6). For each user, a weekly improvement relative to their baseline pain intensity was also computed. Figure 5B represents the percentage of users with relative pain intensity improvement ≥20% (minimally important), ≥30% (moderately important) and ≥50% (substantial). There were 47.6%, 31% and 7.1% of users at week 4 and 68.8%, 58.4% and 29.9% of users at week 72, with a pain intensity improvement ≥20%, ≥30% and ≥50%, respectively.
At D0 the mean pain diffusion across users was 75.1% (SD=20.6), in other words, users suffered from 14 body parts over 19 assessed on average. The mean pain diffusion score decreased to 67.4% (SD =22.2) at week 4 and 57.7% (SD =28.5) at week 72. For each user, a weekly improvement relative to their baseline pain diffusion was computed. Figure 6. The grey area represents the 1st and 3rd quartiles represents the evolution of median relative pain diffusion improvement as reported by users who filled out the weekly questionnaire, for every week between week 4 and week 72.
 |
Figure 6 Evolution of the median relative pain diffusion improvement. The grey area represents the 1st and 3rd quartiles. |
Stiffness was measured with a VAS-100. At D0 the mean stiffness level across users was 71.2 (SD=22.7). Figure 7 represents the evolution of median relative stiffness improvement as reported by users who filled out the weekly questionnaire, for every week between week 4 and week 72.
 |
Figure 7 Evolution of the median relative stiffness improvement. The grey area represents the 1st and 3rd quartiles. |
Fatigue was measured with a VAS-100. At D0 the mean stiffness level across users was 80.3 (SD=18.6). Figure 8 represents the evolution of median relative fatigue improvement as reported by users who filled out the weekly questionnaire, for every week between week 4 and week 72.
 |
Figure 8 Evolution of the median relative fatigue improvement. The grey area represents the 1st and 3rd quartiles. |
Adherence
Data collection on device use was dependent on wristbands synchronization with their smartphone application. Table 2. displays the number of available data set for each trimester of the 18-month study period and the percentages of adherent users per trimester. A set includes all sessions recorded and synchronized by a user during a trimester. A user was categorized as “adherent” for a given trimester if they had performed at least 2 sessions/day for at least 80% of the trimester duration. Figure 9 displays the mean number of sessions/day performed across users, every day of the 18 months of the study period.
 |
Figure 9 MMW device use along the time. Mean sessions per day. The grey area represents the deviation from the mean. |
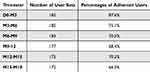 |
Table 2 MMW Use |
Seasonal Effect
The effect of seasons on FIQ recorded at D0 was not statistically significant. Figure 10 displays the boxplots of the FIQ-D0 total scores depending on seasons.
 |
Figure 10 Mean FIQ-D0 total scores depending on seasons. |
Discussion
The goal of this study was twofold. The first was to report, for the first time, real-life data on the use of a MMW-based neuromodulation device and its impact on several health dimensions in a self-declared FM population. The second was to describe the long-term evolution in QoL of a population of FM users, by reporting 18 months of data tracking.
Over a 12-month inclusion period, 1125 users of the MMW-based neuromodulation device presented with FM and their persistence rate 18 months after initiation was 34.5%. Here, we analyzed the data of 185 users meeting our inclusion criteria Their device use was recorded continuously during the 18 months and several health dimensions were tracked weekly or quarterly. Data analysis showed that three months after the starting use, participants’ QoL and quality of sleep were improved by 27% and 21% respectively, compared to D0 and these improvements remained stable up to M18. Based on Bennett et al’s (2009) FIQ severity categorization, the majority of users (62.5%) were in the severe category at D0 but most moved to the moderate (35.5%-43%) or mild (34.9%-43.8%) categories between M3 and M18. Compared to their FIQ total score at D0, between 65.2% and 73.7% of users improved their score by ≥14%, MCID defined by Bennet et al28 between M3 and M18. These benefits were also perceived by users who, for at least a third between M3 and M18, assessed their QoL as much or very much improved compared to D0. Looking at weekly data, we found that the median relative improvement in pain intensity compared to baseline was 17.9% at week 4 and that this median relative improvement went up to 37.1% at week 72. On the other hand, if stiffness and fatigue also improved quickly (median relative improvements at week 4 compared to baseline were 29.8% and 24.5% respectively), their evolution remained rather stable over time (median relative improvements at week 72 were 30.4% and 28.2% respectively).
The results presented in the present article corroborate and extend those of a randomized clinical study, showing that use of a MMW device combined with coaching improves the QoL of patients with FM, as compared to standard care.32 In the clinical trial, patients were included and followed for 9 months. The Immediate group used the MMW device from D0 to M6, the Delayed group used the device from M3 to M9. The results showed significant improvement in QoL for the Immediate group compared to the Delayed group at M3, with a mean FIQ reduction of 21.7% and 7.2%, respectively. In addition, the FIQ reduction from D0 to M3 found in the Immediate group was maintained at M6 but FIQ scores tended to rise again between M6 and M9 when patients were not using the device. Here, data from people with 18 months history of use showed that benefits were preserved with a continuous use of the device.
The improvements shown in this study cannot be explained by seasonal effects since users did not all start using the device at the same time of year and the effect of season on FIQ scores at D0 was found not significant. This long-term study offers an opportunity to contribute valuable data to the literature regarding the so-called seasonality effect,33 or, in this particular case, the absence of such an effect.
The mechanism assumed behind the MMW neuromodulation is the central release of neurotransmitters following the peripheral stimulation on nerve endings.15,16 This activates the descending pain inhibitory pathway, deactivates the salience network, and changes functional connectivity, thereby leading to pain relief.7 A study on healthy patients showed that exposure to MMW raises the pain perception threshold,17 which could potentially explain the benefits found in patients with central sensitization syndromes, like FM. Neuromodulation techniques were found to be effective in reducing FM symptoms and are generally appropriate for nociplastic pain syndromes.34 In long-term user profiles described in the present paper, we found that pain intensity reduced steadily over the course of the 18-month investigation, a result difficult to achieve with pharmacological treatments.35,36
Devices such that the wristband used in this study present various advantages for people with nociplastic pain. First, patients can use them autonomously, which gives them a sense of empowerment and control over their pain.37 Second, devices often come with digital tracking tools (here, a smartphone app) that provide feedback on device use and can improve adherence and therefore outcomes.38 The data presented here showed that, on average, users performed 2.8 (SD = 1.8) sessions per day after 18 months, compared to the 3 sessions per day recommended initially. Additionally, 2/3 of the users maintained at least 2 sessions per day for at least 4 out of every 5 days, adherence threshold defined in Maindet et al32 ‘s clinical trial. These results stand out from the common treatment non-adherence reported in chronic pain patients.39 Third, neuromodulation devices are accessible. As opposed to other non-pharmacological treatments that rely on significant resources (for example, spa therapy, acupuncture, cryotherapy, cognitive-behavioral therapies, etc)., neuromodulation devices are a viable option for a broader population, especially those with limited access to healthcare resources. Finally, physical activity remains the most desirable approach to managing chronic pain. It should be encouraged not only for its pain modulation benefits but also for its broader health preventive and curative actions.40,41 However, it can be challenging to implement for patients with severe chronic pain,42 and the synergy between a neuromodulation device and physical activity could be promising for overall outcomes.
This study presents the typical challenges and limits of real-world investigations. First, it was an open label, single-arm retrospective study, meaning that users chose to use the device and were not randomized into using the device (introducing selection bias). Furthermore, unlike in a clinical trial, the FM diagnoses reported in our studies rely on users’ self-declarations rather than those of medical practitioners. In addition, data were those of users who kept using the product and services for as long as 18 months and do not include users who dropped out before (introducing ascertainment bias). Second, the quality of sleep and pain diffusion were assessed through custom questionnaires. Consequently, direct comparisons with other studies should be made with caution. Third, medication intake or any other interventions that could have influenced the evolution of the users’ health parameters were not analyzed, because they were not recorded. Therefore, the reader must consider that the data presented may not result solely from the use of the MMW device and application solution. Despite those limitations, real world data are valuable to represent treatments usage and benefits in patients’ daily life and in the long-term, and complement data from randomized, controlled clinical trials.
Conclusion
The significant improvements in QoL, pain intensity, and sleep quality, maintained over time, underscore the MMW device’s ability to provide sustained relief and enhance daily lives of people with FM. As digital health technologies continue to evolve, the integration of such innovative solutions into chronic pain management protocols presents a valuable opportunity for improving patient care. Future studies should aim to further validate these findings in larger and more diverse populations. The use of companion apps helping to track both device use and health parameters should allow the generation of large and valuable real-world data.
Disclosure
Laure Minier, Paolo Zanini, Emilie Chipon, David Crouzier are affiliated with Remedee Labs. Dr Erwan Treillet reports grants from Remedee, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Clauw DJ. Fibromyalgia and related conditions. Mayo Clin Proc. 2015;90(5):680–692. doi:10.1016/j.mayocp.2015.03.014
2. Wolfe F, Häuser W. Fibromyalgia diagnosis and diagnostic criteria. Ann Med. 2011;43(7):495–502. doi:10.3109/07853890.2011.595734
3. Bidari A, Ghavidel-Parsa B. Nociplastic pain concept, a mechanistic basis for pragmatic approach to fibromyalgia. Clin Rheumatol. 2022;41(10):2939–2947. doi:10.1007/s10067-022-06229-5
4. Häuser W, Brähler E, Ablin J, Wolfe F. Modified 2016 American college of rheumatology fibromyalgia criteria, the analgesic, anesthetic, and addiction clinical trial translations innovations opportunities and networks–American pain society pain taxonomy, and the prevalence of fibromyalgia. Arthritis Care & Res. 2021;73(5):617–625. doi:10.1002/acr.24202
5. Al-Athari Y, Mahawish M. Fibromyalgia: a review. MEWFM. 2024;22(3). doi:10.5742/MEWFM.2024.95257627
6. Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318–328. doi:10.1136/annrheumdis-2016-209724
7. Martinez JE, Guimarães I. Fibromyalgia – are there any new approaches? Best Pract Res. 2024;38(1):101933. doi:10.1016/j.berh.2024.101933
8. Langhorst J, Musial F, Klose P, Häuser W. Efficacy of hydrotherapy in fibromyalgia syndrome--a meta-analysis of randomized controlled clinical trials. Rheumatology (Oxford). 2009;48(9):1155–1159. doi:10.1093/rheumatology/kep182
9. Maindet C, Maire A, Vermorel C, et al. Spa therapy for the treatment of fibromyalgia: an open, randomized multicenter trial. J Pain. 2021;22(8):940–951. doi:10.1016/j.jpain.2021.02.010
10. Deare JC, Zheng Z, Xue CCL, et al. Acupuncture for treating fibromyalgia. Cochrane Database Syst Rev. 2013;2013(5):CD007070. doi:10.1002/14651858.CD007070.pub2
11. Langhorst J, Klose P, Dobos GJ, Bernardy K, Häuser W. Efficacy and safety of meditative movement therapies in fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Rheumatol Int. 2013;33(1):193–207. doi:10.1007/s00296-012-2360-1
12. Goldfarb AH, Jamurtas AZ. β-endorphin response to exercise. Sports Med. 1997;24(1):8–16. doi:10.2165/00007256-199724010-00002
13. Vescovi PP, Coiro V. Hyperthermia and endorphins. Biomed. Pharmacother. 1993;47(8):301–304. doi:10.1016/0753-3322(93)90078-Y
14. Kaada B, Torsteinbø O. Increase of plasma beta-endorphins in connective tissue massage. Gen Pharmacol. 1989;20(4):487–489. doi:10.1016/0306-3623(89)90200-0
15. Radzievsky AA, Rojavin MA, Cowan A, Alekseev SI, Ziskin MC, Ziskin MC. Peripheral neural system involvement in hypoalgesic effect of electromagnetic millimeter waves. Life Sci. 2001;68(10):1143–1151. doi:10.1016/S0024-3205(00)01016-X
16. Radzievsky AA, Gordiienko OV, Alekseev S, Szabo I, Cowan A, Ziskin MC. Electromagnetic millimeter wave induced hypoalgesia: frequency dependence and involvement of endogenous opioids. Bioelectromagnetics. 2008;29(4):284–295. doi:10.1002/bem.20389
17. Minier L, Debouzy JC, Foerster M, Pierre V, Maindet C, Crouzier D. Hypoalgesia and parasympathetic effects of millimeter waves on experimentally induced pain in healthy volunteers. Electromagnetic Biol Med. 2023;42(1):3–11. doi:10.1080/15368378.2022.2162919
18. Korpan NN, Saradeth T. Clinical effects of continuous microwave for postoperative septic wound treatment: a double-blind controlled trial. Am J Surg. 1995;170(3):271–276. doi:10.1016/S0002-9610(05)80013-3
19. Moazezi Z, Hojjati SMM, Ayrapetyan S. Low intensity millimeter wave as a potential tool in treatment of diabetic sensorymotor polyneuropathy. Int Dent Med Disord. 2008;1:6.
20. Bakaliuk TG, Zoria LV, Pogorila MA. [Microwave resonance therapy in primary osteoarthrosis: the pathogenetic validation of its clinical use. Patol Fiziol Eksp Ter. 1998;4:22–25.
21. Pilozzi A, Carro C, Huang X. Roles of β-endorphin in stress, behavior, neuroinflammation, and brain energy metabolism. IJMS. 2020;22(1):338. doi:10.3390/ijms22010338
22. Donisi V, De Lucia A, Pasini I, et al. e-health interventions targeting pain-related psychological variables in fibromyalgia: a systematic review. Healthcare. 2023;11(13):1845. doi:10.3390/healthcare11131845
23. Collinge W, Soltysik R, Yarnold P. Fibromyalgia impact reduction using online personal health informatics: longitudinal observational study. J Med Internet Res. 2020;22(4):e15819. doi:10.2196/15819
24. Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2005;4:CD004274. doi:10.1002/14651858.CD004274.pub4
25. Williams DA. Web-based behavioral interventions for the management of chronic pain. Curr Rheumatol Rep. 2011;13(6):543–549. doi:10.1007/s11926-011-0212-8
26. Schaefer CP, Adams EH, Udall M, et al. Fibromyalgia outcomes over time: results from a prospective observational study in the United States. Open Rheumatol J. 2016;10(1):109–121. doi:10.2174/1874312901610010109
27. Perrot S, Dumont D, Guillemin F, Pouchot J, Coste J. Research FG for Q of L. Quality of life in women with fibromyalgia syndrome: validation of the QIF, the French version of the fibromyalgia impact questionnaire. J Rheumatol. 2003;30(5):1054–1059.
28. Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB. Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol. 2009;36(6):1304–1311. doi:10.3899/jrheum.081090
29. Hurst H, Bolton J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manipulative Physiol Ther. 2004;27(1):26–35. doi:10.1016/j.jmpt.2003.11.003
30. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. doi:10.1016/j.jpain.2007.09.005
31. Abeler K, Sand T, Friborg O, Bergvik S. Seasonality in pain, sleep and mental distress in patients with chronic musculoskeletal pain at latitude 69° N. Chronobiol. Int. 2020;37(11):1650–1661. doi:10.1080/07420528.2020.1764011
32. Maindet C, Dumolard A, Veloso M, et al. Therapy combining millimeter wave-based neuromodulation with coaching for the improvement in quality of life of patients with fibromyalgia: a prospective, multicenter, randomized, controlled trial [abstract]. Arthritis Rheumatol. 2023;75(suppl 9).
33. Owen JEL. Comment on D.G.Hawley and F. Wolfe. PAIN. 1995;62(1):125. doi:10.1016/0304-3959(95)00078-7
34. Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397(10289):2098–2110. doi:10.1016/S0140-6736(21)00392-5
35. Häuser W, Walitt B, Fitzcharles MA, Sommer C. Review of pharmacological therapies in fibromyalgia syndrome. Arthritis Res Therapy. 2014;16(1):201. doi:10.1186/ar4441
36. Giorgi V, Sarzi-Puttini P, Pellegrino G, et al. Pharmacological treatment of fibromyalgia syndrome: a practice-based review. Curr Pain Headache Rep. 2024;28(12):1349–1363. doi:10.1007/s11916-024-01277-9
37. Grass JA. Patient-Controlled Analgesia. Anesthesia Analg. 2005;101(5S):44–61. doi:10.1213/01.ANE.0000177102.11682.20
38. Seewoodharry MD, Maconachie GDE, Gillies CL, Gottlob I, McLean RJ. The effects of feedback on adherence to treatment: a systematic review and meta-analysis of RCTs. Am J Preventive Med. 2017;53(2):232–240. doi:10.1016/j.amepre.2017.03.005
39. Timmerman L, Stronks DL, Groeneweg JG, Huygen FJ. Prevalence and determinants of medication non‐adherence in chronic pain patients: a systematic review. Acta Anaesthesiol Scand. 2016;60(4):416–431. doi:10.1111/aas.12697
40. Ambrose KR, Golightly YM. Physical exercise as non-pharmacological treatment of chronic pain: why and when. Best Pract Res Clin Rheumatol. 2015;29(1):120–130. doi:10.1016/j.berh.2015.04.022
41. Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809. doi:10.1503/cmaj.051351
42. Vancampfort D, Brunner E, McGrath RL, Hemmings L, Van Damme T. Correlates of sedentary behavior in people with fibromyalgia: a systematic review. Int J Rheumatic Dis. 2023;26(5):841–849. doi:10.1111/1756-185X.14678
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


