Back to Journals » Journal of Pain Research » Volume 18
Fu’s Subcutaneous Needling Combined with Kinematic Acupuncture versus Electroacupuncture in the Treatment of Cervical Spondylotic Radiculopathy: A Randomized Controlled Trial
Authors Lin Y, Hong W, Sui L, Jiang Q, Jiang G, Yan W, Xu N, Zhang R
Received 11 November 2024
Accepted for publication 30 January 2025
Published 12 March 2025 Volume 2025:18 Pages 1191—1204
DOI https://doi.org/10.2147/JPR.S498728
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Houman Danesh
Yingtong Lin,1,2,* Wanyi Hong,3,* Lili Sui,4 Qian Jiang,1 Ganghui Jiang,5 Weixin Yan,5,* Nenggui Xu,1,2,6,* Rui Zhang5,*
1Clinical Medical College of Acupuncture Moxibustion and Rehabilitation, Guangzhou University of Chinese Medicine, Guangzhou, People’s Republic of China; 2Guangdong Provincial Key Laboratory of Acupuncture and Moxibustion of Chinese Medicine, Guangzhou, People’s Republic of China; 3Shenshan Medical Center, Memorial Hospital of Sun Yat-Sen University, Shanwei, People’s Republic of China; 4First Clinical Medical School, Guangzhou University of Chinese Medicine, Guangzhou, People’s Republic of China; 5The First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, People’s Republic of China; 6South China Research Center for Acupuncture and Moxibustion of Guangzhou University of Chinese Medicine, Guangzhou University of Chinese Medicine, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Nenggui Xu, Email [email protected]
Background: Degenerative Cervical Myelopathy (DCM) is an overarching term that encompasses a broad spectrum of degenerative conditions affecting the cervical spine. Cervical Spondylosis Radiculopathy (CSR) represents a prevalent yet particularly severe type within the broader spectrum of Degenerative Cervical Myelopathy (DCM). Currently, conservative treatments, such as acupuncture, traction, physical therapy, and medication, are the standard methods used. As a widely applied physical therapy for musculoskeletal disease, Fu’s Subcutaneous Needling (FSN) therapy could be considered when choosing treatment interventions for complement. Electroacupuncture, a commonly used acupuncture treatment, has been proven effective by multiple studies. The comparative analysis with electroacupuncture is specifically aimed at assessing the potential advantages and therapeutic efficacy of FSN therapy in the management of CSR. This is particularly pertinent in instances where conventional conservative interventions and traditional acupuncture techniques may fall short in providing adequate symptom relief.
Methods: The study was a single-centered study without blinding. 80 eligible patients were randomly assigned into two groups, with 40 in each group. The study group received FSN combined with Kinematic acupuncture, the control group received electroacupuncture treatment.
Results: The results after treatment demonstrated that the study group had significantly higher scores in VAS (P=0.001), NPQ (P=0.000), NDI (P=0.000), TY (P=0.000), SF-36 (P=0.000), Hand-numbness (P=0.004), total effective rate (P=0.004) and Analgesic effect time (P=0.001) compared to the control group. The follow-up results also indicated that the experimental group outperformed the control group in VAS (P=0.000), NPQ (P=0.000), NDI (P=0.000), TY (P=0.000), SF-36 (P=0.000), however, the results of Hand-numbness scoring showed no significant statistical difference between both two groups (P=0.302), neither did Relieve duration (P=0.562).
Conclusion: In general, Fu’s Subcutaneous Needling combined with Kinematic acupuncture method is more effective in relieving symptoms and promoting recovery of CSR.
Trail Registration: The clinical trial has been registered at the Chinese Clinical Trial Registry (NO. ChiCTR2300068507).
Keywords: Fu’s Subcutaneous Needling, kinematic acupuncture, Cervical Spondylotic Radiculopathy, randomized controlled trial
A Letter to the Editor has been published for this article.
Introduction
Globally, degenerative cervical myelopathy (DCM) stands as the primary cause of spinal cord dysfunction among adults.1 This disease is characterized by chronic and progressive dysfunction stemming from degenerative alterations in the cervical spine, which encompass disc degeneration, osteophyte formation, ligament hypertrophy or ossification, among others.2,3 Such degenerative processes may result in the compression of the spinal cord or nerve roots. Specifically, when nerve root compression induces localized pain and sensory abnormalities, the resultant disease is defined as Cervical Spondylotic Radiculopathy (CSR).4 Cervical Spondylotic Radiculopathy is a clinical disease characterized by unilateral pain radiation and numbness in the upper limb.5 It is commonly associated with the degenerative changes in the cervical disc and intervertebral joint, which can cause mechanical compression. Additionally, the compression of the cervical nerve root vein congestion can stimulate the nerve root and cause pain.6 CSR is responsible for 60% to 70% of the overall incidence of cervical spondylosis, making it the most prevalent type.7 If the physiological curvature of the cervical spine remains altered for an extended period and is not corrected, local muscles in the neck will experience spasm and edema. This can lead to the cervical spine’s local decompensation, worsening its adverse effects on the normal function of the cervical spine and the blood vessels, as well as local nutrient metabolism, eventually leading to the dynamic and static imbalance of the cervical spine, thus causing a vicious cycle.8–10
Currently, conservative therapy and surgical treatment are the primary treatments for cervical CSR. While surgical treatment has demonstrated definitive effects, it is often associated with high risk, cost, and recurrence rates.11 As a result, conservative therapy, such as traction, physical therapy, and medication, is commonly preferred for CSR treatment.12–14 Existing research indicates that15–17electroacupuncture, a modality of acupuncture, has been extensively validated for its efficacy in managing CSR. This technique amplifies the therapeutic stimulation by introducing a microcurrent to the acupuncture needles. Through the precise stimulation of acupoints with filiform needles and the strategic application of pulsatile currents, electroacupuncture demonstrably mitigates cervical muscle spasms, curtails the permeation of inflammatory mediators, augments local blood flow, and dissipates hematomas, consequently alleviating the compressive symptoms affecting the nerve roots.18–20 FSN is a form of physical therapy that using disposable floating needles to sway in subcutaneous tissues of skin around specific MTrPs (also known as myofascial trigger point) or adjacent limbs. The objective is to improve the ischemic state of the affected muscles, eliminate MTrPs, and promote muscle tissue recovery.21 Furthermore, multiple clinical studies have found that FSN can effectively manage musculoskeletal pain with long-lasting effect.22–24 Similarly, Kinematic acupuncture therapy is based on the theory of “movement cortex stimulation therapy” that involves patients moving their affected area or related parts during needle stimulation to increase the stimulation and then enhance the treatment’s effectiveness.25 The diversity and multi-modal nature of conservative treatment for CSR are advantageous. Therefore, this study aims to explore the clinical efficacy and basis of FSN combined with Kinematic acupuncture in treating CSR, which may provide additional options and guidance for clinicians in treating CSR.
Methods
Trail Design and Participants
This study was conducted at a single clinic and was randomized, but not blinded, aimed to recruit 80 patients diagnosed with CSR from the Acupuncture and Rehabilitation Department of the First Affiliated Hospital of Guangzhou University of Chinese Medicine, between February 2023 to July 2024. While patients in the study group received FSN combined with Kinematic acupuncture, the control group underwent electroacupuncture treatment. All participants provided written informed consent prior to their involvement in the study.
The trial complies with the Declaration of Helsinki and this research plan has been reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine (NO. K-2022-080), and it was registered with the Chinese Clinical Trial Registry as ChiCTR2300068507, Feb 21st, https://www.chictr.org.cn/.
Diagnosis, Inclusion and Exclusion Criteria
Based on the “Standard for diagnosis and efficacy evaluation of traditional Chinese medicine syndromes and diseases” issued by the State Administration of Traditional Chinese Medicine in 1994,26 the diagnosis of CSR involvement should meet the following criteria: neck pain accompanied by upper limb pain, which worsens with neck extension; reduced sensation, muscle atrophy, abnormal tendon reflexes, and other indications in the area affected by the compressed nerve root; positive findings in the brachial plexus traction test (Eaton test) or neck compression test (Spurling test); cervical X-ray or CT imaging demonstrating narrowing of the nerve root canal.
Inclusion criteria: Inclusion requirements include patients who meet the above diagnostic criteria and are between the ages of 18 and 60, regardless of gender, have not received other treatment in the last three months, and demonstrate good compliance and willingness to participate in the study by signing the informed consent form.
Exclusion criteria: patients with CSR resulting from trauma or other causes, as well as patients with other types of cervical spondylosis such as myelocytic, sympathetic, and vertebral artery types. Patients with cognitive dysfunction or mental illness, severe cardiovascular, cerebrovascular, liver, or kidney dysfunction, and pregnant or lactating women were also excluded. Patients who were unwilling or unable to cooperate or complete the course of treatment due to other reasons were excluded. Additionally, those who had participated in any drug clinical trials in the six months prior to screening or were deemed unsuitable for the study by the researchers were excluded.
When it comes to the safety of subjects, participation in the study must be stopped as determined by the investigator if any of the following conditions arise: exacerbation of symptoms, occurrence of serious adverse events (such as pain, broken needle, fainting during acupuncture treatment, or infection), poor compliance, and the like.
Interventions
The study group underwent FSN combined with Kinematic acupuncture treatment using medium-sized disposable needles, produced by Nanjing Paifu Medical Technology Co., Ltd. During treatment, patients were seated and MTrP points and affected muscles were identified in the neck, shoulder, and forearm muscles.21 Procedure: To begin, identify the patient’s MTrP point and mark the needle entry point 5–10cm away from it. Then, thoroughly disinfect and sterilize the skin at the needle entry point. Proceed by selecting a disposable needle and swiftly piercing the skin at an angle of 15–20 degrees. Once inserted, manipulate the needle back and sway for 5 minutes using the needle point as a fulcrum. During this time, the patient should engage in reperfusion therapy (passive resistance exercise) under the guidance of the doctor. After 3–5 treatments in each affected area, the patient should stand up and perform active exercises such as cervical spine forward flexion and extension, left and right rotation, left and right lateral flexion, arm lifting, and shoulder lifting. Once the pain is significantly relieved or localized muscle stiffness has subsided, the needle core can be safely withdrawn. Place a hose under the skin and secure it with a transparent dressing. The patient should be advised on precautions to take to keep the tube in place and rest as needed. The hose can be removed four hours later by a qualified healthcare provider. Treatment should be repeated once every other day, for a total of three sessions in one course. Two courses are recommended for optimal results.
The control group received electroacupuncture treatment using stainless steel needles that were 0.30×25mm (1 inch) or 0.30×40mm (1.5 inches) in size with Tianzhu, Fengchi, Jianjing, Binao, Quchi, Hegu and Jiaji acupoints corresponding to the cervical vertebrae segment. The steps were as follows: Sterile disinfection treatment was carried out on the acupoint local skin, and millineedles were inserted to achieve “Deqi.” The G6805-2A electronic acupuncture treatment instrument was used for 10 minutes in dense wave mode followed by 20 minutes in disperse-dense wave mode with current intensity tolerated by the patient. Treatment was administered every other day for a total of three times per course. Two courses of treatment were observed. A one-month telephone follow-up was conducted after the treatment ended.
To evaluate the efficacy of both patient groups at three points in time, namely before treatment, immediately after treatment, and after follow-up.
Outcome Measures
Main Outcome Measures
The study utilized various outcome measures to evaluate the effectiveness of the treatment. The Visual analogue scale (VAS),27,28 Northwick Park (NPQ),29 and total effective rate were the primary measures. Patients were instructed to use the VAS score to indicate the severity of their pain on a 10cm ruler, where 1cm equaled 1 point. The higher the score, the more severe the pain. The NPQ score, which reflects the quality of life of patients with neck pain, also indicated the severity of the pain. The total effective rate was calculated in accordance with the “Standard for diagnosis and efficacy evaluation of traditional Chinese medicine syndromes and diseases”26 the Total Effective Rate = [number of (cure cases + remarkably effective cases + effective cases) / total number of cases] × 100%.
Secondary Outcome Measures
The Neck Disability Index (NDI),30 Tanaka Yasuhisa symptom scale(TY),31 SF-36 mental component summary,32 Hand-numbness score, Analgesic effect time and Relieve duration were used as secondary outcome measures. NDI measured cervical spine dysfunction, while TY assessed the severity of symptoms, signs, and hand function. The SF-36 scale assessed the quality of life of respondents, the Hand-numbness score reflected the degree of numbness experienced by patients, the scoring method for the Hand-numbness score was the same as that used for the VAS score.The Analgesic effect time recorded the time required from the start of treatment until the patient felt pain relief, and Relieve duration recorded the duration of pain relief after the patient received treatment, the data were continuously measured for a period of 7 days, and the average value of the 7-day period was utilized for data analysis.
Sample Size
Samples were collected from patients in both the ward and outpatient of Acupuncture and Rehabilitation Department of the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine between February 2023 and July 2024. Sample estimation was carried out using the following equation: n1= n2 = (Uα + Uβ)2 × P(1 - P) / (P1 - P2)2, with P= (P1×n1 + P2×n2) / (n1 + n2), P indicates the Total Effective Rate, P1 indicates the effective rate of study group, P2 indicates the effective rate of control group. For our study, we chose α=0.05, which corresponds to a probability of type 1 error (Uα=1.960), and β=0.2, which corresponds to a probability of type 2 error (Uβ=0.842). Referencing previous literature findings,33 if n1= 41, P1= 95.12%, n2= 40, P2= 80%. Combining the two groups, the total effective rate of P was 88%, and the minimum sample size for each group was determined to be 36, factoring in the potential maximum shedding rate of 20% and considering constraints around time, funding, and minimum sample size. Ultimately, we selected a final sample size of 80 cases.
Randomisation
Patients who met the inclusion criteria were recruited and sequentially numbered from 1 to 80 in the order of their visit and randomly assigned to two groups using statistical software SPSS 26.0, with each group comprising 40 patients (Y. L and W. H), and then made a card and place it inside an opaque, sealed envelope (Q. J). Write the corresponding number on the outside of the envelope (L. S). Label the patients based on their treatment and hand them the envelope with the matching number (G. J). This will determine their corresponding random number and group.
Statistic methods
Statistical analysis of the data was performed using SPSS 26.0 (IBM, USA). The data were tested Normal Distribution Test, and baseline differences between groups were analyzed using the homogeneity of variance method. For quantitative data (such as height, weight, age and scores in this study), Mean ± SD deviation was used, and homogeneity of data was determined by Independent Sample t-test. When there was non-conforming homogeneity of variance, Satterthwaite t-test was used. Quantitative data that did not meet the normal distribution were expressed through median and interquartile distance ([M (IQR)]), and the Wilcoxon signed rank test was used for nonparametric testing of differences between groups, the Mann–Whitney U-Test was used for nonparametric testing of differences between two groups. Qualitative data were expressed as a percentage (the Total Effective Rate), and the Chi-square Test was utilized to compare the differences between the two groups. It indicates that there is a statistically significant difference between the two groups when P<0.05.
Results
Participant Flow and Recruitment
The study evaluated 181 patients for a diagnosis of CSR, with 80 of them considered for inclusion. During the study, 117 patients were excluded (Figure 1). Finally, the data of 79 patients were analyzed, of which 39 were in the test group and 40 in the control group. One patient withdrew early due to being unable to tolerate the pain during the FSN course. Our study recruited 80 patients diagnosed with CSR from the Acupuncture and Rehabilitation Department of the First Affiliated Hospital of Guangzhou University of Chinese Medicine, between Feb 21st 2023 to July 21st 2024. And a follow-up survey was conducted two weeks after the end of the treatment.
 |
Figure 1 Process diagram of a randomized controlled trial of the efficacy of Fu’s Subcutaneous Needling combined with Kinematic acupuncture for treating Cervical Spondylotic Radiculopathy. |
Baseline Characteristic
There were no significant differences in general data (gender, age, height, weight, disease duration, and cervical joint mobility34) between the treatment and control groups (P>0.05). Furthermore, the clinical data between the two groups were comparable (refer to STable1).
Numbers Analysed
For study group, 39 participants included in analysis, for control group were 40. The analysis was by original assigned groups (Figure 1).
Outcomes and Estimation
Comparison of the Total Effective Rate Between the Two Groups
Table 1 presents a comparison of the total effective rate between the study and control groups. The study group showed a better overall efficacy at total effective rate of 97.44%, 95% CI: [0.865, 0.999] (38/39) compared to the control group at 75.00%, 95% CI: [0.588, 0.873] (30/40). The difference was statistically significant.
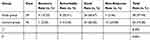 |
Table 1 Comparison of Total Effective Rates Before and After Treatment Between Both Groups |
Comparison of the Scoring Results Between the Two Groups
Prior to treatment, there were no significant differences (P>0.05) in VAS, NPQ, NDI, TY, SF-36, and hand numbness scores between the two groups, as demonstrated by STables 2 and 3. After the treatment, both groups experienced significant improvement (P<0.05), which indicated that both groups were effective (Table 2 and Figure 2). The study group exhibited considerable progress in all scores compared to the control group, with a statistically significant difference (P<0.05). Specifically, concerning SF-36 scores, the study group surpassed the control group in elevating the scores for bodily pain, vitality, social function, and health transition, with a significant difference (P<0.05). Physical functioning, general health, role emotional, and mental health scores, however, did not differ significantly (P>0.05), as illustrated by Figure 3 and Table 3. Moreover, regard to Analgesic effect time, the effective time of the treatment in study group was shorter than that in control group, with a statistically significant difference (P<0.05). For Relieve duration, Although the duration of remission in control group was relatively longer than that in study group, it did not differ significantly (P>0.05)(Figure 4 and Table 4).
 |
Table 2 Comparison of the Scoring Indicators Between the Two Groups (Mean±SD) |
 |
Table 3 Comparison of the SF-36 Score Indicators Between the Two Groups (Mean±SD) |
 |
Table 4 Comparison of the Time Indicators Between the Two Groups (Mean±SD) |
 |
Figure 2 Line chart for comparison of scoring indicators before and after treatment between the two groups. Note: *The difference was statistically significant (P<0.05). |
 |
Figure 3 Histogram for comparing the scoring indicators before and after treatment between the two groups (SF-36). |
 |
Figure 4 Comparison of the time indicators between the two groups. |
The results of the follow-up survey showed no significant differences (P>0.05) in VAS, NPQ, NDI, and TY scores between pre- and post-treatment scores within the group (refer to STable 2). This suggests that the therapeutic effects of both treatments on CSR pain symptoms and functional impairments did not decline significantly after treatment completion and remained stable However, the total SF-36 scores recorded post-treatment improved further during follow-up, indicating the continued betterment of patients’ overall health status (refer to STable 2-SF-36 total score), and this difference was statistically significant. Moreover, the study group exhibited greater improvement in VAS, NPQ, NDI, TY, and SF-36 total score than the control group during follow-up (refer to STables 2 and 3). However, for hand numbness score, the situation differed. In the study group, the difference between follow-up and treatment results was statistically significant (t3 Study group=−2.364, P3 Study group=0.023, P3 Study group<0.05), while in the control group, it was not significant (t3 Control group=1.778, P3 Study group=0.083, P3 Study group>0.05) (refer to STable 2-Numbness).
Harms
The potential harms and adverse events that arose in this trial include: a. pain resulting from needle puncture; b. needle breakage within the skin or body; c. syncope during acupuncture insertion; d. bleeding or subcutaneous hematoma; e. peripheral nerve damage caused by needle puncture; f. infection during the course of tube indwelling period. Apart from one woman in the study group who withdrew from the trial due to pain intolerance, no evident harms or adverse reactions were observed in the remaining patients.
Discussion
The proper curvature and movement of the cervical spine rely heavily on the strength and tone of the neck muscles. A decline in these qualities can result in abnormal motion and curvature of the spine, which negatively impact blood circulation and nutrient metabolism, as well as accelerating the pain of neck.8,9 This, in turn, can worsen cervical spine dysfunction. For this reason, it’s crucial to improve the soft tissue tension surrounding the cervical spine and restore its physiological curvature in order to reduce pain and nerve root compression symptoms.
FSN therapy for CSR targets the affected muscle (Figure 5). During the therapy, the needle insertion and swaying manoeuvre creates strong mechanical stimulation on the affected and surrounding connective tissues.21 This traction force helps relieve inflammatory adhesions, reduce inflammation, and enhance reperfusion therapy. By repeatedly relaxing and contracting the affected muscle, as well as indwell the hose at last, FSN therapy helps engorge it, improve its ischemic and hypoxia state, and ultimately prolong stimulation for better results. Studies indicate that FSN’s therapeutic mechanism is closely linked to the efficient conduction of bioelectricity within loose connective tissue.10,21,35,36 The swaying motion generates positive piezoelectricity, changing the liquid crystal nanostructure in the subcutaneous loose connective tissue.37,38 The bioelectric stimulation released by positive piezoelectricity produces a reverse piezoelectric effect when it reaches a specific lesion site via loose connective tissue. This effect modifies the local ion channel state, permeability of cell membranes, regulates cell function, alleviates muscle pain, and restores muscle function. Additionally, mechanical traction stimulates nerve endings present in the subcutaneous fascial layer, modulates pain, and improves local capillary and lymphatic circulation.39,40 In addition, it has also been proposed that FSN may activate the immune system’s repair mechanism by stimulating it.25 However, more research is still necessary to confirm this proposal.
 |
Figure 5 (A-D) Affected muscles. |
The study reveals that the treatment plan for the study group demonstrated notable effectiveness in alleviating neck pain, as well as relieving upper limb and finger pain caused by CSR, with shorter consuming time of analgesic effect and long-lasting, non-recurrent effects in comparison to the control group. Moreover, it demonstrates a positive impact on enhancing neck and upper limb activity function, as well as daily entertainment and social activities. Nevertheless, the treatment’s impact on diminishing hand numbness was moderately satisfactory, and despite demonstrating good efficacy post-treatment, it was challenging to maintain during follow-up, hinting towards patients possibly relapsing. Besides, the duration of analgesia in study group was not better than that in control group, suggesting that the treatment in study group does not have the advantage of extending the duration of analgesia, which indicated that the study group, despite exhibiting superior and faster efficacy, still maintained comparable duration of efficacy to the control group.
The overall superior efficacy of FSN therapy, as observed in this study, is potentially attributable to several factors. Firstly, despite the comparable duration of acupuncture sessions in both electroacupuncture and FSN (FSN: 3–5 treatments in each affected area, 5 minutes each; electroacupuncture: 25 minutes), the FSN therapy incorporates a 4-hour indwelling catheter post-needle extraction to consolidate and sustain the therapeutic effect. In contrast, electroacupuncture lacks this extended dwell time, resulting in more durable efficacy for patients undergoing FSN. Secondly, FSN therapy is complemented by the patient’s passive resistance movements, which differ significantly from the resting state maintained during electroacupuncture sessions. These active limb movements facilitate accelerated lymphatic and blood circulation in the affected areas, thereby alleviating pain and muscle tension caused by poor local blood flow and restoring muscle balance. Additionally, the choice of needles in both treatments varies significantly. The use of a thicker, firmer, and hollow long needle (0.60×52mm) for FSN, as opposed to the thinner needle (0.30×25mm or 0.30×40mm) used in electroacupuncture, leads to a broader stimulation and therapeutic range during acupuncture manipulation. Consequently, FSN can more rapidly improve the local microcirculation affected by nerve root compression and yielding therapeutic outcomes. Therefore, Compared to traditional electroacupuncture therapy, FSN therapy has a more comprehensive treatment range and stronger, longer-lasting stimulation, which effectively improves affected muscles. Originally, the reperfusion technique can be regarded as an innovative therapy of Kinematic acupuncture. FSN combined with Kinematic acupuncture promotes recovery by accelerating blood circulation around ischemic tissues through continuous contraction and relaxation compared to a relatively stationary state of the body. While the therapeutic efficacy of FSN has been substantiated, it is imperative to acknowledge that in instances of severe nerve compression, surgical intervention remains the primary treatment option, notwithstanding the high risks, costs, and potential for recurrence typically associated with surgery. Such surgical treatments should be undertaken without delay. In these cases, FSN therapy and other conservative therapies are more appropriately reserved for patients who are not eligible for surgery or can be utilized as complementary therapies to surgical treatment.
Above all, the study still has limitations, such as a lack of more objective efficacy indicators such as serum inflammatory factor levels and imaging changes (CT, MR or X-ray), and the Kinematic acupuncture method not quantify each active movement frequency and duration. Additionally, TCM typing for the included patients was not detailed enough. Therefore, this study still requires further detailed research in the future. During the follow-up period, the reasons that caused the recurring hand numbness symptoms in the study group remained unclear. It is necessary to conduct further research on the limitations of FSN therapy or the potential errors attributed to the insufficient sample size.
Conclusion
The study’s findings demonstrate that the utilization of FSN combined with Kinematic acupuncture and electroacupuncture, both of them can effectively alleviate symptoms in CSR patients, approach results in pain relief and improved numbness. Notably, FSN combined with Kinematic acupuncture produced superior therapeutic outcomes, serving as a valuable clinical reference for treating CSR. Therefore, the study results have practical application in clinical settings.
Abbreviations
FSN: Fu’s Subcutaneous Needling; CSR: Cervical Spondylosis Radiculopathy; MTrP: Myofascial trigger point; VAS: The Visual analogue scale; NPQ: Northwick Park; NDI: The Neck Disability Index; TY: Tanaka Yasuhisa symptom scale, SF-36: SF-36 mental component summary.
Data Sharing Statement
All data sets and research materials associated with this study have not been archived in any repositories or websites. However, interested parties may obtain these materials from the corresponding author upon making a reasonable request.
Ethics Approval and Consent to Participate
This study has obtained informed consent from all participants to participate in the clinical trial, and its protocol was reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine in Sep 2022 (No. K-2022-080). Additionally, the study was registered with the Chinese Clinical Trial Registry in Feb 2023 (No. ChiCTR2300068507).
Acknowledgments
We acknowledge The First Affiliated Hospital of Guangzhou University of Chinese Medicine for collecting the data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by a project of the Traditional Chinese Medicine Innovation Teams and Talents of the State Administration of Traditional Chinese Medicine (ZYYCXTD-C-202004), Nenggui Xu’s research on Acupuncture for Brain Diseases (Traditional Chinese Medicine A1-2601-24-415-109Z02), The Innovation Team Program of Universities in Guangdong Province (NO.2024KCXTD027), National Natural Science Foundation of China (No. 82430125 and 82204813), General Program of Guangdong Key Laboratory of Traditional Chinese Medicine and Acupuncture (No.04), Supported by Sanming Project of Medicine in Shenzhen (No.SZZYSM202311015), The open operating funds for key laboratories in Guangdong Province, Applied Basic Research Project of Guangzhou City (2023A04J1859), and 2024 Guangdong Provincial Key Research Platforms in Higher Education Institutions(2024KCXTD027).
Disclosure
The authors declare no competing interests in this work.
References
1. Badhiwala JH, Ahuja CS, Akbar MA, et al. Degenerative cervical myelopathy — update and future directions. Nat Rev Neurol. 2020;16(2):108–124. doi:10.1038/s41582-019-0303-0
2. Saunders LM, Sandhu HS, Mcbride L, et al. Degenerative cervical myelopathy: an overview. Cureus. 2023. doi:10.7759/cureus.50387
3. Tu J, Vargas Castillo J, Das A, et al. Degenerative Cervical Myelopathy: insights into Its Pathobiology and Molecular Mechanisms. J Clin Med. 2021;10(6):1214. doi:10.3390/jcm10061214
4. Davies BM, Mowforth ZOD, Smith EK, et al. Degenerative cervical myelopathy. BMJ;2018. k186. doi:10.1136/bmj.k186
5. Beckworth WJ, Abramoff BA, Bailey IM, et al. Acute cervical radiculopathy outcomes: soft disc herniations vs osteophytes. Pain Med. 2021;22(3):561–566. doi:10.1093/pm/pnaa341
6. Watkins RG. Cervical disc herniations, radiculopathy, and myelopathy. Clin Sports Med. 2021;40(3):513–539. doi:10.1016/j.csm.2021.03.006
7. Yang F, Li WX, Li UZ, et al. Balance chiropractic therapy for cervical spondylotic radiculopathy: study protocol for a randomized controlled trial. Trials. 2016;17(1):513. doi:10.1186/s13063-016-1644-2
8. Kim R, Wiest C, Clark K, et al. Identifying risk factors for first-episode neck pain: a systematic review. Musculoskelet Sci Pract. 2018;33:77–83. doi:10.1016/j.msksp.2017.11.007
9. Zhang Q, Yue EJ, Zeng X, et al. Acupuncture for chronic neck pain: a protocol for an updated systematic review. Syst Rev. 2016;5(1):76. doi:10.1186/s13643-016-0257-x
10. Peng J, Yang J, Feng J, et al. The effect of Fu’s subcutaneous needling combined with reperfusion approach on surface electromyography signals in patients with cervical spondylosis and neck pain: a clinical trial protocol. Biomed Res Int. 2022;2022(1):1761434. doi:10.1155/2022/1761434
11. Braakman R. Management of cervical spondylotic myelopathy and radiculopathy. J Neurol, Neurosurg, Psych. 1994;57(3):257. doi:10.1136/jnnp.57.3.257
12. Bono CM, Ghiselli G, Gilbert TJ, et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011;11(1):64–72. doi:10.1016/j.spinee.2010.10.023
13. Li W, Yao C, Zhou Y, et al. changes of endothelin-1 and calcitonin gene-related peptide concentrations in patients with cervical radiculopathy after wrist-ankle acupuncture-moxibustion and hot compression with Chinese herbal medicine. Genet Res. 2021;2021:5433742. doi:10.1155/2021/5433742
14. Pan S-L, Zheng S-L, Zhou X-H, et al. Acupuncture combined with Jingtong granule for nerve-root type cervical spondylosis and its effects on IL-6, TNF-α, IL-1β and hemorheological indexes. Zhongguo Zhen jiu=Chin Acupunct Moxibustio. 2019;39(12):1274–1278.
15. Yan K, Huang R, Li S, et al. Clinical effects and mechanism of the modified erxian decoction plus electroacupuncture in the treatment of cervical spondylotic radiculopathy. China J Trad Chin Med Pharm. 2023;38(08):3935–3939.
16. Hu Tianyuan YH. Clinical effect of wentong jibi decoction combined with electroacupuncture at ”qinglingpoints” on cervical spondylotic radiculopathy and serum inflammatory indexes. Chin Arch Trad Chin Med. 2020;38(08):35–39.
17. Tian HZ, Sun ZR, Zhang QH, et al. Observation of therapeutic effect on cervical Jiaji electro acupuncture treatment of nerve root type cervical spondylosis. J Emerg Trad Chin Med. 2015;24(06):1050–1052.
18. Su H, Chen H, Zhang X, et al. Electroacupuncture ameliorates pain in cervical spondylotic radiculopathy rat by inhibiting the CaMKII/CREB/BDNF signaling pathway and regulating spinal synaptic plasticity. Brain and Behavior. 2023;13(10). doi:10.1002/brb3.3177
19. Wu Y, Sun Y, Zhang J, et al. Correlation study on effects of electroacupuncture on the muscle condition and MNCV in rabbits with lumbar nerve root compression. Zhongguo Zhen jiu=Chin Acupunct Moxibustio. 2011;31(11):1009–1014.
20. Guo Y-J, Su S-Y, Su H, et al. Mechanism of analgesic effect of electroacupuncture on rats with cervical spondylosis radiculopathy based on activation of astrocytes and HMGB1/TLR4/MyD88 signaling pathway. Zhen ci yan jiu= Acupunct Res. 2024;49(9):909–916. doi:10.13702/j.1000-0607.20230789
21. Jiang Y-N, Li J, Chen Y-H, et al. Relationship between the inserting sites of Fu’s subcutaneous needling and traditional acupoints: revelation to acupuncture and moxibustion. Zhongguo Zhen jiu=Chin Acupunct Moxibustio. 2023;43(1):95–100.
22. Li G-F, Fu Z-H. The enlightenment of Fu’s subcutaneous needling on pain medicine. Zhongguo Zhen jiu=Chin Acupunct Moxibustio. 2014;34(6):591–593.
23. Chiu PE, Fu Z, Sun J, et al. Efficacy of Fu’s subcutaneous needling in treating soft tissue pain of knee osteoarthritis: a randomized clinical trial. J Clin Med. 2022;11(23):7184. doi:10.3390/jcm11237184
24. Fu Z-H, Wang J-H, Sun J-H, et al. Fu’s subcutaneous needling: possible clinical evidence of the subcutaneous connective tissue in acupuncture. J Altern Comp Med. 2007;13(1):47–52. doi:10.1089/acm.2006.6125
25. Lin Q, Luo N-S, Yang C-Y, et al. Revelation of Fu’s subcutaneous needling therapy on the development of acupuncture and moxibustion. Zhongguo Zhen jiu=Chin Acupunct Moxibustio. 2020;40(3):307–314.
26. STATE ADMINISTRATION OF TRADITIONAL CHINESE MEDICINE PC. Standard for Diagnosis and Efficacy Evaluation of Traditional Chinese Medicine Diseases and Syndromes. Nanjing University Press Nanjing; 1994.
27. Itoh K, Katsumi Y, Hirota S, et al. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement Ther Med. 2007;15(3):172–179. doi:10.1016/j.ctim.2006.05.003
28. Chiu TT, Hui-Chan CW, Cheing G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabilitat. 2005;19(8):850–860. doi:10.1191/0269215505cr920oa
29. Leak A, Cooper J, Dyer S, et al. The northwick park neck pain questionnaire, devised to measure neck pain and disability. Rheumatology. 1994;33(5):469–474. doi:10.1093/rheumatology/33.5.469
30. Chung S, Jeong YG. Effects of the craniocervical flexion and isometric neck exercise compared in patients with chronic neck pain: a randomized controlled trial. Physiother Theory Pract. 2018;34(12):916–925. doi:10.1080/09593985.2018.1430876
31. Fu S, Zhang R, Zhong M, et al. Clinical effect of Qihuang needle therapy combined with meridian sinew theory on cervical spondylotic radiculopathy. Acta Chin Med. 2021;36(08):1795–1798.
32. Brazier JE, Harper R, Jones N, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Br Med J. 1992;305(6846):160–164. doi:10.1136/bmj.305.6846.160
33. Kang M, Zhang B, Chen L. Clinical study of Fu’s subcutaneous needling treating CSR. J Clin Acupunct Moxibustio. 2018;034(006):52–54.
34. Dvorak J, Panjabi M, Grob D, et al. Clinical validation of functional flexion/extension radiographs of the cervical spine. Spine. 1993;18(1):120–127. doi:10.1097/00007632-199301000-00018
35. Langevin HM. Acupuncture, connective tissue, and peripheral sensory modulation. Crit Rev Eukaryotic Gene Exp. 2014;24(3):249–253. doi:10.1615/critreveukaryotgeneexpr.2014008284
36. Wilke J, Krause F, Vogt L, et al. What is evidence-based about myofascial chains: a systematic review. Arch Phys Med Rehabil. 2016;97(3):454–461. doi:10.1016/j.apmr.2015.07.023
37. Berrueta L, Muskaj I, Olenich S, et al. Stretching Impacts Inflammation Resolution in Connective Tissue. J Cell Physiol. 2016;231(7):1621–1627. doi:10.1002/jcp.25263
38. Langevin HM, Bouffard NA, Churchill DL, et al. Connective tissue fibroblast response to acupuncture: dose-dependent effect of bidirectional needle rotation. J Altern Comp Med. 2007;13(3):355–360. doi:10.1089/acm.2007.6351
39. Jialei T, Zhonghua F, Hongru Z. The analysis with mechanism of Fu’s subcutaneous needling. Lishizhen Med Materia Medica Res. 2014;25:3006–3008.
40. Xu W, Wu J, Xu P. An Immunological Hypothesis of Fu’s subcutaneous needling acupuncture. J Acupunct Meridian Stud. 2021;14(3):110–115. doi:10.51507/j.jams.2021.14.3.110
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

