Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 18
Exploring Causal Relationships Between Gut Microbiota, Inflammatory Cytokines, and Inflammatory Dermatoses: A Mendelian Randomization Study
Authors Huang Z, Lu T, Lin J, Ding Q, Li X, Lin L
Received 13 September 2024
Accepted for publication 16 January 2025
Published 13 March 2025 Volume 2025:18 Pages 579—592
DOI https://doi.org/10.2147/CCID.S496091
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Carlos A. Torres-Cabala
Zirui Huang, Tao Lu, Jiahua Lin, Qike Ding, Xiaoting Li, Lihong Lin
Department of Dermatology, First Affiliated Hospital of Shantou University Medical College, Shantou, Guangdong, People’s Republic of China
Correspondence: Tao Lu, Email [email protected]
Background: Some studies have established a link between gut microbiota, inflammatory proteins, and inflammatory dermatoses. However, the mediating role of inflammatory proteins in the gut-skin axis remains unclear.
Methods: Data on inflammatory proteins and gut microbiota were drawn from the GWAS catalog and MiBioGen consortium, with inflammatory skin disease data provided by the FinnGen consortium. Using genome-wide association studies (GWAS), we performed linkage disequilibrium score regression (LDSC) to assess genetic correlations and conducted a two-step Mendelian Randomization (MR) analysis to investigate circulating inflammatory proteins as potential mediators between gut microbiota and inflammatory dermatoses.
Results: MR analysis identified 38 gut microbiota and 23 inflammatory proteins associated with inflammatory skin diseases. After false discovery rate (FDR) correction, four gut microbiota taxa—Eubacterium fissicatena, Bacteroidaceae, Allisonella, and Bacteroides, remained statistically significant (OR = 1.32, 95% CI: 1.16– 1.50, adjusted P = 0.007; OR = 2.25, 95% CI: 1.48– 3.42, adjusted P = 0.026; OR = 1.42, 95% CI: 1.18– 1.70, adjusted P = 0.014; OR = 2.25, 95% CI: 1.48– 3.42, adjusted P = 0.013), with only IL-18R1 significantly associated with eczema (OR = 1.05, 95% CI: 1.03– 1.08, adjusted P = 0.017). Further mediation analysis showed that IL-15RA mediated 11% of the pathway between Veillonellaceae and eczema, while FGF19 mediated 6% of the pathway between genus LachnospiraceaeUCG001 and psoriatic arthritis.
Conclusion: These findings provide potential targets for therapeutic interventions in inflammatory skin diseases.
Keywords: gut microbiota, inflammatory dermatoses, Mendelian randomization, inflammatory proteins, genetic correlation
Introduction
Inflammatory skin diseases encompass a broad spectrum of dermatological conditions, primarily characterized by skin inflammation that manifests as redness, swelling, pain, and itching. These conditions may arise from dysregulated immune responses, genetic predispositions, environmental triggers, infections, or allergic reactions.1 Furthermore, patients with moderate to severe psoriasis are reported to have an increased risk of developing metabolic syndrome and atherosclerotic cardiovascular disease.2,3
The gut-skin axis, proposed in recent years, has highlighted the relationship between gut microbiota and skin disorders.4 Clinical studies have demonstrated a decreased Firmicutes/Bacteroidetes ratio in patients with acne, characterized by a lower abundance of Firmicutes and a higher abundance of Bacteroidetes compared to healthy controls.4,5 Similarly, patients with psoriatic arthritis show reduced levels of Akkermansia and Ruminococcus.6,7 Additionally, a lower abundance of Ruminococcaceae has been observed in patients with eczema and acne.5,8 These discoveries all suggest a potential causal relationship between gut microbiota and inflammatory skin diseases.
Pathological activation of the immune system results in the accumulation of immune cells and the release of inflammatory proteins, such as interleukins, chemokines, and growth factors. These processes can activate specific inflammatory pathways, leading to the development of inflammatory skin disorders. For instance, the TNF-α/IL-23/IL-17 pathway plays a central role in maintaining psoriasis, while an imbalance in TH2 responses is key to the pathogenesis of atopic dermatitis (AD), alongside contributions from Th22, Th17/IL-23, and Th1-regulated pathways.9 Among these inflammatory mediators, IL-18 promotes Th1-mediated responses, with elevated IL-18R expression detected in the lesioned skin of patients with psoriasis, eczema, and AD.10 Similarly, high expression of FGF19 has been observed in the lesioned skin of psoriasis patients, suggesting its role in disease progression.11 IL-15RA, essential for T-cell regulation, is significantly upregulated in patients with rheumatoid arthritis (RA), highlighting its broader involvement in inflammatory pathways.12 Additionally, increased serum levels of CCL-4 have been reported in patients with AD and psoriasis compared to healthy individuals.13 Given the critical role of these inflammatory pathways, targeting cytokines such as IL-18, FGF19, IL-15RA, and chemokines like CCL-4 has become a promising therapeutic strategy.
Extensive research has shown that the gut microbiota plays a crucial role in regulating the inflammatory response. Imbalance in gut microbiota leads to overgrowth and release of bacterial products like lipopolysaccharides and peptidoglycans, causing inflammation.14 Recent research has shown a correlation between gut microbiota and IL-2R, which plays a contributory role in the inflammation of psoriasis.9 Additionally, Fusicatenibacter can induce IL-10 in intestinal mucosa to exert anti-inflammatory effects, potentially modulating systemic inflammation.15 Conversely, a reduced abundance of Fusicatenibacter has been reported in rheumatoid arthritis, suggesting there was a association between gut microbiota, cytokines, and inflammatory diseases.16 However, due to the observational studies being easily affected by some confounding bias, such as sample size of patients, environment, and age, the conclusions have varied in different studies. For instance, one study showed lower microbial diversity in psoriasis patients, while another showed no significant difference.17 Additionally, it is difficult to infer causality between gut microbiota/inflammatory proteins and inflammatory dermatoses from observational studies. Furthermore, it is not clear whether inflammatory proteins act as mediators in the pathway from gut microbiota to inflammatory skin diseases.
GWAS has identified numerous human genetic variants linked to various diseases by examining correlations between millions of genetic variations and disease outcomes. By using genetic variations as instrumental variables (IVs), MR infers causal relationships between exposures and outcomes.18 Moreover, bidirectional MR effectively mitigates confounding biases in traditional epidemiological studies and ascertains directional causality between interconnected phenotypes. This study employs MR analysis to investigate whether specific inflammatory proteins, particularly IL-15RA and IL-18R1, mediate the connection between gut microbiota and inflammatory dermatoses. The findings aim to provide a foundation for developing future treatment strategies targeting both gut microbiota and inflammatory pathways.
Methods
Study Design
Based on GWAS summary data, we conducted a two-step MR-analysis in order to examine the role of circulating inflammatory proteins as potential mediators in the association between intestinal microbiota and six inflammatory skin diseases including acne, allergic contact dermatitis, eczema, psoriasis vulgaris, psoriatic arthritis and seborrheic dermatitis. Moreover, we employed LDSC and reverse two-sample MR to figure out the genetic correlation and reverse causal link between the gut microbiota and inflammatory proteins in relation to inflammatory diseases. More details are shown in Figure 1. Our study followed the STROBE-MR reporting guidelines and no ethical approval was required.19
 |
Figure 1 Study design. Abbreviations: LDSC, linkage disequilibrium score regression; SNP, single nucleotide polymorphisms; MR,Mendelian randomization. |
Data Source
GWAS summary data for gut microbiota was obtained from the MiBioGen consortium, which encompassed 18,340 participants across 24 cohorts from 11 countries. It is worth noting that the majority of participants (N=13,266) had European ancestry. The MiBioGen research team conducted 16s ribosomal RNA gene sequencing for all participants to identify and categorize the gut microbiota into five distinct categories: phylum, class, order, family, and genus.20 Inflammatory proteins came from a recent study and was measured using the Olink Target Inflammation panel, composed of 91 inflammatory proteins,21 and genome-wide genetic data from 11 cohorts consisting of 293,646 individuals (6509 cases and 287,137 controls) who were all European.
The GWAS summary statistics for psoriatic arthritis were sourced from the IEU Open GWAS project (GWAS ID: ieu-b-5116, n case = 5065, n control = 21,286; https://gwas.mrcieu.ac.uk/).22 As for other inflammatory diseases, they could all be obtained in the FinnGen consortium (https://www.finngen.fi/en/access_results), in which participants were screened according to International Classification of Diseases diagnosis codes. We obtained GWAS summary data in the FinnGen biobank for psoriasis vulgaris, which included 5,018 cases and 330,975 controls, while we also drew on GWAS summary data for acne, which involved 2313 cases and 328,747 controls. In addition, we extracted GWAS summary data for seborrheic dermatitis (n case = 2949, n control = 367,046), allergic contact dermatitis (n case = 3846, n control = 306,909), and eczema (n case = 30,359, n control = 278,795) in the FinnGen consortium. More details are shown in Table S1.
Instrumental Variables (IVs)
In our study, we used specific criteria to select IVs for MR analysis with single nucleotide polymorphisms (SNPs). (1) Correlation with exposure: SNPs had to show a significant correlation with gut microbiota, with a p-value less than 5×10^-8. Due to limited SNPs meeting this, a p-value threshold of 1×10^-5 was used for gut microbiota and 5×10^-6 for inflammatory proteins.23,24 (2) Linkage disequilibrium (LD) removal: a clumping procedure was performed to remove LD, using an R^2 threshold of 0.001 and a window size of 10,000 kb. (3) Robustness assessment: the association between IVs and exposures was evaluated using the F statistic, calculated as F = β2/se2. SNPs with an F value below 10 were excluded to minimize biases. (4) Association with outcome check: SNPs selected were examined in LDlink to identify any associations with the outcome. SNPs related to the outcome were excluded to avoid potential pleiotropy. These criteria were implemented to ensure the reliability of our MR analysis.
Statistical Analysis
Genetic Correlation Analysis
Conducting genetic correlation analysis through LDSC solely based on aggregated summary statistics from GWAS, incorporating all SNPs in the analysis, enables us to mitigate any bias from sample overlap. In univariate LDSC, performing regression analysis between the chi-square statistics of GWAS and LD scores enables the estimation of SNP-based liability-scale heritability (h2) of data in every GWAS summary.25 By conducting regression analysis between the product of z-scores from two studies and LD scores, the genetic covariance can be calculated. Genetic correlation (rg) can be obtained by standardizing the genetic covariance using SNP-heritability.26 In addition, in accordance with HapMap3 ref, SNPs meeting the following criteria were selectively eliminated from the GWAS summary data. The criteria were: (1) variants was not SNPs like indel, (2) SNPs were repeating and ambiguous (3) if providing MAF, SNPs with MAF<0.01 would be excluded.27
Mendelian Randomization Analysis
Primary Analysis
To investigate the causal link between gut microbiota/inflammatory proteins and inflammatory skin diseases, we primarily employed the inverse variance weight (IVW) method, supplemented by MR-Egger, weighted median, simple mode, and weighted mode methods.28 In MR studies, the IVW method is the main tool for estimating causal effects, providing higher statistical power for hypothesis testing. It integrates Wald estimates for each SNP through a meta-analytic approach to evaluate the effects of gut microbiota and inflammatory proteins on inflammatory diseases. During regression analysis, the intercept term is omitted, and the inverse variance (se2) of the outcome serves as a weighting factor. Results are unbiased in the absence of horizontal heterogeneity.29 MR-Egger regression operates on the premise that the instrumental variable’s strength is not influenced by direct effects. It identifies and adjusts for causal relationships between IVs and outcomes. If the intercept is close to zero, indicating no horizontal pleiotropy, MR-Egger findings closely match those from IVW.30 Furthermore, we conducted reverse two-sample MR analysis to figure out the causal relationship from inflammatory diseases to gut microbiota and inflammatory proteins. It is noteworthy that the three categories of gut microbial taxa (the Verrucomicrobiae class, the Verrucomicrobiales order, and the Verrucomicrobiae family) are identical. Consequently, we have chosen to retain only the results pertaining to the Verrucomicrobiae family.
Mediation Analysis
After carrying out MR analysis from gut microbiota and inflammatory proteins to inflammatory diseases, we further explored the causal relationship of gut microbiota to inflammatory proteins that exerted large significant differences with inflammatory diseases. In the presence of a significant difference between gut microbiota and inflammatory proteins, MVMR analysis was conducted to investigate whether inflammatory proteins act as mediators in the path from gut microbiota to inflammatory diseases. It is worth noting that in two-sample MR analysis, the impact of gut microbiota on inflammatory diseases was characterized as the “total effect” (β1), whereas in MVMR, it is referred to as the “direct effect” (β2). In addition, the effect of inflammatory proteins on inflammatory diseases in MVMR analysis was defined as β3, while the influence exerted by gut microbiota on inflammatory proteins in two-sample MR analysis was labeled as β4. The mediating effect could be calculated as β3*β4, and the mediated ratio could be quantified by (β3*β4)/β1.31 Confidence intervals (95% CI) and odds ratios were estimated by the delta method. In addition, the Sobel test was utilized to assess the significance of mediator.
Sensitivity Analysis
Cochran’s Q test was utilized to evaluate the presence of heterogeneity among IVW IVs. Heterogeneity is considered to be present if the p-value is below 0.05. In addition, the random-effects IVW model is employed in the presence of heterogeneity (P < 0.05), while the fixed-effects IVW model is used when there is no heterogeneity (P > 0.05)32. To identify the presence of pleiotropy among SNPs, we employed the MR-Egger intercept with a p-value below 0.05 as an indicator of noteworthy pleiotropic effects.30 By employing the MR pleiotropy residual sum and outlier (MR-PRESSO) methodology, we detected outliers and evaluated the robustness of our analysis to examine the existence of horizontal pleiotropy. Through the identification and removal of such outliers, we obtained refined estimates that accounted for their influence. Moreover, to ensure the reliability of our analysis, leave-one-out analysis was carried out.33
To enable our results to be more rigorous, differences were considered significant if the p-value was still less than 0.05 after conducting the Benjamin−Hochberg procedure (FDR) in LDSC and MR analysis. In addition, it was represented as a suggestive association when p-values were less than 0.05 and the FDR-corrected p-value was above 0.05.34 The MR analysis performed in this study was executed utilizing the R software (version 4.2.3), employing the two-sample package (version 0.5.9), and MR-PRESSO (version 1) for the analysis.
Results
Genetic Correlation Analysis
LDSC regression analysis was utilized to elucidate the genetic correlations between 196 gut microbiota and inflammatory diseases, as well as between 91 inflammatory proteins and these diseases. Owing to the incomputable negative heritability in LDSC, only 135 gut microbiota and 87 inflammatory proteins were included in the LDSC analysis. Based on univariate LDSC the heritability (h2) of SNPs in 135 gut microbiota and 87 inflammatory proteins was estimated to range from 0.0006 to 0.21 in microbiota and 0.004 to 0.19 in inflammatory proteins (Tables S2 and S3). The results which were with significant difference between gut microbiota/inflammatory proteins and inflammatory diseases were shown in Table 1 and Table 2. It was worth noting that after conducting FDR correction, 4 cytokines still remained significantly associated with acne. DNER, IL-1 alpha, IL 20 and PD-L1 were all associated with higher risk of developing acne (rg = 0.63, P = 0.003, adjusted P = 0.034; rg = 1.12, P = 0.001, adjusted P = 0.033; rg = 1.08, P = 0.0001, adjusted P = 0.005; rg = 0.66, P = 0.002, adjusted P = 0.034).
 |
Table 1 Genetic Correlation Between Gut Microbiota and Inflammatory Dermatoses |
 |
Table 2 Genetic Correlation Between Inflammatory Proteins and Inflammatory Dermatoses |
Mendelian Randomization
According to the criteria of screening, 2559 SNPs were selected as IVs for 196 gut microbiota and 1819 SNPs were chosen as IVs for inflammatory proteins. As shown in Figures 2 and 3, we found that 11, 8, 3, 4, 8, and 5 gut microbiota had a significant causal effect on acne, allergic contact dermatitis, eczema, psoriasis, psoriatic arthritis, and seborrheic dermatitis, respectively, while 2, 5, 5, 6, 5, and 5 inflammatory proteins were associated with these conditions respectively. The results of the estimates of causal associations between 196 gut microbiota/inflammatory proteins and inflammatory diseases are presented in Tables S3–S7. It is noteworthy that, following FDR correction, four gut microbiota remained statistically significant. In the MR analysis linking gut microbiota to psoriasis vulgaris, the genus Eubacterium fissicatena group remained significantly associated with an increased risk of developing psoriasis vulgaris (OR = 1.32, 95% CI: 1.16–1.50, P = 0.00004, adjusted P = 0.007). Additionally, family Bacteroidaceae, genus Allisonella and genus Bacteroides were identified as significant risk factors for acne (OR = 2.25, 95% CI: 1.48–3.42, P = 0.0001, adjusted P = 0.026; OR = 1.42, 95% CI: 1.18–1.70, P = 0.0002, adjusted P = 0.014; OR = 2.25, 95% CI: 1.48–3.42, P = 0.0001, adjusted P = 0.013). Moreover, IL-18R1 remained significantly related to eczema after FDR correction (OR = 1.05, 95% CI: 1.03–1.08, P = 0.0002, adjusted P = 0.017).
 |
Figure 2 Forest plot of significant effects between gut microbiota and inflammatory dermatoses, using the IVW method. |
Mediation Analysis
Following MR analysis of gut microbiota and inflammatory proteins to inflammatory diseases, we explored the causal relationships between gut microbiota and inflammatory proteins. These gut microbiota and inflammatory proteins put into this MR analysis were all associated with inflammatory diseases with significant differences respectively (Figure 4 and Table S8). Subsequently, we carried out MVMR analysis to figure out whether inflammatory proteins acted as mediators from gut microbiota to inflammatory skin diseases (Table 3). After entering IL-15RA into MVMR to assess the correlation of family Veillonellaceae to eczema, the correlation still remained statistically significant, and the mediating effect was calculated as −0.008 (OR = 0.992, 95% CI: 0.984–0.998) while the mediating proportion was 11%. Similarly, entering FGF19 into MVMR analysis, for class Actinobacteria and genus LachnospiraceaeUCG001 to psoriatic arthritis, still showed significant differences from FGF19 to psoriatic arthritis in two pathways, respectively, with a mediating effect of −0.026 and −0.024 (OR = 0.974, 95% CI: 0.934–1.001; OR = 0.976, 95% CI: 0.944–0.998). In addition, after conducting the Sobel test, only IL-15RA as a mediator from family Veillonellaceae for eczema, and FGF19 as a mediator from genus LachnospiraceaeUCG001 for psoriatic arthritis remained statistically significant. For other inflammatory proteins, after MVMR analysis, no intermediary effect was shown.
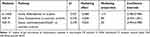 |
Table 3 Mediating Analysis From Gut Microbiota to Inflammatory Dermatoses |
Sensitivity Analysis
Heterogeneity existed between TNFB and acne (P = 0.041) while heterogeneity was found between CCL20 and eczema through Cochran’s Q test (Figure 4). Hence, a random-effects IVW model was applied when heterogeneity existed. Except for the results mentioned above, there was no heterogeneity found in the remaining results. According to MR-Egger intercept regression analysis and MR-PRESSO, there was no significant horizontal pleiotropy in our study (Tables S9–S11).
Reverse Causality Analysis
In the reverse MR analysis, we selected inflammatory skin diseases as the exposure and 196 gut microbiota and 91 inflammatory proteins as the outcomes. As shown in Figure 4, we found a bidirectional relationship between the genus Odoribacter and psoriasis vulgaris (OR = 1.03, 95% CI: 1.00–1.06, P = 0.028). Regarding inflammatory proteins, acne was associated with a decreased risk of TNFB (OR = 0.95, 95% CI: 0.91–0.99, P = 0.007), while allergic contact dermatitis was linked to an increased risk of CCL-19 (OR = 1.11, 95% CI: 1.03–1.20, P = 0.008). Additionally, psoriasis vulgaris was associated with a decreased risk of IL-18R1 (OR = 0.98, 95% CI: 0.96–1.00, P = 0.027). Except for heterogeneity detected between TNFB and allergic contact dermatitis, no heterogeneity or horizontal pleiotropy was detected based on Cochran’s Q test and MR-Egger. More details are shown in Tables S12–S15.
Discussion
To our knowledge, this is the first study to use two-step MR analysis to explore whether inflammatory proteins mediate the pathway from gut microbiota to inflammatory dermatoses. Based on GWAS data, we identified suggestive associations and estimated genetic correlations between gut microbiota, inflammatory proteins, and inflammatory dermatoses. The lack of overlap between LDSC regression analysis and MR analysis indicates that the findings from MR analysis are independent of shared genetic components. Furthermore, MVMR analysis identified IL-15RA and FGF-19 as mediators. This study pioneers the causal investigation of how gut microbes and cytokines interact to influence inflammatory skin diseases, providing the first genetic-level evidence of cytokine mediation from gut microbiota to these conditions.
As part of the gut-skin axis, extensive research has highlighted the critical role of gut microbiota in skin disorders. Dysbiosis, or an imbalance in microbiota diversity, is considered one of the key underlying causes of inflammatory skin diseases. It enhances host susceptibility, disrupts mucosal immune tolerance, and directly influences neurotransmitter production or modulates neurotransmitter metabolism pathways, ultimately impacting skin health.35 Although previous observational studies have noted significant differences in microbiota diversity in patients with skin disorders, causality remains unclear due to the limitations of observational research. In contrast, MR analysis, based on genetic variations, is less affected by confounding factors and allows for causal inferences between gut microbiota and inflammatory skin disorders.
Previous observational studies have suggested a reduced abundance of Ruminococcaceae in patients with eczema and acne,5,8 indicating a potential association with disease pathogenesis. However, these studies could not establish causality. In contrast, our MR-based findings provide robust genetic evidence that Ruminococcaceae exerts a causal, protective effect against allergic contact dermatitis, psoriasis vulgaris, and seborrheic dermatitis. In addition to Ruminococcaceae, our study identifies several microbiota, such as LachnospiraceaeUCG001 and Bifidobacterium, as protective factors against inflammatory dermatoses. These protective microbes commonly produce short-chain fatty acids (SCFAs), such as acetate, propionate, and butyrate, which travel from the gut to the skin and can modulate local immune responses.36 Thus, Ruminococcaceae may confer protection by modulating immune responses via SCFA production. SCFAs enhance innate immune cell function, potentially improving the skin’s defense against inflammation. They also shape adaptive immunity by influencing T and B cell differentiation.36 Accordingly, interventions that increase SCFA levels—either through microbiota manipulation or direct supplementation, may offer therapeutic potential. Another study linked Veillonellaceae enrichment with higher propionate levels in patients with Glycogen Storage Disease, suggesting that Veillonellaceae may regulate inflammation via SCFA modulation.37 Consistent with these findings, we show that Veillonellaceae is associated with reduced eczema risk, reinforcing its potential anti-inflammatory role. Furthermore, our MR analysis reveals that Bifidobacterium is associated with a reduced risk of acne. By enhancing tryptophan levels and its metabolites, Bifidobacterium may help maintain intestinal barrier integrity and alleviate acne-related inflammation.38 These findings strengthen the hypothesis that Bifidobacterium plays a causal role in the prevention of inflammatory dermatoses.
Moreover, our study identifies several bacteria, including Fusicatenibacter, Flavonifractor, and Odoribacter, as potentially protective factors against inflammatory dermatoses, possibly through their interaction with circulating inflammatory cytokines. Flavonifractor prausnitzii is a well-known microbial marker for various inflammatory conditions, such as psoriasis and AD.39 Elevated Flavonifractor abundance has been observed in moderate-severe AD and bullous pemphigoid, suggesting a pattern of involvement across different conditions.40,41 Correlations between Flavonifractor and multiple inflammatory markers further implicate it in immune dysregulation. Additionally, Fusicatenibacter and Odoribacter have shown the ability to induce regulatory pathways such as IL-10 production and regulatory T cell enhancement that could help maintain immune balance.15,16,42 These findings suggest that beyond traditionally studied taxa, a broader range of gut microbes may contribute to modulating immune responses in the skin. Our study also identified gut microbiota genera Erysipelatoclostridium, Anaerostipes, Eggerthella, and Eisenbergiella to be associated with inflammatory skin diseases. However, related research is limited and requires more exploration.
Our MR analysis reveals a causal relationship between IL-18R1 and the increased risk of allergic contact dermatitis, eczema, and psoriasis vulgaris, supporting prior findings. IL-18R is expressed on various immune cells such as Th1, NK, and mast cells, suggesting a broad immunomodulatory function.43 Higher IL-18R expression in lesional skin compared to healthy skin may explain its role in driving these inflammatory processes.10 Similarly, IL-6 shows a causal link with conditions such as allergic contact dermatitis and psoriasis vulgaris. IL-6, a pleiotropic cytokine, correlates with psoriasis severity, consistent with our causal inference. Moreover, IL-6-driven mononuclear cell infiltration likely sustains inflammation in contact dermatitis.44
Our MR analysis shows that FGF19 reduces the risk of acne and psoriatic arthritis, suggesting a protective effect. As a member of the fibroblast growth factor family, FGF19 influences immune responses and keratinocyte biology. Although its role in acne remains unclear, previous studies have reported elevated FGF19 expression in lesioned skin of psoriasis patients, suggesting that it may be involved in inflammation regulation.11 Thus, FGF19 may maintain immune balance and keratinocyte homeostasis, potentially slowing disease progression. Our study also identified several chemokines, such as CCL-20, as protective factors for inflammation. However, given the limited research available, further studies are needed to investigate this relationship in greater detail.
Our study provides genetic evidence that IL-15RA and FGF19 act as mediators in the pathway from gut microbiota to inflammatory diseases. Specifically, IL-15RA mediated the effect of Veillonellaceae on eczema, while FGF19 mediated the association between Actinobacteria, LachnospiraceaeUCG001, and psoriatic arthritis. IL-15RA, a high-affinity α chain that forms a trimeric receptor complex with IL-2Rβ and IL-2Rγ, triggers downstream signaling pathways such as MAPKs and promotes the secretion of proinflammatory cytokines, including IL-6, IL-8, and TNF-α.12 While previous studies have observed elevated IL-15RA expression in RA, its role in eczema has not been previously explored.12 Notably, a mouse model has shown exacerbated allergic inflammation due to IL-15 deficiency, which may relate to eczema pathogenesis.45 Identifying IL-15RA as a mediator offers new insight into eczema pathogenesis and suggests a potential therapeutic target. For psoriatic arthritis, FGF19 mediated the association between Actinobacteria and LachnospiraceaeUCG001 with disease risk. Elevated FGF19 levels in psoriatic lesions suggest its involvement in keratinocyte regulation and inflammatory processes.11 However, the mediating effect was relatively modest, implying that gut microbiota may regulate inflammatory skin disorders through additional pathways. These microbial taxa produce SCFAs, which reduce proinflammatory cytokines and influence circulating metabolites, thereby shaping immune responses in the skin. SCFAs, particularly butyrate, have been shown to control the differentiation and function of mucosal Tregs. Dysregulation of Treg cells or an imbalance in cytokines, particularly elevated pro-inflammatory cytokines like IL-6 and IL-17, can contribute to the onset and progression of inflammatory dermatosis.46 These findings underscore the importance of gut microbiota and their metabolites in modulating immune responses in inflammatory dermatoses.
Strengths and Limitations
Our research offers several key advantages. First, this is the first study to investigate the genetic correlation by LDSC analysis and causal relationship by MR analysis between gut microbiota, inflammatory proteins, and inflammatory dermatoses, such as acne, allergic contact dermatitis, eczema, psoriasis vulgaris, psoriatic arthritis and seborrheic dermatitis. We also figured out, through two-step MR, whether inflammatory proteins serve as mediators in the pathway from gut microbiota to inflammatory skin disorders, which provides genetic evidence for further treatment targeting gut microbiota or cytokines. In addition, our investigation was conducted based on robust methodology by leveraging GWAS and MR, which minimizes confounding biases relative to traditional studies. Furthermore, our research employs a comprehensive methodology to ensure result reliability. Sensitivity analyses were performed, utilizing Cochran’s Q test to assess heterogeneity, MR-Egger intercept and MR-PRESSO to detect horizontal pleiotropy.
Despite its strengths, our research also has some limitations. First, since the GWAS data primarily originates from European populations, the findings may not be generalizable to other ethnicities. Secondly, although MR analysis helps infer causal relationships, it can not completely eliminate all confounding variables. While MR analysis serves as a hypothesis-driven approach, it necessitates experimental and clinical studies to confirm the causal relationship between gut microbiota/inflammatory proteins and inflammatory dermatoses. Additionally, this study relies on cross-sectional genetic data, which limits the ability to capture dynamic changes in gut microbiota or cytokine levels over time. Longitudinal studies are required to better understand the temporal interactions between these factors and their influence on the progression of inflammatory skin diseases. Finally, although we identified IL-15RA and FGF19 as mediators, their mediating proportions were relatively modest, suggesting that additional pathways or mechanisms may play significant roles in the gut-skin axis.
Conclusion
As far as we know, this is the first study to examine whether inflammatory proteins mediate the pathway from gut microbiota to inflammatory dermatoses using a two-step MR analysis. Drawing from GWAS data, we identified IL-15RA and FGF19 as mediators, providing novel insights into the gut-skin axis and its potential therapeutic targets. Despite modest mediating effects, these findings highlight the complexity of the gut-skin axis and suggest additional unexplored pathways. Future research with diverse populations and longitudinal data is needed to validate and expand these results. This study provides a foundation for developing microbiota-based or cytokine-targeted therapies, offering new directions for treating inflammatory skin diseases.
Data Sharing Statement
The genome-wide association study (GWAS) data for inflammatory proteins is accessible through the GWAS catalog, while gut microbiota data is available from the MiBioGen consortium. Information on inflammatory skin disorders can be obtained via the FinnGen consortium. Code used in the analysis are available at https://github.com/.
Consent for Publication
Not required.
Consent to Participate
Not required.
Ethical Approval
According to Article 32 of the “Measures for the Ethical Review of Life Science and Medical Research Involving Humans” (National Health Commission [2023] No. 4), research using anonymized, publicly available data is exempt from ethical review, provided it does not involve sensitive personal information or individual-level interventions. This study exclusively utilizes anonymized public data, with no individual-level interventions, and complies with relevant regulations. Therefore, it qualifies for exemption from ethical review. The data source and anonymization process have been clearly stated for transparency and compliance.
Acknowledgments
We sincerely thank all the researchers who have generously shared their GWAS data. See Supplementary for Abbreviations list.
Funding
This study did not receive specific funding.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Liu TJ, Lin LL, McMeniman E. et al. Cytokine/Chemokine assessment as a complementary diagnostic tool for inflammatory skin diseases. Front Immunol. 2022;13:1028435. doi:10.3389/fimmu.2022.1028435
2. Wu JJ, Kavanaugh A, Lebwohl MG, Gniadecki R, Merola JF. Psoriasis and metabolic syndrome: implications for the management and treatment of psoriasis. J Eur Acad Dermatol Venereol. 2022;36(6):797–806. doi:10.1111/jdv.18044
3. Masson W, Lobo M, Molinero G. Psoriasis and cardiovascular risk: a comprehensive review. Adv Ther. 2020;37(5):2017–2033. doi:10.1007/s12325-020-01346-6
4. Mahmud MR, Akter S, Tamanna SK, et al. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022;14(1):2096995. doi:10.1080/19490976.2022.2096995
5. Deng Y, Wang H, Zhou J, Mou Y, Wang G, Xiong X. Patients with acne vulgaris have a distinct gut microbiota in comparison with healthy controls. Acta Derm Venereol. 2018;98(8):783–790. doi:10.2340/00015555-2968
6. Olejniczak-Staruch I, Ciążyńska M, Sobolewska-Sztychny D, Narbutt J, Skibińska M, Lesiak A. Alterations of the skin and gut microbiome in psoriasis and psoriatic arthritis. Int J mol Sci. 2021;22(8):3998. doi:10.3390/ijms22083998
7. Scher JU, Ubeda C, Artacho A, et al. Decreased bacterial diversity characterizes the altered gut microbiota in patients with psoriatic arthritis, resembling dysbiosis in inflammatory bowel disease. ARTHRITIS RHEUMATOL. 2015;67(1):128–139. doi:10.1002/art.38892
8. West CE, Rydén P, Lundin D, Engstrand L, Tulic MK, Prescott SL. Gut microbiome and innate immune response patterns in IgE-associated eczema. Clin Exp Allergy. 2015;45(9):1419–1429. doi:10.1111/cea.12566
9. Zhang X, Shi L, Sun T, Guo K, Geng S. Dysbiosis of gut microbiota and its correlation with dysregulation of cytokines in psoriasis patients. BMC Microbiol. 2021;21(1):78. doi:10.1186/s12866-021-02125-1
10. Wittmann M, Purwar R, Hartmann C, Gutzmer R, Werfel T. Human keratinocytes respond to interleukin-18: implication for the course of chronic inflammatory skin diseases. J Invest Dermatol. 2005;124(6):1225–1233. doi:10.1111/j.0022-202X.2005.23715.x
11. Yu X, Yan N, Li Z, Hua Y, Chen W. FGF19 sustains the high proliferative ability of keratinocytes in psoriasis through the regulation of Wnt/GSK-3β/β-catenin signalling via FGFR4. Clin Exp Pharmacol Physiol. 2019;46(8):761–769. doi:10.1111/1440-1681.13103
12. Machado Diaz AC, Chico Capote A, Arrieta Aguero CA, et al. Proinflammatory soluble interleukin-15 receptor alpha is increased i n rheumatoid arthritis. Arthritis. 2012;2012:943156. doi:10.1155/2012/943156
13. Purzycka-Bohdan D, Nedoszytko B, Zabłotna M, Gleń J, Szczerkowska-Dobosz A, Nowicki RJ. Chemokine profile in psoriasis patients in correlation with disease severity and pruritus. Int J mol Sci. 2022;23(21):13330. doi:10.3390/ijms232113330
14. Li F, Wang M, Wang J, Li R, Zhang Y. Alterations to the gut microbiota and their correlation with inflammatory factors in chronic kidney disease. Front Cell Infect Microbiol. 2019;9:206. doi:10.3389/fcimb.2019.00206
15. Zhou MS, Zhang B, Gao ZL, et al. Altered diversity and composition of gut microbiota in patients with allergic rhinitis. Microb Pathog. 2021;161(Pt A):105272. doi:10.1016/j.micpath.2021.105272
16. Yu D, Du J, Pu X, et al. The gut microbiome and metabolites are altered and interrelated in patients with rheumatoid arthritis. Front Cell Infect Microbiol. 2022;11:763507. doi:10.3389/fcimb.2021.763507
17. Polak K, Bergler-Czop B, Szczepanek M, Wojciechowska K, Frątczak A, Kiss N. Psoriasis and gut microbiome-current state of art. Int J mol Sci. 2021;22(9):4529. doi:10.3390/ijms22094529
18. Tam V, Patel N, Turcotte M, Bosse Y, Pare G, Meyre D. Benefits and limitations of genome-wide association studies. Nat Rev Genet. 2019;20(8):467–484. doi:10.1038/s41576-019-0127-1
19. Skrivankova VW, Richmond RC, Woolf BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: the STROBE-MR Statement. JAMA J Am Med Assoc. 2021;326(16):1614–1621. doi:10.1001/jama.2021.18236
20. Kurilshikov A, Medina-Gomez C, Bacigalupe R, et al. Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat Genet. 2021;53(2):156–165. doi:10.1038/s41588-020-00763-1
21. Zhao JH, Stacey D, Eriksson N, et al. Genetics of circulating inflammatory proteins identifies drivers of immune-mediated disease risk and therapeutic targets [published correction appears in Nat Immunol. 2023 Sep 7]. Nat Immunol. 2023;24(9):1540–1551. doi:10.1038/s41590-023-01588-w
22. Soomro M, Stadler M, Dand N, et al. Comparative genetic analysis of psoriatic arthritis and psoriasis for the discovery of genetic risk factors and risk prediction modeling. Arthritis Rheumatol. 2022;74(9):1535–1543. doi:10.1002/art.42154
23. Mao R, Yu Q, Li J. The causal relationship between gut microbiota and inflammatory dermatoses: a Mendelian randomization study. Front Immunol. 2023;14:1231848. doi:10.3389/fimmu.2023.1231848
24. Jiang P, Yu F, Zhou X, Shi H, He Q, Song X. Dissecting Causal Links Between Gut Microbiota, Inflammatory Cytokines, and DLBCL: a Mendelian Randomization Study. Blood Adv. 2024. doi:10.1182/bloodadvances.2023012246.
25. Bulik-Sullivan BK, Loh PR, Finucane HK, et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015;47(3):291–295. doi:10.1038/ng.3211
26. Wielscher M, Amaral AFS, van der Plaat D, et al. Genetic correlation and causal relationships between cardio-metabolic traits and lung function impairment. Genome Med. 2021;13(1):104. doi:10.1186/s13073-021-00914-x
27. Bulik-Sullivan B, Finucane HK, Anttila V, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47(11):1236–1241. doi:10.1038/ng.3406
28. Liu X, Tong X, Zou Y, et al. Mendelian randomization analyses support causal relationships between blood metabolites and the gut microbiome. Nat Genet. 2022;54(1):52–61. doi:10.1038/s41588-021-00968-y
29. Burgess S, Dudbridge F, Thompson SG. Combining information on multiple instrumental variables in Mendelian randomization: comparison of allele score and summarized data methods. Stat Med. 2016;35(11):1880–1906. doi:10.1002/sim.6835
30. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–525. doi:10.1093/ije/dyv080
31. He J, Huang M, Li N, Zha L, Yuan J. Genetic association and potential mediators between sarcopenia and coronary heart disease: a bidirectional two-sample, two-step mendelian randomization study. Nutrients. 2023;15(13):3013. doi:10.3390/nu15133013
32. Burgess S, Small DS, Thompson SG. A review of instrumental variable estimators for Mendelian randomization. Stat Methods Med Res. 2017;26(5):2333–2355. doi:10.1177/0962280215597579
33. Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–698. doi:10.1038/s41588-018-0099-7
34. Zhang Z, Cheng L, Ning D. Gut microbiota and sepsis: bidirectional Mendelian study and mediation analysis. Front Immunol. 2023;14:1234924. doi:10.3389/fimmu.2023.1234924
35. Shi YZ, Tao QF, Qin HY, Li Y, Zheng H. Causal relationship between gut microbiota and urticaria: a bidirectional two-sample mendelian randomization study. Front Microbiol. 2023;14:1189484. doi:10.3389/fmicb.2023.1189484
36. Yao Y, Cai X, Fei W, Ye Y, Zhao M, Zheng C. The role of short-chain fatty acids in immunity, inflammation and metabolism. Crit Rev Food Sci Nutr. 2022;62(1):1–12. doi:10.1080/10408398.2020.1854675
37. Ceccarani C, Bassanini G, Montanari C, et al. Proteobacteria overgrowth and butyrate-producing taxa depletion in the gut microbiota of glycogen storage disease type 1 patients. Metabolites. 2020;10(4):133. doi:10.3390/metabo10040133
38. Jung GW, Tse JE, Guiha I, Rao J. Prospective, randomized, open-label trial comparing the safety, efficacy, and tolerability of an acne treatment regimen with and without a probiotic supplement and minocycline in subjects with mild to moderate acne. J Cutaneous Med Surg. 2013;17(2):114–122. doi:10.2310/7750.2012.12026
39. Huang S, Mao J, Zhou L, Xiong X, Deng Y. The imbalance of gut microbiota and its correlation with plasma inflammatory cytokines in pemphigus vulgaris patients. Scandinavian J Immunol. 2019;90(3):e12799. doi:10.1111/sji.12799
40. Wang Y, Hou J, Tsui JC, et al. Unique gut microbiome signatures among adult patients with moderate to severe atopic dermatitis in southern Chinese. Int J mol Sci. 2023;24(16):12856. doi:10.3390/ijms241612856
41. Liu X, van Beek N, Cepic A, et al. The gut microbiome in bullous pemphigoid: implications of the gut-skin axis for disease susceptibility. Front Immunol. 2023;14:1212551. doi:10.3389/fimmu.2023.1212551
42. Lima SF, Gogokhia L, Viladomiu M, et al. Transferable immunoglobulin a-coated odoribacter splanchnicus in responders to fecal microbiota transplantation for ulcerative colitis limits colonic inflammation. Gastroenterology. 2022;162(1):166–178. doi:10.1053/j.gastro.2021.09.061
43. Hu Y, Wang J, Zhang H, et al. Enhanced Expression of IL-18 and IL-18BP in plasma of patients with eczema: altered expression of IL-18BP and IL-18 receptor on mast cells. Mediators. Inflamm. 2017;2017:3090782. doi:10.1155/2017/3090782
44. Frempah B, Luckett-Chastain LR, Gallucci RM. IL-6 Negatively Regulates IL-22rα Expression on Epidermal Keratinocytes: Implications for Irritant Contact Dermatitis. J Immunol Res; 2019. Vol. 2019. 6276254. doi:10.1155/2019/6276254
45. Mathias CB, Schramm CM, Guernsey LA, et al. IL-15-deficient mice develop enhanced allergic responses to airway allergen exposure. Clin Exp Allergy. 2017;47(5):639–655. doi:10.1111/cea.12886
46. Hou T, Sun X, Zhu J, et al. IL-37 ameliorating allergic inflammation in atopic dermatitis through regulating microbiota and AMPK-mTOR signaling pathway-modulated autophagy mechanism. Front Immunol. 2020;11:752. doi:10.3389/fimmu.2020.00752
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Revealing the Impact of Gut Microbiota on Acne Through Mendelian Randomization Analysis

Ji X, Wu S, Zhao D, Bai Q, Wang Y, Gong K, Zheng H, Zhu M
Clinical, Cosmetic and Investigational Dermatology 2024, 17:383-393
Published Date: 8 February 2024
Genomics-Microbiome Based Assessment of Bidirectional Causality Between Gut Microbiota and Psoriasis
Gao Q, Liu JH, Ma WY, Cheng ZL, Hao PS, Luo NN
Clinical, Cosmetic and Investigational Dermatology 2024, 17:435-445
Published Date: 13 February 2024
The Effect of Circulating Inflammatory Proteins on Endometriosis: A Mendelian Randomization Study
Wei Y, Zhao X, Li L
ImmunoTargets and Therapy 2024, 13:585-593
Published Date: 1 November 2024
The Causal Effect Between Human Microbiota and Scabies: A Study from the Genetic Perspective
Zheng Q, Li Y, Zhu W, Xu X, Sheng G, Li L
Clinical, Cosmetic and Investigational Dermatology 2024, 17:2803-2812
Published Date: 6 December 2024
Causal Relationships Between Gut Microbiota, Metabolites, and Diabetic Nephropathy: Insights from a Two-Sample Mendelian Randomization Analysis
Song X, Cui J, Li S, Huang B
International Journal of Nephrology and Renovascular Disease 2024, 17:319-332
Published Date: 10 December 2024



