Back to Journals » Journal of Inflammation Research » Volume 18
Exportin-T Promotes Breast Cancer Progression via PI3K/AKT/mTOR Signaling Pathway
Authors Hou Z, Ma W, Ren D, Shen N, Bi W, Guo M, Li X, Wang Y , Jia H
Received 16 January 2025
Accepted for publication 16 May 2025
Published 21 May 2025 Volume 2025:18 Pages 6467—6481
DOI https://doi.org/10.2147/JIR.S512905
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Zhichao Hou,1 Wenxia Ma,2 Dongliang Ren,1 Ningning Shen,2 Weilin Bi,1 Meiqin Guo,1 Xinzheng Li,1 Yanhong Wang,3 Hongyan Jia4
1Department of Breast Surgery, The Second Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 2Department of Pathology, The Second Hospital of ShanXi Medical University, Tai Yuan, People’s Republic of China; 3Department of Microbiology and Immunology, Shanxi Medical University, Taiyuan, People’s Republic of China; 4Department of Breast Surgery, First Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China
Correspondence: Hongyan Jia, Department of Breast Surgery, First Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China, Email [email protected]
Purpose: Breast cancer (BC) is the most common malignant tumor in women. Exportin-T (XPOT) which is a member of the karyopherin -β family has been identified as a prognostic biomarker in various cancers, but its role in BC remains inadequately understood. This study aims to investigate the clinical characterization and molecular mechanism of XPOT in BC.
Material and Methods: A retrospective RNA-seq data analysis based on a cohort of 966 BC patients from The Cancer Genome Atlas database (TCGA) and 1904 patients from the Molecular Taxonomy of Breast Cancer International Consortium database was conducted for analyzing the correlation between XPOT expression and BC clinical pathological features. In addition, small interfering RNA transfection was used to downregulate XPOT expression in MDA-MB-468/231 cell lines followed by cell proliferation assessed via Cell Counting Kit-8 assays, meanwhile, BC cell migration and invasion capabilities were measured using Transwell test. Expression levels of CDK4/6 and key proteins in the PI3K/Akt/mTOR signaling pathway were assessed using Western blotting.
Results: We found that XPOT was enriched in estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, larger tumor size, and cases with increased lymph node metastasis BC. XPOT was identified as a potential biomarker for the basal subtype of BC and a prognostic factor for the overall survival of patients with BC. Furthermore, XPOT promoted the proliferation and invasion of BC cells, likely through activation of the PI3K/AKT/mTOR signaling pathway, which in turn to upregulate cyclin D and CDK4/6 to drive tumor progression.
Conclusion: Our findings indicate that XPOT overexpression is associated with poor clinical characteristics and poor prognosis in BC, promoting disease progression by activating PI3K/AKT/mTOR pathway. These findings highlight XPOT as a potential therapeutic target in BC.
Keywords: breast cancer, exportin-T, cell proliferation, PI3K/AKT/mTOR signaling, prognosis biomarkers
Introduction
Breast cancer (BC) is the most commonly diagnosed malignant tumor and a leading cause of cancer-related deaths among females worldwide. In the United States alone, it is projected that in 2024, approximately 313,510 women will be diagnosed with BC, and 42,780 will die from the disease,1 accounting for approximately 32% of all cancer cases. Despite advances in early screening and comprehensive treatments-including surgery, radiotherapy, chemotherapy, endocrine therapy, and targeted therapy-have reduced recurrence and metastasis rates, nearly all patients with metastatic BC eventually succumb to the disease.2 Thus, further investigation of the mechanisms underlying BC progression is crucial for developing new therapeutic targets.
Exportins are a group of karyopherins that mediate the transport of proteins from the nucleus to the cytoplasm and play a key role in regulating the localization of various crucial cancer-related proteins.3 Dysregulated expression or mislocalization of karyopherins has been observed in numerous cancers, contributing to sustained cancer cell proliferation, apoptosis resistance, and immune escape.4,5 Exportin-T (XPOT), a member of the karyopherin -β family, functions as a specific export receptor of transfer RNA (tRNA).6,7 XPOT shuttles between the nucleus and cytoplasm through nuclear pore complexes by interacting with GTP-bound Ran.8 Studies have shown that XPOT promotes tumor progression in several cancers, including pleural mesothelioma,9 hepatocellular carcinoma,10 and promyelocytic leukemia.11 Despite the growing evidence of XPOT’s oncogenic role, the specific pathways and mechanisms by which XPOT influences BC progression remain unclear. Thus, elucidating the functional and regulatory mechanisms of XPOT in BC is of significant importance.
In this study, we used bioinformatic analyses to examine XPOT expression profiles in BC using data from the Cancer Genome Atlas (TCGA) database12 and the Molecular Taxonomy of Breast Cancer International Consortium (METABRIC) database.13 We investigate the association between XPOT expression and clinicopathological characteristics, as well as patient survival outcomes in BC. Furthermore, cell-based experiments were conducted to analyze the molecular mechanisms through which XPOT regulates the PI3K/AKT/mTOR signaling pathway and cell cycle progression. Collectively, our findings offer novel insights into the role of XPOT in promoting BC progression and suggest that XPOT could be a promising therapeutic target for BC treatment.
Materials and Methods
Data Resource and Processing
The transcriptomic expression data with corresponding clinicopathologic information were obtained from TCGA (113 normal breast samples and 1109 BC samples) and METABRIC (1904 BC samples). The collected clinicopathologic information included age, tumor diagnosis, tumor size, lymph node status, estrogen receptor (ER) status, progesterone receptor (PR) status, human epidermal growth factor receptor 2 (HER2) status, tumor grade, American Joint Committee on Cancer (AJCC) stage, molecular subtype, and follow-up details. After excluding patients lacking specific molecular subtype data, 966 TCGA BC patients were used as the training set, and 1904 METABRIC BC patients served as the validation set. Data filtering was conducted using the “rma” function in the R package (R Studio version 2023.09.1+494, R version 4.3.1) to remove missing or duplicated entries. Since all patient data were de-identified, Institutional Review Board approval was exempted from local ethics committee (the Second Hospital of ShanXi Medical University) as per the committee’s guidelines.
Functional Enrichment Analysis
Genes most relevant to XPOT were uploaded to the Database for Annotation, Visualization, and Integrated Discovery (DAVID, v6.8). Using the official gene symbol as the identifier and selecting Homo sapiens was selected as species, we performed Gene Ontology (GO) analysis and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses. The top six pathways with significant enrichment (p< 0.05) are presented in this study.
Gene Set Variation Analysis (GSVA)
The gene list for cell division processes and cell cycle regulation was obtained from the AmiGO 2 portal (http://amigo.geneontology.org/amigo). Functional enrichment scores for each BC sample were calculated using the R environment with default parameters, and the enrichment results were visualized using the pheatmap package. Pearson correlation analysis was used to determine the correlation between XPOT expression and gene sets related to cell division and cell cycle regulation.
Gene Set Enrichment Analysis (GSEA)
GSEA was conducted using the GSEA software (version 4.3.2) from the Broad Institute14 to examine associations between XPOT expression and various biological processes and pathways, following the software’s user guide. RNA-seq data from TCGA and METABRIC were used, and the gene set h.all.v2023.2.Hs.symbols.gmt” was obtained from the MSigDB collection.15 Patients were categorized into two BC phenotypes based on XPOT expression levels. Enrichment significance was determined by normalized enrichment scores (NES) after 1000 permutations, with a gene set considered significantly enriched when p-value < 0.05 and false discovery rate (FDR) is < 0.25.
Cell Culture and Transfection
Human BC cell lines, including MDA-MB-468, SK-BR-3, MCF-7, MDA-MB-231, and normal mammary epithelial cell line MCF-10A were obtained from the ATCC cell bank (https://www.atcc.org/, USA). Cells were cultured in a 5% CO2 incubator at 37°C, with medium changed every 2–3 days. To inhibit XPOT expression, three small interfering RNAs (siRNAs) targeting XPOT were purchased from RIBOBIO (https://www.ribobio.com/, Guangzhou, China) with sequences as follows: si-XPOT_1: GGUGUGUGCAGAAGCUCUAGC, si-XPOT_2: GCACAUUCCAUGUGUACUAUU, si-XPOT_3: GCUGGAGUGCUGAUUGUUAAU. Cells (4~6×105 cells/well) were inoculated in 6-well plates and cultured transfected with Lipofectamine 2000 (Invitrogen) when cell confluence reached 50–70%. Transfection efficiency was evaluated by quantitative real-time PCR (qRT-PCR) after 48 hours.
qRT-PCR
Total RNA was extracted from the five cell lines and MDA-MB-468/231 cells transfected with si-XPOT1/2. Reverse transcription was performed using the reverse transcription kit provided by TOLOBIO (NO. 22112–01) to synthesize complementary DNA (cDNA). Primer sequences for XPOT were: sense: GTGCAAAAGTTCGGAGCAGG; anti-sense: GGCTTGTTTCCTTTCTGCCG. GAPDH primers were used for normalization (forward primer: TCAAGAAGGTGGTGAAGCAGG and reverse primer: TCAAAGGTGGAGGAGTGGGT). Fluorescence levels were measured with a NanoDrop ND-800 UV spectrophotometer, and amplification was conducted on an ABI3500 system. Relative mRNA gene expression levels were calculated using the 2−ΔΔCt method, and experiments were performed in triplicate.
Western Blotting
Total protein was extracted from the aforementioned five cell lines and MDA-MB-468/231 cells transfected with si-XPOT1/2 using RIPA lysis buffer (Beyotime Technology, Shanghai, China). Samples (20 μg protein) were separated via SDS-PAGE gel and transferred onto PVDF membranes (Millipore IPVH00010 and ISEQ15150). Membranes were blocked with 10% nonfat milk and incubated with the primary antibody overnight, followed by secondary antibody incubation with HRP-linked anti-mouse or anti-rabbit IgG (Jackson, 111–035-003) for 2 hours at room temperature. Visualization was performed with an ECL detection system (Thermo, NO. NCI5079). Primary antibodies used in our study are listed in Table S1.
Cell Proliferation Assay
After 48 hours of transfection, MDA-MB-468 (4 × 10³ cells/well) and MDA-MB-231 (5 × 10³ cells/well) cells were seeded in 96-well plates with six wells per group. Cell proliferation was assessed at 24, 48, and 72 hours using the Cell Counting Kit-8 (CCK-8, DOJINDO, Japan) under standard conditions.
Transwell Invasion Assay
Cell migration assays were conducted in a 24-well Transwell inserts with 8 um pore PET membranes. The bottom layer contained 600 µL of culture median with 20% serum, while the upper layer contained 200 µL serum-free culture median with 5×104 cells. After 5 hours (MDA-MB-468) or 16 hours (MDA-MB-231), insets were fixed with methanol and stained with crystal violet. For the invasion assay, Matrigel was applied to the inserts, and the cell number was increased to 1 × 105 cells/well.
Cell Cycle Analysis
Cells were fixed in 70% ice-cold ethanol at 4°C overnight, washed with PBS, and treated with RNase A (0.1 mg/mL) for 30 minutes at 37°C. After staining with propidium iodide (PI, GeneCodex, NO. C035), cell cycle distribution was analyzed using a FACSCalibur flow cytometer (CytoFLEX S).
Apoptosis Analysis
Cells with the indicated treatments were harvested, washed once with PBS and resuspended in 100 µL binding buffer. After incubation with Annexin V-FITC and PI (both GeneCodex) at RT for 30 min, apoptosis analysis was conducted on a FACSCalibur flow cytometer (CytoFLEX S).
Statistical Analyses
Statistical analyses and visualization were conducted using R software and IBM SPSS Statistics (version 25.0). Group comparisons were made using an unpaired t-test for two groups or one-way ANOVA. Correlations between the two groups were tested by Pearson correlation analysis. Survival analysis was conducted with Kaplan-Meier curves and Log rank tests. Significance was set at p < 0.05.
Results
XPOT Expression and its Association with Malignancy in BC
High levels of XPOT expression were found to correlate with specific clinical and pathological traits associated with more aggressive BC phenotypes. XPOT was highly enriched in tumor tissues compared with normal tissues in TCGA cohort (Figure S1D). Additionally, XPOT expression was distributed asymmetrically across tumor T stage, N stage, AJCC stage, age, ER status, PR status, HER2 status, and molecular subtype in both the TCGA and METABRIC cohorts (Figure 1A and B). Specifically, XPOT was enriched in ER-negative (Figure 1C) and PR-negative BC cases (Figure 1D) in TCGA cohort, with similar trends observed in METABRIC cohort (Figure 1G and H). In both datasets, larger tumors and those with more positive lymph node status also showed higher XPOT expression (Figure 1E, I, F, J). Additionally, XPOT was notably elevated in METABRIC patients with higher AJCC stages (except stage IV), younger age (<55 years), HER2 positivity, and higher tumor grade (Figure S1E–H). Meanwhile, there was no statistical correlation between XPOT expression and other clinicopathological characteristics, like AJCC stage (Figure S1A), age (Figure S1B), and HER2 status (Figure S1C) in TCGA cohort. Overall, these results suggest XPOT enrichment in patients with aggressive BC traits.
XPOT as a Potential Basal Subtype Biomarker and Independent Prognostic Indicator for BC
Analysis of XPOT expression across BC subtypes indicated a significant enrichment of XPOT in the basal subtype, in both TCGA and METABRIC datasets (P < 0.001) (Figure 2A and C). XPOT demonstrated good specificity in identifying the basal subtype, with an area under the curve (AUC) for receiver operating characteristic (ROC) of 71.8% in TCGA and 74.3% in METABRIC(Figure 2B and D). This suggests that XPOT could serve as a potential biomarker for the basal subtype and supports its association with more malignant BC cases.
To evaluate the prognostic value of XPOT in BC, we performed Kaplan-Meier survival analysis and Cox proportional hazards modeling using data from TCGA and METABRIC. Kaplan-Meier analyses demonstrated that high XPOT expression is associated with poorer overall survival, confirming its prognostic value in both TCGA and METABRIC datasets (Figure 2E and F). Cox regression analysis identified XPOT as an independent prognostic factor, alongside age, tumor size, lymph node status, and hormone receptor status, in both the TCGA and METABRIC datasets (Tables 1 and 2).
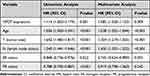 |
Table 1 Univariate and Multivariate Analysis of Prognostic Parameters in TCGA Database with Overall Survival (OS) |
 |
Table 2 Univariate and multivariate analysis of prognostic parameters in METABRIC database with overall survival (OS) |
Role of XPOT in Cell Proliferation and Tumor Progression in BC
To explore the biological functions associated with XPOT, we identified the genes most related to XPOT using Spearman correlation analysis (|R| > 0.5, P < 0.05) across the TCGA and METABRIC datasets. The detailed list of these genes is presented in Tables S2 and S3. GO and KEGG analysis were then performed based on the above gene sets. In the TCGA, biological processes most associated with XPOT included cell division (Figure S2A). Additionally, the cellular components most related to XPOT were nucleoplasm, cytosol and nucleus (Figure S2B), while the molecular functions involved protein binding and ATP binding (Figure S2C). The signaling pathways most associated with XPOT included the cell cycle and cellular senescence pathways (Figure 3A). The XPOT-related biological processes, cellular components, molecular functions, and signaling pathway identified in METABRIC were consistent with those in TCGA (Figures S2D–F and B). These findings suggest that XPOT may contribute to tumor progression by promoting cell division and cell cycle regulation.
Dysregulation of the cell cycle is a hallmark of cancer, often leading to uncontrolled cell proliferation. To investigate XPOT’s role in this process, we examined its impact on key aspects of cell division and cycle regulation. Using the GSVA in the TCGA and METABRIC dataset, we assessed the enrichment scores for the cell proliferation process. The correlation analysis revealed a positive association between XPOT expression and cell cycle activity in TCGA (Figure 3C), with similar results observed in METABRIC (Figure 3D). These results suggest that XPOT plays a role in promoting in cell proliferation in BC.
XPOT was found to play a role in tumor proliferation; therefore, we investigated its relationship with established cell proliferation marks, including MKI67, CCNB1, CDK4/6, KRAS, PCNA, CCNE1, and mini-chromosome replication maintenance 2/6 (MCM2/6), which are involved in the initiation of eukaryotic genome replication,16 in both TCGA and METABRIC datasets (Figure 3E). XPOT exhibited a strong positive association with these proliferation marks, contributing to the growth of tumor in BC. Additionally, we selected six cell proliferation-related gene sets, defined by the Molecular Signatures Database (MSigDB) Hallmark in gene set variant analysis,15 as markers: G2M checkpoint, E2F target, MYC targets v1, MYC targets v2, Mitotic spindle, and P53 pathway. As illustrated in Figure 3F and G the XPOT expression showed significantly positive correlations with most of these cell proliferation-related gene sets in both TCGA and METABRIC. These findings suggest that XPOT may regulates cell cycle through proliferation-related markers, which serve as critical cell cycle checkpoints that promote tumor progression in BC.
Effect of XPOT on the Proliferation, Migration, and Apoptosis of BC Cells
Given the prognostic significance and tumor proliferation predictive value of XPOT in BC, we further examined its biological functions in BC cells. Initially, we validated the high expression levels of XPOT in multiple BC cell lines using qRT-PCR and Western Blot assay (Figure 4A and B). Among these, MDA-MB-468 and MDA-MB-231, which exhibited the highest XPOT expression, were selected for further experiments. Three different siRNAs targeting XPOT and a negative control (si-NC) plasmid were then constructed and transfected into these cell lines. The knockdown efficiency was confirmed by qRT-PCR and Western Blot assay (Figure 4C and D), with si-XPOT-1 (si-1), the highest effective siRNA, chosen for subsequent experiments.
To assess changes in cell viability, a CCK-8 assay was performed at various time points following transfection. The results demonstrated a significant reduction in cell proliferation 48 hours after XPOT knockdown (Figure 4E). In migration assays, the number of cells crossing the membrane was markedly reduced in XPOT knockdown cells (Figure 4F). Similarly, invasion assays showed a significant decrease in the number of cells traversing the Matrigel in both cell lines following XPOT knockdown (Figure 4G).
Flow cytometry analysis of cell cycle distribution revealed that silencing XPOT increased the G0/G1 phase ratio while reducing the S phase ratio (Figure 5A), indicating that XPOT knockdown prevents cells from progressing from the G0/G1 to the S phase. Additionally, flow cytometry analysis of apoptosis showed that the percentage of apoptotic cells was higher in XPOT-silenced cells than in control cells (Figure 5B). These results indicate that XPOT promotes the proliferation and invasion capacity of BC cells while inhibiting apoptosis in vitro.
XPOT Upregulates Cyclin D and CDK4/6 by Activating the PI3K/AKT/mTOR Signaling Pathway to Influence Tumor Progression in BC
To investigate the potential mechanisms by which XPOT may regulate BC development, we performed Gene Set Enrichment Analysis (GSEA) on Hallmark gene sets in MSigDB. Based on median XPOT expression levels in the TCGA and METABRIC datasets, patients were divided into high and low XPOT expression groups. The analysis revealed that the high XPOT expression group was significantly enriched PI3K/AKT/mTOR and MTORC1 signaling (Figure 6A-D). These results indicated an underlying mechanism that XPOT promotes BC progression by activating the PI3K/AKT/ mTOR signaling pathway.
To further investigate the mechanisms underlying XPOT’s effects, we performed Western blot analysis to evaluate the expressions of cell cycle-regulating proteins and determine whether XPOT knockdown alters the levels of cell cycle checkpoint proteins and key components of the PI3K/AKT/mTOR signaling pathway. The results showed that silencing XPOT significantly reduced the phosphorylation levels of PI3K, AKT, and mTOR compared to control cells (Figure 6E and F), suggesting that XPOT promotes BC progression by activating the PI3K/AKT/mTOR pathway. Moreover, XPOT knockdown led to a marked decrease in CDK4, CDK6, and cyclin D levels, while expression level of the cell cycle-inhibiting protein P27 was upregulated. The above findings indicate that XPOT could regulate the cell cycle by upregulating CDK4, CDK6, and cyclin D expression and promote BC progression via the PI3K/AKT/mTOR pathway.
Discussion
BC is the most common malignancy and the leading cause of cancer-related death among women worldwide. Despite great advances in the diagnosis and treatment, BC relapses in a considerable number of patients, highlighting the urgent need to identify novel biomarkers with clinical and prognostic relevance. In this study, we focused XPOT, a member of karyopherin -β. The karyopherin superfamily have been considered as an extremely promising targets for cancer therapy.17 XPOT itself plays a critical role in the nucleocytoplasmic trafficking of tRNAs, contributing to protein translation for cell growth and metabolism.7,18
Previous studies have reported that XPOT play important functions in multiple cancers including in pleural mesothelioma, hepatocellular carcinoma, promyelocytic leukemia, neuroblastoma. For instance, Lin et al reported significant upregulation of XPOT in hepatocellular carcinoma using data from 95 pairs of TCGA and GEO datasets, as well as 16 fresh tumor specimens analyzed by qRT-PCR and immunohistochemistry.10 Similarly, research by Pan et al revealed that XPOT overexpression in neuroblastoma was associated with poor clinical outcomes, including age at diagnosis >18 months, MYCN amplification, advanced INSS stage, and poor prognosis, suggesting XPOT as a therapeutic target in this cancer.19
In BC, Dai et al demonstrated that XPOT overexpression was linked to worse survival outcomes in triple-negative breast cancer (TNBC), and that inhibition of XPOT suppressed TNBC cell proliferation both in vitro and in vivo, suggesting that XPOT’s role as an oncogenic gene in TNBC.20 Our findings are consistent with this, as we analyzed XPOT expression in various BC subtypes using mRNA-seq data from 2870 BC patients in TCGA and METABRIC. Our results showed that XPOT was enriched in more malignant BC subtypes, particularly in the basal subtype, and was positively correlated with the cell proliferation based on GO enrichment, functional analysis, and GSVA.
Moreover, we found that XPOT expression closely mirrored that of cell proliferation-related markers and gene sets. GSEA further revealed that XPOT activates the PI3K/AKT/mTOR signaling pathway to promote BC progression. Functional studies of BC cells showed that XPOT knockdown inhibited cell proliferation and migration of BC cells, while upregulating cyclin D and CDK4/6 by activating the PI3K/AKT/mTOR signaling pathway, thus influencing tumor progression. Nuclear transport receptors have been reported to be associated with cell cycle regulation. This regulation can occur either directly through interactions with chromatin and the expression of genes involved in cell cycle progression,21 by regulating the nucleocytoplasmic distribution of cell cycle-related cargo molecules4 or by coordinating cell cycle events.22
Published studies indicated that in liver cancer, XPOT knockdown causes cell cycle arrest in the G0/G1 phase by downregulating cell cycle regulators such as cyclin-dependent kinase-1 and cyclin A.10 In neuroblastoma, RNA interference studies demonstrated that XPOT knockdown inhibited cell proliferation and migration.19 Consistent with these studies, our analysis revealed that XPOT-related genes were enriched in biological functions related to cell division and cell cycle, as shown by GO, KEGG and GSVA. Moreover, XPOT are positively correlated with critical cell cycle checkpoints such as CCNB1, CCNE1 and CDK4/6. Furthermore, XPOT inhibition decreased BC cell proliferation, migration, and invasion, and promoted apoptosis in vitro. Flow cytometry analysis after XPOT knockdown in MDA-MB-231 and MDA-MB-468 cells showed a higher proportion of cells in the G0/G1 phase and a lower proportion in the S phase, indicating cell cycle arrest at the G0/G1 stage.
The PI3K/AKT/mTOR signaling pathway is frequently dysregulated in human malignancies,23 and blocking this pathway has emerged as a promising strategy for BC therapy.24–26 Downstream mTOR is a vital protein kinase in this pathway, regulates the tumor cell growth, proliferative, survival, and angiogenesis.27 Dysregulation of PI3K/AKT/mTOR signaling leads to uncontrolled cell proliferation, genomic instability, and metabolic reprogramming all of which promote tumorigenesis.28 Elevated XPOT has been shown to contribute to chromosome instability and worsen prognosis in BC patient.29 However, further studies are needed to fully elucidate the mechanisms by which XPOT enhances BC malignancy. Our study revealed genes in the PI3K/AKT/mTOR signaling pathway are significantly enriched in the high XPOT expression group, and that XPOT knockdown reduces PI3K, AKT, and mTOR phosphorylation levels. These findings suggested that XPOT promotes BC progression by activating the PI3K/AKT/mTOR pathway.
Our study has several limits indeed. First, our analysis was based on publicly available sequencing data, which may introduce inherent biases. Second, while we demonstrated the involvement of the PI3K/AKT/mTOR pathway in BC progression, the association between the gene and other well known signaling pathways that were related with BC development, for instance TP53 and immune invasion related signaling pathways have not been included in the study, additional tumor-related signaling pathways should be explored to better understand their role in BC development. Third, follow-up studies involving animal models and clinical samples are needed to validate the findings observed in vitro.
Conclusions
Our study underscores the biological functions and prognostic significance of XPOT in BC. We found that XPOT overexpression is associated with adverse clinical features, including negative ER/PR status, larger tumor size, and increased lymph node metastasis, all of which correlate with poor prognosis in BC patients. Mechanistically, XPOT promotes tumor progression in BC by upregulating cyclin D and CDK4/6 through the activation of the PI3K/AKT/mTOR signaling pathway. These findings offer valuable insights into the potential of targeting XPOT for BC therapy.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The Cancer Genome Atlas (TCGA), the Molecular Taxonomy of Breast Cancer International Consortium (METABRIC), and Molecular Signatures Database (MSigDB) are public databases that allow unlimited reuse under open licenses. Ethics approval had been obtained prior to the conduction of the study involving patients included in these databases. Users can freely download relevant data in these databases for conducting research, based on which users can also draft related articles for publication. Our research is based on open-source data from these datasets and follows the data access policies and publication guidelines of these datasets, with no ethical concerns or any conflicts of interest. Therefore, this study was exempted from obtaining approval from the local ethics committee (the Second Hospital of ShanXi Medical University) as per the committee’s guidelines.
Consent for Publication
The manuscript was approved by all authors for publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Research Project Supported by The Basic Research Project of Shanxi Province (No:202103021223441), The Science Popularization and Propaganda Special Project of Shanxi Province (No:202204091001024) and The Physician Research Project of Shanxi Medical Association (No: YSXH-QL2023RX006).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA. 2024;74(1):12–49. doi:10.3322/caac.21820
2. Nolan E, Lindeman GJ, Visvader JE. Deciphering breast cancer: from biology to the clinic. Cell. 2023;186(8):1708–1728. doi:10.1016/j.cell.2023.01.040
3. Turner JG, Dawson J, Sullivan DM. Nuclear export of proteins and drug resistance in cancer. Biochem Pharmacol. 2012;83(8):1021–1032. doi:10.1016/j.bcp.2011.12.016
4. Çağatay T, Chook YM. Karyopherins in cancer. Curr Opin Cell Biol. 2018;52:30–42. doi:10.1016/j.ceb.2018.01.006
5. Tran EJ, King MC, Corbett AH. Macromolecular transport between the nucleus and the cytoplasm: advances in mechanism and emerging links to disease. BBA. 2014;1843(11):2784–2795. doi:10.1016/j.bbamcr.2014.08.003
6. Arts GJ, Fornerod M, Mattaj IW. Identification of a nuclear export receptor for tRNA. Curr Biol. 1998;8(6):305–314. doi:10.1016/S0960-9822(98)70130-7
7. Kutay U, Lipowsky G, Izaurralde E, et al. Identification of a tRNA-specific nuclear export receptor. Molecular Cell. 1998;1(3):359–369. doi:10.1016/S1097-2765(00)80036-2
8. Kuersten S, Arts GJ, Walther TC, Englmeier L, Mattaj IW. Steady-state nuclear localization of exportin-t involves RanGTP binding and two distinct nuclear pore complex interaction domains. Mol Cell Biol. 2002;22(16):5708–5720. doi:10.1128/MCB.22.16.5708-5720.2002
9. Melaiu O, Melissari E, Mutti L, et al. Expression status of candidate genes in mesothelioma tissues and cell lines. Mutat Res. 2015;771:6–12. doi:10.1016/j.mrfmmm.2014.11.002
10. Lin J, Hou Y, Huang S, et al. Exportin-T promotes tumor proliferation and invasion in hepatocellular carcinoma. Mol Carcinogenesis. 2019;58(2):293–304. doi:10.1002/mc.22928
11. Suzuki T, Koyama Y, Hayakawa S, Munakata H, Isemura M. 1,25-Dihydroxyvitamin D3 suppresses exportin expression in human promyelocytic leukemia HL-60 cells. Biomed Res. 2006;27(2):89–92. doi:10.2220/biomedres.27.89
12. Tomczak K, Czerwińska P, Wiznerowicz M. The Cancer Genome Atlas (TCGA): an immeasurable source of knowledge. Contemp Oncol. 2015;19(1a):A68–77. doi:10.5114/wo.2014.47136
13. Curtis C, Shah SP, Chin SF, et al. The genomic and transcriptomic architecture of 2000 breast tumours reveals novel subgroups. Nature. 2012;486(7403):346–352. doi:10.1038/nature10983
14. Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA. 2005;102(43):15545–15550. doi:10.1073/pnas.0506580102
15. Liberzon A, Birger C, Thorvaldsdóttir H, Ghandi M, Mesirov JP, Tamayo P. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Systems. 2015;1(6):417–425. doi:10.1016/j.cels.2015.12.004
16. Tirosh I, Izar B, Prakadan SM, et al. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-seq. Science. 2016;352(6282):189–196. doi:10.1126/science.aad0501
17. Azizian NG, Li Y. XPO1-dependent nuclear export as a target for cancer therapy. J hematol oncol. 2020;13(1):61. doi:10.1186/s13045-020-00903-4
18. Cook AG, Fukuhara N, Jinek M, Conti E. Structures of the tRNA export factor in the nuclear and cytosolic states. Nature. 2009;461(7260):60–65. doi:10.1038/nature08394
19. Pan LJ, Chen JL, Wu ZX, Wu YM. Exportin-T: a novel prognostic predictor and potential therapeutic target for neuroblastoma. Technol Cancer Res Treat. 2021;20:15330338211039132. doi:10.1177/15330338211039132
20. Dai H, Yang X, Sheng X, et al. XPOT disruption suppresses TNBC growth through inhibition of specific tRNA nuclear exportation and TTC19 expression to induce cytokinesis failure. Int J Bio Sci. 2023;19(16):5319–5336. doi:10.7150/ijbs.85006
21. Yasuda Y, Miyamoto Y, Yamashiro T, et al. Nuclear retention of importin α coordinates cell fate through changes in gene expression. EMBO J. 2012;31(1):83–94. doi:10.1038/emboj.2011.360
22. Roscioli E, Di Francesco L, Bolognesi A, et al. Importin-β negatively regulates multiple aspects of mitosis including RANGAP1 recruitment to kinetochores. J Cell Biol. 2012;196(4):435–450. doi:10.1083/jcb.201109104
23. Glaviano A, Foo ASC, Lam HY, et al. PI3K/AKT/mTOR signaling transduction pathway and targeted therapies in cancer. Mol Cancer. 2023;22(1):138. doi:10.1186/s12943-023-01827-6
24. Chien AJ, Tripathy D, Albain KS, et al. MK-2206 and standard neoadjuvant chemotherapy improves response in patients with human epidermal growth factor receptor 2-positive and/or hormone receptor-negative breast cancers in the I-SPY 2 Trial. J clin oncol. 2020;38(10):1059–1069. doi:10.1200/JCO.19.01027
25. Hanker AB, Sudhan DR, Arteaga CL. Overcoming endocrine resistance in breast cancer. Cancer Cell. 2020;37(4):496–513. doi:10.1016/j.ccell.2020.03.009
26. Vicier C, Sfumato P, Isambert N, et al. TAKTIC: a prospective, multicentre, uncontrolled, phase IB/II study of LY2780301, a p70S6K/AKT inhibitor, in combination with weekly paclitaxel in HER2-negative advanced breast cancer patients. Eur J Cancer. 2021;159:205–214. doi:10.1016/j.ejca.2021.09.040
27. Tian T, Li X, Zhang J. mTOR signaling in cancer and mTOR inhibitors in solid tumor targeting therapy. Int J Mol Sci. 2019;20(3):755. doi:10.3390/ijms20030755
28. Lien EC, Dibble CC, Toker A. PI3K signaling in cancer: beyond AKT. Curr Opin Cell Biol. 2017;45:62–71. doi:10.1016/j.ceb.2017.02.007
29. Vaidyanathan S, Thangavelu PU, Duijf PH. Overexpression of ran GTPase components regulating nuclear export, but not mitotic spindle assembly, marks chromosome instability and poor prognosis in breast cancer. Targeted Oncol. 2016;11(5):677–686. doi:10.1007/s11523-016-0432-y
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







