Back to Journals » Cancer Management and Research » Volume 17
Exploration of the Evaluation Value of Combined Magnetic Resonance Imaging and Ultrasound Blood Flow Parameters in Cervical Lymph Node Metastasis of Thyroid Cancer
Authors Sun X, Wei Z, Luo Y, Wang M
Received 19 November 2024
Accepted for publication 5 March 2025
Published 20 March 2025 Volume 2025:17 Pages 651—659
DOI https://doi.org/10.2147/CMAR.S505730
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kattesh Katti
Xiaosong Sun,1 Zhengchao Wei,1 Yiqiang Luo,2 Ming Wang1
1Department of Thyroid-Head & Neck Surgery, Jilin Cancer Hospital, Changchun, People’s Republic of China; 2Department of Preventive Health Care, Jilin Cancer Hospital, Changchun, People’s Republic of China
Correspondence: Ming Wang, Email [email protected]
Background: Thyroid cancer exhibits the highest cervical lymph node metastasis rate (20– 50%) among head and neck malignancies, with occult metastasis occurring in 30– 80% of papillary carcinoma cases. However, conventional single-modality imaging faces certain challenges: MRI has limited sensitivity for detecting micro-metastases (< 2mm), while Doppler ultrasound may overlook metastases in isoechoic lymph nodes. Therefore, it is crucial to evaluate the diagnostic value of combining MRI and CDUS. This study aims to retrospectively analyze the diagnostic value of combining MRI and CDUS blood flow parameters in detecting cervical lymph node metastasis in thyroid cancer and to compare the diagnostic performance with MRI or CDUS alone.
Objective: To analyze the evaluation value of combining MRI and color Doppler ultrasound (CDUS) blood flow parameters in detecting cervical lymph node metastasis of thyroid cancer, particularly for occult metastases.
Methods: A retrospective analysis was conducted on 263 thyroid cancer patients (June 2022-June 2024). Diagnostic consistency between MRI, CDUS parameters (resistive index, pulsatility index, vascular patterns) and pathology were compared. Multimodal evaluation criteria were established: (1) MRI positive signs (lymph node diameter > 8mm, cystic change, enhancement heterogeneity) (2) CDUS thresholds (RI≥ 0.75, PI≥ 1.25 with chaotic vascularity).
Results: Among 263 patients, 98 had pathologically confirmed metastases. CDUS showed higher consistency with pathology (Kappa=0.783) than MRI (Kappa=0.645). Combined modality achieved 94.9% sensitivity vs 86.7% (CDUS) and 78.6% (MRI), with accuracy improving from 82.1%/75.3% to 89.4% (P< 0.05). Notably, 12/22 occult metastases (≤ 3mm) were only detected by combined approach.
Conclusion: The synergistic combination leverages MRI’s structural characterization and CDUS’s hemodynamic sensitivity, effectively overcoming single-modality limitations in detecting micro-metastases. This dual-assessment protocol addresses thyroid cancer’s propensity for early lymphatic spread, providing critical preoperative staging guidance.
Keywords: magnetic resonance imaging, ultrasound blood flow parameters, thyroid cancer, cervical lymph node metastasis, evaluation value
Introduction
Thyroid cancer is the most common endocrine malignancy, with an increasing incidence worldwide.1 Among the various subtypes of thyroid cancer, papillary thyroid carcinoma (PTC) is the most common, accounting for approximately 85% of all cases.2 Cervical lymph node metastasis, especially in PTC patients, presents a significant challenge in clinical management.3 Cervical lymph node metastasis not only affects the clinical staging of thyroid cancer but is also closely related to patient prognosis.4 Accurate assessment of cervical lymph node metastasis in thyroid cancer patients is critical for formulating appropriate treatment plans and improving patient survival rates.
In recent years, with advances in imaging technology, magnetic resonance imaging (MRI) and color Doppler ultrasound (CDUS) have been widely used in the diagnosis and evaluation of thyroid cancer. MRI, as a non-invasive examination method, can provide high-resolution soft tissue contrast images, aiding in the identification of cervical lymph node size, morphology, and internal structure.5 However, MRI still has limitations in detecting early lymph node metastasis. CDUS, by measuring hemodynamic parameters, provides important insights into the blood flow characteristics of lymph nodes.6 Studies7 have shown that changes in blood flow within lymph nodes are often closely associated with malignant metastasis, thus giving CDUS significant diagnostic value in the early detection of cervical lymph node metastasis.
However, there have been conflicting results in previous studies regarding the sensitivity and accuracy of MRI and CDUS in detecting lymph node metastases in thyroid cancer. Some studies have shown that MRI has higher accuracy in identifying larger metastases but is less effective for micro-metastases, while others suggest that CDUS is more sensitive in detecting smaller metastases due to its ability to visualize blood flow patterns. Despite these advances, both methods, when used individually, still have limitations, particularly in terms of sensitivity and specificity. These controversies highlight the need for further investigation into the combined diagnostic value of MRI and CDUS blood flow parameters in thyroid cancer.
Given these points, this study aims to explore the combined application of MRI and CDUS blood flow parameters to assess cervical lymph node metastasis in thyroid cancer, with the goal of providing evidence for optimizing clinical diagnosis and treatment plans. By comparing the performance of MRI, CDUS, and their combination, we hope to offer a more accurate and reliable method for the early detection of lymph node metastasis, ultimately improving patient outcomes.
Subjects and Methods
Study Subjects and Inclusion Criteria
A retrospective analysis was conducted on the clinical and imaging data of 263 patients with thyroid cancer treated in our hospital from June 2022 to June 2024. Inclusion criteria: (1) All patients were clinically diagnosed with thyroid cancer through relevant tests;8 (2) All patients underwent surgery for the first time; (3) Patients were ≥18 years old, with no gender restriction; (4) The clinical data of the participants were complete and authentic for analysis. Exclusion criteria: (1) Patients with other types of thyroid diseases; (2) Patients with other primary malignant tumors; (3) Patients with preoperative confirmed cervical lymph node metastasis; (4) Pregnant or lactating women; (5) Patients with allergies or contraindications to the procedures and examinations performed in this study; (6) Patients with cognitive, communicative, or psychiatric disorders; (7) Patients with incomplete clinical data.
Methods
MRI
A Philips 1.5 TMR scanner was used, equipped with a single-channel soft surface coil. Scanning parameters: matrix of 512*512, slice thickness of 3~4 mm, spacing of 0.3~0.4 mm, and FOV of 16~20 cm. The scanning sequences included axial T1WI, T2WI, and DWI (with b-values of 0 and 800 s/m²), as well as multiphase enhanced T1WI. A high-pressure injector was used for intravenous injection of the gadolinium contrast agent (Magnevist, Bayer Pharmaceuticals) at a rate of 3 mL/s. Images were acquired before contrast injection and at 30s, 60s, 120s, 180s, 240s, and 300s after contrast injection. All patients underwent respiratory training before MRI, and respiratory gating technology was applied to ensure the acquisition phase remained at the same respiratory level, in order to avoid artifacts caused by patient breathing and swallowing.
Criteria for diagnosing cervical lymph node metastasis:9 (1) Cystic lesions of the lymph nodes or cystic lymph nodes with a thin wall; (2) The smallest transverse diameter of the lymph node ≥15 mm; (3) High signal intensity in both T1 and T2 phases.
CDUS
A Philips iE33 CDUS scanner was used, with a probe frequency of 3~11 MHz. Real-time scanning of the cervical lymph nodes of the thyroid was performed to observe the echo characteristics of the lymph nodes. Energy Doppler was activated, and the gain was appropriately increased until clear blood flow signals were observed. The strongest blood flow signal plane was identified and saved as the standard plane in the workstation to calculate the MCVD value. Criteria for diagnosing cervical lymph node metastasis:10 (1) Enlargement of the cervical lymph nodes with the longest diameter >5 mm; (2) The ratio of long to short diameter ≤2; (3) Blurred boundaries of the cervical lymph nodes with cortical thickening ≥3 mm; (4) Fusion phenomenon; (5) Abundant blood flow distribution inside the lymph node; (6) Blood flow parameter MCVD >0.2.
Observation Indicators
Examination Results
The consistency between the MRI results, CDUS blood flow parameters, and pathological examination results was compared.
Diagnostic Performance
Pathological examination was used as the gold standard, and the diagnostic performance of MRI, CDUS blood flow parameters, and the combination of both for diagnosing cervical lymph node metastasis in thyroid cancer was compared.
Diagnostic Value
Pathological examination was used as the gold standard, and ROC curves were used to analyze the diagnostic value of MRI, CDUS blood flow parameters, and their combination in diagnosing cervical lymph node metastasis in thyroid cancer.
Statistical Analysis
GraphPad Prism 8 software was used for graphing, and SPSS 22.0 software was used for data analysis. Categorical data were expressed as [n (%)], and the chi-square test was used. Normally distributed quantitative data were expressed as  , and independent sample t-tests were used for group comparisons. The Kappa test was used to analyze the consistency between MRI results, CDUS blood flow parameters, and pathological examination results. Receiver operating characteristic (ROC) curves were plotted to analyze the diagnostic value of MRI, CDUS blood flow parameters, and their combination in diagnosing cervical lymph node metastasis in thyroid cancer. A value of P<0.05 was considered statistically significant.
, and independent sample t-tests were used for group comparisons. The Kappa test was used to analyze the consistency between MRI results, CDUS blood flow parameters, and pathological examination results. Receiver operating characteristic (ROC) curves were plotted to analyze the diagnostic value of MRI, CDUS blood flow parameters, and their combination in diagnosing cervical lymph node metastasis in thyroid cancer. A value of P<0.05 was considered statistically significant.
Results
Analysis of Thyroid Cancer Metastatic Lymph Node Features in CDUS and MRI Imaging
The data of patients with true positive diagnoses by CDUS were analyzed, revealing the following signs of metastatic lymph nodes (Figure 1a–c): Lymph node enlargement, with the longitudinal diameter often exceeding 1 cm, but the ratio of longitudinal to transverse diameter usually <2. The shape is irregular, round, or nearly round, with an unclear boundary for accurate localization. Disordered blood flow signals within the node: The internal echo is uneven, and the lymphatic hilum structure is displaced from its original position. The MRI results of positive patients showed that T1WI. imaging often showed that the metastatic lymph node had a similar density to the surrounding tissue, but on T2WI. imaging, a higher density could be observed (Figure 1d–f).
Basic Information of Study Subjects
Table 1 presents the basic information of the study subjects, including age, gender, histopathological types of thyroid cancer, lymph node metastasis status, and TNM staging. These characteristics are key factors in evaluating the clinical presentation and metastasis of thyroid cancer patients.
Analysis of MRI Examination Results and CDUS Blood Flow Parameters
Pathological examination showed that among the 263 thyroid cancer patients, 98 had cervical lymph node metastasis, while the remaining 165 patients did not. The consistency of the CDUS blood flow parameter examination results with the pathological examination results (Kappa = 0.783) was higher than that of MRI examination (Kappa = 0.645), as shown in Table 2.
 |
Table 1 Basic Information of Study Subjects |
Comparison of Diagnostic Performance of MRI, CDUS Blood Flow Parameters, and Their Combination for Cervical Lymph Node Metastasis in Thyroid Cancer
The sensitivity and accuracy of the combined examination for diagnosing cervical lymph node metastasis in thyroid cancer were higher than those of CDUS blood flow parameters or MRI examination alone. Additionally, the sensitivity and accuracy of CDUS blood flow parameters were higher than those of MRI examination (P<0.05). There was no significant difference in specificity between the two methods and their combination in diagnosing cervical lymph node metastasis in thyroid cancer (P>0.05), as shown in Table 3.
 |
Table 2 Analysis of MRI Examination Results and CDUS Blood Flow Parameters |
Comparison of Diagnostic Value of MRI, CDUS Blood Flow Parameters, and Their Combination for Cervical Lymph Node Metastasis in Thyroid Cancer
The areas under the curve (AUC) for MRI examination, CDUS blood flow parameters, and their combination in diagnosing cervical lymph node metastasis in thyroid cancer were 0.807, 0.835, and 0.906, respectively. The AUC of the combined examination was higher than that of CDUS blood flow parameters or MRI examination alone (P<0.05), as shown in Table 4 and Figure 2.
 |
Table 3 Comparison of Diagnostic Performance of MRI, CDUS Blood Flow Parameters, and Their Combination for Cervical Lymph Node Metastasis in Thyroid Cancer |
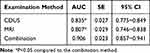 |
Table 4 Comparison of Diagnostic Value of MRI, CDUS Blood Flow Parameters, and Their Combination for Cervical Lymph Node Metastasis in Thyroid Cancer |
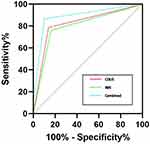 |
Figure 2 ROC Curve Analysis of MRI, CDUS Blood Flow Parameters, and Their Combination for Diagnosing Cervical Lymph Node Metastasis in Thyroid Cancer. |
Discussion
The neck is the most common site for lymph node metastasis in head and neck malignant tumors and is also a major area for terminal lymph node metastasis from thoracic and abdominal tumors.11 Therefore, accurately assessing the metastasis of cervical lymph nodes plays a crucial role in determining tumor staging and selecting treatment plans. However, due to the complex structure of the neck and the varying depths of lymph nodes, surgeons often rely on palpation during surgery to assess whether the lymph nodes are enlarged and to judge the metastasis, which in turn determines whether to perform cervical lymph node dissection. This method of relying on palpation is prone to missed diagnoses and misdiagnoses, especially for early or small lymph node metastases, which may be difficult to detect.12 At the same time, unnecessarily enlarging the surgical scope may cause unnecessary trauma to patients without metastasis, increasing surgical risks, prolonging postoperative recovery time, and ultimately affecting the patient’s quality of life.13 In recent years, with the rapid development of imaging technology, MRI has been widely used in diagnosing cervical lymph node lesions. MRI can not only clearly show the size and morphology of lymph nodes but also to a certain extent determine whether lymph node metastasis exists.14 However, MRI still presents a high rate of false positives and false negatives in clinical practice, especially when evaluating early or small lymph node metastases, where its accuracy remains insufficient.15 The primary disadvantage of MRI is its inability to reliably detect micro-metastases, particularly those less than 2mm in size, due to its limited sensitivity in these cases. Furthermore, MRI can sometimes be hindered by factors such as patient movement and artifacts from surrounding structures.
In contrast, CDUS demonstrates unique advantages in assessing tumor hemodynamics. CDUS, by reflecting the microvascular generation and blood perfusion within tumor tissue, provides crucial evidence for determining tumor growth, invasion, and metastasis.16 The key advantage of CDUS is its ability to evaluate blood flow within lymph nodes, which can highlight areas of angiogenesis—a critical indicator of metastasis. Studies17 have shown that the proliferation, invasion, and metastasis of tumor cells depend on the blood supply from newly formed blood vessels, and CDUS can display clear blood flow imaging, showing the low-speed blood flow and vascular network structure within the tumor, almost unaffected by blood flow direction and angle. Therefore, CDUS can evaluate tumor growth and metastasis by observing tumor angiogenesis, especially showing high diagnostic value in assessing cervical lymph node metastasis. However, CDUS has limitations in terms of its ability to resolve fine details in deeply located lymph nodes, especially in the central neck region, where ultrasound penetration can be limited. Additionally, CDUS relies on operator experience, and variability in results may occur.
The results of this study show that the consistency between CDUS blood flow parameters and pathological examination results is significantly higher than that of MRI. In particular, in diagnosing cervical lymph node metastasis of thyroid cancer, the sensitivity and accuracy of CDUS blood flow parameters are superior to MRI, indicating that CDUS has higher clinical utility in assessing cervical lymph node metastasis. This is consistent with the results of several studies,18,19 further proving the importance of CDUS in evaluating tumor metastasis. Given the advantages and disadvantages of each technique, a combined approach of CDUS and MRI offers a more comprehensive assessment of cervical lymph node metastasis. MRI can provide clear structural information, such as lymph node size and shape, which is particularly useful for detecting larger or well-defined metastatic nodes. In contrast, CDUS complements MRI by evaluating blood flow characteristics, which helps detect smaller or early metastases that might not be visible on MRI. When lymph nodes are located in challenging areas (such as the central neck region) or when they present with ambiguous features (eg, irregular margins or atypical blood flow), the combined use of CDUS and MRI ensures higher diagnostic precision.
Related research20 indicates that rapid tumor growth is often accompanied by the process of angiogenesis, which not only promotes the expansion of tumor size but also increases the risk of tumor cells entering blood vessels and the bloodstream, significantly raising the possibility of distant metastasis through the blood or lymphatic systems. In imaging evaluations of cervical lymph nodes, conventional ultrasound and CDUS have shown good imaging results in clinical practice. However, there is no unified standard for the size threshold of metastatic lymph nodes in the neck, and this uncertainty may lead to false positive or false negative results in the diagnostic process.21,22 Particularly when observing lymph nodes in the central region, the deep location and complex structure of this area limit the penetration power of ultrasound, making it difficult to clearly display the detailed anatomical structure of this region, leading to missed diagnoses. Additionally, there is some overlap in the imaging characteristics of metastatic and non-metastatic lymph nodes. For instance, some non-metastatic lymph nodes may exhibit typical metastatic characteristics such as blurred margins and rich blood flow signals, while some metastatic lymph nodes may show imaging features such as clear margins and uniform internal structure. The overlap of these imaging features reduces the accuracy of diagnosing metastatic lymph nodes, affecting diagnostic precision. To address these issues, recent studies23 have proposed the combined use of CDUS and MRI in diagnosing lymph node metastasis. MRI, with its high tissue contrast and resolution, allows for multiplanar imaging and clearly displays the structures of cervical blood vessels and lymph nodes.24,25 Especially with the application of fat suppression techniques, MRI can better reveal abnormal lymph nodes, significantly improving imaging quality in complex cervical regions. Compared to CDUS, MRI can not only provide more accurate structural information of lymph nodes but also reduce interference from artifacts, further enhancing image spatial resolution and contrast between lesions and surrounding normal tissues.26 The results of this study show that the combined use of CDUS and MRI has higher accuracy in diagnosing cervical lymph node metastasis in thyroid cancer. Through comparative analysis of the AUC, it was found that the AUC of the combined examination is significantly higher than that of CDUS blood flow parameters or MRI alone, indicating that combined diagnosis can effectively improve the diagnostic value of cervical lymph node metastasis. In summary, the combined examination of CDUS blood flow parameters and MRI can not only improve the diagnostic accuracy of cervical lymph node metastasis in thyroid cancer but also provide more reliable preoperative evaluation and treatment planning.
It should be noted that although the results of this study provide important evidence for the clinical application of MRI and CDUS in the combined diagnosis of cervical lymph node metastasis in thyroid cancer, there are still several limitations: (1) Limitations of study design: This study is a single-center retrospective study. Although the sample size is relatively sufficient, the data is limited to one hospital, which may introduce regional and selection biases, limiting the generalizability of the results. Additionally, the retrospective design means that data collection for some cases may be incomplete, potentially affecting the comprehensiveness of the diagnostic results. (2) Heterogeneity of different types of thyroid cancer and lymph node metastasis characteristics: This study did not conduct detailed subtype analysis of different types of thyroid cancer and their corresponding metastasis characteristics. Thyroid cancer includes various types such as papillary carcinoma, follicular carcinoma, medullary carcinoma, and anaplastic carcinoma. There are significant differences in the mechanisms and clinical manifestations of lymph node metastasis among different subtypes. Future studies should explore the sensitivity and specificity of different imaging methods in relation to the metastasis characteristics of each subtype of thyroid cancer, to provide more personalized diagnostic strategies. (3) Cost and efficiency of combined examinations: Although the combined use of MRI and CDUS improves diagnostic efficiency, this combined application in clinical practice involves higher examination costs, especially since MRI is relatively expensive and time-consuming, which may impact the rational allocation of medical resources and the financial burden on patients. In conclusion, this study shows that the combined diagnosis of MRI and CDUS has significant advantages in diagnosing cervical lymph node metastasis in thyroid cancer, but there are still several limitations. Future research should expand sample sizes, refine cancer subtype analyses, and optimize imaging techniques and processes to further improve diagnostic accuracy and clinical feasibility.
Conclusion and Limitations
In summary, the combined examination of CDUS blood flow parameters and MRI can not only improve the diagnostic accuracy of cervical lymph node metastasis in thyroid cancer but also provide more reliable preoperative evaluation and treatment planning.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethics
This study was approved by the ethics committee of Jilin Cancer Hospital. Informed consent was obtained from all study participants. All the methods were carried out in accordance with the Declaration of Helsinki.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Nabhan F, Dedhia PH, Ringel MD. Thyroid cancer, recent advances in diagnosis and therapy. Int J Cancer. 2021;149(5):984–992. doi:10.1002/ijc.33690
2. Boucai L, Zafereo M, Cabanillas ME. Thyroid cancer: a review. JAMA. 2024;331(5):425–435. doi:10.1001/jama.2023.26348
3. Filetti S, Durante C, Hartl D, et al. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30(12):1856–1883. doi:10.1093/annonc/mdz400
4. Araque KA, Gubbi S, Klubo-Gwiezdzinska J. Updates on the management of thyroid cancer. Horm Metab Res. 2020;52(8):562–577. doi:10.1055/a-1089-7870
5. Zhang H, Hu S, Wang X, et al. Prediction of cervical lymph node metastasis using MRI radiomics approach in papillary thyroid carcinoma: a feasibility study. Technol Cancer Res Treat. 2020;19:1533033820969451. doi:10.1177/1533033820969451
6. Leng X, Liu J, Zou Q, et al. Application of color Doppler ultrasound and US shear wave elastography with connective tissue growth factor in the risk assessment of papillary thyroid carcinoma. BMC Med Imaging. 2024;24(1):173. doi:10.1186/s12880-024-01354-w
7. Grimm D. Recent advances in thyroid cancer research. Int J Mol Sci. 2022;23(9):4631. doi:10.3390/ijms23094631
8. Giovanella L, Tuncel M, Aghaee A, et al. Theranostics of thyroid cancer. Semin Nucl Med. 2024;54(4):470–487. doi:10.1053/j.semnuclmed.2024.01.011
9. Park VY, Han K, Kim HJ, et al. Radiomics signature for prediction of lateral lymph node metastasis in conventional papillary thyroid carcinoma. PLoS One. 2020;15(1):e0227315. doi:10.1371/journal.pone.0227315
10. Guo JN, Song L-H, Yu P-Y, et al. Ultrasound elastic parameters predict central lymph node metastasis of papillary thyroid carcinoma. J Surg Res. 2020;253:69–78. doi:10.1016/j.jss.2020.03.042
11. Wang C, Yu P, Zhang H, et al. Artificial intelligence-based prediction of cervical lymph node metastasis in papillary thyroid cancer with CT. Eur Radiol. 2023;33(10):6828–6840. doi:10.1007/s00330-023-09700-2
12. Liu W, Zhang D, Jiang H, et al. Prediction model of cervical lymph node metastasis based on clinicopathological characteristics of papillary thyroid carcinoma: a dual-center retrospective study. Front Endocrinol. 2023;14:1233929. doi:10.3389/fendo.2023.1233929
13. Xiao J, Meng S, Zhang M, et al. Optimal method for detecting cervical lymph node metastasis from papillary thyroid cancer. Endocrine. 2023;79(2):342–348. doi:10.1007/s12020-022-03213-6
14. Qin H, Que Q, Lin P, et al. Magnetic resonance imaging (MRI) radiomics of papillary thyroid cancer (PTC): a comparison of predictive performance of multiple classifiers modeling to identify cervical lymph node metastases before surgery. Radiol Med. 2021;126(10):1312–1327. doi:10.1007/s11547-021-01393-1
15. Cho SJ, Suh CH, Baek JH, et al. Diagnostic performance of MRI to detect metastatic cervical lymph nodes in patients with thyroid cancer: a systematic review and meta-analysis. Clin Radiol. 2020;75(7):562.e1–562.e10. doi:10.1016/j.crad.2020.03.025
16. Lee CU, Hesley GK, Uthamaraj S, et al. Using ultrasound color Doppler twinkling to identify biopsy markers in the breast and axilla. Ultrasound Med Biol. 2021;47(11):3122–3134. doi:10.1016/j.ultrasmedbio.2021.04.018
17. Alexander LF, Patel NJ, Caserta MP, et al. Thyroid ultrasound: diffuse and nodular disease. Radiol Clin North Am. 2020;58(6):1041–1057. doi:10.1016/j.rcl.2020.07.003
18. Wu L, Shi Y, Liu B, et al. Expression of lncRNA-HOTAIR in the serum of patients with lymph node metastasis of papillary thyroid carcinoma and its impact. Oncol Lett. 2020;20(1):907–913. doi:10.3892/ol.2020.11620
19. Huang T, Huang P-T, Luo Z-Y, et al. Use superb microvascular imaging to diagnose and predict metastatic cervical lymph nodes in patients with papillary thyroid carcinoma. J Cancer Res Clin Oncol. 2024;150(5):268. doi:10.1007/s00432-024-05770-x
20. Li T, Kang G, Wang T, et al. Tumor angiogenesis and anti-angiogenic gene therapy for cancer. Oncol Lett. 2018;16(1):687–702. doi:10.3892/ol.2018.8733
21. Misra D, Panjwani S, Rai S, et al. Diagnostic efficacy of color Doppler ultrasound in evaluation of cervical lymphadenopathy. Dent Res J. 2016;13(3):217–224. doi:10.4103/1735-3327.182180
22. Damaševičius R Explainable artificial intelligence methods for breast cancer recognition. Innov Discov. 2024;1(3):25. doi:10.53964/id.2024025
23. Cui H, Yan R, Zhai Z, et al. Comparative analysis of 3D time-resolved contrast-enhanced magnetic resonance angiography, color Doppler ultrasound and digital subtraction angiography in symptomatic carotid stenosis. Exp Ther Med. 2018;15(2):1654–1659.
24. Wang H, Liu K, Ren J, et al. Magnetic resonance imaging characteristics of papillary thyroid carcinoma for the prediction of cervical central compartment lymph node metastasis. J Comput Assist Tomogr. 2019;43(6):963–969. doi:10.1097/RCT.0000000000000883
25. Wang P, Chen J, Zhao W Overview of early detection for breast cancer: current status and future perspectives. J Mod Med Oncol. 2023;3:10. doi:10.53964/jmmo.2023010
26. Iqbal MA, Wang X, Guoliang Z, et al. A comparison of the efficiency of diagnostic ultrasound and magnetic resonance imaging of cervical lymph nodes in papillary thyroid carcinoma. J Xray Sci Technol. 2021;29(6):1033–1044. doi:10.3233/XST-210927
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


