Back to Journals » Nature and Science of Sleep » Volume 16
Higher Levels of Morning and Daytime Light Exposure Associated with Positive Sleep Indices in Professional Team Sport Athletes
Authors Stevenson S, Suppiah H, Ruddy J, Murphy S, Driller M
Received 20 May 2024
Accepted for publication 18 August 2024
Published 28 August 2024 Volume 2024:16 Pages 1279—1290
DOI https://doi.org/10.2147/NSS.S471017
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Shauna Stevenson,1 Haresh Suppiah,1 Joshua Ruddy,2 Sean Murphy,2 Matthew Driller1
1Sport, Performance, and Nutrition Research Group, School of Allied Health, Human Services, and Sport, La Trobe University, Melbourne, Australia; 2Essendon Football Club, Melbourne, Australia
Correspondence: Shauna Stevenson, School of Allied Health, La Trobe University, Plenty Road, Bundoora, Melbourne, VIC, 3086, Australia, Tel +61 450 782 680, Email [email protected]
Objective: Light exposure techniques have been recommended to combat sleep issues caused by disruption to circadian regularity in the athletic population, although studies are lacking.
Methods: A total of 17 professional male Australian Football athletes (age ± SD: 22 ± 3 years) wore a wrist actigraph to measure sleep parameters, and a wearable light sensor to measure melanopic equivalent daylight illuminance (mEDI, in lux) for 14 days. Participants completed three sleep questionnaires at the end of the data collection period and completed well-being surveys 6 times. The Sleep Regularity Index (SRI) for each player was also calculated from actigraphy data. Light exposure data were organised into three different timeframes: morning (wake time + 2 hours), daytime (end of morning to 6 pm), and evening (2 hours leading up to bedtime) for analysis. Repeated measures correlation was conducted for objective sleep measures and mEDI values per timeframe. Pearson’s correlation was conducted on subjective sleep measures and well-being measures against mEDI values per timeframe.
Results: Higher morning light was associated with significantly (p < 0.001) greater total sleep time (r = 0.31). Higher daytime light exposure was associated with higher subjective sleep quality (r = 0.48, p < 0.05). Higher evening light exposure was associated with higher Athlete Sleep Screening Questionnaire (ASSQ) global scores (r = 0.52, p < 0.05). There were no other significant correlations between light exposure and sleep or well-being measures (p > 0.05).
Conclusion: Higher morning and daylight exposure levels were associated with various positive objective and subjective sleep measures in professional team sport athletes, supporting the need for education on optimising light exposure to improve circadian function, sleep, and health.
Keywords: mEDI, actigraphy, wearable light sensors, lux, circadian rhythms
Introduction
It has been reported that elite athletes may struggle to meet the recommended guidelines for sleep,1 negatively impacting their capacity to train and perform in their chosen sport2 as sleep is crucial for the physiological, cognitive, and psychological aspects of athletic performance.2 One of the most important cues for circadian rhythms and sleep is the exposure to natural light intensities during the morning and daytime, and dim light in the evening.3 Attempts have been made to use artificial light exposure in athletes as a means to improve sleep, with limited success.4 However, there is a paucity of studies describing the light exposure habits of athletes, and their impact on sleep and well-being metrics.
Team sport athletes may have an increased likelihood of poor sleep5,6 due to various factors including environmental factors such as light or noise,7 and late-night matches.8 Furthermore, increases in core temperature,2 muscle tension, and pain following training or competition can cause athletes to experience poor sleep9 and can ultimately have detrimental consequences on an athlete’s performance, well-being, and psychophysiological recovery measures.2 Furthermore, increases in acute training load may be associated with increased wake after sleep onset, and decreased sleep duration, efficiency and quality in Australian Football League (AFL) players.10
Alarmingly, 59.1% of team-sport athletes lack a strategy to address sleep disturbances.6 Implementing sleep hygiene protocols (eg, maintaining consistent bed and wake times, avoiding late naps, sleeping in a cool and dark environment, avoiding blue-light emitting technology before bedtime) has returned positive results for short-term sleep efficiency and sleep latency in elite cricket players11 and also increases in total sleep time in elite netball players.12 However, while often included in sleep hygiene education, details on the light exposure habits in athletes are still largely unknown.
It has been proposed that sleep and wakefulness are regulated by a two-process model of homeostatic drive (Process S) and circadian drive (Process C).13 The suprachiasmatic nuclei synchronises these processes using light signals of varying intensities as the main environmental cue.14 Timing of light exposure is important as daylight aids wakefulness and alertness in the early day, whereas the absence of light in the evening promotes sleepiness.15 Team sport athletes may experience challenges in obtaining sufficient natural light due to indoor training (eg, morning gym sessions, team meetings) and increased exposure to artificial light from electronic devices16 and competition in brightly lit venues.2
In a within-subject cross-over study on recreational athletes exploring light regulation, participants underwent combined sleep schedules with either light regulation or no light regulation.4 Athletes with a strict sleep-wake cycle reported improved sleep onset latency (∆SOL = 17 min) and higher subjective sleep quality. However, athletes with a more flexible sleep-wake cycle also improved sleep-reported sleep onset latency with light regulation (∆SOL = 8 min).4 Another study found that students without sun exposure or exercise for a week had significantly later bed and wake times than those receiving 30 minutes of light exposure or both aerobic exercise and sun exposure.17 Higher daytime light exposure was associated with less frequent tiredness (OR = 0.80–0.82),17 suggesting that low daytime light exposure can be classed as a critical environmental risk factor when considering sleep, mood, and circadian-related outcomes.18
The development of new technologies to continuously measure light exposure during daily activities in humans has seen recent advancements. For example, wearable light-sensing devices placed on or around the collar that track the intensity, spectrum, and pattern of light exposure in free-living conditions19 and workplace settings20 have been reported in the last few years. Past studies relied on lux as the main measurement for exploring light exposure habits in humans; however, photopic lux has been reported to be limited in its ability to quantify the circadian effects of light in humans.21 Therefore, more recently, melanopic equivalent daytime illuminance (mEDI) has been proposed.22 The standardised metric mEDI quantifies light for its ability to activate the melanopsin-based photoreception of intrinsically photosensitive retinal ganglion cells (ipRGCs)21 and has been reported to be a robust predictor of nonvisual responses such as melatonin suppression and circadian phase resetting under a wide range of conditions.22
Despite recommendations for light regulation to enhance subjective sleep,4 to our knowledge, no studies have measured light exposure and sleep outcomes in an elite athlete setting. Further, there is a lack of research on the relationship between sleep/wake routines, assessed using the sleep regularity index (SRI),23 and light exposure habits in athletes. Therefore, this study aimed to investigate the relationship between light exposure during the morning, throughout the day, and in the evening, on sleep and well-being metrics over 15 days in a cohort of professional Australian Football League players.
Methods
Participants
An information session regarding the study was presented to a single football club in the top league of the Australian Football League (~30 athletes), and the option to volunteer in the study was given. Following the presentation, 20 athletes volunteered to participate in the study, with the other 10 either being injured at the time or not participating in full training. A sample of 17 male professional Australian Football athletes (mean ± SD; age: 22 ± 3 years; height: 188 ± 8 cm; body mass: 87 ± 6 kg) completed the study, with three athletes not completing due to two injuries following the start of the study and one light button breaking during the study, reducing our sample to 17. All athletes were of elite standard and amongst the best players in the world in their given sport according to the classification as outlined by McKay and colleagues24. The study took place during the summer (January) in Melbourne, Australia, during the early pre-season phase of the AFL schedule. All participants were undertaking ~5 days of training consisting of between 8 and 12 sessions throughout each week during the study (including on-field training and strength and conditioning sessions). Total training hours were ~18 hours per week. Athletes provided informed consent to take part in the study, and ethical approval was obtained through the La Trobe University’s Human Research Ethics Committee (#HEC22369) and is in accordance with the Declaration of Helsinki.
Study Design
The current study implemented an observational study design. Participants wore a wrist actigraphy device and a wearable light sensor attached to the collar of their clothing for 14 complete days (15 nights). Participants were instructed to wear their actigraphs and wearable light sensors throughout the entire study and were instructed to only take wearable light sensors off during training (placed on a table within the same lighting environment – either outside in full natural light or inside on a table in the gym), when showering, and when sleeping (set on their bedside table, with sensors unobstructed during the night). Participants were instructed to avoid covering their light button at any stage and maintain their normal sleeping and light exposure habits throughout the study period.
Sleep Monitoring
Athletes were instructed to wear an actigraphy device (Fitbit Charge 5, Fitbit Inc, San Francisco, CA, USA) on their wrist to measure their sleep and day-to-day activity. The device was worn on either the dominant or non-dominant wrist, whatever was the most comfortable for the individual.25 The device was a wearable fitness tracker embedded with a triaxial accelerometer and uses Bluetooth to automatically connect and transfer data to a smartphone via a software application. Previous studies have found that wrist actigraphy devices from the same manufacturer have shown no significant difference (p > 0.05) in sleep onset latency and total sleep time in healthy adults when compared to the gold standard polysomnography.26 Indeed, devices from this manufacturer have also been reported to outperform many other consumable wearables, and research-grade actigraphy devices, deeming them appropriate for determining sleep duration in human participants.27 Sleep indices including total sleep time (TST), total time in bed (TTB), sleep efficiency (SE), sleep latency (SL), sleep time (ST), and wake time (WT) were used to assess athlete sleep patterns and behaviours in the current study. These sleep metrics were used, as they have been deemed as the most accurate measures from actigraphy, when compared to polysomnography.26
Wearable Light Sensing Devices
Daily light exposure was measured with a lightweight, wearable light sensor (LYS Button by LYS Technologies LTDTM, Copenhagen, Denmark). The wearable light sensor is a small clip-on monitor that collects ambient light in the visible and near-infrared spectra (Figure 1). The device tracks the number of spectral properties of light a user is exposed to every 15 seconds and transmits data via Bluetooth to a smartphone containing the manufacturer’s software (LYS Collect, LYS technologies LTDTM, Copenhagen, Denmark). The wearable light sensors measure melanopic equivalent daylight illuminance (mEDI – measured in lux). According to the manufacturers, the sensor has a mean standard error of 5–10% depending on intensity, with an engineered bias to indoor lighting scenes (ie, illuminances between 0 and 500 lx). Light meters were worn on each participant’s clothing (on the collar) during waking hours and placed on the bedside table at night when athletes were asleep. Unpublished observations from our laboratory indicate that the wearable light sensors used in the current study are both valid and reliable when compared to a gold standard light meter. The coefficient of variation (CV%) when compared to a gold standard light meter (LX1330B, Dr.Meter, California, USA) was deemed acceptable (CV ~ 1.8%, typical error of estimate = 9.5 lux). Inter-device reliability was also deemed acceptable (CV ~ 2.5%, ICC ~0.92).
 |
Figure 1 The wearable light sensing devices (LYS technologies LTD) used in the current study. |
Data Collection Procedures
Data collection occurred between January 9th and January 24th (summer), in Melbourne, Australia (coordinates = 37.8136° S, 144.9631° E), Australian Eastern Daylight Time. During the study period, average daily temperature 21 ± 3 °C and average rainfall was 0.66 ± 1.83 mm. Natural daylight duration started at 0617 h ± 0:04 h:mins (sunrise) to 0841 h ± 0:01 h:mins (sunset) during the data collection period. Data were collected from both sleep monitoring and light sensing devices daily when synced to a mobile device and transferred to a computer for further analysis. mEDI (in lux) was measured and used to assess athlete’s light exposure every 15 seconds throughout the entire data collection period.
Preparation and Treatment of Light Data
The following treatment of light data was performed in Python. The presence of values indicating that there was no light and no movement detected during waking hours were removed, as it was likely that their wearable device was not on their person. Secondly, outlier detection was carried out using a median imputation approach, whereby the interquartile range was calculated for each athlete at 5-minute intervals. Any mEDI values above the upper bound of the IQR were considered an outlier. Each upper bound was specific to the athlete and each 5-minute interval. This was then iterated over the raw data for the whole 2-week data collection period. After outlier detection, the median value for each athlete in 5-minute periods was imputed. Light data were then aggregated into three different timeframes: morning: whereby light data were individually extracted for two hours post-wake time, daytime light exposure (two hours post-individual wake time to 6 pm) and evening light exposure (two hours before individual bedtime) on each separate day of data collection.
Well-Being Data
Athletes completed a wellness survey every morning of main training or craft skills training (3 times per week). The survey data were completed on their mobile devices between waking and 0900 h. Survey data included an athlete self-rating on a scale of 1–10 on their motivation, and sleep quality, with; 1 = very poor, and 10 = excellent.
Athlete Sleep Behaviour Questionnaire (ASBQ)
The Athlete Sleep Behaviour Questionnaire (ASBQ) is an 18-item self-rated questionnaire regarding sleep habits and sleep behaviour among elite athletes. The ASBQ has been used as a practical tool to help identify maladaptive sleep behaviours.28 The questionnaire asks participants how frequently they engaged in specific behaviours over the past month (never, rarely, sometimes, frequently, or always) and the weighting for each response (1 = never, 2 = rarely, 3 = sometimes, 4 = frequently, and 5 = always) was summed to provide an ASBQ global score. A high ASBQ score (≥42) is indicative of poor sleep behaviours, 37–41 corresponds to “moderate” sleep behaviour, and a low score (≤36) indicates no problems with athletes’ sleep behaviours.28 This is the only questionnaire that identifies sleep behaviours specific to athletes28 and has been reported to have acceptable reliability (Intraclass correlation = 0.87) when re-tested and has moderate to large correlations with validated questionnaires such as Sleep Hygiene Index (SHI), the Epworth Sleepiness Scale (ESS) and the Pittsburgh Sleep Quality Index (PSQI).28
Athlete Sleep Screening Questionnaire (ASSQ)
The Athlete Sleep Screening Questionnaire (ASSQ) is a self-rated 15-item questionnaire used to distinguish clinically significant sleep disturbances and daytime dysfunction in athletes and provide interventions based on the type and severity of the problem reported.29 This tool assesses both sleep and circadian factors of sleep quantity, sleep quality, insomnia, and chronotype with a timeframe of “over the recent past”.29 Research has shown that this tool accurately determines which participating athletes may find benefit in undertaking preventative measures and identify those who may experience clinically significant sleep problems that may require further assessment.30 Sleep Difficulty Score (SDS) is calculated from the scores of questions 1, 3, 4, 5, and 6 and is used to classify if athletes’ level of clinical sleep problems (0–4 = none; 5–7 =mild; 8–10 = moderate; or 11–17 severe), and a higher score indicates poorer sleep quality.
Brief Pittsburgh Sleep Quality Index (B-PSQI)
The Brief Pittsburgh Sleep Quality Index (B-PSQI) is a shorter version of the original Pittsburgh Sleep Quality Index (PSQI),31 therefore improving the efficiency and applicability of its use.32 The B-PSQI contains six items with questions on bedtime, wake time, sleep latency, sleep duration, wake after sleep onset, and sleep quality over the past month. The B-PSQI scores range from 0 to 15 whereby higher scores (>5) are indicative of poorer sleep quality.32 Previous research has reported that the B-PSQI is a valid and reliable screening tool for measuring sleep quality.32 All questionnaires were administered at the end of the data collection period via a URL link on their mobile devices. Questionnaire data were collected and managed using REDCap (Research Electronic Data Capture, Vanderbilt, USA) electronic data capture tools hosted at La Trobe University.
Sleep Regularity Index (SRI)
The Sleep Regularity Index (SRI) evaluates variations in sleep and wake cycles on a night-to-night basis by taking into account changes in sleep onset and wake times.23 It estimates the probability that an individual’s sleep-wake pattern aligns from one day to the next, and this assessment is aggregated over the study duration to generate a comprehensive SRI score. A score of 100 on the SRI signifies an identical sleep-wake cycle between consecutive days, whereas a score of 0 indicates no overlap in sleep-wake cycles from one day to the next.
Statistical Analysis
All statistical analyses were conducted using the Jamovi statistical package (Jamovi Version 0.8, Jamovi Project 2018). Athletes’ SRI values were determined through binary sleep-wake data, with sleep onset and wake times derived from wrist actigraphy and converted into UNIX time, coding each time as “1” for sleep or “0” for wake. The R (RStudio) statistical software (version 2023.12.1; R Foundation for Statistical Computing, Vienna, Austria) and the sleepreg package33 were employed for SRI calculations. Before analysis, data were checked for outliers by visual inspection of a box plot and quantile–quantile plot. mEDI data were aggregated for each timeframe to allow for correlation analysis. A total of 407 datapoints were aggregated on the objective sleep measures and light data (163 for morning, 139 for daytime and 105 for evening). This included average mEDI per timeframe per day individual to each participant. Repeated measures correlation was conducted to investigate light exposure from the three different timeframes (morning, day, and evening) on each athlete’s objective sleep parameters measured every day over 14 days following the procedures outlined by Bakdash & Marusich.34 A Pearson’s correlation was conducted on average mEDI from each timeframe against athletes’ SRI scores, scores from questionnaires (collected at the end of data collection), and well-being measures (motivation, coping, and self-perceived sleep quality) collected 3 times a week over the 2-week data collection period. The scores from the well-being measures were then aggregated to get one value over the whole data collection period, so therefore these measures did not fit the repeated measures model. The strength of the correlation between light exposure and other measures was assessed using the following thresholds: <0.1, trivial; 0.1–0.3, small; 0.3–0.5, moderate; 0.5–0.7, large; 0.7–0.9, very large; and 0.9–1.0, almost perfect.35 Statistical significance was set at p < 0.05.
Results
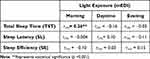
Descriptive statistics for sleep characteristics and light exposure levels and results of the questionnaires are shown in Table 1. The mean, standard deviations and interquartile range of light exposure in the three specified timeframes throughout the data collection period are shown in Table 2.
 |
Table 2 Melanopic Equivalent Daylight Illuminance (mEDI) Scores Across Three Different Time Periods: Morning (Wake Time + 2 Hours), Daytime (End of Morning to 6 pm) and Evening (2 Hours Pre-Bedtime) |
The sleep questionnaire outcomes (Table 1) show an average ASBQ score of 39 which aligns with typical sleep behaviour profiles among the athletes in this study.28 Further, a mean global score of 4 in the B-PSQI signifies an absence of sleep-related issues as the mean score falls below 5.32 Lastly, a mean SDS score of 5 in the ASSQ denotes the presence of “mild” sleep problems within the current study cohort.30
The correlation results between light exposure at different times of day and sleep and well-being metrics are reported in Table 3 and Table 4 and illustrated on Figures 2 and 3. Repeated measures correlation found a significant, small correlation between morning light exposure and total sleep time (r = 0.26, p = 0.001) (Table 3 and Figure 2). Pearson’s correlation results found a significant, small correlation between daytime light exposure and sleep quality (r = 0.48, p = 0.05) (Table 4 and Figure 3) and lastly, a significant, strong correlation between evening light exposure and ASSQ scores was found (r = 0.52, p = 0.04) (Table 4 and Figure 3).
Discussion
This study sought to investigate the relationship between light exposure throughout different times of the day on elite athlete’s sleep and well-being metrics over two weeks. It was found that higher levels of morning light exposure were positively correlated with longer total sleep time and daytime light exposure was positively correlated with higher subjective sleep quality. Further, higher evening light exposure levels in the two hours prior to bedtime were correlated with higher ASSQ scores, indicating poorer sleep behaviours. However, no significant relationships were found between light exposure levels and any other measures including sleep latency, sleep efficiency, SRI, ASBQ, B-PSQI, coping and motivational levels during the data collection period.
Previous studies have shown that one week of bright-light administration in the morning has advantageous effects on sleep measures.36 When comparing one-week of bright light exposure (~2500 lux for 60 minutes) and dim-light exposure (~100 lux) during the morning (1–1.5 h before their baseline weekday waking time) in insomnia patients, those under bright light showed a significant 51-minute increase in total sleep time during 3 weeks post-intervention.36 Although the current study measured habitual light exposure in athletes (without any lighting intervention), repeated measures results also showed a significant positive correlation between morning light exposure and total sleep time. A previous study where participants from the general population measured daily light exposure using a wrist-worn light logger (SpectraWear, Manchester, UK) which utilises mEDI (in lux) as the measurement of light found that brighter light exposure after waking was linked to reduced sleep inertia.37 The importance of obtaining high levels of light in the morning has been previously emphasised by Yin et al38 to help maintain internal clock and, in turn, improve sleep quality. Additionally, increased light exposure has been stated to be of benefit due to morning light having a phase-advancing effect on the human circadian system14 and it has been established that carefully timed exposure to bright light in the morning (and also restriction of short-wavelength light in the evening) shortens subjective sleep latency in recreational athletes.4 However, our study did not show any significant correlations between objective sleep latency and light exposure, possibly due to sleep latency being considerably low for the whole cohort (~7 minutes).
Pearson’s correlation results of this study show that athlete’s light exposure during the daytime was higher than that obtained in the morning hours and was positively correlated with subjective sleep quality. This finding is in agreement with previous studies that found that greater daytime light exposure predicts better sleep quality in healthy participants.39 The cohort in this study spent a considerable amount of time training outdoors (~2.5 hours on average each day), which may be higher than the general population37 and those of a similar age, who have been reported to only spending 9% of their waking day in light levels above 1000 lux.40 Increased exposure to melanopic light throughout the day has advantageous effects on alertness, performance and sleep,41 and interestingly, there is limited evidence of high daytime light exposure having any negative effects on circadian physiology.41 However, lack of exposure to natural light is associated with poor quality of sleep.42 Further, previous studies have found that increasing daytime light exposure results in more consistent sleep timing and circadian phase43 and insufficient daytime light exposure can delay the circadian system and suppress melatonin levels and subjective sleepiness in the evening and at night.4
Evening light exposure levels in the current study are above the recommendations suggested by Brown et al,41 whereby the recommended maximum mEDI is 10 lux measured at the eye at least three hours before bedtime. In our study, on average, athletes obtained ~75 lux in the evening which is over the suggested recommendations by Brown and colleagues41. However, this is consistent with previous literature whereby participants from the general population also reported many instances of readings >10 lux in the lead up to bedtime,37 which was also associated with increased sleep onset latency. Pearson’s correlation results found that higher light exposure in the evening was associated with higher ASSQ scores, thus, indicating increased instances of sleep disturbance and daytime dysfunction. However, while there were no other significant relationships between nighttime light exposure and objective or subjective sleep metrics, it is important to note that there is evidence that the effects of brighter evening light can be mitigated by brighter light exposure obtained earlier in the day.41
Even though questionnaire results showed no significant relationships with morning or daytime light exposure, athletes exhibited an average global score of ~5 in the ASSQ, which indicates a “mild” SDS score.30 The ASSQ global score was significantly correlated with higher levels of evening light exposure. Compared to previous studies, the ASSQ scores exhibited in this study are relatively similar to other team-sport athletes such as soccer players pre-competition (SDS score = 4.8).44 Further to this, while there was no significant relationship between SRI results and light exposure, the average SRI score in our cohort was ~79, which indicates that athletes sleep patterns are relatively regular,23 though slightly lower than the SRI scores of ~85 previously reported in team-sport athletes.45 Irregular sleep patterns are associated with delayed circadian rhythms23 and those with regular sleep patterns have reported to have greater sleep efficiency and less variability in total sleep time.45
There are several limitations associated with the current study. Firstly, the sample size was relatively small due to difficulty in recruiting elite athletes, which in turn may have affected the study findings. The participants in this study were from a homogenous, elite Australian Rules football team, playing at the top level of competition for their sport. In order to increase the sample size, multiple teams would have been required, which would introduce further limitations such as different training schedules and locations. We considered expanding the study in a lower level of semi- or non-professional athletes but decided this would not be as representative of the sleep and light exposure patterns of elite athletes. Additionally, participants in this study were instructed to wear the light sensor on their clothes and were subject to error if sensors were left on removed clothes or covered by additional clothing. Further to this, participants were instructed to wear the light sensor on the collar of their clothes, as close to the eyes as possible. However, light exposure levels recorded in this study may not reflect the actual light exposure at the level of the cornea. It is also important to note that inter-individual differences may be present in how an individual may perceive light and how susceptible to the effects they are to the light they are exposed to.46 Lastly, given the difficulties in getting athletes to adhere to wearing the light sensors 24/7 over longer periods of time, and the required large amounts of data analysis, subjective questionnaires and surveys detailing light exposure habits might be a worthwhile consideration. Questionnaires such as the Light Exposure Behaviour Assessment (LEBA)47 may provide a viable alternative to objective light monitoring. However, the LEBA is yet to be validated against objective measures such as wearable light sensors.
In this study, we found that higher morning and daytime light was associated with positive objective and subjective sleep parameters, and higher evening light in the lead-up to bedtime may be detrimental to sleep quality in athletes. Thus, it is suggested that athletes obtain sufficient morning and daytime light levels and decrease their light exposure levels in the lead-up to bedtime in order to maximise athlete’s sleep, and potentially their subsequent recovery and performance. The results of the current study support the need for education on optimising light exposure throughout the day to improve circadian function, sleep and health and also the implementation of interventions to optimise light exposure throughout the day and minimise light exposure at night. Furthermore, the athletes in the current study likely exhibited high levels of light exposure throughout the waking day due to predominantly training outdoors (~2.5 hours per day). Therefore, further investigation of the light exposure habits of indoor-based athletes and the magnitude of the subsequent effects it may have on sleep parameters should be considered in future research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gupta L, Morgan K, Gilchrist S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 2017;47(7):1317–1333. doi:10.1007/s40279-016-0650-6
2. Walsh NP, Halson SL, Sargent C, et al. Sleep and the athlete: narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2021;55(7):356–368. doi:10.1136/bjsports-2020-102025
3. Duffy JF, Czeisler CA. Effect of light on human circadian physiology. Sleep Med Clin. 2009;4(2):165–177. doi:10.1016/j.jsmc.2009.01.004
4. Knufinke M, Nieuwenhuys A, Geurts SAE, et al. Dim light, sleep tight, and wake up bright–Sleep optimization in athletes by means of light regulation. Europ J Sp Sci. 2021;21(1):7–15. doi:10.1080/17461391.2020.1722255
5. Driller MW, Suppiah H, Rogerson D, Ruddock A, James L, Virgile A. Investigating the sleep habits in individual and team-sport athletes using the Athlete Sleep Behavior Questionnaire and the Pittsburgh Sleep Quality Index. Sleep Sci. 2022;15(1):112–117. doi:10.5935/1984-0063.20210031
6. Juliff LE, Halson SL, Peiffer JJ. Understanding sleep disturbance in athletes prior to important competitions. J Sci Med Sport. 2015;18(1):13–18. doi:10.1016/j.jsams.2014.02.007
7. Samuels C. Sleep, Recovery, and Performance: the New Frontier in High-Performance Athletics. Neurol Clinics. 2008;26(1):169–180. doi:10.1016/j.ncl.2007.11.012
8. McGuckin TA, Sinclair WH, Sealey RM, Bowman P. The effects of air travel on performance measures of elite Australian rugby league players. Europ J Sp Sci. 2014;14(SUPPL.1). doi:10.1080/17461391.2011.654270
9. Halson SL. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. 2014;44(SUPPL.1):13–23. doi:10.1007/s40279-014-0147-0
10. Pitchford NW, Robertson SJ, Sargent C, Cordy J, Bishop DJ, Bartlett JD. Sleep quality but not quantity altered with a change in training environment in elite Australian rules football players. Internat J Sports Physiol Perform. 2017;12(1):75–80. doi:10.1123/ijspp.2016-0009
11. Driller MW, Lastella M, Sharp AP. Individualized sleep education improves subjective and objective sleep indices in elite cricket athletes: a pilot study. J Sport Sci. 2019;37(17):2121–2125. doi:10.1080/02640414.2019.1616900
12. O’Donnell S, Driller MW. Sleep-hygiene education improves sleep indices in elite female athletes. Int J Exercise Sci. 2017;10(4):522–530.
13. Borbely AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1(3):195–204.
14. Dumont M, Beaulieu C. Light exposure in the natural environment: relevance to mood and sleep disorders. Sleep Med. 2007;8(6):557–565. doi:10.1016/j.sleep.2006.11.008
15. Knufinke M, Fittkau-Koch L, Møst EIS, Kompier MAJ, Nieuwenhuys A. Restricting short-wavelength light in the evening to improve sleep in recreational athletes–A pilot study. Europ J Sp Sci. 2019;19(6):728–735. doi:10.1080/17461391.2018.1544278
16. Silvani MI, Werder R, Perret C. The influence of blue light on sleep, performance and wellbeing in young adults: a systematic review. Front Physiol. 2022;13. doi:10.3389/fphys.2022.943108
17. Lee H, Kim S, Kim D. Effects of exercise with or without light exposure on sleep quality and hormone reponses. J Exerc Nutrit Biochem. 2014;18(3):293–299. doi:10.5717/jenb.2014.18.3.293
18. Burns AC, Saxena R, Vetter C, Phillips AJK, Lane JM, Cain SW. Time spent in outdoor light is associated with mood, sleep, and circadian rhythm-related outcomes: a cross-sectional and longitudinal study in over 400,000 UK Biobank participants. J Affective Disorders. 2021;295:347–352. doi:10.1016/j.jad.2021.08.056
19. van Lieshout-Van Dal E, Snaphaan L, Bouwmeester S, de Kort Y, Bongers I. Testing a single-case experimental design to study dynamic light exposure in people with dementia living at home. Appl Sci. 2021;11(21). doi:10.3390/app112110221
20. Aries MBC, Fischl G, Lowden A, Beute F. The relationship of light exposure to sleep outcomes among office workers. Part 1: working in the office versus at home before and during the COVID-pandemic. Light Res Technol. 2022. doi:10.1177/14771535221136096
21. Lucas RJ, Peirson SN, Berson DM, et al. Measuring and using light in the melanopsin age. Trends Neurosci. 2014;37(1):1–9. doi:10.1016/j.tins.2013.10.004
22. Brown TM. Melanopic illuminance defines the magnitude of human circadian light responses under a wide range of conditions. J Pineal Res. 2020;69(1):1–14. doi:10.1111/jpi.12655
23. Phillips AJK, Clerx WM, O’Brien CS, et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep. 2017;7(1):1–13. doi:10.1038/s41598-017-03171-4
24. McKay AKA, Stellingwerff T, Smith ES, et al. Defining training and performance caliber: a participant classification framework. Internat J Sports Physiol Perform. 2022;17(2):317–331. doi:10.1123/ijspp.2021-0451
25. Driller MW, O’Donnell S, Tavares F. What wrist should you wear your actigraphy device on? Analysis of dominant vs. non-dominant wrist actigraphy for measuring sleep in healthy adults. Sleep Sci. 2017;10(3):132–135. doi:10.5935/1984-0063.20170023
26. Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Accuracy of wristband fitbit models in assessing sleep: systematic review and meta-analysis. J Med Inter Res. 2019;21(11):e16273. doi:10.2196/16273
27. Chinoy ED, Cuellar JA, Huwa KE, et al. Performance of seven consumer sleep-tracking devices compared with polysomnography. Sleep. 2021;44(5). doi:10.1093/sleep/zsaa291
28. Driller MW, Mah CD, Halson SL. Development of the athlete sleep behavior questionnaire: a tool for identifying maladaptive sleep practices in elite athletes. Sleep Sci. 2018;11(1):37–44. doi:10.5935/1984-0063.20180009
29. Samuels C, James L, Lawson D, Meeuwisse W. The athlete sleep screening questionnaire: a new tool for assessing and managing sleep in elite athletes. Br J Sports Med. 2016;50(7):418–422. doi:10.1136/bjsports-2014-094332
30. Bender AM, Lawson D, Werthner P, Samuels CH. The clinical validation of the athlete sleep screening questionnaire: an instrument to identify athletes that need further sleep assessment. Sp Med Open. 2018;4(1). doi:10.1186/s40798-018-0140-5
31. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research; 1989
32. Sancho-Domingo C, Carballo JL, Coloma-Carmona A, Buysse DJ. Brief version of the Pittsburgh Sleep Quality Index (B-PSQI) and measurement invariance across gender and age in a population-based sample. Psychol Assess. 2021;33(2):111–121. doi:10.1037/pas0000959
33. Windred DP, Jones SE, Russell A, et al. Objective assessment of sleep regularity in 60 000 UK Biobank participants using an open- source package; 2021:1–4.
34. Bakdash JZ, Marusich LR, Xu Y, Long Q, Yang J, Yuan J. Repeated measures correlation. Front Psychol. 2017;8:1–13. doi:10.3389/fpsyg.2017.00456
35. Atkinson G, Nevill A. Measures of reliability in sports medicine and science. Sports Med. 2000;30(5):375–381. doi:10.2165/00007256-200030050-00005
36. Lack L, Wright H, Paynter D. The treatment of sleep onset insomnia with bright morning light. Sleep Biol Rhythms. 2007;5(3):173–179. doi:10.1111/j.1479-8425.2007.00272.x
37. Didikoglu A, Mohammadian N, Johnson S, et al. Associations between light exposure and sleep timing and sleepiness while awake in a sample of UK adults in everyday life. Proc Natl Acad Sci. 2023;120(42):1–9. doi:10.1073/pnas
38. Yin J, Julius AA, Wen JT. Optimization of light exposure and sleep schedule for circadian rhythm entrainment. PLoS One. 2021;16:e0251478. doi:10.1371/journal.pone.0251478
39. Wams EJ, Woelders T, Marring I, et al. Linking light exposure and subsequent sleep: a field polysomnography study in humans. Sleep. 2017;40(12). doi:10.1093/sleep/zsx165
40. Scheuermaier K, Laffan AM, Duffy JF. Light exposure patterns in healthy older and young adults. J Biol Rhyth. 2010;25(2):113–122. doi:10.1177/0748730410361916
41. Brown TM, Brainard GC, Cajochen C, et al. Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults. PLoS biol. 2022;20(3):e3001571. doi:10.1371/journal.pbio.3001571
42. Harb F, Hidalgo MP, Martau B. Lack of exposure to natural light in the workspace is associated with physiological, sleep and depressive symptoms. Chronobiol Int. 2015;32(3):368–375. doi:10.3109/07420528.2014.982757
43. Papatsimpa C, Schlangen LJM, Smolders KCHJ, Linnartz JPMG, de Kort YAW. The interindividual variability of sleep timing and circadian phase in humans is influenced by daytime and evening light conditions. Sci Rep. 2021;11(1):1–14. doi:10.1038/s41598-021-92863-z
44. Biggins M, Purtill H, Fowler P, et al. Sleep in elite multi-sport athletes: implications for athlete health and wellbeing. Phys Ther Sport. 2019;39:136–142. doi:10.1016/j.ptsp.2019.07.006
45. Halson SL, Johnston RD, Piromalli L, et al. Sleep regularity and predictors of sleep efficiency and sleep duration in elite team sport athletes. Sp Med Open. 2022;8(1). doi:10.1186/s40798-022-00470-7
46. Woelders T, Beersma DGM, Gordijn MCM, Hut RA, Wams EJ. daily light exposure patterns reveal phase and period of the human circadian clock. J Biol Rhyth. 2017;32(3):274–286. doi:10.1177/0748730417696787
47. Siraji MA, Lazar R, Duijnhoven J, et al.. Light exposure behaviour assessment (LEBA): a novel self-reported instrument to capture light exposure-related behaviour; 2022.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.