Back to Journals » Risk Management and Healthcare Policy » Volume 18
Exploring Implications of Risk Communication Strategies in Diminishing Adversities of Misinformation and Disinformation Against Hepatitis Vaccination in Global South
Authors Mehdi M , Raza SH , Yousaf M , Li B, Zaman U, Riaz S
Received 17 October 2024
Accepted for publication 14 March 2025
Published 1 April 2025 Volume 2025:18 Pages 1133—1145
DOI https://doi.org/10.2147/RMHP.S501423
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kyriakos Souliotis
Miqdad Mehdi,1 Syed Hassan Raza,2 Muhammad Yousaf,3 Bingqiang Li,1 Umer Zaman,4 Sohail Riaz5
1School of Law, Shanxi University, Taiyuan, 030006, People’s Republic of China; 2School of Media and Communication, Taylor’s University, Subang Jaya, Selangor, 47500, Malaysia; 3Centre for Media and Communication Studies, University of Gujrat, Gujrat, 50700, Pakistan; 4Endicott College of International Studies (ECIS), Woosong University, Daejeon, 34606, Korea; 5Media and Communication Studies, Comsat University Islamabad, Lahore Campus, Lahore, Pakistan
Correspondence: Miqdad Mehdi; Bingqiang Li, School of Law, Shanxi University, Taiyuan, 030006, People’s Republic of China, Tel +86 15691753163, Email [email protected]; [email protected]
Background and Purpose: Concern over the low hepatitis immunization rates is growing. It is generally believed that misinformation and disinformation are the main barriers to the success of mass immunization campaigns. This study intends to investigate the matter of online misinformation and disinformation about hepatitis vaccination and its implications.
Material and Methods: The researchers employed a cross-sectional research design vis-à-vis a web-based survey method to collect data. Data were collected from a nationally representative sample of 1931 internet users across Pakistan. Participation in the study was voluntary. Data collection continued for four months, from Mar 1, 2024, to Jun 30, 2024.
Results: The “results” of structural equation modeling show that misinformation and disinformation substantially structure risk perception regarding hepatitis, which, in turn, impacts problem recognition, involvement recognition, and constraint recognition. Besides, the outcomes uncovered that the chain of problem identification impacts situational motivation, which drives risk communication behaviors. Also, these risk communication behaviors are closely linked to individuals’ motivation to receive the hepatitis vaccine.
Conclusion: This research concludes that managing misinformation and disinformation via strategically designed, valid, and reliable digital interventions improves the public’s active response regarding willingness to get vaccinated against hepatitis. This study contributes to increasing public acceptance of the hepatitis vaccine by utilizing reliable and valid digital interventions to achieve a more active public health response.
Keywords: misinformation, disinformation, global south, hepatitis, risk communication, vaccine
Introduction
Hepatitis is a significant health issue across the globe. It affects infants and adolescents residing in underdeveloped and developing nations alike. For instance, it is found that almost 1.5 million clinical cases of hepatitis are reported worldwide annually.1 However, the infection rate is probably as much as ten times higher than the expected statistics. Vaccine hesitancy is not a new phenomenon. The WHO declared vaccine hesitancy among the top 10 threats to global health systems.2
Nevertheless, in the current age of mediated realities wherein media shapes our understandings of the social world,3,4 misinformation, and disinformation, the distrust in the efficacy and safety of vaccines has increased many-fold.5–7 It has been found that misinformation and disinformation are as dangerous as pandemics,8 and this health misinformation kills people like a pandemic.7 Media are considered an essential source of health risk-related disseminated communication.9 However, media coverage is also a source of concern regarding the acceptance of vaccines.5 Moreover, the abundance of misinformation and disinformation corresponds to distrust in health authorities and harms public health,10 affecting willingness to vaccinate against hepatitis. Therefore, misinformation and disinformation streams are a prime cause of vaccine hesitancy among the masses.10–12 Hepatitis B infection is a daunting global health challenge,13,14 and most affected continents include Asia, Africa, southern Europe, and Latin America.15
Globally, approximately 2 billion people are infected with hepatitis B,13,15–17 and 400 million among them are suffering from chronic hepatitis infection.16,18 Pakistan is highly endemic to hepatitis B,18 with about nine million people infected with hepatitis B.19 Notably, the infection rate is steadily rising in the country. The reason may be the lack of proper health facilities, poor economic status, and less public awareness about the transmission of major communicable diseases, including Hepatitis B and HIV.16 Similarly, adults in economically advanced countries also suffer from hepatitis A, and its rapid spread is of grave concern.1 For instance, its primary transmission source is the consumption of water or food contaminated by the feces of individuals who are carriers of the disease.1,14 Hepatitis A is usually characterized by low complications, a lack of chronicity, and a generally favorable prognosis.14 In the general population survey in the US, a seroprevalence rate of hepatitis A was determined to be 31.3% (9.4% for ages 6–11, and substantially higher rates were observed, ie, at 74.6% for those aged 70 and above).20 Moreover, hepatitis A is less frequently encountered in children and young adults, as previously reported, with a remarkably low seroprevalence rate in Pakistan. It is also significantly greater among adults over 40 years of age.18
Previous research conducted in the context of hepatitis has examined the impact of an individual’s knowledge and understanding of the hepatitis virus and the hepatitis vaccine on their intentions and behavior regarding hepatitis vaccination.14,18,21,22 However, these studies have only utilized limited measures of hepatitis cognition. Vaccine hesitancy, which refers to the deliberate delay or refusal of vaccination despite the availability of accessible vaccination services, poses a considerable obstacle in the management of hepatitis and other preventable diseases through vaccination.23–26 As a result, the World Health Organization (WHO) has recognized it as a significant global health issue, necessitating attention and intervention. Past research highlights that social media platforms such as Twitter, Facebook, YouTube, and Instagram substantially facilitate information’s widespread and expeditious dissemination.27 The dissemination of misinformation through social media has been associated with a range of adverse effects. These include the amplification of incorrect interpretations of scientific information, the intensification of polarization of opinions, the spread of fear and panic, and the potential hindrance of individuals’ access to essential healthcare services.24,26 The rapid dissemination of inaccurate health information during a public health emergency is facilitated by the widespread accessibility of online resources, mainly through smartphones.28–30
A careful examination of literature has identified an increasing prevalence of inadequate health-related information circulated via social media platforms during pandemics, environmental crises, and health emergencies.31,32 Previous studies noted that spreading unreliable information regarding health issues increases vaccine hesitancy and promotes unverified treatments.26 Research has found that YouTube videos related to emerging infectious diseases indicated that a significant portion, approximately 20–30%, were found to contain inaccurate or misleading information.28,33 Thereby, this study aims to examine the role of online misinformation and disinformation about hepatitis, and the implications of risk communication campaigns in influencing the public’s willingness to receive the hepatitis vaccine.
To theorize this phenomenon this study drew an analogy with the situational theory of problem-solving (hereafter STOPS). STOPS as an extended and generalized version of the situational theory of publics (theory of publics) highlights the pivotal perceptions and situational constructs in shaping the public’s communicative behaviors.34,35 Within the realm of hepatitis, risk perception influences constraint recognition, problem recognition, and problem involvement. As a result, the primary challenges arise from a deficiency in trust towards getting immunized, which stems from the proliferation of misinformation,36 dissemination of disinformation,37 and the presence of conspiracy beliefs.38 Consequently, this can decrease an individual’s situational motivation and engagement in other immunization-related issues.
STOPS affirms that the perceptual factors (ie, constraint, problem, and involvement recognition) correspond to situational motivation. The perceptual and situational factors result in individuals engaging in risky communicative behaviors related to problem-solving. These behaviors include actively seeking information regarding a hepatitis vaccine (risk information seeking) and evaluating all available information to select the most relevant information about vaccine-related concerns (known as information forefending). The behavior associated with vaccine intake problems can be traced back to these communicative actions.
Additionally, situational factors in problem resolution and the level of activeness in risk communication, play a significant role in shaping individuals’ intentions to uptake vaccines. The primary advantage of the STOP framework resides in its capacity to predict individuals’ inclination towards engaging in problem-solving activities including searching for appropriate information on the hepatitis vaccine as a result of the realization of the problem. This study introduces novel contextual antecedents that elucidate the perceptual and situational factors that delineate the public’s risk communication behaviors, such as information seeking when addressing the issue of hepatitis vaccination, as proposed in the conceptual model in Figure 1.
The research expands on the implications of the STOP theory beyond communicative behaviors and involves public behavior related to hepatitis vaccination acceptance. Furthermore, previous literature is very sparse in linking situational, perpetual, and social factors. For example, people do not live in isolation; they engage with the virtual world.39 They simultaneously obtain misinformation, disinformation, and health information from official sources and social circles. Therefore, the study investigates how managing infodemics is critical in determining the willingness or intention to get vaccinated. Based on this conceptual model, this study proposes the following hypotheses:
H1: Misinformation and disinformation positively impact risk perception about hepatitis vaccine safety (Hereafter RPHV). H2–4: RPHV positively impacts (H2) individuals’ problem recognition, (H3) individuals’ involvement recognition, and (H4) constraint recognition of hepatitis vaccine safety. H5: Individuals’ problem recognition (H5a), Individuals’ involvement (H5b), and Individuals’ constraint recognition (H5c) of hepatitis vaccine safety positively influence their situational motivation (hereafter SMHV). H6: SMHV positively influences risk communicative behaviors (RCB hereafter). H7: RCB positively impacts willingness to get vaccinated against hepatitis.
Methods and Materials
Design and Procedure
This study utilized a cross-sectional research design to investigate the influence of misinformation/disinformation on vaccination regarding hepatitis. An online survey method was used to collect data from the sample of 1931 internet users across Pakistan. The data was gathered using an online questionnaire disseminated via Google Forms. The questionnaire link was distributed across numerous social media platforms, including two filter questions to meet the inclusion criteria. Considering the nature and purpose of the study, the target population for the survey included internet users exposed to hepatitis vaccination-associated misinformation or disinformation. The researchers intended to recruit respondents susceptible to misinformation and disinformation. Therefore, the questionnaire included two filter questions, and those who agreed and met the criteria were only included in this research. The participation condition criteria were: (1) must be adult participants and (2) internet users exposed to misinformation or disinformation about the hepatitis vaccine. Only those respondents who ticked “yes” on filter questions were led to the main questionnaire and requested to sign an informed consent form to ensure ethical and volunteer participation in the study. Data collection continued for three months, from Mar 1, 2024, to Jun 30, 2024.
Sample Size Determination
Pakistan had approximately “82.90 million active internet users in 2022”.4,40,41 To confirm sample generalization, the study undertook a two-fold strategy. Firstly, to confirm the appropriate sample, this research used a G-Power analysis, which confirmed that a sample size greater than 1789 is suitable, with a significant effect size of 0.49, ensuring a predictive power of greater than 90%. Secondly, the researchers used a formula to verify that a sample size greater than 1500 can demonstrate an acceptable generalizability representing a population of under 100 million internet users at a 2.5% confidence level.42 For this research, a minimum sample of 1789 adult internet users was chosen to ensure robust data analysis employing covariance-based structural equation modeling (CB-SEM), which requires data to match normality assumptions. An additional 15% to 20% of data was gathered as a precaution to defend against potential generalizability problems, especially in the event of outlier detection and removal. This strategy reduced the prospect that a decrease in the sample would concede the strength of the findings.
Content Validity Rating
Experts were requested to provide feedback to ensure the content and translational validity. They reviewed definitions of constructs and ascertained their appropriateness. Considering the review of the experts and academicians, the researchers calculated content validity and found it to be within the suggested threshold of 0.66. The variables were measured at the highest level to ensure the application of robust statistical analysis. It is customary that the variables’ measurement level determines the type of statistical test we use to analyze data.43
Measurement
All constructs in this study were measured on a 5-point Likert scale (5 = strongly agree, 4 = agree, 3 = neutral, 2 = disagree, 1 = strongly disagree).
Misinformation and Disinformation
The variable of misinformation and disinformation was measured using five items. The items were as follows: (1) “Hepatitis vaccine development did not involve valid safety testing”, (2) “Hepatitis vaccine contains dangerous nanoparticles that will affect human health”, (3) “Hepatitis vaccine is a population control mechanism”, (4) “The microchip can be implanted in my body through hepatitis vaccine”, and (5) “The hepatitis vaccine negatively affects human health”.
STOPS Variables
Four items were adapted and modified from the literature to examine RPHV.44 Four items, taken from the literature, were used to measure each of the two variables: PR, IR, and CR.34,45 SMHV was tapped using three items adjusted from previous research.34 RCB is conceptualized as a second-order construct comprising four dimensions: information seeking, forfending, attending, and permitting. Each dimension was measured using two items as recommended by the literature.34,45
Dependent Variable
Willingness to get hepatitis vaccinated was assessed using three items tailored from the previous research.46
Results
Descriptive Analysis
The research was initiated using demographic analysis to identify the attributes of the sample. The “results” are reported in Table 1, suggesting diverse participation.
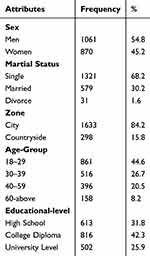 |
Table 1 Demographic Attributes |
Initially, the study ran several statistical tests using the SPSS 24.0 program, including tests for data normalcy, variance inflation (VIF), outlier visualization, and Pearson’s test for correlation. After identifying and removing 85 outliers, the “results” showed that the data had been sufficiently normalized. Additionally, all measures were found well below the cutoff value of 10. Ergo, the outcomes of VIF tests indicated that multicollinearity was not a considerable concern. Table 2 displays the bivariate correlation “results” and the correlated variables according to the study’s theory.
 |
Table 2 Pearson’s Correlation Test |
Confirmatory Factor Analysis (CFA)
Following the descriptive analysis, this study used structural equation modeling (SEM) techniques to perform a confirmatory factor analysis using Amos 23.0. The internal reliability, validity, and good fit model may all be validated more effectively with SEM. The CFA measurement “results” demonstrated An excellent fit model (see Table 3). The suggested range for the acceptable values of GFI, TLI, IFI, and CFI is 0.90 to 1. Similarly, an RMSEA value of less than 0.60 is deemed sufficient, and x2/df needs to fall between 1 and 5. Acceptable values for the chi-square per degree of freedom, absolute, and incremental indices (like CFI and TLI) were indicated by the values in Table 3, and item loadings are reported in Table 4.
 |
Table 3 Confirmatory Factor Analysis |
 |
Table 4 Standardizehd Loadings |
Following the recommended standard estimations for composite reliability (greater than 0.80) and AVE (greater than 0.50), the “results” in Table 5 suggested satisfactory “results”.
 |
Table 5 Validities |
The discriminant validity was estimated using the Fornell and Larcker approach for each study construct. Since the variables were more closely related to their original variables than they were to other variables in a measurement model, the “results” showed that discriminant validity had been established (see Table 5). A structural model was evaluated for the good fit model indices before conducting inferential statistics, and the outcomes were satisfactory (see Table 3).
Inferential Statistics
SEM path analysis was used in this study to examine the seven postulations that were put forth. H1 forecasted how misinformation and disinformation will affect RPHV. The SEM findings showed that misinformation and disinformation had a significantly positive (β =0.47) impact on RPHV, supporting H1. The “results” specified a substantial impact of individuals’ RPHV (β =0.49) on problem detection, which upheld H2. The third hypothesis (H3) was also supported, suggesting that an individual’s RPHV positively influences problem recognition (β =0.54). In addition, H4 postulated that people’s RPHV has had an impact on constraint recognition; the “results” confirmed this, revealing a positive and significant coefficient (β =0.38).
The impact of (H5a) problem (β =0.29), (H5b) involvement (β =0.52), and (H5c) constraint recognition (β = −0.19) on one’s motivation (see Table 6 and Figure 2) in addressing hepatitis, vaccine uptake was also examined using the SEM path analysis. H5a, H5b, and H5c were, therefore, validated. H6 anticipated that situational motivation has a favorable impact on risk communication behaviors; this hypothesis was verified (β =0.43). Lastly, H7 was confirmed by the direct, positive, and substantial effect of risk communication behaviors on WVH (β =0.51).
 |
Table 6 Hypothesis Testing |
 |
Figure 2 Structural Model. |
Discussion
This study aims to predict the influence of misinformation and disinformation on willingness to get vaccinated against hepatitis and communicative behavior in problem-solving. To achieve this end, this study applied STOPS to measure the outcome variable of WVH. Moreover, it investigates the role of communicative actions in problem-solving. The researchers proposed several hypotheses to explore the relationship between the constructs. The study posited that misinformation and disinformation influence risk perception. The findings indicate that misinformation and disinformation affect risk perception about the hepatitis vaccine. Previous studies also noted that spreading unreliable information about health issues increases vaccine hesitancy and promotes unverified treatments.26,28,33 To counter the infodemics of misinformation and disinformation and make communication campaigns effective to motivate the public and reduce uncertainty about vaccine side effects (risk perception) determine one’s impetus to get a solution in such a situation to accept vaccine. Hence, the study’s findings expand on the implications of the STOP theory beyond communicative behaviors and involve public behavior related to hepatitis vaccination acceptance in a developing country.
In addition, the study postulated that risk perception corresponds to the realization of the problem, involvement, and constraint evaluation, and “results” supported these tenets. These “results” indicate that the prevailing threat of risk perception regarding hepatitis instills a willingness to identify problems, problem involvement, and constraints.34,47 This promotes motivation among individuals and influences their risk-communicative behavior. When individuals show more motivation, they are more willing to exhibit communicative action on their part to solve the problem of hepatitis vaccine acceptance.34 This underscores the significance of news media in creating awareness and encouraging the public to perceive hepatitis as a problem, emphasizing the prevalence and severity of hepatitis infections. This increased relevance and severity of the hepatitis problem increases the public’s involvement. The emotional stories of the individuals affected with hepatitis correspond to emotional connections and motivation to reduce the constraints regarding the problem, encourage them to seek information from trusted sources and credible information and engage in collective problem-solving to gain more acceptance of vaccination drives aimed at fighting the menace of hepatitis. This is where interventions in the form of credible and correct messages from authorities such as the government, doctors, pharmacists, religious community leaders, and WHO are key for risk communicative action. To elaborate, academic scholars and healthcare practitioners could design effective strategies to deal with misinformation and disinformation and direct individuals toward credible sources of evidence-based information24 vis-à-vis enhancing media literacy and encouraging fact-checking before consuming information sources.
In a similar vein, the findings of this study corroborated STOPS’s proposition that when an individual encounters a problematic situation, in our case, the risk of hepatitis increases the individual’s motivation to acquire domain-specific information. These findings also align with previous literature, validating that the problem-recognition chain influences motivation to address the problem.42,48 The increased motivation corresponds to increased information seeking and adopting collective communication action to developing risk communication behavior to deal with the infodemics of misinformation and disinformation on the one hand and relying on valid information to foster community-orientated communicative action wherein individuals overcome barriers and show more willingness to acceptance vaccines. In addition to these sources, news media also plays a vital role in disseminating information, creating awareness, and cultivating acceptance of vaccines.48–50
Moreover, the findings of the study also validate H6. It elaborates on how individuals seek information during risky situations and how this information corresponds to risky communicative behavior. Put differently, the higher the motivation to resolve the problem, the higher the risk of communication behavior to do something to deal with the situation. For instance, when hepatitis problem recognition, involvement recognition, and constraint recognition are higher, the motivation is also higher in addressing the problem (hepatitis risk). Likewise, the study’s findings endorse H7, emphasizing that risk communication shapes public behavior and persuades them to get immunized against hepatitis. In other words, enhanced risk communication behavior corresponds to the willingness to get immunized and ensure safety against hepatitis.26,46,51 In the current digital media ecology flooded with misinformation and disinformation, strategic communication strategies by authorities such as the government and WHO are essential to combat the pandemic of infodemics to cultivate the willingness to get immunized among the masses and restore trust in the authorities.
From the perspective of dealing with hepatitis vaccination reluctance among masses in Pakistan in particular and in the developing Global Southern countries in general, the findings of this study are significant and valuable for health authorities. These findings emphasize that management of the pandemic of infodemics such as misinformation and disinformation is critical to promote willingness to get hepatitis vaccination. Simply put, digital health information (digital interventions) provided by official authorities such as the government, doctors, religious community scholars, and WHO or health experts persuade the masses to acquire additional information regarding risk communication behavior.21,37 To meet this challenge, valid, reliable, and persuasive digital health interventions could be critical in persuading the masses to be vaccinated.52,53 In summary, misinformation and disinformation management with health and environmental campaigns at the mass level to counter health problems such as hepatitis are essential to improve public response.
Theoretical Contribution
This study supports the theoretical tenets of STOPS in the context of health communication. It elaborates on the key role of communicative actions in managing the pandemic of misinformation and disinformation. The findings robustly advance the contribution of STOPS to health-related problem-solving in global southern countries, especially Pakistan. The findings of STOPS offer empirical support to describe communicative actions in the current digital media ecology regarding vaccination against hepatitis.
The study “results” support that misinformation and disinformation should be managed through risk communication strategies vis-à-vis digital interventions to enhance vaccination against hepatitis.54 Therefore, this study suggests a model that can provide a more reasonable solution for resolving hepatitis safety concerns among the general public in the global southern countries. This study validates that STOPS is a valuable model and theoretical framework for health communication. Consequently, this theory significantly supports researchers in developing motivation to address the problem of hepatitis vaccine safety issues. It presents a blueprint for strategic health communication campaigns. The STOPS can be effective in identifying the gap between channels of misinformation and disinformation, addressing the challenges of limited resources vis-à-vis strategic use of news media sources such as radio in the local languages, keeping in view the cultural and religious sensitivities of the populations, and cultivating community-based communicative actions. The strategic and community-orientated use of trusted news media opinion leaders and trusted religious leaders could be used as interventions to encourage community-based communication action to identify and highlight the hepatitis problem, reduce constraints, and increase relevancy and involvement with the problem to develop collective communicative actions to enhance willingness to get vaccinated among the larger segments of the populace.
Practical Contribution
The communicative model has not been extensively used in health communication research. In the current media digital ecology abundant with misinformation and disinformation, identifying problem chains and introducing digital interventions could induce motivation to get risk information that could correspond to risk communication behavior, which is necessary for creating a willingness to get immunized against hepatitis. Health communication authorities frequently promote public awareness to rectify issues of vaccine hesitancy. The findings of this study provide guidelines for health authorities to design strategically effective digital interventions to manage misinformation and disinformation. Targeted campaigns can be launched to address the targeted problems, resulting in more positive public engagement. In short, the “results” provide examples of how campaign objectives can be defined using STOPS tenets by performing a simple evaluation matrix before designing health campaigns. Expert authorities could be invited to tailor media messages to the localized community’s needs, demands, and norms to increase the willingness of the masses towards vaccines, especially hepatitis vaccines. The strategic and targeted messages could focus on community opinion leaders such as religious leaders (imams) who are effective in using pulpit communication and word of mouth to persuade illiterate segments of the population to accept the hepatitis vaccine. To illustrate, eradicating polio from Pakistan is a good example.55
Limitations and Future Research
This study used a cross-sectional research design that was appropriate for investigating the association between variables. Future studies could utilize experimental or quasi-experimental research designs to ascertain the cause-and-effect relationship between the chains of variables used in STOPS. Moreover, future studies could use referent criteria in addition to other constructs to assess the subjective judgment rules people use to solve vaccination-related problems in global southern societies. The findings of the study may not be generalizable to other global southern countries keeping in view the contexts and different cultural, and religious factors. Moreover, recruiting samples using the Internet may not result in a representative sample of the population which may also limit the generalizability of the findings from the sample to the population.
Conclusion
Based on the “results” it can be concluded that risk communication behavior shapes public willingness to get vaccinated against hepatitis. Therefore, more situation-specific information about the underpinning problem (ie, the selection of an appropriate vaccine against hepatitis) could be made accessible through several official credible, and valid digital sources. These digital interventions improve the public’s response regarding willingness to vaccinate against hepatitis. In summary, health communication authorities such as the WHO government and religious authorities could be key to enhancing public acceptance of hepatitis vaccines. To meet this end, strategic health communication campaigns (eg, public service messages, digital content) can disseminate reliable, credible, and valid digital information support (eg, using experts) that can effectively improve positive public health responses toward hepatitis vaccination.
Data Sharing Statement
The data supporting the findings are available from the corresponding author upon reasonable request.
Ethical Approval and Informed Consent
All study participants signed written consent, and all information was kept confidential. Ethical clearance was gained from the departmental research Review committee of the Centre for Media and Communication Studies, University of Gujrat, Gujrat-Pakistan. The study was performed according to Helsinki Declaration principles.
Acknowledgments
We want to thank our data collectors and study participants.
Author Contributions
All authors contributed significantly to the work reported, either in its conception, study design, execution, acquisition of data, analysis, and interpretation, or in all of these areas. They also took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This study was funded by Shanxi University, Taiyuan, Xiao Dian Qu, 030006, China.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Franco E, Meleleo C, Serino L, et al. Hepatitis A: epidemiology and prevention in developing countries. World J Hepatol. 2012;4(3):68–73. doi:10.4254/wjh.v4.i3.68
2. Vraga EK, Brady SS, Gansen C, et al. A review of HPV and HBV vaccine hesitancy, intention, and uptake in the era of social media and COVID-19. Elife. 2023;12. doi:10.7554/eLife.85743
3. Iftikhar M, Yousaf M, Raza SH, Zaman U, Ogadimma EC. Unraveling the nexus: exploring the interplay of mass media, personality traits and social norms in fostering protective behavior against smog. Glob Knowl Mem Commun. 2024. doi:10.1108/GKMC-01-2024-0045
4. Yousaf M. Mass media in Pakistan: historical evolution, challenges, and prospects. In: Okocha DO, Yousaf M, Onobe MJ, editors. Handbook of Research on Deconstructing Culture and Communication in the Global South. IGI Global; 2023:21–35.
5. Dixon GN, Clarke CE. Heightening uncertainty around certain science: media coverage, false balance, and the autism-vaccine controversy. Sci Commun. 2013;35(3):358–382.
6. Enders AM, Uscinski J, Klofstad C, Stoler J. On the relationship between conspiracy theory beliefs, misinformation, and vaccine hesitancy. PLoS One. 2022;17(10):e0276082.
7. Lee SK, Sun J, Jang S, et al. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022;12(1):13681. doi:10.1038/s41598-022-17430-6
8. Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676. doi:10.1016/S0140-6736(20)30461-X
9. Vasterman P, Yzermans CJ, Dirkzwager AJ. The role of the media and media hypes in the aftermath of disasters. Epidemiol Rev. 2005;27(1):107–114.
10. Hassan Raza S, Yousaf M, Zaman U, et al. Unlocking infodemics and mysteries in COVID-19 vaccine hesitancy: nexus of conspiracy beliefs, digital informational support, psychological well-being, and religious fatalism. Vaccine. 2023;41(10):1703–1715. doi:10.1016/j.vaccine.2023.01.047
11. Aquino F, Donzelli G, De Franco E, et al. The web and public confidence in MMR vaccination in Italy. Vaccine. 2017;35(35):4494–4498. doi:10.1016/j.vaccine.2017.07.029
12. Jolley D, Douglas KM. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One. 2014;9(2):e89177. doi:10.1371/journal.pone.0089177
13. Zhu R, Zhang H-P, Yu H, et al. Hepatitis B virus mutations associated with in situ expression of hepatitis B core antigen, viral load and prognosis in chronic hepatitis B patients. Pathol Res Pract. 2008;204(10):731–742. doi:10.1016/j.prp.2008.05.001
14. Ali L, Moon H, Jung K, et al. An overview of treatment response rates to various anti-viral drugs in Pakistani Hepatitis B Virus infected patients. Virol J. 2011;8:1–4. doi:10.1186/1743-422X-8-1
15. Li G, Li W, Guo F, et al. A novel real-time PCR assay for determination of viral loads in person infected with hepatitis B virus. J Virol Methods. 2010;165(1):9–14. doi:10.1016/j.jviromet.2009.12.009
16. Alam MM, Zaidi SZ, Malik SA, et al. Serology based disease status of Pakistani population infected with Hepatitis B virus. BMC Infect Dis. 2007;7:1–4. doi:10.1186/1471-2334-7-64
17. Paraskevis D, Haida C, Tassopoulos N, et al. Development and assessment of a novel real-time PCR assay for quantitation of HBV DNA. J Virol Methods. 2002;103(2):201–212. doi:10.1016/S0166-0934(02)00033-2
18. Noorali S, Hakim ST, McLean D, et al. Prevalence of Hepatitis B virus genotype D in females in Karachi, Pakistan. J Infect Dev Countries. 2008;2(5):373–378. doi:10.3855/jidc.200
19. Hakim S, Kazmi S, Bagasra O. Seroprevalence of hepatitis B and C genotypes among young apparently healthy females of Karachi-Pakistan. Libyan J Med. 2008;3(2):66–70. doi:10.3402/ljm.v3i2.4760
20. Bell BP, Kruszonmoran D, Shapiro C, et al. Hepatitis A virus infection in the United States: serologic results from the Third National Health and Nutrition Examination Survey. Vaccine. 2005;23(50):5798–5806. doi:10.1016/j.vaccine.2005.03.060
21. Nankya-Mutyoba J, Aizire J, Makumbi F, et al. Hepatitis B virus perceptions and health seeking behaviors among pregnant women in Uganda: implications for prevention and policy. BMC Health Serv Res. 2019;19(1):760. doi:10.1186/s12913-019-4516-0
22. Liu C, Nicholas S, Wang J. The association between protection motivation and hepatitis b vaccination intention among migrant workers in Tianjin, China: a cross-sectional study. BMC Public Health. 2020;20(1):1219. doi:10.1186/s12889-020-09292-2
23. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi:10.1016/j.vaccine.2015.04.036
24. Jin Q, Raza SH, Yousaf M, et al. Can communication strategies combat COVID-19 vaccine hesitancy with trade-off between public service messages and public skepticism? Experimental evidence from Pakistan. Vaccines. 2021;9(7):757. doi:10.3390/vaccines9070757
25. Jin Q, Raza SH, Yousaf M, et al. Ingraining polio vaccine acceptance through public service advertisements in the digital era: the moderating role of misinformation, disinformation, fake news, and religious fatalism. Vaccines. 2022;10(10):1733. doi:10.3390/vaccines10101733
26. Gao J, Raza SH, Yousaf M, et al. How does digital media search for COVID-19 influence vaccine hesitancy? Exploring the trade-off between google trends, infodemics, conspiracy beliefs and religious fatalism. Vaccines. 2023;11(1):114. doi:10.3390/vaccines11010114
27. Zimba O, Gasparyan AY. Social media platforms: a primer for researchers. Reumatologia. 2021;59(2):68–72. doi:10.5114/reum.2021.102707
28. Li HO-Y, Bailey A, Huynh D, et al. YouTube as a source of information on COVID-19: a pandemic of misinformation? BMJ Global Health. 2020;5(5):e002604. doi:10.1136/bmjgh-2020-002604
29. Puri N, Coomes EA, Haghbayan H, et al. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586–2593. doi:10.1080/21645515.2020.1780846
30. Kamboh SA, Ittefaq M, Yousaf M. Editorial journalism and environmental issues in the majority world. Int J Commun. 2022;16:23.
31. Borges Do Nascimento IJ, Pizarro AB, Almeida JM, et al. Infodemics and health misinformation: a systematic review of reviews. Bull World Health Organ. 2022;100(9):544–561. doi:10.2471/BLT.21.287654
32. Denecke K, Atique S. Social media and health crisis communication during epidemics. Participatory Health Through Social Media. 2016;42–66. doi:10.1016/B978-0-12-809269-9.00004-9
33. Shao C, Feo T, Harvey TA, et al. The spread of low-credibility content by social bots. Nat Commun. 2018;9(1):1–9. doi:10.1038/s41467-017-02088-w
34. Kim J-N, Grunig JE. Problem solving and communicative action: a situational theory of problem solving. J Commun. 2011;61(1):120–149. doi:10.1111/j.1460-2466.2010.01529.x
35. Kim J-N. Communicant Activeness, Cognitive Entrepreneurship, and a Situational Theory of Problem Solving. University of Maryland, College Park; 2006.
36. Verma G, Bhardwaj A, Aledavood T, et al. Examining the impact of sharing COVID-19 misinformation online on mental health. Sci Rep. 2022;12(1):8045. doi:10.1038/s41598-022-11488-y
37. Balakrishnan V. COVID-19 and fake news dissemination among Malaysians – motives and its sociodemographic correlates. Int J Disaster Risk Reduct. 2022;73:102900. doi:10.1016/j.ijdrr.2022.102900
38. Lazić A, Žeželj I. A systematic review of narrative interventions: lessons for countering anti-vaccination conspiracy theories and misinformation. Public Underst Sci. 2021;30(6):644–670. doi:10.1177/09636625211011881
39. Gisondi MA, Chambers D, La TM, et al. A Stanford conference on social media, ethics, and COVID-19 misinformation (INFODEMIC): qualitative thematic analysis. J Med Internet Res. 2022;24(2):e35707. doi:10.2196/35707
40. Kemp S. Digital 2022: Pakistan. 2022.
41. Okocha DO, Yousaf M, Onobe MJ, eds.. Handbook of Research on Deconstructing Culture and Communication in the Global South. IGI Global; 2023.
42. Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–610. doi:10.1177/001316447003000308
43. Mahmood N, Yousaf M. Making Sense of Statistical Analysis: A Researcher’s Handbook of Data Analysis Using IBM SPSS. National Book Foundation; 2024.
44. Nan X, Xie B, Madden K. Acceptability of the H1N1 vaccine among older adults: the interplay of message framing and perceived vaccine safety and efficacy. Health Commun. 2012;27(6):559–568. doi:10.1080/10410236.2011.617243
45. Jiang H, Kim J-N, Liu B, et al. The impact of perceptual and situational factors on environmental communication: a study of citizen engagement in China. Environ Commun. 2019;13(5):582–602. doi:10.1080/17524032.2017.1346517
46. Yoda T, Katsuyama H. Willingness to receive COVID-19 vaccination in Japan. Vaccines. 2021;9(1):48. doi:10.3390/vaccines9010048
47. Grunig JE. A situational theory of publics: conceptual history, recent challenges and new research. In: Moss D, MacManus T, Vercic D, editors. Public Relations Research: An International Perspective. ITB Press; 1997:3–46.
48. Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet. 2010;376(9748):1261–1271. doi:10.1016/S0140-6736(10)60809-4
49. Chen J, Wang Y. Social media use for health purposes: systematic review. J Med Internet Res. 2021;23(5):e17917. doi:10.2196/17917
50. de Vere Hunt I, Linos E. Social media for public health: framework for social media-based public health campaigns. J Med Internet Res. 2022;24(12):e42179. doi:10.2196/42179
51. Shen H, Xu J, Wang Y. Applying situational theory of problem solving in cancer information seeking: a cross-sectional analysis of 2014 hINTS survey. J Health Commun. 2019;24(2):165–173. doi:10.1080/10810730.2019.1587111
52. Jaspal R, Breakwell GM. Social support, perceived risk and the likelihood of COVID-19 testing and vaccination: cross-sectional data from the United Kingdom. Curr Psychol. 2022;41(1):492–504. doi:10.1007/s12144-021-01681-z
53. Yousaf M, Hassan Raza S, Mahmood N, et al. Immunity debt or vaccination crisis? A multi-method evidence on vaccine acceptance and media framing for emerging COVID-19 variants. Vaccine. 2022;40(12):1855–1863. doi:10.1016/j.vaccine.2022.01.055
54. Lohiniva A-L, Nurzhynska A, Hudi A-H, et al. Infodemic management using digital information and knowledge cocreation to address COVID-19 vaccine hesitancy: case study from Ghana. JMIR Infodemiol. 2022;2(2):e37134. doi:10.2196/37134
55. Hussain SF, Boyle P, Patel P, et al. Eradicating polio in Pakistan: an analysis of the challenges and solutions to this security and health issue. Global Health. 2016;12(1):63. doi:10.1186/s12992-016-0195-3
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Public Perceptions Towards Online Health Information: A Mixed-Method Study in Eastern Province of Saudi Arabia
Alanzi TM
Journal of Healthcare Leadership 2023, 15:259-272
Published Date: 26 October 2023


