Back to Journals » Open Access Journal of Sports Medicine » Volume 16
Exploration of Inertial Sensor-Derived Kinematic Predictors for Dynamic Balance Assessment in the Active Adult
Authors Phuaklikhit C , Shah VR, Muraki S, Dixon PC, Loh PY
Received 18 February 2025
Accepted for publication 27 June 2025
Published 11 July 2025 Volume 2025:16 Pages 67—78
DOI https://doi.org/10.2147/OAJSM.S523553
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Prof. Dr. Andreas Imhoff
Chairat Phuaklikhit,1,2 Vaibhav R Shah,3,4 Satoshi Muraki,5 Philippe C Dixon,3,4,6 Ping Yeap Loh5
1Graduate School of Design, Faculty of Design, Kyushu University, Fukuoka, Japan; 2Faculty of Physical Therapy and Sports Medicine, Rangsit University, Pathumthani, Thailand; 3Institute of Biomedical Engineering, Faculty of Medicine, University of Montreal, Quebec, Canada; 4Centre de Recherche Azrieli du CHU Sainte-Justine, Quebec, Canada; 5Department of Health Life Design and Science, Faculty of Design, Kyushu University, Fukuoka, Japan; 6Department of Kinesiology and Physical Activity, McGill University, Quebec, Canada
Correspondence: Ping Yeap Loh, Department of Human Life Design and Science, Faculty of Design, Kyushu University, 4-9-1 Shiobaru, Minami-ku, Fukuoka, 815-8540, Japan, Email [email protected]
Purpose: The modified Star Excursion Balance Test (mSEBT) is a clinical tool for dynamic balance assessment. While researchers have examined individual joint kinematic predictors of dynamic balance performance, limited data exist on body and joint sway during the test execution. Further investigation of kinematic predictors’ influence on dynamic balance is needed to improve assessment methodologies. This study aimed to examine the relationship between the center of mass and lower limb kinematics as predictors of mSEBT performance.
Patients and Methods: Twenty-seven participants with no history of lower limb joint instability were recruited for this study. The inertial sensors were positioned on the non-dominant leg: trunk, thigh, shank, and foot. The participants completed the mSEBT barefoot following standardized practice trials with three test trials per direction. The reach distance and lower limb kinematic data were recorded. Spearman rank’s correlation and stepwise multiple regression analyses identified key predictors of dynamic balance performance.
Results: Ankle dorsiflexion was a strong predictor of normalized reach distance in the anterior direction (r² = 0.34, p < 0.001). Body center of mass displacement was the strongest predictor of posteromedial and posterolateral reach (r² = 0.55, p < 0.001; r2 = 0.57, p = < 0.001, respectively). The combined influence of the body center of mass and hip flexion accounted for 65% of the variance in the posterior reach assessments.
Conclusion: This study highlights the key biomechanical factors that influence dynamic balance, focusing on the interaction between joint mobility and segmental control. Ankle dorsiflexion is critical for anterior balance, whereas hip flexion and body center of mass displacement are essential for posterior balance.
Keywords: postural balance, accelerometry, lower extremity, biomechanical phenomena
Introduction
Dynamic balance is essential for physical performance, injury prevention, and rehabilitation, particularly among physically active individuals. Maintaining balance during complex movements requires intricate coordination of neuromuscular and biomechanical systems.1,2 The modified Star Excursion Balance Test (mSEBT) or Y-Balance Test, an adaptation of the Star Excursion Balance Test (SEBT), is widely used to assess dynamic balance and predict lower extremity injury risk.3 The mSEBT reach distances reflect dynamic postural control, including lower extremity balance, flexibility, and strength. This assessment challenges participants to maintain a stable base of support while maximizing their reach with the opposite limb.4 The anterior and posterior reach directions in the mSEBT impose distinct biomechanical and neuromuscular demands. Anterior reach tasks emphasize quadriceps and hip abductor control, whereas posterior reaches rely on hip extensor activation, trunk stabilization, and anticipatory postural adjustments (APAs) to maintain balance during movements. These directional differences give rise to specific postural control strategies, which are important to consider when interpreting reach performance.5 SEBT performance can reveal asymmetries and deficits associated with lower extremity injuries, identifying subtle neuromuscular control and dynamic stability differences following injury.6,7 However, mSEBT scores fluctuate based on factors such as age, athletic proficiency, and population characteristics.8,9 Additionally, this clinical test relies on visual and observational assessments, limiting the ability to identify the underlying kinematic factors influencing balance performance.
Technological advancements in motion analysis, particularly portable Inertial Measurement Units (IMUs), have improved the ability to quantify dynamic movements with high precision. IMUs, integrating gyroscopes, accelerometers, and magnetometers, provide accurate orientation measurements and real-time kinematic data during dynamic tasks.10 They offer advantages such as portability, ease of use, and data collection in naturalistic environments. Despite their increasing application in biomechanical research, few studies have incorporated IMUs into dynamic balance assessments.11–13 This integration could enhance the reliability and validity of balance testing, offering precise insights into the biomechanical factors influencing performance and injury risk.
Balance testing protocols using IMUs allow for more accurate quantification of joint range of motion (ROM) and center of mass (COM) displacement than visual assessment methods.14 Previous 3D motion analysis studies have highlighted the significance of trunk and lower limb kinematics, such as trunk, hip, and ankle ROM, in influencing mSEBT scores.5,15 Similarly, IMU-measured COM displacement is a critical indicator of postural control and balance stability, aiding in assessing balance impairments.13,14 However, prior studies have primarily examined individual components, either joint kinematic or COM displacement, which limits the understanding of their combined impacts on dynamic balance performance. Additionally, research on joint kinematic variables in dynamic balance evaluation remains scarce.16
Given the biomechanical complexity of the mSEBT, a comprehensive analysis that integrates both lower limb joint ROM and COM displacement may offer deeper insights into postural control mechanisms. A more integrated approach could enhance the precision of functional assessments in populations with balance impairments. Therefore, the objective of this study was to examine the combined effects of lower limb joint and COM kinematic factors during the mSEBT, in order to determine their individual and collective contributions to dynamic balance performance. We hypothesized that COM control would positively predict reach distance across all directions. Additionally, we posited that hip ROM would be associated with improved performance in the posteromedial and posterolateral directions, whereas greater ankle ROM would enhance reach in the anterior direction.
Methodology
Participants
We recruited 27 physically active adults (16 males, 11 females; age: 26 ± 5 years; height: 1.67 ± 0.09 m; weight: 63.87 ± 14.40 kg) from Kyushu University, Fukuoka, Japan. The sample size was determined using a statistical power analysis conducted with G*Power (version 3.1.9.7), applying a linear multiple regression fixed-effects model. The effect size (f2) was set at 1, based on the coefficient of determination (R2) between ankle dorsiflexion and the anterior reach score,15 with seven potential predictors included. A sample of 27 participants was required to achieve a statistical power of 0.90 at a significance level of p < 0.05. The inclusion criteria were as follows: (1) age between 18 and 45 years, (2) right leg dominance, assessed using the Waterloo Footedness Questionnaire-Revised, and (3) possession of a healthy ankle, verified with the Cumberland Ankle Stability Tool (CAIT) questionnaire (score >24). Participants were excluded if they met any of the following criteria: (1) acute leg or back injury within 5 days before the experiment, (2) moderate to severe muscle fatigue before testing, or (3) any health abnormalities (eg, fever, dizziness, diarrhea) during the study period. This study was approved by the Research Ethics Review Committee of the Faculty of Design, Kyushu University (approval number: 593/2023).
Experiment Setup
Demographic data and screening forms were collected before testing. After attaching IMU sensors to the stance leg, participants stood on a test platform with their eyes open and hands on hips to perform the mSEBT barefoot. Each participant practiced the leg reach four times for familiarization. The final test consisted of three consecutive trials in each direction,17 with a one-minute rest between trials. Upon completion of the motions, the reach distance in each direction was measured using a distance measuring tape.
Experiment Protocol and Data Collection
Inertial Measurement Units (IMUs) Sensor Assessment
Four IMU sensors (Xsens DOT, Xsens Technologies B.V., Netherlands) were used to analyze the joint kinematics at a sampling frequency of 60 Hz. To minimize potential strap movement, the skin was first cleaned with alcohol before sensor placement. A firm Velcro strap was then applied directly to the skin, and each sensor, secured within a 3D-printed holder, was mounted on the strap to ensure stability and prevent sensor shift. Sensors were placed on the spinous process of the L5 vertebrae (trunk), middle half of the thigh (thigh), tibial tuberosity (shank), and middle half of the metatarsal bone (foot) (Figure 1). Kinematic data in three axes were recorded during a movement task and transmitted to an iPad app (Movella DOT™, v.2023.6.0) for data visualization. The raw IMUs data were exported via the Movella DOT™ Data Exporter (v.2023.6.0) and analyzed offline using MATLAB (MathWorks, R2023b, Update 4). This study examined the ROM of the lower extremity in the sagittal plane of the stance leg. Additionally, a single sensor analyzed COM displacement, represented by the root mean square displacement (RMSD) in the anteroposterior and mediolateral directions (X–Y axes). Although COM was estimated using a single sensor positioned at the L5 vertebrae level, representing a simplified method compared to multisegmental modeling, this approach has been shown to yield valid and reliable measurements in dynamic balance assessments and was therefore deemed acceptable for this study.13,18 Test–retest reliability for balance assessment using the IMUs approach was moderate to good, with an intraclass correlation coefficient (ICC) of 0.71 for RMSD and 0.60–0.87 for other time-domain parameters. The assessment demonstrated validity compared to the center of pressure in the gold standard protocol19 and correlated highly with the Berg Balance Scale and Timed Up and Go test in clinical applications.20
Modified Star Excursion Balance Test (mSEBT)
The mSEBT assesses dynamic balance and predicts lower limb injury, particularly ankle instability.21 This test modifies the eight-direction SEBT into three directions, demonstrating high sensitivity and intra-rater reliability, with ICC values of 0.88 (range, 0.84–0.93), 0.88 (range, 0.85–0.94), and 0.90 (range, 0.68–0.94) for the anterior, posterolateral, and posteromedial directions, respectively.6,22 The testing platform consisted of a nylon fabric with an anti-slip pad and three tape lines. The anterior line was positioned 135° from the posterior lines, which were spaced 90° apart. All lines were marked in 1 cm increments.
Participants performed a single-leg stance at the center intersection using their stabilized leg, which was the left side since all participants were right lower limb dominant. Foot placement was standardized by aligning the great toe tip with the intersection’s center (designated as the zero point) for the anterior reach. The posterior reach was standardized by positioning the posterior aspect of the heel at the zero point. Throughout the task, participants were required to keep their hands on their hips to minimize upper body movement. Participants were instructed to reach their other leg as far as possible, touched the line with their big toe, and returned to the initial two-foot standing position.23 Knee and hip flexion of the stance leg were permitted to maximize the reach (Figure 1). A trial was deemed unsuccessful and repeated if participants: 1) could not maintain a single-leg stance, 2) moved the fixed foot from the marked point, 3) failed to keep both hands on the hips, 4) lost balance and failed to return to the two-foot standing position, 5) exhibited noticeable swaying during the test, 6) contacted the ground with any part of the reaching leg before returning to the center, or 7) shifted weight to the reaching leg while touching the ground. The average reach distance was recorded in each direction.
Data Processing
The ROM of the lower extremity on the stance leg side was calculated from raw IMUs data using the methods developed and described by Shah, based on McGrath’s approach.24,25 ROM in the sagittal plane was determined between sensor pairs as follows: 1) hip flexion/extension (F/E) using the trunk and thigh sensors, 2) knee F/E using the thigh and shank sensors, and 3) ankle dorsiflexion/plantarflexion (DF/PF) using the shank and foot sensors. The combination of hip, knee, and ankle ROM was calculated as a composite parameter. Strap-down integration of the linear acceleration signal from a single IMU sensor analyzed body and joint COM displacement. The trunk sensor represented body COM, while the shank sensor quantified knee displacement. The foot sensor identified ankle motion. IMUs data were filtered using a low-pass 4th-order Butterworth filter with a 6 Hz cut-off frequency.24
Normalized reach distance was calculated using individual leg length (from the anterior superior iliac spine to medial malleolus) with the following equation: average reach distance divided by leg length multiplied by 100 (Equation 1),26 as this method accounts for differences in leg length, providing a more equitable measure of dynamic balance across sexes.27
Data Analysis
Statistical analyses were conducted using SPSS (Version 28; IBM Inc., Armonk, NY, USA). Descriptive statistics were computed for normalized reach distance in each direction, ROM of the hip, knee, and ankle, and RMSD of the body, knee, and ankle COM. Data normality was assessed using the Shapiro–Wilk test, which indicated a non-normal distribution. Therefore, Spearman’s rank correlation coefficient was used to examine relationships between normalized reach distance in different directions and trunk/lower extremity kinematics.13,28 Stepwise multiple linear regression was performed to identify the most significant kinematic predictors for each mSEBT reach direction. This model selection approach was used to determine the proportion of variance (R²) in reach performance explained by each predictor variable, thereby identifying the most pertinent contributors. To reduce the risk of overfitting due to small sample size, correlation analysis was first used to narrow the number of predictors for each direction. The regression analysis then incorporated the most correlated kinematic variables within each domain. Furthermore, k-fold cross-validation was used to assess the model’s predictive performance and stability. Additionally, variance inflation factor (VIF) values were evaluated to confirm the absence of multicollinearity, using a threshold of VIF > 5. Statistical significance was set at P < 0.05.
Results
Thirty participants were initially recruited; however, three were excluded—two due to left-leg dominance and one due to a history of ankle sprain. The Cumberland Ankle Instability Tool yielded an average score of 28 ± 2.3.
The hip, knee, and ankle kinematic patterns during the mSEBT revealed direction-specific movement strategies. Figure 2 illustrates the mean ROM in each lower limb joint, with the shaded region representing the standard deviation during the testing cycle (ie, single-leg squat). The data were normalized to 1000 time units, corresponding to a total duration of 16s, with each time unit representing 0.016 s. In the anterior direction, the knee exhibited the most angular displacement, peaking at 550 time units concurrent with the hip. The ankle remained relatively stable, reaching its peak last. In the posteromedial direction, the hip played a more prominent role, initiating movement earlier and peaking at 600 time units. The knee contributed moderately at a similar time, while the ankle exhibited minimal displacement, peaking before the proximal joints. In the posterolateral direction, the hip showed the most angular displacement, initiating movement first and peaking at 590 time units. The knee peaked slightly earlier at 580 time units, with a maximum angle of 40 °. The ankle remained consistent, peaking at 10–15 °, concurrent with the knee.
Normalized reach distance scores were: 70.9 ± 4.2% of leg length in the anterior direction, 82.9 ± 6.1% in the posteromedial direction, and 76.5 ± 8.5% in the posterolateral direction. Table 1 presents the descriptive statistics (mean ± standard deviation) for trunk and lower extremity kinematics. The relationships between normalized reach distances and corresponding kinematic data in each direction are listed in Table 2.
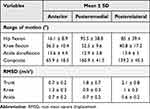 |
Table 1 Kinematic Data of Trunk and Lower Extremity on the Stance Limb During the mSEBT |
 |
Table 2 Correlation Coefficients of Trunk and Lower Extremity Kinematics with Normalized Reach Scores in All mSEBT Directions |
Violin plots of the cross-validated R² values revealed distinct patterns of predictive performance across the three reach directions (anterior, posteromedial, and posterolateral). In the anterior direction, the model incorporating ankle DF ROM exhibited the lowest median R² (~34%). In contrast, for both posteromedial and posterolateral directions, models including body COM displacement showed moderate predictive accuracy (median R² ~56%). Notably, the addition of hip F ROM to COM displacement significantly improved model performance, increasing median R² values to approximately 65% in both posterior directions. The shape and width of the violin plot indicated that models combining COM displacement and hip ROM not only yielded higher median R² values but also demonstrated tighter distributions, suggesting improved consistency and generalizability across folds. In contrast, anterior balance may be more dependent on local joint mobility (Figure 3). The regression equations were formulated as follows: anterior direction; ŷ = 63.485 + 0.556x, where x represents ankle DF ROM. Posteromedial direction; ŷ = 69.235 + 4.066x1 + 0.066x2, and posterolateral direction; ŷ = 60.931 + 4.375x1 + 0.091x2, where x1 is trunk RMSD and x2 representing hip F ROM. No outliers were detected in the regression model (Table 3 and Figure 4).
 |
Table 3 Stepwise Regression Analysis for Kinematic Variables Prediction Performance on the mSEBT |
 |
Figure 4 Scatter plot of the relationship between the best single kinematic predictor and normalized reach distance in (A) anterior, (B) posteromedial (blue), and posterolateral (red) directions. |
Discussion
This study examined the interaction between lower limb joint mobility (hip, knee, and ankle ROM) and COM shifts during the mSEBT, and evaluated their individual and combined effects on balance outcomes. Results indicated that ankle dorsiflexion significantly predicts anterior reach. Additionally, the increased normalized reach distance in the posterior direction was primarily achieved through increased trunk RMSD, greater hip flexion, or a combination of both.
Kinematic Pattern
This study quantified lower-limb kinematic patterns during single-leg reaching tasks, as illustrated in Figure 2, which visually represents joint angular displacement and coordination. In the anterior reach, movement initiation was nearly simultaneous across the hip, knee, and ankle joints, suggesting a balanced coordination strategy. The knee exhibited the largest angular displacement and the earliest peak, highlighting its primary role in forward movement, whereas the hip likely provided additional support for balance. These findings align with previous research indicating that the knee joint is the primary contributor to anterior directional tasks due to its significant role in forward propulsion.29 However, the ankle remained relatively stable, exhibiting minimal angular displacement, likely due to its function as a stabilizer and the inherently limited sagittal plane ROM in a dorsiflexed posture during stance.
In the posterior reach, the hip played a dominant role in maintaining stability and controlling movement, initiating motion earlier than the knee and ankle, underscoring its critical function. The knee showed moderate angular displacement, supporting the reaching motion, while the ankle continued to act as a stabilizer. Compared to the anterior direction, the posterior reach relied more on hip motion, with the knee serving as a secondary contributor. This reflects the increased demand for hip strength and mobility to stabilize and control movement as the reach extends farther from the body’s COM. These findings align with previous research emphasizing the importance of hip control in multidirectional balance tasks.23
Anterior Reaching Control
Ankle DF ROM is crucial for lower limb biomechanics and stability during functional tasks. This study identified significant relationships between ankle DF ROM, knee RMSD, and anterior reach performance. Table 3 summarizes these relationships, emphasizing the predictive role of ankle DF ROM in anterior reach tasks. This finding aligns with previous research indicating that ankle DF ROM correlates with normalized reach distance and serves as the strongest predictor, alongside trunk extension, in anterior reach tasks.15 Ankle DF ROM is linked to increased knee flexion during landing and squatting tasks, influencing knee flexion angles in single-leg squat tasks.30 Additionally, individuals with chronic ankle instability demonstrate reduced anterior normalized reach during dynamic postural control assessments, which is associated with restricted ankle DF ROM.31 The role of DF ROM in forward stability has also been highlighted, showing its association with landing mechanics and postural control. Restricted ankle DF ROM alters landing patterns, leading to increased hip adduction and knee valgus, which may elevate injury risk.32
Knee alignment control is another factor influencing forward-reaching control. Knee sway reflects a participant’s ability to stabilize dynamically while allowing slight knee movements to fine-tune balance.23 Individuals with effective neuromuscular control can sway without compromising stability, thereby maximizing reach. The knee serves as a critical force transfer point between the foot and hip within the lower kinetic chain.33 Subtle knee sway adjustments optimize alignment and coordination across the kinetic chain, enhancing forward movement and task performance. These dynamic adjustments improve reach mechanics by maintaining stability and efficiently distributing the mechanical load across the lower limbs.
Posterior Reaching Control
A previous study on joint kinematic predictors reported angular displacement as the primary predictor of normalized reach distance for posterior direction tasks. The study found that hip flexion combined with ipsilateral and contralateral trunk bending as the most predictive factor for posteromedial and posterolateral reaching, respectively.15 In contrast, our study found that trunk RMS displacement was the optimal predictor for both posterior reaches. Dynamic balance control for backward postural stability involves complex interactions among multiple joints and sensorimotor strategies. APAs are critical in maintaining balance during dynamic movements, such as backward reaching. These adjustments encompass changes in kinematics, kinetics, and muscle activity patterns to counteract perturbations and stabilize the body.34
Trunk RMSD represents the body’s COM, contributing significantly to stability through coordinated joint COM adjustments, particularly at the hip, knee, and ankle.35 This study found a significant correlation between the posterior dynamic balance score, body COM, and knee RMSD. Notably, body COM has emerged as the primary mechanism for controlling backward-reaching movements, as demonstrated in both healthy individuals and those with ankle balance deficits.13 Figure 4 visually represents this interaction, illustrating the relationship between COM dynamics and reach scores during posterior reaching tasks.
The knee joint plays a crucial role in balance control during dynamic tasks. Research indicates that knee joint stiffness and viscosity adjust to maintain postural equilibrium before movement initiation.36 Additionally, the knee provides a corrective compensatory mechanism in postural regulation, facilitating anticipatory sensorimotor strategies through neuroplasticity.37 In conclusion, body COM and the knee joint’s role in COM control are critical for maintaining balance during these movements.
Moreover, regarding the kinematic pattern of posterior reaching, hip flexion facilitates forward trunk displacement, compensating for the backward movement of the reaching leg and maintaining the COM within the base of support. This forward trunk movement coordinated with hip flexion is essential for weight distribution control and body stabilization during dynamic balance tasks.23,29 These findings emphasize the critical role of hip flexion in COM adjustment and dynamic stability during the SEBT, particularly in the posterior leg reach.
Interpreting these findings within the framework of APAs and segmental coordination models enhances their theoretical significance. APAs are feedforward mechanisms that prepare the body for movement by activating stabilizing muscles. The significant involvement of body displacement and hip coordination in the posterior reach direction indicates that effective APAs are essential for shifting and stabilizing the COM during challenging postural transitions. Similarly, segmental coordination models describe how body segments interact in a temporally precise and mechanically efficient sequence. Our results align with these patterns: anterior reach relies more on ankle mobility and knee-driven propulsion, whereas posterior reach requires the coordinated action of the trunk, hip, and knee. This supports the view that dynamic balance is not solely a function of joint flexibility or strength but rather of integrated neuromuscular control involving the entire kinetic chain. These frameworks contextualize the observed direction-specific strategies and provide insight into how impairments in one segment may influence the entire movement system.
Application to Sports and Rehabilitation
These findings have important implications for both athletic performance and rehabilitation. Enhancing ankle DF ROM and hip control in athletic contexts may improve performance in tasks that require directional changes, landings, or single-leg stability. In rehabilitation, targeted interventions can address specific joint mechanics, such as ankle mobility or trunk control, based on direction-specific deficits observed in the mSEBT. For example, athletes recovering from ankle injuries may benefit from DF mobility training to restore anterior reach capacity. In contrast, individuals with posterior instability may require core- and hip-focused strategies to enhance COM control.
Limitations and Further Study
This study had several limitations. First, the participants were primarily young, healthy individuals, potentially limiting the generalizability of the results to other demographic groups. Future research should include larger and more diverse cohorts with variations in age, physical activity levels, and injury backgrounds to improve applicability. Additionally, expanding the scope to include sports-specific or high-impact movements may enhance the relevance of these findings for athletic performance and rehabilitation. Second, this study examined angular displacement in a single plane in relation to balance performance. Future research should explore the complex multiplanar interactions between joints during functional tasks. Third, this assessment requires adequate balance and mobility, making it unsuitable for individuals at high risk of falls, who may need alternative evaluations tailored to their functional capabilities. Consequently, the specific joint and COM control mechanisms identified in this study may not directly translate to other dynamic balance assessments that involve different movement strategies or target distinct domains of postural control. Finally, although the model demonstrated promising associations between variables, some confidence intervals were relatively broad, indicating variability in the estimates. Nonetheless, this study represents a significant initial effort to integrate both COM displacement and joint ROM in predicting dynamic balance performance. Further research with larger sample sizes is warranted to validate and extend these preliminary findings.
Conclusion
This study highlights key biomechanical factors influencing dynamic balance, emphasizing the interplay between joint mobility and segmental movement control. The findings confirm that ankle DF ROM is a primary determinant of anterior reach performance, while body COM displacement and hip F ROM play significant roles in the posteromedial and posterolateral directions. The stepwise regression models demonstrated strong predictive power, reinforcing the relevance of joint mobility and segmental control in dynamic balance. Notably, this study demonstrated the feasibility and precision of using single and multiple IMU sensors to capture key biomechanical parameters, highlighting valuable applications in clinical and sports settings. Although the findings were derived from healthy adults, they provide critical insights that may inform future research and practice in broader populations, including individuals with balance deficits. These results contribute to a deeper understanding of dynamic balance mechanisms and support the integration of wearable technology in biomechanical assessment and intervention design.
Summary
- Ankle dorsiflexion predicted anterior reach performance, whereas the body center of mass (COM) displacement was the strongest predictor of posterior reach performance. The addition of hip flexion increased the predictive power, highlighting the combined role of COM control and hip mechanics in dynamic balance. This synergy underscores the importance of trunk stability and hip flexibility in postural control during multidirectional movement, particularly in the posterior direction.
- Kinematic patterns revealed direction-specific strategies: the knee dominated anterior reach tasks with the largest angular displacement, whereas the hip was the primary contributor to posterior reaches. The ankle played a stabilizing role in all directions.
- This study demonstrated the usefulness of Inertial Measurement Units (IMUs) sensors for capturing biomechanical data and improving balance assessment precision. The findings emphasize the potential of IMU-based methodologies to enhance future clinical and sports experiments.
Abbreviations
APAs, Anticipatory postural adjustments; COM, Center of mass; DF/PF, Dorsiflexion/Plantarflexion; F/E: Flexion/Extension; IMUs: Inertial measurement units; mSEBT: Modified Star Excursion Balance Test; RMSD: Root mean square displacement; ROM: Range of motion.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Statement
The study was approved by the Research Ethics Review Committee of the Faculty of Design, Kyushu University (approval number: 593/2023) on December 27, 2023. Before the experiment, all participants were given information about the study protocol and underwent a health status screening. The consent form was signed by the participants before the testing. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Acknowledgment
We thank all participants for their support with the experiment. Philippe C Dixon acknowledges support from the Fonds de Recherche Québec (FRQ) (Santé sector) Junior 1 research scholar award. https://doi.org/10.69777/311675.
Funding
This research did not receive any specific grant from public, commercial, or non-profit funding agencies.
Disclosure
The authors state that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
References
1. Yiou E, Caderby T, Hussein T. Adaptability of anticipatory postural adjustments associated with voluntary movement. World J Orthop. 2012;3(6):75–86. doi:10.5312/wjo.v3.i6.75
2. Kiefer AW, Riley MA, Shockley K, et al. Multi-segmental postural coordination in professional ballet dancers. Gait Posture. 2011;34(1):76–80. doi:10.1016/j.gaitpost.2011.03.016
3. Plisky P, Schwartkopf-Phifer K, Huebner B, Garner MB, Bullock G. Systematic review and meta-analysis of the y-balance test lower quarter: reliability, discriminant validity, and predictive validity. Int J Sports Phys Ther. 2021;16(5):1190–1209. doi:10.26603/001c.27634
4. Robinson R, Gribble P. Kinematic predictors of performance on the star excursion balance test. J Sport Rehabil. 2008;17(4):347–357. doi:10.1123/jsr.17.4.347
5. Nelson S, Wilson CS, Becker J. Kinematic and kinetic predictors of Y-balance test performance. Int J Sports Phys Ther. 2021;16(2):371–380. doi:10.26603/001c.21492
6. Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131–137. doi:10.2519/jospt.2006.36.3.131
7. Herrington L, Hatcher J, Hatcher A, McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009;16(2):149–152. doi:10.1016/j.knee.2008.10.004
8. Bouillon LE, Baker JL. Dynamic balance differences as measured by the star excursion balance test between adult-aged and middle-aged women. Sports Health. 2011;3(5):466–469. doi:10.1177/1941738111414127
9. McCann RS, Kosik KB, Beard MQ, Terada M, Pietrosimone BG, Gribble PA. Variations in star excursion balance test performance between high school and collegiate football players. J Strength Cond Res. 2015;29:2765–2770. doi:10.1519/JSC.0000000000000947
10. Taylor L, Miller E, Kaufman KR. Static and dynamic validation of inertial measurement units. Gait Posture. 2017;57:80–84. doi:10.1016/j.gaitpost.2017.05.026
11. Deodato M, Coan L, Buoite Stella A, et al. Inertial sensors-based assessment to detect hallmarks of chronic ankle instability during single-leg standing: is the healthy limb “healthy”? Clin Biomech. 2023;107:106036. doi:10.1016/j.clinbiomech.2023.106036
12. Liu J, Zhang X, Lockhart TE. Fall risk assessments based on postural and dynamic stability using inertial measurement unit. Saf Health Work. 2012;3(3):192–198. doi:10.5491/SHAW.2012.3.3.192
13. Phuaklikhit C, Junsri T, Maikaew U. The correlation of centre of mass evaluation utilising accelerometry-based measurement and the clinical dynamic balance test in professional football athletes with chronic ankle instability. Heliyon. 2023;9(6):e17318. doi:10.1016/j.heliyon.2023.e17318
14. Germanotta M, Mileti I, Conforti I, Del Prete Z, Aprile I, Palermo E. Estimation of human center of mass position through the inertial sensors-based methods in postural tasks: an accuracy evaluation. Sensors. 2021;21(2):1–17. doi:10.3390/s21020601
15. Kang MH, Kim GM, Kwon OY, Weon JH, Oh JS, An DH. Relationship between the kinematics of the trunk and lower extremity and performance on the Y-balance test. Pm&r. 2015;7(11):1152–1158. doi:10.1016/j.pmrj.2015.05.004
16. Phuaklikhit C, Junsri T, Saito S, Muraki S, Loh PY. Biomechanical and physiological variables in dynamic and functional balance control during single-leg loading in individuals with chronic ankle instability: a scoping review. Sports. 2024;12(8):224. doi:10.3390/sports12080224
17. Picot B, Terrier R, Forestier N, Fourchet F, McKeon PO. The star excursion balance test: an update review and practical guidelines. Int J Athl Ther Train. 2021;26(6):285–293. doi:10.1123/ijatt.2020-0106
18. Floor-Westerdijk MJ, Schepers HM, Veltink PH, Asseldonk EHF, van Buurke JH. Use of inertial sensors for ambulatory assessment of center-of-mass displacements during walking. IEEE Trans Biomed Eng. 2012;59(7):2080–2084. doi:10.1109/TBME.2012.2197211
19. Mancini M, Salarian A, Carlson-Kuhta P, et al. ISway: a sensitive, valid and reliable measure of postural control. J Neuroeng Rehabil. 2012;9(1):59. doi:10.1186/1743-0003-9-59
20. O’Sullivan M, Blake C, Cunningham C, Boyle G, Finucane C. Correlation of accelerometry with clinical balance tests in older fallers and non-fallers. Age Ageing. 2009;38(3):308–313. doi:10.1093/ageing/afp009
21. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911–919. doi:10.2519/jospt.2006.2244
22. Powden CJ, Dodds TK, Gabriel EH. The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: a systematic review. Int J Sports Phys Ther. 2019;14(5):683–694. doi:10.26603/ijspt20190683
23. Gribble PA, Hertel J, Plisky P. Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339–357. doi:10.4085/1062-6050-47.3.08
24. Shah VR, Dixon PC, Willmott AP. Corrigendum to “Evaluation of lower-body gait kinematics on outdoor surfaces using wearable sensors” [J. Biomech]. 177 (2024) 112401]. J Biomech. 2025;(178):112425. doi:10.1016/j.jbiomech.2024.112425
25. McGrath D, Greene BR, O’Donovan KJ, Caulfield B. Gyroscope-based assessment of temporal gait parameters during treadmill walking and running. Sports Engine. 2012;15(4):207–213. doi:10.1007/s12283-012-0093-8
26. Bulow A, Anderson JE, Leiter JR, Macdonald PB, Peeler J. The modified star excursion balance and Y-balance test results differ when assessing physically active healthy adolescent females. Int J Sports Phys Ther. 2019;14(2):192–203. doi:10.26603/ijspt20190192
27. Gribble PA, Hertel J. Considerations for normalizing measures of the star excursion balance test. Meas Phys Educ Exerc Sci. 2003;7(2):89–100. doi:10.1207/S15327841MPEE0702_3
28. López-Valenciano A, Ayala F, De Ste Croix M, Barbado D, Vera-Garcia FJ. Different neuromuscular parameters influence dynamic balance in male and female football players. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):962–970. doi:10.1007/s00167-018-5088-y
29. Earl JE, Hertel J. Lower-extremity muscle activation during the star excursion balance tests. J Sport Rehabil. 2001;10(2):93–104. doi:10.1123/jsr.10.2.93
30. Dill KE, Begalle RL, Frank BS, Zinder SM, Padua DA. Altered knee and ankle kinematics during squatting in those with limited weight-bearing–Lunge ankle-dorsiflexion range of motion. J Athl Train. 2014;49(6):723–732. doi:10.4085/1062-6050-49.3.29
31. Hoch MC, Staton GS, Medina McKeon JM, Mattacola CG, McKeon PO. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport. 2012;15(6):574–579. doi:10.1016/j.jsams.2012.02.009
32. Akbari H, Shimokochi Y, Sheikhi B. Ankle dorsiflexion range of motion and landing postures during a soccer-specific task. PLoS One. 2023;18(3):e0283150. doi:10.1371/journal.pone.0283150
33. Hewett TE, Ford KR, Hoogenboom BJ, Myer GD, Timothy hewett CE. Understanding and preventing ACL injuries: current biomechanical and epidemiologic considerations-update 2010. North Ame J Sports Phys Therap. 2010;5(4):234–251.
34. Commissaris DACM, Toussaint HM. Anticipatory postural adjustments in a bimanual, whole body lifting task with an object of known weight. Hum Mov Sci. 1997;16(4):407–431. doi:10.1016/S0167-9457(97)00007-9
35. Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(suppl_2):ii7–ii11. doi:10.1093/ageing/afl077
36. Patla AE, Ishac MG, Winter DA. Anticipatory control of center of mass and joint stability during voluntary arm movement from a standing posture: interplay between active and passive control. Exp Brain Res. 2002;143(3):318–327. doi:10.1007/s00221-001-0968-6
37. Gauchard GC, Vançon G, Meyer P, Mainard D, Perrin PP. On the role of knee joint in balance control and postural strategies: effects of total knee replacement in elderly subjects with knee osteoarthritis. Gait Posture. 2010;32(2):155–160. doi:10.1016/j.gaitpost.2010.04.002
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





