Back to Journals » Cancer Management and Research » Volume 17
Expression and Diagnostic Value of Nrf2 and p62 in Cervical Squamous Cell Carcinoma and Intraepithelial Lesions
Received 19 December 2024
Accepted for publication 2 May 2025
Published 24 May 2025 Volume 2025:17 Pages 1005—1013
DOI https://doi.org/10.2147/CMAR.S513226
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Wei Wei, Xingyan Hu, Qing Han
Department of Gynaecology, Yichang Central People’s Hospital, The First College of Clinical Medical Science, China Three Gorges University, Yichang, Hubei, People’s Republic of China
Correspondence: Qing Han, Department of Gynaecology, Yichang Central People’s Hospital, The First College of Clinical Medical Science, China Three Gorges University, Yichang, Hubei, People’s Republic of China, Email [email protected]
Background: This study aims to explore the value of Nuclear Transcription Factor Erythroid 2-Related Factor 2 (Nrf2) and the selective autophagy adapter protein p62/Sequestosome 1 (SQSTM1) in diagnosing cervical squamous cell carcinoma (SCC) and squamous intraepithelial lesions (SIL).
Methods: Paraffin specimens from 125 cervical SCC patients, 102 low-grade SIL (LSIL) patients, 101 high-grade SIL (HSIL) patients, and 49 patients with benign/reactive cervical squamous epithelium were collected at Yichang Central People’s Hospital from 2010 to 2023. Immunohistochemistry was used to detect Nrf2 and p62 expression. Positive expression was defined by visible light yellow, brownish-yellow, or brown cytoplasmic particles. The correlation between the two proteins and their diagnostic value were analyzed.
Results: Both Nrf2 and p62 were predominantly localized to the cytoplasm in various cervical lesions. The expression levels of Nrf2 and p62 were significantly higher in LSIL, HSIL, and SCC than in benign/reactive epithelium (all P< 0.001), and lower in LSIL than in HSIL and SCC (all P< 0.001). A positive correlation was found between Nrf2 and p62 in all lesion types (all P< 0.05). ROC analysis indicated that the diagnostic accuracy was enhanced when Nrf2 and p62 were used in combination, as opposed to using either marker individually.
Conclusion: Nrf2 and p62 are either not expressed or expressed at low levels in benign/reactive squamous epithelium, with expression increasing in LSIL, and being highest in HSIL and SCC. Both markers show a positive correlation across different cervical lesions, and either Nrf2 or p62 alone can effectively diagnose various cervical lesions, with even better diagnostic outcomes when used in combination.
Keywords: nuclear factor erythroid 2-related factor 2, Nrf2, p62, cervical squamous cell carcinoma, SCC, intraepithelial lesions, diagnostic biomarkers
Background
Cervical cancer is among the most prevalent malignant tumors in women, ranking fourth in both incidence and mortality among female cancers globally. In 2020, there were approximately 604,127 new cases and 341,831 deaths worldwide.1 In China, cervical cancer’s incidence and mortality rates place it among the top ten malignant tumors affecting women, ranking sixth and seventh, respectively.2 Histopathologically, cervical cancer is primarily divided into two types: squamous cell carcinoma (SCC), which originates from squamous cells, and adenocarcinoma, which arises from glandular cells. SCC constitutes approximately 80% of cervical cancers and typically evolves from benign cellular atypical hyperplasia to cervical intraepithelial neoplasia (CIN).3
Nuclear factor-erythroid 2-related factor 2 (Nrf2) is a key regulator of a suite of cytoprotective genes, capable of safeguarding cells under stress conditions such as exposure to reactive oxygen species and electrophilic agents.4 In recent years, an increasing number of studies have shown that Nrf2 is overexpressed in various cancers and plays a significant role in cancer promotion.5 Research has revealed that Nrf2 has a substantial impact on cervical cancer,6,7 and compared to normal cervical squamous epithelium, Nrf2 and its downstream gene quinone NADH dehydrogenase 1 (NQO1) are most highly expressed in cervical squamous cell carcinoma (SCC), followed by cervical intraepithelial neoplasia (CIN).8 This finding suggests Nrf2’s role in the transition from normal squamous epithelium to SCC.
The selective autophagy adaptor protein p62/Sequestosome 1 (SQSTM1) is a multifunctional intracellular protein that is widely involved in biological processes such as autophagy, signal transduction, and oxidative stress response. Downregulating p62 can induce cervical cancer cells apoptosis.9 In addition, p62 engages in interactions with a diverse array of molecules, including mitogen-activated protein kinase kinase 3 (MEKK3), neighbor of BRCA1 gene 1 (Nbr1), receptor-interacting protein 1 (RIP1), regulatory-associated protein of mTOR (Raptor), tumor necrosis factor receptor-associated factor 6 (TRAF6), autophagy marker LC3, Kelch-like ECH-associated protein 1 (Keap1), ubiquitin, and numerous others. As a result, p62 significantly impacts diverses signaling pathways such as inflammation, mTORC1, and nuclear factor-κB (NF-κB).10 Importantly, aberrant expression of p62 can disrupt the normal functionality of the Nrf2 pathway,11,12 which is closely associated with the progression of cervical lesions. Furthermore, studies have indicated that p62 is overexpressed in various malignant tumors and contributes to cancer progression.13 However, the diagnostic value of Nrf2 and p62 in cervical cancer and intraepithelial lesions has not been previously reported, and their correlation in different cervical lesions is not well understood.
Immunohistochemistry (IHC) serves as a highly valuable tool in differentiating between normal, preinvasive, and invasive cervical lesions by detecting the expression patterns of specific biomarkers. In normal cervical epithelium, IHC can identify the characteristic expression patterns of various proteins that maintain normal cellular function. CIN lesions often show abnormal expression of key biomarkers. One of the most well-known is p16INK4a. In normal cervical tissue, p16INK4a is either not expressed or only weakly expressed. However, in CIN, especially high-grade CIN, there is strong, diffuse nuclear and cytoplasmic staining of p16INK4a. In invasive cervical cancer, IHC can detect multiple markers that are associated with the aggressive behavior of cancer cells. For squamous cell carcinoma, the expression of p63, a transcription factor, is often retained, which helps in differentiating it from other types of carcinomas. In conclusion, incorporating p62 immunohistochemistry in the analysis of Nrf2 is an absolute necessity. By simultaneously examining the expression patterns of Nrf2 and p62 through immunohistochemistry, we can gain a more comprehensive and in - depth understanding of the complex molecular mechanisms underlying cervical cancer and intraepithelial lesions. This integrated approach will enable us to elucidate how these two factors interact and collaborate in the context of cervical disease, ultimately providing more valuable insights for accurate diagnosis and effective treatment strategies.
In conclusion, this study aims to detect the expression of Nrf2 and p62 in cervical cancer and intraepithelial lesions, analyze their correlation, and ultimately assess their diagnostic value in these conditions.
Methods
Study Population
Paraffin specimens were collected from the Yichang Central People’s Hospital between January 2010 and December 2023. The collection included 125 cases of cervical squamous cell carcinoma (SCC), 109 cases of high-grade squamous intraepithelial lesions (HSIL), 97 cases of low-grade squamous intraepithelial lesions (LSIL), and 67 cases of benign or reactive squamous epithelium.
Reagents and Methods
Main Reagents
Monoclonal antibody Nrf2 (1:200, catalog number AB62352) was purchased from Abcam company. Monoclonal antibody p62 (1:200, catalog number 88588S) was purchased from CST company. Primary antibody diluent and Phosphate-Buffered Saline (PBS) were both purchased from Beijing Zhongshan Jinqiao Company. Secondary antibodies and chromogenic substrate were purchased from Dako company.
Immunohistochemistry
Paraffin sections, 4 μm in thickness, are placed in a 65°C incubator overnight to ensure proper processing. Following this, the sections undergo deparaffinization using xylene. Excess fluid is then removed through a graded series of ethanol washes: 100%, 95%, 85%, and 75%. Afterward, the sections are rinsed with distilled water to prepare them for antigen retrieval. The retrieval process involves the use of an EDTA solution at a pH of 9.0, which is applied under high pressure to facilitate the exposure of antigenic sites. Once the sections are ready, the primary antibody is added, and the samples are incubated at room temperature for 1.5 hours to allow for antibody binding. Subsequently, the secondary antibody is introduced, and the sections are incubated in a 37°C incubator for an additional hour to enhance the signal detection. The colorimetric development is achieved using 3,3′-diaminobenzidine tetrahydrochloride (DAB), which produces a visible color reaction at the site of antigen-antibody complex formation. After the color development, the sections are rinsed with tap water to remove any unbound DAB. To provide contrast and highlight cellular structures, the sections are counterstained with hematoxylin. Finally, the sections are sealed with a neutral resin to protect and preserve the immunohistochemical staining.
To demonstrate the specificity of the Nrf2 and p62 antibodies in immunohistochemical detection, negative and positive controls were included in the study.
Result Interpretation
Two pathology experts Cohen’s kappa coefficient between the two pathologists was 0.900 (95% CI: 0.823–1.000) independently reviewed and recorded the results. In cases where the results were inconsistent, a third expert made the final judgment. Nrf2 and p62 were considered positive if light yellow, brownish-yellow, or brownish particles were observed in the cytoplasm.
The scoring was based on two criteria:14 (1) staining intensity of positive cells: 0 points for no staining, 1 point for light yellow, 2 points for brownish-yellow, and 3 points for brownish; (2) the percentage of positive cells: less than 5% for 1 point, 5–30% for 2 points, more than 30–60% for 3 points, and more than 60% for 4 points.
Statistical Methods
SPSS 26.0 software was utilized for statistical analysis. The chi-square test was applied to compare Nrf2 and p62 expression between groups, with data presented as both numbers and percentages. Spearman’s rank correlation analysis was conducted to determine the correlation between Nrf2 and p62 within the groups. Binary logistic regression analysis and receiver operating characteristic (ROC) curves were employed to evaluate the diagnostic value of Nrf2 and p62 among the groups. A p-value of less than 0.05 was considered to indicate statistical significance.
Results
Expression of Nrf2 and p62 in Different Cervical Lesions
As shown in Figure 1 and Table 1, both Nrf2 and p62 are localized to the cytoplasm in different cervical lesions. The expression levels of Nrf2 and p62 in benign/reactive cervical squamous epithelium are lower than those in LSIL, HSIL, and SCC (chi-square values of Nrf2 are 46.41, 83.55, and 92.50, respectively; p62 are 17.39, 96.77, and 175.42, respectively, with all P<0.001). Furthermore, the expression of Nrf2 and p62 in LSIL is significantly lower than in HSIL and SCC (chi-square values of Nrf2 are 48.15 and 39.82, respectively; p62 are 103.18 and 181.36, respectively, with all P<0.001).
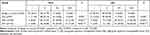 |
Table 1 Comparison of the Expression of Nrf2 and p62 in Different Cervical Lesions |
Although the expression of p62 in HSIL is lower than in SCC (x2=126.93, P< 0.05), there is no statistically significant difference in Nrf2 expression between HSIL and SCC (x2=3.37, P= 0.338).
Correlation of Nrf2 and p62 in Different Cervical Lesions
Nrf2 and p62 show positive correlation in benign/reactive cervical squamous epithelium, LSIL, HSIL, and SCC (all P<0.05) (Table 2).
 |
Table 2 Correlation Between Nrf2 and p62 in Different Cervical Lesions |
Diagnostic Efficacy of Nrf2 and p62 in Different Cervical Lesions
ROC curve analysis indicates that, except for Nrf2 in diagnosing HSIL and SCC, the differences are not statistically significant. The differences in Nrf2, p62, and combined Nrf2 and p62 in diagnosing benign/reactive squamous epithelium and LSIL, benign/reactive squamous epithelium and HSIL, benign/reactive squamous epithelium and SCC, LSIL and HSIL, LSIL and SCC, and HSIL and SCC are all statistically significant (all P<0.05). The combined use of Nrf2 and p62 is more effective in distinguishing these cervical lesions compared to using Nrf2 or p62 alone (Figure 2).
Discussion
Cervical cancer is one of the most common malignant tumors in women worldwide, and in recent years, the age of onset of cervical cancer in China has significantly decreased.15 The probability of cervical LSIL and HSIL progressing to SCC is 1% and 20%~40%, respectively.16,17 Currently, aside from human papillomavirus (HPV) genotyping and the p16INK4a gene, few other molecular markers are widely used in cervical cancer and precancerous lesions. However, p16INK4a positivity is not an absolute indicator for diagnosing HSIL. Therefore, finding more molecular markers to assist in the diagnosis of cervical cancer and precancerous lesions is crucial to avoid unnecessary surgical treatments that may increase the risk of miscarriage or preterm birth in women of childbearing age.
Nrf2 was initially regarded as a chemopreventive compound for cancer and other diseases. Subsequent research has shown that Nrf2 is not only a driving factor in the occurrence, metastasis, and drug resistance of various cancers but also plays new roles in regulating metabolism and other basic cellular functions.18 Studies have indicated the oncogenic role of Nrf2 in cervical cancer. In Uyghur women, cervical SCC and CIN are associated with increased Nrf2 expression and decreased Keap1 expression. Nrf2 is positively correlated with histological grade, lymph node metastasis, and tumor stage, whereas Keap1 is negatively correlated with these indicators. Nrf2 promotes the proliferation, migration, and invasion of cervical SCC cells while inhibiting apoptosis. Nrf2 is expected to be an indicator of poor prognosis in cervical cancer patients.6 Nrf2 and its downstream molecules NQO1 and heme oxygenase-1 (HO1) are expressed at varying levels in cervical tumor tissues. Knocking out Nrf2 in cervical cancer CaSki cells significantly reduces the expression of its downstream genes and promotes chemotherapy drug-induced cell death. Additionally, in vivo experiments have confirmed that cisplatin combined with Nrf2 knockout further inhibits tumor growth.7 In this study, we also found that Nrf2 is overexpressed in cervical SCC compared to benign/reactive cervical squamous epithelium. Additionally, Nrf2 can effectively distinguish between benign/reactive cervical squamous epithelium and LSIL or between LSIL and HSIL. Notably, Nrf2 expression in SCC and HSIL is higher than in benign/reactive cervical and LSIL, but Nrf2 expression in SCC is similar to that of HSIL. The specific reason remains to be discovered in future studies.
Several previous studies suggest that a positive feedback loop exists between Nrf2 and p62. The accumulation of p62 can activate Nrf2 and its downstream target genes, and Nrf2 can directly bind to the antioxidant response element (ARE) sequence in the promoter region of p62 to regulate its expression.19,20 Researchers have found that knocking down p62 significantly reduces cervical cancer cell viability, increases apoptosis, and induces reactive oxygen species. Moreover, knocking out p62 in cervical cancer cells significantly decreases Nrf2 expression,21 confirming their correlation at the cellular level. Currently, the correlation between Nrf2 and p62 in cervical tissues is unclear. This study found a positive correlation between Nrf2 and p62 in benign/reactive cervical squamous epithelium, LSIL, HSIL, and SCC. We further confirmed their correlation at the tissue level. The correlation between Nrf2 and p62 is not only confirmed in cervical tissues; our earlier studies found that Nrf2 and p62 can mutually regulate and positively correlate with each other in breast cancer cells and tissues, inducing breast cancer drug resistance.14 Similarly, the correlation between Nrf2 and p62 has been confirmed in hepatocellular carcinoma and pancreatic ductal adenocarcinoma, thereby inducing tumorigenesis and progression.22,23
As a signal transduction protein, p62 not only coordinates the metabolic reprogramming of cancer cells but also regulates the function of normal cells within the tumor to support tumor growth and proliferation. Increasing evidence shows that p62 is abnormally expressed in various cancers, such as lung cancer, liver cancer, kidney cancer, colorectal cancer, breast cancer, and gastric cancer.24,25 Chen et al26 found that p62 expression varies among invasive cervical cancer, CINII/III, CINI, and normal cervix, and increases with disease severity. The elevated p62 expression might be an early event in the transition from pre - invasive to invasive cervical cancer, as we observed a step-wise increase in p62 expression from normal to pre-invasive and then to invasive lesions. This study also found that p62 expression is lowest in benign/reactive cervical squamous epithelium, followed by LSIL, HSIL, and highest in SCC. In the context of invasive cervical cancer, p62 may play a crucial role in promoting cancer cell survival and proliferation. It has been reported that p62 can activate the NF-κB pathway.27 Activation of NF-κB is known to upregulate the expression of anti - apoptotic genes, which could contribute to the survival of cancer cells in the face of various stressors. Moreover, p62 has been associated with autophagy dysregulation in cancer.28 In normal cells, p62 is degraded through autophagy. However, in invasive cervical cancer, the overexpression of p62 may disrupt normal autophagic flux. We detected a decrease in the co-localization of p62 with autophagosome markers in invasive cancer cells, indicating a potential block in autophagic degradation of p62. This dysregulation could lead to the accumulation of damaged proteins and organelles, further promoting cancer cell growth and invasion.
ROC curve analysis shows that p62 can effectively distinguish between benign/reactive cervical squamous epithelium, LSIL, HSIL, and SCC. Compared to using Nrf2 or p62 alone, the combined use of Nrf2 and p62 is more effective in distinguishing these different cervical lesions. In terms of diagnostic performance for pre- invasive cervical lesions, p16/Ki67 co-expression has been widely used as a reliable biomarker panel.29 Strong and diffuse p16INK4a staining, along with increased Ki67-positive cell proliferation, is highly indicative of high-grade CIN.30 In contrast, our combined analysis of Nrf2 and p62 showed a different pattern. While Nrf2 expression gradually increased from normal to pre-invasive and invasive lesions, p62 also demonstrated a similar trend but with a distinct expression pattern in terms of sub-cellular localization. In pre-invasive lesions, the combination of Nrf2 and p62 did not show as clear-cut a diagnostic pattern as p16/Ki67. However, in some cases where p16/Ki67 results were equivocal, the Nrf2/p62 combination might offer additional insights. For example, in a small subset of low-grade CIN cases with uncertain p16/Ki67 staining, we found that high Nrf2 nuclear expression along with elevated cytoplasmic p62 could be associated with a more advanced pre - invasive state.
Our study has several strengths despite the single - hospital sample origin. The long - term sample collection from 2010 to 2023 within one hospital offers advantages. It enables an in - depth look at cervical lesion progression over time. The consistent medical environment and diagnostic procedures in a single hospital reduce data-collection variability. Immunohistochemistry, combined with descriptive and comparative analyses, gives detailed cell - level insights. We can accurately identify changes in Nrf2 and p62 expression across different cervical lesion stages, providing valuable knowledge about disease - related biological processes.
Nonetheless, our study has significant limitations. The sample is sourced solely from a single hospital. This severely restricts the diversity of the patient population, as it may not represent the broader spectrum of cervical lesion patients in different geographical, ethnic, and socioeconomic backgrounds. Without a sample size calculation, the statistical power of our study remains uncertain, and there is a risk of insufficient sample representativeness. The interpretation of immunohistochemistry results is subject to inter - observer variability, and the absence of a standardized scoring system further challenges result reproducibility. Moreover, factors like patient lifestyle, comorbidities, and family cancer history, which could impact biomarker expression, were not comprehensively considered, limiting the generalizability of our findings. Hence, expanding sample collection to multiple hospitals and diverse patient populations in future studies.
Conclusion
In summary, Nrf2 and p62 are expressed differently in various cervical lesions, with no or low expression in benign/reactive squamous epithelium, increased expression in LSIL, and highest expression in HSIL and SCC. Both show a positive correlation in different cervical lesions and either alone or in combination can effectively diagnose different cervical lesions. Nrf2 and p62 are expected to become molecular markers for clinical diagnosis of cervical lesions, similar to p16INK4a.
Data Sharing Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding authors.
Ethics Statement
The utilization of these data was conducted with the approval of the ethics committee at Yichang Central People’s Hospital. Informed consent was obtained from the patients or their close relatives (when a patient has passed away), as well as from healthy individuals who served as controls. This study strictly adheres to the ethical guidelines outlined in the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work supported by Hubei Province Natural Science Foundation Yichang Innovation and Development Joint Fund (2024AFD189) and Yichang City Science and Technology Plan Projects (2022KZL2-03).
Disclosure
All authors have no competing interests to report.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Qi J, Li M, Wang L, et al. National and subnational trends in cancer burden in China, 2005–20: an analysis of national mortality surveillance data. Lancet Public Health. 2023;8(12):e943–e955. doi:10.1016/S2468-2667(23)00211-6
3. Revathidevi S, Murugan AK, Nakaoka H, Inoue I, Munirajan AK. APOBEC: a molecular driver in cervical cancer pathogenesis. Cancer Lett. 2021;496:104–116. doi:10.1016/j.canlet.2020.10.004
4. Liu Y, Lang F, Yang C. NRF2 in human neoplasm: cancer biology and potential therapeutic target. Pharmacol Ther. 2021;217:107664. doi:10.1016/j.pharmthera.2020.107664
5. Jenkins T, Gouge J. Nrf2 in cancer, detoxifying enzymes and cell death programs. Antioxidants. 2021;10(7):1030. doi:10.3390/antiox10071030
6. Ma J-Q, Tuersun H, Jiao S-J, Zheng J-H, Xiao J-B, Hasim A. Functional role of NRF2 in cervical carcinogenesis. PLoS One. 2015;10(8):e0133876. doi:10.1371/journal.pone.0133876
7. Ma X, Zhang J, Liu S, Huang Y, Chen B, Wang D. Nrf2 knockdown by shRNA inhibits tumor growth and increases efficacy of chemotherapy in cervical cancer. Cancer Chemother Pharmacol. 2012;69(2):485–494. doi:10.1007/s00280-011-1722-9
8. Osman NATAG, Abd El-Maqsoud NMR, El Gelany SAA. Correlation of NQO1 and Nrf2 in female genital tract cancer and their precancerous lesions (Cervix, Endometrium and Ovary). World J Oncol. 2015;6(3):364–374. doi:10.14740/wjon931w
9. Liu T, Zhou Y, Chen L, et al. Splicing factor PTBP1 silencing induces apoptosis of human cervical cancer cells via PI3K/AKT pathway and autophagy. Front Biosci. 2024;29(8):289. doi:10.31083/j.fbl2908289
10. Shi J, Wong J, Piesik P, et al. Cleavage of sequestosome 1/p62 by an enteroviral protease results in disrupted selective autophagy and impaired NFKB signaling. Autophagy. 2013;9(10):1591–1603. doi:10.4161/auto.26059
11. Luo X, Tai Q, Liu X, et al. SQSTM1/p62 confers resistance of intrahepatic cholangiocarcinoma cells to 5-Fluorouracil by promoting Nrf2 nuclear translocation. Mol Cellular Toxicol. 2025:1–11.
12. Foster A, Scott D, Layfield R, Rea SL. An FTLD-associated SQSTM1 variant impacts Nrf2 and NF-κB signalling and is associated with reduced phosphorylation of p62. Mol Cell Neurosci. 2019;98:32–45. doi:10.1016/j.mcn.2019.04.001
13. Hennig P, Fenini G, Di Filippo M, Karakaya T, Beer H-D. The pathways underlying the multiple roles of p62 in inflammation and cancer. Biomedicines. 2021;9(7):707. doi:10.3390/biomedicines9070707
14. Wei Y, Liu D, Jin X, et al. PA-MSHA inhibits the growth of doxorubicin-resistant MCF-7/ADR human breast cancer cells by downregulating Nrf2/p62. Cancer Med. 2016;5(12):3520–3531. doi:10.1002/cam4.938
15. Wang J, Zheng C-X, Ma C-L, et al. Raman spectroscopic study of cervical precancerous lesions and cervical cancer. Lasers Med Sci. 2021;36(9):1855–1864. doi:10.1007/s10103-020-03218-5
16. Kanthiya K, Khunnarong J, Tangjitgamol S, Puripat N, Tanvanich S. Expression of the p16 and Ki67 in cervical squamous intraepithelial lesions and cancer. Asian Pac J Cancer Prev. 2016;17(7):3201–3206.
17. Kawashita S, Matsuda K, Kondo H, et al. Significance of p53-binding protein 1 nuclear foci in cervical squamous intraepithelial lesions: association with high-risk human papillomavirus infection and P16INK4a expression. Cancer Control. 2020;27(1):1073274819901170. doi:10.1177/1073274819901170
18. Rojo de la Vega M, Chapman E, Zhang DD. NRF2 and the hallmarks of cancer. Cancer Cell. 2018;34(1):21–43. doi:10.1016/j.ccell.2018.03.022
19. Schmidlin CJ, Shakya A, Dodson M, Chapman E, Zhang DD. The intricacies of NRF2 regulation in cancer. Semin Cancer Biol. 2021;76:110–119. doi:10.1016/j.semcancer.2021.05.016
20. Zhang W, Feng C, Jiang H. Novel target for treating Alzheimer’s diseases: crosstalk between the Nrf2 pathway and autophagy. Ageing Res Rev. 2021;65:101207. doi:10.1016/j.arr.2020.101207
21. Bian S, Zhao Y, Li F, et al. Knockdown of p62/sequestosome enhances ginsenoside Rh2-induced apoptosis in cervical cancer HeLa cells with no effect on autophagy. Biosci Biotechnol Biochem. 2021;85(5):1097–1103. doi:10.1093/bbb/zbab019
22. Saito T, Ichimura Y, Taguchi K, et al. p62/Sqstm1 promotes malignancy of HCV-positive hepatocellular carcinoma through Nrf2-dependent metabolic reprogramming. Nat Commun. 2016;7:12030. doi:10.1038/ncomms12030
23. Todoric J, Antonucci L, Di Caro G, et al. Stress-activated NRF2-MDM2 cascade controls neoplastic progression in pancreas. Cancer Cell. 2017;32(6):824–839.e8. doi:10.1016/j.ccell.2017.10.011
24. Tao M, Liu T, You Q, Jiang Z. p62 as a therapeutic target for tumor. Eur J Med Chem. 2020;193:112231. doi:10.1016/j.ejmech.2020.112231
25. Kim JS, Bae GE, Kim K-H, et al. Prognostic significance of LC3B and p62/SQSTM1 expression in gastric adenocarcinoma. Anticancer Res. 2019;39(12):6711–6722. doi:10.21873/anticanres.13886
26. Chen M, Ai G, Zhou J, Mao W, Li H, Guo J. circMTO1 promotes tumorigenesis and chemoresistance of cervical cancer via regulating miR-6893. Biomed Pharmacother. 2019;117:109064. doi:10.1016/j.biopha.2019.109064
27. Amit S, Ben-Neriah Y. NF-κB activation in cancer: a challenge for ubiquitination- and proteasome-based therapeutic approach. Semi Cancer Biol. 2003;13:15–28. doi:10.1016/S1044-579X(02)00096-2
28. Verma AK, Bharti PS, Rafat S, et al. Autophagy paradox of cancer: role, regulation, and duality. Oxid Med Cell Longev. 2021;2021:8832541. doi:10.1155/2021/8832541
29. Erozan YS. The Bethesda system for reporting cervical cytology. Acta Cytologica. 2004;48(5):770. doi:10.1159/000326441
30. Miralpeix E, Genovés J, Maria Sole-Sedeno J, et al. Usefulness of p16(INK4a) staining for managing histological high-grade squamous intraepithelial cervical lesions. Mod Pathol. 2017;30(2):304–310. doi:10.1038/modpathol.2016.168
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



