Back to Journals » Journal of Pain Research » Volume 18
Five-Step Knee Adjustment Manipulation Based on the ‘Muscle and Bone Balance’ Principle for Treating Knee Osteoarthritis: Study Protocol for a Randomized Controlled Trial
Authors Da W , Liu S, Qian Q, Zhu B, Chen L, Xue F, Sun P, Xue C, Xue Y, Yang J, Du W, Ding C, Shi Q, Li X
Received 12 November 2024
Accepted for publication 12 March 2025
Published 2 April 2025 Volume 2025:18 Pages 1775—1791
DOI https://doi.org/10.2147/JPR.S502187
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Michael A Ueberall
Weiwei Da,1,2,* Shuang Liu,1,* Qing Qian,1,* Baocai Zhu,1,* Lin Chen,1,* Fan Xue,1 Pan Sun,1 Chunchun Xue,1,2 Yongpeng Xue,1 Jiafan Yang,1 Wenlan Du,1 Chao Ding,1 Qi Shi,1,2 Xiaofeng Li1,2
1Department of Orthopedics and Traumatology, Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 2Qi Shi’s Studio of Famous Chinese Medicine Physician, Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaofeng Li, Email [email protected]
Background: Knee osteoarthritis (KOA) is the leading cause of knee joint dysfunction. Manual therapy (MT) can decrease patients’ levels of pain and improve their functionality. But most traditional methods focus solely on the knee joint or its surrounding tissues, neglecting the impact of the waist, hip, ankle, and lower limb alignment on KOA. The objective is to clarify the effects of the five-step knee adjustment manipulation on KOA, evaluate its efficacy, and explore new treatment approaches for manual KOA therapy.
Methods: (1) 45 healthy volunteers will be recruited to observe the differences in lower limb alignment, quadriceps cross-sectional area, knee joint range of motion (ROM), and gait between healthy individuals and KOA participants. (2) Conduct a multi-center, randomized, single-blind, controlled clinical trial. 120 eligible participants will be included and randomly assigned to a five-step knee adjustment manipulation (FS) group or a sham manipulation (SM) group with a ratio of 1:1. Each group will receive 2 sessions per week applied for 4 weeks and then be followed up for another 8 weeks. The primary outcome is visual analogue scale (VAS). The secondary outcomes include Western Ontario and McMaster Universities Arthritis Index (WOMAC) score, ROM, quadriceps cross-sectional area (CSA), gait analysis, and so on.
Conclusion: This technique emphasizes a holistic approach, addressing the lumbar spine, hip, knee, and ankle joints, as well as related muscle groups, to correct lower limb alignment and restore muscle and bone balance. We think it will contribute to providing a promising alternative intervention for middle-aged and older adults with KOA.
Trial Registration: The study was approved by the Ethics Committee of Shanghai Municipal Hospital of Traditional Chinese Medicine (Ethics No.: 2024SHL-KY-70-01). Registered in Chinese Clinical Trial Registry (No. ChiCTR2400085536).
Keywords: manipulation treatment, knee osteoarthritis, limb alignment, multi-center, muscle and bone balance
Introduction
Background and Rationale
As Osteoarthritis Research International defined osteoarthritis: The disease manifests first as molecular derangement (abnormal joint tissue metabolism) followed by anatomic, and/or physiologic derangements (characterized by cartilage degradation, bone remodeling, osteophyte formation, joint inflammation and loss of normal joint function), which can culminate in illness, osteoarthritis causes considerable social and economic impacts in the world.1 The knee is a commonly affected joint. Nearly 30% of individuals over the age of 45 have radiologic evidence of knee osteoarthritis (KOA), and about half of these people experience knee symptoms.2 Numerous authors have investigated the roles of age, obesity, inflammation, trauma, genetic factors, and musculoskeletal changes in patients with knee osteoarthritis (KOA). However, these studies have primarily focused on alterations in the lower extremity. Recently, knee joint disorders have been linked to changes in spinal alignment, a phenomenon now referred to as knee-spine syndrome.3 Although there is a range of studies demonstrated that progression of knee osteoarthritis or stiff knees were associated with the imbalance of sagittal pelvic-spinal system, the causal relationship between the two is not yet clear.4–6
Conservative treatments such as manual therapy (MT) have demonstrated improvements in pain and physical function for KOA.7,8 Regular manual therapy (MT) can effectively mobilize tight myofascial thigh structures, enhancing outcomes such as increased quadriceps muscle cross-sectional area and improved soft tissue biomechanics.9,10 Furthermore, regular MT may help address impaired joint kinematics, facilitating greater knee mobility with reduced effort, restriction, and pain.11,12 However, the techniques primarily target the knee joint itself and often fail to address spinal and pelvic instability. In line with the knee-spine syndrome paradigm, a holistic approach targeting the pelvic-spinal-lower extremity system could not only attenuate the progression of knee osteoarthritis, but also mitigate the severity of pelvic-spinal imbalance, which may have better long-term effects.
Objectives
Based on the theory of knee-spine syndrome, we developed a five-step knee adjustment manipulation designed to address holistic biomechanical imbalances in the spine, hips, knees, and ankles. This approach treats the knee joint by activating and relaxing key muscles in each region while simultaneously adjusting the corresponding joints. And there is now extensive observational evidence supporting the contention that biomechanical balance is particularly important in the prevention and treatment of KOA.13 So, we believe this approach may show promise in improving functional outcomes and mitigating osteoarthritis progression compared to regular MT, which typically address only localized structural issues. However, the effectiveness of the five-step knee adjustment manipulation has not yet been established, and further research is needed to confirm these preliminary findings.
Consequently, this study seeks to evaluate the effectiveness of our five-step knee adjustment technique in reducing pain, enhancing WOMAC scores, range of motion, CSA of quadriceps and gait mechanics in patients with KOA. We aim to demonstrate the potential superiority of our method in achieving better functional outcomes and quality of life improvements for patients.
Methods
Study Design
This study protocol outlines a two-arm, randomized, single-blind, multicenter clinical trial with a sham manipulation control. A total of 120 KOA patients aged between 40 and 70 years and classified as Kellgren and Lawrence (KL) gradesII–III will be recruited from three hospitals. The protocol for this trial will adhere to rigorous standards as outlined in the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT)14 guidelines. Additionally, the reporting of trial results will follow the Consolidated Standards of Reporting Trials (CONSORT)15 guidelines. The participants will be randomly assigned in a 1:1 ratio to either the treatment group (Five-step knee adjustment manipulation, Biw) or the control group (sham manipulation, Biw). Meanwhile, another 45 healthy volunteers will be included as baseline comparisons to observe the differences in lower limb alignment, quadriceps CSA, knee joint ROM, and gait compared to KOA patients (Figure 1). Outcomes will be recorded and assessed at the 2nd, 4th, 6th, 8th, 12th and 24th weeks following the initial treatment.
 |
Figure 1 Participant Flowchart. Abbreviation: FS Group, five-step knee adjustment manipulation, SM Group, regular knee manipulation group. |
Study Participants
The trial will be conducted at the Department of Orthopedics, Shanghai Municipal Hospital of Traditional Chinese Medicine, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, and Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, located in Shanghai, China.
Participants diagnosed with KOA according to the criteria in the 2021 “Guidelines for the Diagnosis and Treatment of Osteoarthritis”16 by the Rheumatology Branch of the Chinese Medical Association.17 The enrolled participants will be evaluated for eligibility by professional physicians, who will be asked to sign a written informed consent after voluntarily agreeing to participate.
Eligibility Criteria
The inclusion criteria were as follows: X-ray examination demonstrating Kellgren-Lawrence grade II or III osteoarthritis;18 age between 40 and 70 years, regardless of gender; diagnosis of unilateral knee osteoarthritis, regardless of left or right knee involvement; Visual Analog Scale (VAS) score for knee osteoarthritis joint pain ≥3 points and ≤8 points (score range: 0–10 points); willingness to provide informed consent and complete the research protocol as outlined.
The exclusion criteria were as follows: participants with previous knee surgery; participants with acute inflammation or infection around the knee joint; pregnant women; participants with tumors, infections, immune system-related diseases, or poorly controlled diabetes, hypertension, heart disease; participants who took anticoagulants, steroids, immunosuppressants, or other drugs within 3 months before treatment; participants with severe osteoporosis.
Interventions
A total of 120 eligible KOA participants will be randomly divided into “five-step knee adjustment manipulation” (FS) group and regular manual therapy group with sham manipulation (SM) for waist, hip, and ankle, respectively at a ratio of 1:1. Healthy volunteers will not receive any intervention. Both therapies are developed based on “Tuina”19 and “Tuina manipulation”.20
FS Group
The 60 participants in the FS group will be treated with the “five-step knee adjustment manipulation” twice a week for four consecutive weeks. The specific procedure is as follows:
Step 1: Posterior Muscle Activation
① Waist-Hip: Use the left or right palm root to perform a rhythmic spiral movement on the waist muscles (erector spinae muscles) on the opposite side of the affected limb. Follow this by using the elbow pressure method on the waist muscles from top to bottom, holding each point for 2 seconds. While pressing on the buttocks from center to outside on the affected side, holding each point for 1 second. Repeat the manipulation 3–5 times for each position separately, approximately 2 min.
② Lower limb: Use the left or right palm root to knead from the biceps femoris to the heel 2–3 times. Then press the biceps femoris with the elbow from top to bottom 3–5 times, holding each position for 1 second. Pressing around the popliteal fossa and rubbing the hamstrings with the thumb 2–3 times. The triceps surae is grasped and pinched from the popliteal fossa to the heel 3–5 times, approximately 1 min.
Step 2: The Knee and Ankle Joints Adjustment
① Knee joint: Hold the popliteal fossa with the left hand and the middle arch with the right hand. Then right hand drives the calf into extreme external rotation through the arch, extends and everts the dorsum of the foot, left hand fixes the popliteal fossa while pressing firmly in the straight position. Repeat the manipulation 3–5 times, approximately 2 min.
② Ankle joint: Use one hand and five fingers to grasp and knead the interior and exterior sides of the ankle joint, sole of foot, and the transverse and longitudinal arch, followed by extending and everting the foot for 3–5 times, approximately 1 min.
Step 3: Anterior Muscle Activation
Thigh-Calf muscles: Knead and press on the quadriceps, the lateral iliotibial band, the adductor muscles, and the tibialis anterior from top to bottom with palm root and elbow separately for 3–5 times, approximately 2 min.
Step 4: Patellar Releasing Manipulation
① Patellar lifting: Grab and pinch the patella with one hand and five fingers and fix the knee joint with the other hand. Then lift the patella upward to the maximum extent for 3–5 times, approximately 1 min.
② Patellar releasing: Push the patella in four directions (up, down, right and left) with one hand palm root, and fix the knee joint with the other hand. Two hands exert force in opposite directions to stretch the patella 5–10 times, approximately 1 min. Otherwise, hold the patella with the thumb and four fingers of both hands to push the patella to move in four directions.
③ Squeezing infrapatellar fat pad: The participant lies prone with the knee semi-flexed. The therapist wraps their hands around the knee joint, with the thumbs overlapping, and places in the joint gap at the lower pole of the patella. The four fingers of both hands hold the inner and outer sides of the knee joint, respectively. While the participant slowly straightens the knee joint, the thumbs continue to press the infrapatellar fat pad vertically until the knee joint is fully straightened. Repeat the manipulation 3–5 times, approximately 1 min.
Step 5: Adjust the Hip Joint
① Relaxing the hip joint: The therapist holds the popliteal fossa of the affected limb with one hand and the lower end of the tibia with the other hand, then rotates the hip joint clockwise and counterclockwise 5 times respectively with the hip and knee flexed.
② Stretching the adductor muscles: The hip and knee of the affected limb are flexed, then abducted and externally rotated. The outer ankle is placed on the opposite thigh, crossing the legs to form a “4” shape. The therapist uses the ipsilateral hand to press down on the affected side knee and the other hand to stabilize the pelvis on the opposite. Repeat the manipulation 3 times, approximately 1 min. Do not use too much force.
③ Lower limb muscles and joints activation: The therapist stabilizes the knee joint with one hand and holds the ankle with the other hand. The participant straightens the knee joint from the hip and knee flexion position, while the hand holding the ankle provides a certain amount of resistance. Repeat the manipulation 3–5 times, approximately 1 min.
④ Stretching the posterior muscles of the lower limb: The therapist uses one hand to reach around the affected side of the popliteal fossa to stabilize the front of the knee joint, while holding the front of the sole of the foot with the other hand. Raising the affected leg straight to the maximum and dorsiflexing the affected foot to stretch the posterior muscles for 3 times, approximately 1 min.
SM Group
The sham manipulation for 60 KOA participants will be treated twice a week for four consecutive weeks. The methods are as follows:
Step 1: Active Joint Manipulation
① Pressing acupoints: Unlike the overall muscle stimulating manipulation used in the first step intervention of the treatment group, the sham group only selected a few acupoints for stimulation. These acupoints21 include EX-LE04 (Neixiyan), ST35 (Dubi), GB34 (Yanglingquan), SP9 (Yinlinquan), SP10 (Xuehai), ST34 (Liangqiu), BL40 (Weizhong), BL57 (Chengshan), and Ashi acupoints around the knee joint (Table 1). Press the above acupoints in turn for 5 times, approximately 2 minutes. While kneading BL40 (Weizhong) and BL57 (Chengshan) with one hand, the other hand is only placed on the waist and buttocks on the opposite side of the affected limb, no manipulation is done, which is used as a sham technique to compare the first step intervention of the treatment group.
 |
Table 1 Locations of Acupoints for Regular Knee Manipulation |
② Joint Activation: Pluck around the knee joint for 3–5 times, approximately 3 minutes.
Step 2: The Knee Joint Adjustment
① Relaxation knee joint: Only use the rolling and palm kneading around the knee joint to relax, then focus on the painful area and perform manipulations for 3–5 times, approximately 2 minutes.
② Knee joint adduction and abduction: The participant flexes the hip and knee to 90 degrees. The therapist holds the popliteal fossa with one hand and the ankle with the other hand. Then shake the knee joint left and right for 6–7 times under the state of pulling and traction of the knee joint, approximately 3 minutes. The sham manipulation without knee and ankle joint adjustment, which is used as a sham technique to compare the second step intervention of the treatment group.
Step 3: Muscles relaxation
Quadriceps femoris: Gently knead the quadriceps femoris with just using five fingers, approximately 3 minutes. And there is no manipulation on the lateral iliotibial band, the adductor muscles, and the tibialis anterior, which is used as a sham technique to compare the third step intervention of the treatment group.
Step 4: The Patellar Adjustment
① Knead the affected knee with a palm, only rub around the patella and both sides of the knee joint until the participant feels warm inside the joint, which is used as a sham technique to compare the fourth step intervention for the treatment group.
② After the two palms rub against each other to generate heat, place one palm above the patella and hold the ankle with the other hand for about 2 minutes. The patient does not engage in knee or ankle joint resistance exercises, but only relaxes muscles and promotes blood circulation through the heat of the palms, which is used as a shame technique to compare the fifth step intervention for the treatment group.
Step 5: Adjust the Hip and Knee Joint
① The sham manipulation step: Only drive the slight movement of the hip joint by shaking the knee joint left and right, without performing rotational movements of the hip-ankle joint and antagonistic movements of the adductor muscles, which is used as a sham technique to compare the second and fifth step intervention for the treatment group.
② Knee joint flexion and extension: To fully flex and extend the knee joint for 5 times, approximately 2 minutes. The manipulation should be gentle and slow to avoid further damage to the synovial tissue.
Criteria for Discontinuing or Modifying Allocated interventions
Participants will be excluded if they meet the following conditions, and the reasons for withdrawing will be asked and recorded in case report forms (CRFs).
(1) Participants who cannot strictly follow the treatment course.
(2) Participants who take drugs or any other therapies prohibited by the protocol during the observation period.
Strategies to Improve Adherence to interventions
Participants will receive two free X-rays, 3D gaits analyses, and one free MRI examination: one during their initial enrollment and another at the final follow-up, while health volunteers also receive the same free examination during their first visit. All assessments, treatments, and rehabilitation guidance for participants are provided free of charge. The research assistant will be responsible for contacting the participants for follow-up and answering any research-related questions from the participants.
Relevant Concomitant Care Permitted or Prohibited During the Trial
During the trial period, no other Chinese or Western drugs for osteoarthritis and no other treatment methods are allowed, except for the regulated intervention methods. If analgesic drugs are used for KOA, outcome evaluations will be delayed until 3 days after discontinuation of medication to assess its impact.
Provisions for Post‑trial Care
Participants could choose health education and functional exercise guidance post trial that suited their individual needs and goals. Participants also could choose alternative treatments such as acupuncture, poultices, intra-articular glucocorticoid injections, or surgery if they were not satisfied with the efficacy of the current treatment.
Outcomes
The efficacy of the intervention will be evaluated based on main and minor indicators by two independent research assistants, who are blinded to the group allocation. Endpoints will be recorded and assessed on the 2nd, 4th, 6th, 8th, 12th and 24th week after initial treatment (Figure 2).
Baseline
The eligible participants’ general condition, including gender, group type, age, weight, and treatment history of the disease, will be recorded in CRF. The research assistants will complete the primary and secondary outcomes assessment before the first treatment.
Primary Outcome
VAS
The VAS22 scale ranges from 0 to 10 points, with 0 (starting point) representing no knee pain, and 10 (end point) representing unbearable severe knee pain. The participant will use the VAS scale to select the most severe degree of knee pain experienced in the past week.
Secondary Outcomes
WOMAC
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)23 was developed by Bellamy and colleagues in 1988. It is a scoring system specifically designed for assessing hip and knee joint inflammation, which evaluates the structure and function of the knee joint based on pain, stiffness, and daily joint activity function.
Swelling Score
① No Swelling (0 point):24 No visible or palpable swelling in the joints.
② Mild Swelling (1 point): Slight swelling, lighter skin texture over the joints, and bone landmarks remain visible and palpable.
③ Moderate Swelling (2 points): Swelling is more prominent, with minimal skin texture visible, and bone landmarks are not easily distinguishable.
④ Severe Swelling (3 points): Significant swelling, skin appears tight and stretched, and bone landmarks are not visible or palpable.
Range Of Motion (ROM)
The ROM25 denotes the maximum arc achievable during joint movement and is fundamental in assessing limb function. In orthopedic practice, a goniometer is commonly used to quantify ROM, typically expressed in degrees. Methodology: ① The participant assumes a prone position with the knee fully extended and relaxed. ② The stationary arm of the goniometer aligns with the greater trochanter of the femur, while the movable arm aligns with the lateral malleolus of the fibula. ③ The participant actively flexes the knee, while the observer records the degree of flexion until the end range of motion is reached.
15 Meters Fast-Paced Walk Time
The 15-meter walking time26 measurement is a valuable tool for assessing the impact of osteoarthritis on joint function and walking ability in the hip, knee, and ankle joints. This test provides a comprehensive evaluation of the effects of pain and inflammation on mobility. A stopwatch was utilized to measure the time it took the participant to walk a straight distance of 15 meters at their fastest comfortable speed.
Three-Dimensional Gait Analysis
Equipment and Parameters27
The Smart-D 3D gait analysis system (BTS, Italy) was employed for this study. This system comprises an independent gait analysis laboratory featuring a 10-meter-long walkway situated centrally within the laboratory. The walkway is equipped with two force plates for measuring ground reaction forces. Additionally, the system includes eight high-resolution infrared cameras positioned around the walkway to capture three-dimensional motion data. Three high-definition cameras are strategically placed to provide additional visual context.
Operation Method
① Environmental Preparation: To close all doors and windows, remove all luminous objects from the laboratory and maintain a room temperature of 25°C.
② System Calibration: Prior to testing, ensure proper calibration of the system to accurately identify and calibrate the force plates, infrared cameras and video cameras.
③ Participant Measurement: Measure the participant’s height, weight, pelvic width, length of both lower limbs, knee width, and ankle width. Then input the measured anthropometric data into the Smart-D three-dimensional gait analysis system.
④ Marker Placement: Affix body surface markers (infrared reflection fluorescent beads) at specific anatomical landmarks, including the seventh cervical spinous process, bilateral acromion, bilateral anterior superior iliac spines, median upper edge of the sacrum, bilateral greater trochanter of the femur, and bilateral heels.
Use elastic bands to secure a small stick with an infrared reflection fluorescent ball at the distal end to the middle of the bilateral thighs and the outside of the middle of the calves, ensuring parallel alignment to the ground. There are 22 marking points in total.
⑤ Static Model Establishment: Instruct the participant to stand still on the force plate with raised head and chest, looking forward, and maintaining a standard standing posture for 5 seconds. Utilize the Davis KK three-dimensional model to capture various parameters of the participant during static standing and establish a static model.
⑥ Dynamic Gait Analysis: After establishing the standing static model, remove the fluorescent markers from the heels and instruct the participant to walk naturally at their normal speed and habits along a 10-meter trail within the laboratory. Ensure the participant is familiarized with the environment before initiating data recording. Record gait analysis images as the participant walks, ensuring each foot step on a force plate. Collect data from three repetitions to establish a dynamic walking three-dimensional model for further analysis.
Axial Alignment of the Lower Extremity
The axial alignment of the lower extremity28 will be assessed on the full-length, anteroposterior and lateral radiographs of the lower limbs. Include the inferior angle of the femur, the superior angle of the tibia, the medial proximal tibial angle (MPTA) and the distal femoral lateral angle (LDFA) will be measured by an experienced orthopedic doctor.
Cross Sectional Area (CSA)
The affected mid-thigh will be scanned using MRI, with a cross-sectional slice thickness set to 5 mm. After acquiring the MRI images, the cross-sectional areas29 of the quadriceps and biceps femoris muscles, along with fatty infiltration will be analyzed on axial T2-weighted images using the Motic Images Advanced 3.0 testing system software, which was developed by Motic Industrial Group Co., Ltd.
Biomechanical Elastic Parameters of Soft Tissues
To measure the elasticity of soft tissues30 around the knee joint, will be use Shear Wave Elastography (SWE). The observation indicators include the elastic modulus values of the quadriceps femoris (rectus femoris, vastus medialis, vastus lateralis), patellar tendon, and hamstrings (semitendinosus, semimembranosus, biceps femoris).
The Aixplorer Real-time Shear Wave Elastography Ultrasound Diagnostic device (Supersonic Imaging, France) will be used, equipped with a 50 mm L4-15 linear array ultrasound probe, operating at a frequency range of 4–15 MHz. The ultrasound machine will be set to musculoskeletal mode with a measurement range of 0–300 kPa. The examination room temperature will be maintained at 25°C, and patients rested for 5 minutes before the examination.
Locations
① Patellar tendon: From the patellar apex to the tibial tuberosity.
② Rectus femoris: At the junction of the middle and lower third of the line between the anterior superior iliac spine and the midpoint of the patellar base.
③ Vastus lateralis: At the lower third of the line between the anterior superior iliac spine and the lateral edge of the patellar base.
④ Vastus medialis: At the junction of the middle and lower third of the line between the anterior superior iliac spine and the medial edge of the patellar base.
⑤ Semimembranosus: At the junction of the middle and lower third of the line between the midpoint of the gluteal crease and the midpoint of the popliteal crease.
⑥ Semitendinosus: On the posterior medial side of the thigh, intersecting the line through the gluteal muscle and the midpoint of the popliteal crease at the junction of the middle and lower third.
⑦ Biceps femoris: On the posterior lateral side of the thigh, parallel to the semitendinosus muscle.
Operation Methods
① The participant assumes a prone position with the hip joint in neutral rotation and the knee joint fixed at 30 degrees of flexion using a brace. Meanwhile, measurements of the knee extensor group and patellar tendon are taken.
② An experienced sonographer with over 10 years of ultrasonography experience performs both gray-scale and elastic ultrasound on the patellar tendon and knee extensors. To ensure good contact between the probe and the skin, an adequate amount of gel will be used. Initially, a conventional two-dimensional ultrasound examination was conducted with a uniform depth setting of 3–4 cm. The patellar tendon and extensors will be scanned longitudinally along the tendon and muscle. Then, the elastography mode will be activated, and the rectangular region of interest will be set to the system’s maximum size of 13.5×12.5 mm. When measuring the elastic modulus using the Q-box quantitative analysis system, the Q-box diameter will be adjusted according to the thickness of the tendon or muscle. The system automatically calculates the average, maximum, and minimum elastic modulus values (kPa) of the tendon and muscle within the Q-box region. The average elastic modulus will be selected for statistical analysis. For hamstring measurements, the participant remains in the prone position with the knee joint naturally extended. The ultrasound examination will be performed similarly to the prior measurements.
Participant Timeline
The schedule of enrollment, interventions, assessments, and participant visits are shown in Figure 2. The research assistant will arrange the next treatment or follow-up appointment with the participant and notify them 1–2 days in advance via phone or WeChat.
Sample Size
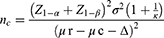
This study was designed with the Visual Analog Scale (VAS) score as the primary outcome indicator to assess pain levels. The control group received regular manipulation therapy for KOA. Based on our previous small sample case observation, we anticipate this difference to be maintained at the 12-week follow-up, with the VAS score of the control group improving by 1.78 points, while the treatment group will improve by 3.39 points. The following statistical parameters were used for the study design: unilateral α (type I error rate) = 0.25, β (type II error rate) = 0.1, standard deviation (σ) = 1.32, Δ = 1/2 of the standard deviation. The ratio of the number of cases in the experimental group to the control group (K) = 1.
The following formula was used to calculate the required sample size for each group:
nr= Knc
The initial sample size was n=35 per group. Considering a 20% shedding rate, and three research centers, with central factors, the sample size was increased to 60 cases in the FS group and 60 cases in the SM group. Then 40 participants per center (20 in the treatment group and 20 in the control group). Additionally, 45 healthy volunteers were included in the study. Each center is responsible for 15 healthy volunteer cases.
Recruitment
Recruitment posters for the study will be posted in prominent locations in the Shanghai Municipal Hospital of TCM outpatient clinic. In addition, the recruitment advertisements will be posted on Shanghai Municipal Hospital of TCM’s official WeChat public account to reach a wider audience and increase visibility.
Assignment of Interventions: Allocation
Sequence Generation
A total of 120 eligible participants will be randomly allocated in a 1:1 ratio to either the FS group or the SM group. The randomization method was undertaken by the Statistics Group of the Clinical Evaluation Center of Shanghai Municipal Hospital of TCM. The randomization was concealed using a central control scheme. After each center enrolled participants, it obtained a random number from the Clinical Evaluation Center and then carried out treatment interventions based on the random number.
Concealment Mechanism
The randomization program and list, comprising the code, randomization number, and treatment regimen for each participant, will be concealed in an opaque envelope. The administration of the randomization process will be overseen by the Clinical Evaluation Center.
Implementation
The Clinical Evaluation Center will inform the manipulation therapists about the participant’s randomization number and treatment group by text or WeChat.
Assignment of Interventions: Blinding
Who Will Be Blinded
While the manipulation therapists will not be blinded to interventions due to they have to know which intervention they use for participants, the participants, outcome evaluators and biostatisticians will be blinded to group details.
Procedure for Unblinding if Needed
The following situations will be unblinded and the specific reasons will be recorded in the CRF:
(1) When the study and data analysis are completed.
(2) Participants actively or passively withdraw from the study. (As shown in 11b).
Data Collection and Management
Plans for assessment and collection of outcomes
Specialized research assistants, who are blind to the allocation, will assess the primary and secondary outcomes at the timepoints during the study (Figure 2). Research assistants at each center will receive standardized training in outcome measurement and assessment before the start of the study.
Plans to promote participant retention and complete follow-up
We will provide professional rehabilitation guidance for participants during the later stages of the study. Additionally, the dedicated individual will be responsible for answering participants’ daily questions. Finally, the transportation subsidy of participants who complete the follow-up will be paid.
Data Management
The data collection work is the responsibility of two independent research assistants. The data entry adopts the double input method, and all patient-related data will be stored confidentially. Once data extraction and statistical analysis are completed, the CRFs will be securely locked in the research office cabinet and managed by the research organizer. All assistants will receive a training course before conducting the study.
Confidentiality
We will strictly protect all participants’ private information in accordance with the law and will not use participants’ identities, phone numbers, or contact addresses for any commercial purposes. Anyone who wishes to access the patients’ original medical records must obtain permission from the research sponsor and regulatory authorities.
Plans for Collection, Laboratory Evaluation and Storage of Biological Specimens for Genetic or Molecular Analysis in This Trial/Future Use
N/A. No biological specimens will be collected in this study.
Statistical Methods
All analyses will follow the intention-to-treat principle, analyzing each participant according to their randomized treatment assignment. Non-compliance with treatment requirements and withdrawals will be ignored in the preliminary analysis. Missing data will not be included in the initial analysis. If data are assumed to be missing at random, the multiple imputation method will be used to handle the missing data. Epidata V3.1 will be used for data input. All statistical tests were two-sided, and p < 0.05 indicated that the difference tested was statistically significant. The specific statistical analysis included three parts: (1) baseline data analysis; (2) efficacy analysis; (3) safety analysis. Data conforming to a normal distribution will be expressed as mean ± standard deviation ( ). The treatment effect data within the same group over time will be analyzed using one-way ANOVA for continuous measurements. If statistical significance is found, the Least Significant Difference (LSD) test will be used for pairwise comparisons. Differences in treatment effects between groups will be analyzed using one-way ANOVA. If statistical significance is found, the LSD test will be used for between-group comparisons. All analyses will be performed using SPSS 26.0, with a test level of α = 0.05 and p < 0.05 as statistically significant.
). The treatment effect data within the same group over time will be analyzed using one-way ANOVA for continuous measurements. If statistical significance is found, the Least Significant Difference (LSD) test will be used for pairwise comparisons. Differences in treatment effects between groups will be analyzed using one-way ANOVA. If statistical significance is found, the LSD test will be used for between-group comparisons. All analyses will be performed using SPSS 26.0, with a test level of α = 0.05 and p < 0.05 as statistically significant.
Interim Analyses
N/A. Previous research findings, coupled with our clinical treatment observations, suggest that manipulation can effectively relieve the symptoms of KOA. Additionally, due to the minimal incidence of advent effects and complications associated with manipulation, the interim analysis was deemed unnecessary.
Methods for Additional Analyses (eg Subgroup Analyses)
N/A. The primary aim of this study is to evaluate the difference in the efficacy of two manipulation techniques for KOA.
Methods in Analysis to Handle Protocol Non-Adherence and Any Statistical Methods to Handle Missing Data
We will use imputation to handle missing values:
(1) If the missing attribute value is numeric, it will be filled in using the average value of that attribute from all other objects.
(2) If the missing attribute value is non-numeric, it will be filled in using the most frequent value of that attribute from all other objects, following the majority principle in statistics.
Plans to Give Access to the Full Protocol, Participant Level-Data and Statistical Code
The protocol for this study is publicly available at the China Registered Clinical Trial Registration Center (ChiCTR2400085536). CRF data will be shared on the clinical trial public management platform ResMan (www.medresman.org.cn) after the trial ends.
Oversight and Monitoring
Composition of the Coordinating Center and Trial Steering Committee
The trial steering committee, comprising the senior supervisor, the Clinical Research Center director, and the ethics committee, who will offer essential monitoring and daily support throughout the trial.
Composition of the Data Monitoring Committee, Its Role and Reporting Structure
The entire process of this trial will be supervised by three-level monitors. The first-level monitor, composed of researchers with manipulation technology certification, will be responsible for the entire progress of the study. The second-level monitor, composed of researchers from the ethics committee, will be responsible for supervising the study. The third-level monitor, composed of data supervisors, will ensure the authenticity of the data. Given that no problems harmful to the participants are expected, no interim analysis will be conducted.
Adverse Event Reporting and Harms
Adverse event (AE) recording and reporting methods
AE that occurs during the study may not necessarily have a causal relationship with treatment, but the severity of symptoms, time of occurrence, duration, and treatment measures should be recorded in the CRF, and their relevance to the experimental treatment method should be evaluated and followed up. The classification of adverse events is recorded according to the CTCAE43.0 five-level scoring system.
Treatment of serious adverse events (SAE)
SAE refers to events that cause death, permanent or significant disability, permanent damage to organ function, or result in hospitalization or prolonged hospitalization. The researcher should immediately take necessary measures to ensure the safety of the subject in the event of an SAE. and must report the SAE to the sponsor and the ethics committee within 24 hours. If the SAE requires emergency unblinding, the clinical trial center and the blind editor should jointly perform the unblinding. The researcher will then decide on further treatment measures based on the unblinded information.
Frequency and Plans for Auditing Trial Conduct
Both the ethics committee and data supervisor will review the progress of the study and the authenticity of the data biannually.
Plans for Communicating Important Protocol Amendments to Relevant Parties (eg Trial Participants, Ethical Committees)
Any modification of the protocol must be approved by the study organizer, the ethics committee, and the clinical research center. Additionally, all modifications must be updated in the clinical research registration center.
Dissemination Plans
Upon completion of the research, the results will be published as articles in both domestic and international journals.
Discussion
At present, the occurrence of knee osteoarthritis is believed to be related to abnormal joint biomechanics caused by abnormal muscle fascia.31 The sagittal spine-pelvis-lower extremity alignment can be significantly affected by spinal disorders, hip osteoarthritis and knee instability. Abnormal sagittal alignment has been identified as a contributor to the pathogenesis of low back pain and patellofemoral joint pain.6 The lumbar spine, hip joint, knee joint, and ankle joint form a biomechanical unit. Muscle imbalance or bone deformity in the knee joint can disrupt the overall balance of the lower limbs and affect other joints. Although manual treatment for KOA has been included in the “Guidelines for the Diagnosis and Treatment of Osteoarthritis (2018 Edition)”32 and its effectiveness has been confirmed,33,34 the exact mechanism of action has not yet been fully elucidated.
The axial alignment of the lower extremity refers to the line extending from the center of the femoral head to the center of the ankle joint. The knee joint acts as the central axis of movement, connecting the hip and ankle joint.35 Degeneration of the knee joint can cause abnormal axial alignment of the lower extremity, leading to changes in the biomechanical load-bearing patterns of the hip and ankle joints. This can further exacerbate the progression of knee joint degeneration.
The most important muscles around the knee joint span two joints. For example, the quadriceps femoris and the hamstrings (biceps femoris, semiteninosus, and semimembranosus) cross both the hip and knee joints. The gastrocnemius originates from the back of the medial and lateral condyles of the femur and inserts at the calcaneus, crossing both the knee and ankle joints. This creates a biomechanical linkage mechanism among the hip, knee, and ankle joints.36 Therefore, the coordinated movement of the hip-knee-ankle axial is essential for maintaining the normal axial alignment and functional activity of the lower limbs.37 Weakness in any part of the joint can lead to the gradual degeneration of the structure and function of other joints.38,39 Long-term abnormal mechanical axis will further exacerbate the occurrence and progression of KOA. Additionally, the lumbar spine, pelvis, and hip joint play a crucial role in regulating and maintaining the body’s mechanical balance.40,41 The unbalance of the lumbar spine in the sagittal and coronal position will affect the dynamic balance of lower limbs through the pelvis.42 Hence, degeneration of any joints and muscles, or changes of spinal-pelvic parameters that can disrupt the axial alignment and form a vicious cycle that further affects the knee joint.43 Tsuj et al44 proposed the concept of ‘knee-spine syndrome, suggesting that low back pain and patellofemoral joint pain are caused by changes in spinal alignment (such as lumbar lordosis) that alter thigh muscle tension and axial alignment of knee when standing. The clinical studies have confirmed a significant positive correlation45 between the spinal inclination angle and the occurrence of KOA. In recent years, the concept of treating both the waist and knees has gained increasing attention in the context of KOA. Studies have shown that improving the abnormal state of the muscle related to the lower limbs has a significant positive effect on KOA.46,47 Manipulation therapy can relieve muscle spasms, restore muscle strength, and reestablish the normal mechanical balance between the muscles and bones around the knee joint.48 The specific mechanism may be that manual therapy improves the biomechanical properties and strength of lower limb’s soft tissues. This, in turn, indirectly restores the abnormal stress patterns of the knee joint, enhances the joint stability, and reduces the load within the joint. Consequently, this alleviates knee joint symptoms and improves the range of motion and function in a short time.49 So, five-step knee adjustment manipulation is straightforward to perform, safe, effective, and well-accepted by patients, making it well-suited for widespread clinical adoption. We also believe that after quickly adjusting and restoring the balance between tissues such as the spinal-pelvic, joints and muscles through our manipulation, patients still need to maintain the functional exercise of their own muscle groups to achieve better long-term efficacy.
Conventional Tuina techniques primarily focus on treating the local knee joint and surrounding soft tissues. Therefore, this study based on the principle of muscle-bone balance, employs the five-step knee adjustment manipulation to adjust the axial alignment of entire structure from the waist-hip-knee-ankle and the activity of key muscles. But we will not include the KOA individuals for KL grade 1 and 4, due to mild degeneration in these patients often responds robustly to any intervention, limiting the ability to discern specific treatment effects. And end-stage degeneration typically requires surgical intervention, and conservative therapies (like manual therapy) show limited long-term efficacy, which falls outside this study’s purposes. Thus, the study aims to improve muscle-bone balance and the mechanical load-bearing pattern, offering a new perspective for the treatment of KL grade II and III osteoarthritis.
However, this study does have certain limitations. First, blinding of manual interventionists could not be implemented due to the nature of the hands-on intervention. Second, although we provide rehabilitation guidance during the follow-up process, we cannot guarantee that all participants will adhere to proper knee joint care and exercise regimens. This variability in adherence may influence the final outcomes. Third, current research and our findings could confirm a correlation between pelvic-spinal system and the severity of knee osteoarthritis, but the causal relationship between the two remains unclear. Future research should aim to determine whether lumbar and hip degeneration contribute to knee osteoarthritis or vice versa, thereby providing more targeted guidance for clinical diagnosis and treatment.
Authors’ Information
1. Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, 274 Zhijiangzhong Road, Shanghai, 200071, China.
2. Qi Shi’s Studio of Famous Chinese Medicine Physician, 274 Zhijiangzhong Road, Shanghai 200032, China.
Abbreviations
KOA, Knee osteoarthritis; VAS, Visual analogue scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; SWE, Shear Wave Elastography; ROM, Range of motion; CSA, Cross Sectional Area; AE, Adverse event; SAE, Serious adverse event; TCM, Traditional Chinese medicine; CRF, Case report form.
Data Sharing Statement
The data and analysis results will be available from the corresponding author upon reasonable request after the completion of the study.
Ethics Approval and Consent to Participate
The trial follows strictly the guidelines of the Declaration of Helsinki (Version 2000). The design and methodologies of this study have been approved by the ethics committee of Shanghai Municipal Hospital of Traditional Chinese Medicine with an ethics approval (NO. 2024SHL-KY-70-01.) and registered in the Chinese Clinical Trial Registry (ChiCTR2400085536). Written informed consent will be obtained from all participants prior to their enrolment in the study.
Acknowledgment
The authors would like to express their gratitude for all the supervisors, investigators, outcome assessors, and participants in this trial.
Author Contributions
Weiwei Da, Shuang Liu, Qing Qian, Baocai Zhu and Lin Chen have contributed equally to this work and share first authorship. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Medical Innovation Project of Shanghai Science and Technology Commission (No. 22Y11922500); Traditional Chinese Medicine Science and Technology Development Project of Shanghai Medical Innovation & Development Foundation (No. WL-XJRY-2021003K); Shanghai Pujiang Program (24PJD101); Traditional Chinese Medicine Inheritance and Development Project of Shanghai Medical Innovation & Development Foundation (No. WLJH2021ZY-GZS001, ZLZX001). The sponsors, include Shanghai Science and Technology Commission and Shanghai Medical Innovation Development Foundation, Shanghai Municipal Human Resources and Social Security Bureau and Shanghai University of TCM, are not involved in the trial process, data collection, statistical analysis, and final results. This paper has been uploaded to Research Square as a preprint: https://www.researchsquare.com/article/rs-4683432/v1.
Disclosure
There is no potential conflict of interest among all authors in this study. All funding is only used for research related expenses, without any labor fees or salary expenses for the authors.
References
1. Kraus VB, Blanco FJ, Englund M, et al. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthr Cartilage. 2015;23(8):1233–1241. doi:10.1016/j.joca.2015.03.036
2. Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA. 2021;325(6):568–578. doi:10.1001/jama.2020.22171
3. Gunay Ucurum S, Kirmizi M, Umay Altas E, et al. Sagittal spinal alignment and mobility and their relation to physical function in women with and without mild-to-moderate knee osteoarthritis. J Biomech. 2023;146(146):111412. doi:10.1016/j.jbiomech.2022.111412
4. Kechagias VA, Grivas TB, Papagelopoulos PJ, et al. Investigation of the relationship between hip and knee osteoarthritis and disordered spinal and pelvic morphology. Cureus. 2022;14(1):e20861. doi:10.7759/cureus.20861
5. Young JJ, Krüger Jensen R, Hartvigsen J, et al. Prevalence of multimorbid degenerative lumbar spinal stenosis with knee or hip osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2022;23(1):177. doi:10.1186/s12891-022-05104-3
6. Pengfei F, Xu W, Pingcheng X, et al. Relationship between spinal imbalance and knee osteoarthritis by using full-body EOS. BMC Musculoskelet Disord. 2023;24(1):402. doi:10.1186/s12891-023-06508
7. Rhon DI, Flynn TW, Shepherd MH, et al. Leveraging the short-term benefits of manual therapy which includes exercise over exercise therapy alone appears justified for knee osteoarthritis. J Orthop Sports Phys Ther. 2023;53(1):49–50. doi:10.2519/jospt.2023.0201
8. Feng T, Wang X, Jin Z, et al. Effectiveness and safety of manual therapy for knee osteoarthritis: an overview of systematic reviews and meta-analyses. Front Public Health. 2023;11:1081238. doi:10.3389/fpubh.2023.1081238
9. Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev. 2011;19(2):82–92. doi:10.1097/JSA.0b013e318210c0aa
10. Andrew AA. Anterolateral knee biomechanics. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1015–1023. doi:10.1007/s00167-017-4494-x
11. Runge N, Aina A, May S. The benefits of adding manual therapy to exercise therapy for improving pain and function in patients with knee or hip osteoarthritis: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2022;52(10):613–675. doi:10.2519/jospt.2022.11062
12. Anwer S, Alghadir A, Zafar H, et al. Effects of orthopaedic manual therapy in knee osteoarthritis: a systematic review and meta-analysis. Physiotherapy. 2018;104(3):264–276. doi:10.1016/j.physio.2018.05.003
13. Taylor AL, Wilken JM, Deyle GD, et al. Knee extension and stiffness in osteoarthritic and normal knees: a video fluoroscopic analysis of the effect of a single session of manual therapy. J Orthop Sports Phys Ther. 2014;44(4):273–282. doi:10.2519/jospt.2014.4710
14. Chan A-W, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 Statement: defining standard protocol items for clinical trials. Rev Panam Salud Publica. 2015;38(6):506–514. doi:10.7326/0003-4819-158-3-201302050-00583
15. Anaesth SJ. The CONSORT statement. Sarah Cuschieri. 2019;13:S27–S30. doi:10.4103/sja.SJA_559_18
16. The Joint Surgery Branch of the Chinese Orthopaedic Association. Chinese guideline for diagnosis and treatment of osteoarthritis (2021 edition). Chin J Ortho. 2021;41(18):1291–1314. doi:10.3760/cma.j.cn121113-20210624-00424
17. The Rheumatology Branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of osteoarthritis. Chinese Journal of Rheumatology. 2010;14(06):416–419.
18. Kohn MD, Sassoon AA, Fernando ND, et al. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886–1893. doi:10.1007/s11999-016-4732-4
19. Fang M, Wang JG. National Traditional Chinese Medicine Higher Education “14th Five-Year Plan” Planning Textbook: Tuina. Beijing: China Press of Chinese Medicine; 2021.
20. Zhou YF. National Traditional Chinese Medicine Higher Education “14th Five-Year Plan” Planning Textbook: Tuina Manipulation. Beijing: China Press of Chinese Medicine; 2021.
21. Zhou YF. National Traditional Chinese Medicine Higher Education “13th Five-Year” Planning Textbook: Tuina Therapy. Beijing: China Press of Chinese Medicine; 2020.
22. Campbell WI, Lewis S. Visual analogue measurement of pain. Ulster Med J. 1990;59(2):149–152.
23. Angst F, Verra ML, Lehmann S, et al. Effects of inpatient rehabilitation in hip and knee osteoarthritis: a naturalistic prospective cohort study with intraindividual control of effects. Arch Phys Med Rehabil. 2013;94(11):2139–2145. doi:10.1016/j.apmr.2013.03.026
24. Hochberg MC, Martel-Pelletier J, Monfort J, et al. Combined chondroitin sulfate and glucosamine for painful knee osteoarthritis: a multicentre, randomised, double-blind, non-inferiority trial versus celecoxib. Ann Rheum Dis. 2016;75(1):37–44. doi:10.1136/annrheumdis-2014-206792
25. Szu-Ying W, Tsai Y-H, Wang Y-T. Acute effects of tissue flossing coupled with functional movements on knee range of motion, static balance, in single-leg hop distance, and landing stabilization performance in female college students. Int J Environ Res Public Health. 2022;19(3):1427. doi:10.3390/ijerph19031427
26. Bennell K, Dobson F, Hinman R. Measures of physical performance assessments: self-paced walk test (SPWT), stair climb test (SCT), six-minute walk test (6MWT), chair stand test (CST), timed up & go (TUG), sock test, lift and carry test (LCT), and car task. Arthritis Care Res. 2011;63(11):S350–70. doi:10.1002/acr.20538
27. Mukaino M, Ohtsuka K, Tanikawa H, et al.Clinical-oriented three-dimensional gait analysis method for evaluating gait disorder. J Vis Exp. 2018;(133):57063. doi:10.3791/57063
28. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–749. doi:10.2106/00004623-198769050-00016
29. Talpey SW, Axtell R, Gardner E, et al. Discriminative ability of lower limb strength and power measures in lacrosse athletes. Int J Sports Med. 2023;44(1):29–37. doi:10.1055/a-1870-4041
30. Flatres A, Aarab Y, Nougaret S, et al. Real-time shear wave ultrasound elastography: a new tool for the evaluation of diaphragm and limb muscle stiffness in critically ill patients. Crit Care. 2020;24(1):34. doi:10.1186/s13054-020-2745-6
31. O’neill TW, Felson DT. Mechanisms of osteoarthritis (OA) pain. Curr Osteoporos Rep. 2018;16(5):611–616. doi:10.1007/s11914-018-0477-1
32. Association CO. Guidelines for the diagnosis and treatment of osteoarthritis (2018 edition). Chin J Orthop. 2018;38(12):705–715.
33. Field T. Knee osteoarthritis pain in the elderly can be reduced by massage therapy, yoga and tai chi: a review. Complement Ther Clin Pract. 2016;22:87–92. doi:10.1016/j.ctcp.2016.01.001
34. Mingyu Z, Yizhou B, qi Z, et al. Evaluation on curative effects of tuina in treating knee osteoarthritis based on Pingle bonesetting ‘sinew stagnation and bone dislocation’ theory. China J Trad Chin Med Pharm. 2017;32(03):1372–1374.
35. Moon H-S, Choi C-H, Jung M, et al. The effect of knee joint rotation in the sagittal and axial plane on the measurement accuracy of coronal alignment of the lower limb. BMC Musculoskelet Disord. 2020;21(1):470. doi:10.1186/s12891-020-03487-9
36. Kubota K, Yokoyama M, Hanawa H, et al. Muscle co-activation in the elderly contributes to control of hip and knee joint torque and endpoint force. Sci Rep. 2023;13(1):7139. doi:10.1038/s41598-023-34208-6
37. Wheatley BB, Chaclas NA, Seeley MA. Patellofemoral joint load and knee abduction/adduction moment are sensitive to variations in femoral version and individual muscle forces. J Orthop Res. 2023;41(3):570–582. doi:10.1002/jor.25396
38. Iijima H, Shimoura K, Ono T, et al. Proximal gait adaptations in individuals with knee osteoarthritis: a systematic review and meta-analysis. J Biomech. 2019;87:127–141. doi:10.1016/j.jbiomech.2019.02.027
39. Charlton JM, Hatfield GL, Guenette JA, et al. Ankle joint and rearfoot biomechanics during toe-in and toe-out walking in people with medial compartment knee osteoarthritis. PM R. 2019;11(5):503–511. doi:10.1016/j.pmrj.2018.08.388
40. Dubousset J. Three-dimentional analysis of the scoliotic deformity. Ped Spine Prin Prac. 1994.
41. Pengfei W, Yaning L, Yufeng L, et al. Establishment of lumbar-pelvic-hip finite element model and biomechanical analysis. Chin J Tissue Engine Res. 2023;27(36):5741–5746. doi:10.12307/2023.708
42. Haddas R, Satin A, Lieberman I. What is actually happening inside the “cone of economy”: compensatory mechanisms during a dynamic balance test. Eur Spine J. 2020;29(9):2319–2328. doi:10.1007/s00586-020-06411-w
43. Tsuji T, Matsuyama Y, Goto M, et al. Knee-spine syndrome: correlation between sacral inclination and patellofemoral joint pain. J Orthop Sci. 2002;7(5):519–523. doi:10.1007/s007760200092
44. Fuqiang G, Feng L, Zhang K, et al. Hip-spine syndrome: the impact of hip pathology on lumbar spine alignment. Chin J Spine Spinal Cord. 2011;21(08):699–702.
45. Daoliang C. Clinical study on lumbar spine Tuina for the treatment of knee osteoarthritis. Chin Manipul Rehab Med. 2018;9(18):29–30.
46. Tanaka R, Umehara T, Kawabata Y, et al. Effect of continuous compression stimulation on pressure-pain threshold and muscle spasms in older adults with knee osteoarthritis: a randomized trial. J Manipulative Physiol Ther. 2018;41(4):315–322. doi:10.1016/j.jmpt.2017.09.011
47. Atkins DV, Eichler DA. The effects of self-massage on osteoarthritis of the knee: a randomized, controlled trial. Int J Ther Massage Bodywork. 2013;6(1):4–14. doi:10.3822/ijtmb.v6i1.119
48. Haibo W, Xuefeng G, Yongju Y, et al. Discussion on “knee is the junction of tendons and bones” and its application based on the theory of Zang-Xiang in traditional Chinese medicine. Liaoning J TCM. 2018;45(07):1396–1398.
49. Zlotnicki JP, Naendrup JH, Ferrer GA, et al. Basic biomechanic principles of knee instability. Curr Rev Musculoskelet Med. 2016;9(2):114–122. doi:10.1007/s12178-016-9329-8
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.