Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Higher Neutrophil-Percentage-to-Albumin Ratio Was Associated with Poor Outcome in Endovascular Thrombectomy Patients
Authors Xu M, Zhai Q, Wei B, Chen S, E Y, Huang Z, Qi J, Xu Y
Received 31 January 2025
Accepted for publication 18 April 2025
Published 26 April 2025 Volume 2025:21 Pages 565—573
DOI https://doi.org/10.2147/TCRM.S519263
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Maoxia Xu,* Qian Zhai,* Bin Wei,* Shuaiyu Chen, Yan E, Zhihang Huang, Jinwen Qi, Yiming Xu
Department of Neurology, Nanjing First Hospital, Nanjing Medical University, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yiming Xu, Department of Neurology, Nanjing First Hospital, Nanjing Medical University, No. 86 Changle Road, Nanjing, Jiangsu Province, 210000, People’s Republic of China, Tel/Fax +86 02552271000, Email [email protected]
Background and Purpose: The neutrophil percentage-to-albumin ratio (NPAR) is connected with all-cause mortality and stroke-related pneumonia. The purpose of this study was to assess the diagnostic efficacy of NPAR in predicting functional outcomes at 90 days after endovascular thrombectomy (EVT).
Methods: We retrospective analyzed consecutive patients who underwent EVT at Nanjing First Hospital from October 2019 to June 2024. NPAR was defined as the percentage of neutrophils divided by the albumin levels. An unfavorable outcome was indicated by a modified Rankin Scale score of 3– 6 at 90 days. Multivariable logistic regression models were utilized to investigate the association between NPAR and functional outcomes after EVT treatment.
Results: A total of 713 patients (mean age, 70.5 ± 11.9 years; 430 males) were finally enrolled for analysis. Among these, 357 (50.1%) patients exhibited unfavorable outcomes at 90 days. Multivariate regression analysis indicated that elevated NPAR levels at admission were independently associated with poor outcome (adjusted odds ratio: 6.921; 95% confidence interval, 4.216– 11.363; P= 0.001) in ischemic stroke patients undergoing EVT. Furthermore, the restricted cubic spline observed a positive and nonlinear association between the NPAR and poor outcome at 90 days (P for linearity=0.001).
Conclusion: This study indicated that higher NPAR levels were associated an increased risk of poor outcome at 90 days in patients treated with EVT, suggesting that NPAR could serve as a viable prognostic biomarker for ischemic stroke after EVT.
Keywords: ischemic stroke, NPAR, albumin, thrombectomy
Introduction
Ischemic stroke is a leading global cause of death and disability.1 Recent randomized controlled trials demonstrated that endovascular thrombectomy (EVT) is beneficial for acute ischemic stroke patients resulting from proximal anterior circulation artery occlusion.2 Despite the prolonged time window for EVT, the incidence of mortality and disability stemming from ischemic stroke and its consequences remains high.3 Therefore, it is essential to stratify patients with high-risk of unfavorable functional outcome accurately after EVT.
Numerous studies highlight the significant impact of infection on stroke, which greatly affects prognosis.4,5 Neutrophils serve a dual role; besides their antimicrobial function, their dysregulation and hyperactivity may lead to tissue damage following severe inflammation or trauma.6 Neutrophils also play a detrimental role in atherogenesis, especially during the initial stages marked by endothelial dysfunction and the onset of vascular inflammation, as well as in advanced atherosclerosis associated with plaque rupture and atherothrombosis.7 It has been suggested that neutrophils are considerably elevated in individuals with poor clinical outcome at 3 months.8 Furthermore, decreased albumin levels also result in negative consequences for patients with ischemic stroke.9 The neutrophil-percentage-to-albumin ratio (NPAR) serves as a readily available and effective indicator of inflammation, calculated from the neutrophil percentage and albumin concentration. Emerging evidence has established that the NPAR demonstrates significant prognostic utility across distinct stroke domains. Population-based studies have established its positive correlation with overall stroke incidence.10 In hemorrhagic stroke specifically, elevated NPAR levels independently predict unfavorable functional outcome following spontaneous intracerebral hemorrhage.11 Furthermore, NPAR exhibits prognostic value for critical stroke complications including: stroke-associated pneumonia risk stratification,11 all-cause mortality12 and ischemic stroke recurrence.13
While the prognostic significance of NPAR has been established in general stroke populations, its association with clinical outcomes in EVT-treated patients remains unclear. Therefore, we performed this study using a retrospective cohort to evaluate the relationship between NPAR levels and 90-day functional outcomes in anterior circulation ischemic stroke patients undergoing EVT.
Subjects and Methods
Study Design and Population
A retrospective analysis was performed on consecutive patients with acute occlusive stroke in the proximal anterior circulation arteries who had EVT treatment at Nanjing First Hospital (Nanjing, Jiangsu province, China) from October 2019 to June 2024. The criteria for inclusion were as follows: (1) individuals aged 18 years or older; (2) diagnosed with acute proximal vascular occlusion in the anterior circulation (internal carotid artery and middle cerebral artery: M1/M2 segments); (3) and had accessible data for the calculation of the NPAR. We excluded patients meeting any of the following criteria: (1) recent infection within two weeks preceding stroke onset; (2) significant hepatic or renal dysfunction; (3) active malignancies including hematologic disorders (leukemia, myelodysplastic syndromes) and solid tumors; (4) diagnosed autoimmune conditions. We also excluded patients who underwent EVT exclusively with intra-arterial thrombolysis. All procedures performed in studies involving human participants were reviewed and approved by the Ethics Committee of Nanjing First Hospital. This study complies with the Declaration of Helsinki. Due to its retrospective nature; patient consent was waived by the Ethics Committee of Nanjing First Hospital. Patient data confidentiality was maintained in Nanjing First Hospital.
Baseline Variable Collection
The demographic and clinical data, including age, sex, admission blood pressure, vascular risk factors, National Institutes of Health Stroke Scale (NIHSS), and infarct volume, and Trial of Org 10,172 in Acute Stroke Treatment (TOAST) subtypes were collected after admission. Hypertension was defined as either (1) systolic/diastolic blood pressure ≥140/90 mmHg recorded on three separate occasions, or (2) current use of antihypertensive medications regardless of blood pressure readings. Hyperlipidemia was defined as a total cholesterol concentration ≥5.7 mmol/L, triglyceride concentration ≥1.7 mmol/L, low-density lipoprotein-cholesterol concentration≥3.6 mmol/L, and/or having received treatment for dyslipidemia. Diabetes mellitus was defined as either a fasting blood glucose level ≥7.0 mmol/L or current use of glucose-lowering medications.
Pre-treatment infarction core was quantified using the Alberta Stroke Program Early Computerized Tomography (ASPECT) score. The American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology grading system were used to evaluate the collateral blood status, with grades 0–1 indicating poor collateral circulation and grades 2–4 indicating moderate to excellent.14 Successful recanalization was defined as modified thrombolysis in a cerebral infarction score of 2b or 3.15 The sICH was diagnosed using the Heidelberg Bleeding Classification within 72 hours following EVT.16 All angiography and computed tomography imaging were reviewed by 2 physicians who were blinded to the clinical outcomes. In case of disagreement, a third physician was invited for a final decision. Upon patient arrival at the emergency department, venous blood samples were immediately collected. Complete blood count analysis including leukocyte, neutrophil, and lymphocyte quantification, along with serum albumin levels, were determined using a standardized automated biochemical analyzer. NPAR was defined as the percentage of neutrophils divided by the albumin levels.
Outcome Assessment
The modified Rankin Scale (mRS) is widely adopted for assessing functional outcomes in stroke patients. Standardized 3-month poststroke follow-up assessments were conducted by certified neurologists through either structured telephone interviews or in-person clinic visits. The primary study outcome was poor functional outcome, which defined as mRS score ranging from 3–6.17
Statistical Analysis
Data analysis was performed using SPSS version 24.0 (IBM, Armonk, New York) and R (version 4.2.2). Categorical variables were calculated as count (percentage), and continuous variables were presented as mean (± standard deviation [SD]) or median (interquartile range [IQR]). The Mann–Whitney U-test, Student’s t-test, Fisher’s exact test, or Chi-square test were used to conduct the comparisons as appropriate. We performed the binary logistical regression analysis to evaluate the association of NPAR with 90-day poor outcome. Multivariable regression model was adjusted for age, sex, and variables with a P < 0.1 in the univariate analysis including baseline NIHSS score, baseline ASPECTS, poor collateral status, successful reperfusion, sICH, and NPAR levels. Furthermore, we also evaluated the pattern and magnitude of the relationship between NPAR and poor outcome using a logistic regression model with restricted cubic splines with 3 knots (at 5th, 50th and 95th percentiles) adjusted for covariates in model 3.
Results
Baseline Characteristics
The study cohort consisted of 713 consecutive participants for final analysis. The baseline demographic, clinical, and radiological characteristics were listed in Table 1. The average age was 70.5 years, with a male percentage of 60.3%. The median baseline NIHSS was 14.0 (interquartile range, 10.0–17.0), the baseline ASPECTS was 9.0 (interquartile range, 8.0–10.0), and 37.7% of patients received prior intravenous thrombolysis. Successful reperfusion was successfully accomplished in 89.5% of patients. According to the Heidelberg Bleeding Classification, 81 patients (11.5%) were categorized as having sICH. Age and baseline NIHSS score differed significantly with increasing categories of NPAR quartile (Table 1).
 |
Table 1 Baseline Characteristics Stratified by the Quartile of NPAR Score |
Associations Between NPAR and Clinical Outcomes
During the 90 days follow-up, 357 patients (50.1%) experienced an unfavorable outcome. The clinical, laboratory, and imaging characteristics of patients with and without poor outcome were illustrated in Table 2. In univariate analysis, patients with poor outcome were older than those with favorable outcomes (mean age, 72.3±11.2 years versus 68.8±12.3 years; P=0.001). The elevated baseline NIHSS (median, 14.0 versus 10.0; P = 0.002), diminished baseline ASPECTS (median, 9.0 versus 9.0; P = 0.022), unsuccessful reperfusion (87.1% versus 91.9%; P = 0.039), poor collateral circulation (57.4% versus 48.9%; P = 0.022), and sICH (14.6% versus 8.1%; P = 0.007) were more prevalent in the unfavorable outcome group, as compared to the favorable group. Moreover, baseline NPAR was elevated in patients with poor outcome compared to those without it (mean, 2.46 ± 1.13 versus 2.0 ± 0.71; P=0.001).
 |
Table 2 Clinical Characteristics of Study Participants According to Patients With Unfavorable Outcome at 3 months |
In the multivariable analysis, higher NPAR levels were substantially correlated with an increased risk of poor outcome at 90 days in EVT patients (odds ratio, 6.921; 95% confidence range, 4.216–11.363; P = 0.001). In addition, the restricted cubic spline indicated a linear relationship between NPAR and unfavorable functional outcome at 90 days (P for linearity=0.001; Figure 1).
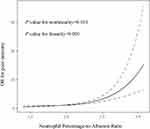 |
Figure 1 Association was fitted with restricted cubic spline with 3 knots (at 5th, 55th, 95th percentiles) adjusted for covariates included in model 3 in Table 3. The reference point for NPAR levels were the midpoint of the reference group from categorical analysis. |
 |
Table 3 Binary Regression Analysis for the Association Between NPAR Score and Unfavorable Outcome at 3 months |
Discussion
Our study found an elevated NPAR at admission as an independent risk factor for poor functional outcome in patients treated with EVT. The correlation persisted even after controlling for potential confounding variables including baseline NIHSS, pre-treatment ASPECTS, poor collateral status, successful reperfusion, sICH.
Accumulating evidence indicates that standardized inflammatory scores have been integrated into contemporary clinical algorithms for prognostic stratification.18 The NPAR, as an innovative inflammatory biomarker, may assist in forecasting the outcome in patients undergoing EVT. It indicates that elevated systemic inflammation correlates with poorer short-term functional results in patients following EVT. This study aimed to assess the correlation between NPAR and poor outcome at 90 days after EVT. This result corresponds with the increasing comprehension of systemic inflammation’s role in stroke causation and its impact on neurological recovery after ischemic brain injury.19 Previous researches had established that many inflammatory indices are associated with unfavorable outcomes at 90 days in individuals with ischemic stroke.20–22 Significantly, unlike other hematologic inflammatory markers such as interleukin-6, neutrophil-to-lymphocyte ratio, and eosinophil-to-lymphocyte ratio, the NPAR include albumin, a nutritional indicator. Decreased serum albumin levels were found to be independently linked to a poor prognosis at 90 days in large vessel occlusive patients after EVT.23 Our study extended the current knowledge about the adverse influence of NPAR in ischemic stroke as it demonstrated a negative association between NPAR levels and poor prognosis in patients treated with EVT.
The mechanisms by which NPRA affects clinical outcomes in ischemic stroke patients after EVT are not completely understood, but several underlying pathophysiological pathways have been postulated. Firstly, during stroke events, neutrophils may be swiftly recruited to ischemic brain regions, releasing matrix metalloproteinases-9 (MMP-9), which degrade tight junction proteins and basal lamina type IV collagen, thereby enhancing blood-brain barrier permeability, leading to BBB disruption and tissue damage, accompanied by edema and hemorrhage.24–27 It has been demonstrated that neutrophils activate platelets, endothelial cells, and antigen-presenting cells, triggering a proinflammatory immune response in atherogenesis and atherothrombosis.28 Additionally, neutrophils may trigger the production of cytokines by macrophages and activate T helper 17 cells by producing NETs, which would increase pro-inflammatory reactions and lead to the instability and rupture of atherosclerotic plaque.28,29 Secondly, collateral blood flow is crucial for preserving hemoperfusion when major vascular occlusion takes place.30 Another risk factor for a poor outcome during endovascular therapy of ischemic stroke is hypotension.31 Since serum albumin plays a major role in colloidal osmotic pressure, low levels of this protein can both decrease collateral flow and increase infarct edema, which can result in a poor clinical outcome for large artery occlusive stroke following EVT. More neurons may be saved and infarct expansion pressing on healthy brain tissue may be avoided if the ischemic infarct area receives adequate blood perfusion. According to experimental research, albumin’s clinically significant inhibitory effect on the erythrocyte sedimentation rate increases cerebral blood flow.32 In addition, serum albumin could restrain platelet aggregation, reduce the various cytokines adhesion within postcapillary microcirculation,33,34 and inhibit carotid atherosclerosis.35
The study’s methodological strengths include (1) a sufficiently powered sample size and (2) the inclusion of a well-defined homogeneous cohort of ischemic stroke patients undergoing EVT, both of which enhance the validity of investigating the correlation between NPAR levels and clinical outcome. However, this study has several limitations should be addressed. Firstly, because this was a retrospective trial, we were unable to determine the causal relationship between NPAR and 90-day poor outcome. Secondly, this study relied on a registry that retrospectively collected patient related-data, which inevitably induced systematic bias. Thirdly, additional follow-up measures were required because the NPAR levels were only assessed once following admission. Therefore, the interpretation of our results should be approached with caution.
In conclusion, this study demonstrated that elevated NPAR levels were significantly associated with unfavorable 90-day functional outcomes in ischemic stroke patients undergoing EVT. These findings underscored the need for large-scale prospective multicenter studies to validate the prognostic value of this novel inflammatory biomarker and elucidate the underlying pathophysiological mechanisms.
Data Sharing Statement
The raw data supporting this study’s findings are available on request from the corresponding author, without undue reservation.
Ethics Approval and Consent to Participate
All procedures performed in studies involving human participants were reviewed and approved by the Ethics Committee of Nanjing First Hospital. This study complies with the Declaration of Helsinki. Due to its retrospective nature; patient consent was waived by the Ethics Committee of Nanjing First Hospital. Patient data confidentiality was maintained in Nanjing First Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was partly supported by the Science and Technology Development Fund of Nanjing Medical University (NMUB2019181).
Disclosure
All the authors declare that there is no conflict of interest.
References
1. Tu WJ, Wang LD; Special Writing Group of China Stroke Surveillance Report. China stroke surveillance report 2021. Mil Med Res. 2023;10(1):33. doi:10.1186/s40779-023-00463-x
2. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–1731. doi:10.1016/S0140-6736(16)00163-X
3. Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21. doi:10.1056/NEJMoa1706442
4. Elkind MSV, Boehme AK, Smith CJ, Meisel A, Buckwalter MS. Infection as a stroke risk factor and determinant of outcome after stroke. Stroke. 2020;51(10):3156–3168. doi:10.1161/STROKEAHA.120.030429
5. Parikh NS, Merkler AE, Iadecola C. Inflammation, autoimmunity, infection, and stroke: epidemiology and lessons from therapeutic intervention. Stroke. 2020;51(3):711–718. doi:10.1161/STROKEAHA.119.024157
6. Mortaz E, Alipoor SD, Adcock IM, Mumby S, Koenderman L. Update on neutrophil function in severe inflammation. Front Immunol. 2018;9:2171. doi:10.3389/fimmu.2018.02171
7. Chistiakov DA, Bobryshev YV, Orekhov AN. Neutrophil’s weapons in atherosclerosis. Exp mol Pathol. 2015;99(3):663–671. doi:10.1016/j.yexmp.2015.11.011
8. Semerano A, Laredo C, Zhao Y, et al. Leukocytes, collateral circulation, and reperfusion in ischemic stroke patients treated with mechanical thrombectomy. Stroke. 2019;50(12):3456–3464. doi:10.1161/STROKEAHA.119.026743
9. Babu MS, Kaul S, Dadheech S, Rajeshwar K, Jyothy A, Munshi A. Serum albumin levels in ischemic stroke and its subtypes: correlation with clinical outcome. Nutrition. 2013;29(6):872–875. doi:10.1016/j.nut.2012.12.015
10. Ye C, Mo Y, Su T, et al. Cross-sectional study on the association between neutrophil-percentage-to-albumin ratio (NPAR) and prevalence of stroke among US adults: NHANES 1999-2018. Front Neurol. 2025;16:1520298. doi:10.3389/fneur.2025.1520298
11. Lv XN, Shen YQ, Li ZQ, et al. Neutrophil percentage to albumin ratio is associated with stroke-associated pneumonia and poor outcome in patients with spontaneous intracerebral hemorrhage. Front Immunol. 2023;14:1173718. doi:10.3389/fimmu.2023.1173718
12. Chen Z, Xie D, Li Y, et al. Neutrophil albumin ratio is associated with all-cause mortality in stroke patients: a retrospective database study. Int J Gen Med. 2022;15:1–9. doi:10.2147/IJGM.S323114
13. Yang D, Niu C, Li P, Du X, Zhao M, Jing W. Study of the neutrophil percentage-to-albumin ratio as a biomarker for predicting recurrence of first-episode ischemic stroke. J Stroke Cerebrovasc Dis. 2024;33(1):107485. doi:10.1016/j.jstrokecerebrovasdis.2023.107485
14. Zaidat OO, Yoo AJ, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650–2663. doi:10.1161/STROKEAHA.113.001972
15. Zhang X, Yuan K, Wang H, et al. Nomogram to predict mortality of endovascular thrombectomy for ischemic stroke despite successful recanalization. J Am Heart Assoc. 2020;9(3):e014899. doi:10.1161/JAHA.119.014899
16. von Kummer R, Broderick JP, Campbell BC, et al. The heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015;46(10):2981–2986. doi:10.1161/STROKEAHA.115.010049
17. Zhang X, Peng M, Feng C, et al. Nomogram predicting early neurological improvement in ischaemic stroke patients treated with endovascular thrombectomy. Eur J Neurol. 2021;28(1):152–160. doi:10.1111/ene.14510
18. Cicek V, Kilic S, Dogan S, et al. Predictive value of inflammatory scores for left atrium thrombosis in ischemic stroke without atrial fibrillation. Medicina. 2024;60:2046. doi:10.3390/medicina60122046
19. Simats A, Liesz A. Systemic inflammation after stroke: implications for post-stroke comorbidities. EMBO Mol Med. 2022;14(9):e16269. doi:10.15252/emmm.202216269
20. Dargazanli C, Blaquière M, Moynier M, et al. Inflammation biomarkers in the intracranial blood are associated with outcome in patients with ischemic stroke. J Neurointerv Surg. 2025;17(2):159–166. doi:10.1136/jnis-2023-021365
21. Cao W, Song Y, Bai X, et al. Systemic-inflammatory indices and clinical outcomes in patients with anterior circulation acute ischemic stroke undergoing successful endovascular thrombectomy. Heliyon. 2024;10(10):e31122. doi:10.1016/j.heliyon.2024.e31122
22. Han Y, Lin N. Systemic inflammatory response index and the short-term functional outcome of patients with acute ischemic stroke: a meta-analysis. Neurol Ther. 2024;13(5):1431–1451. doi:10.1007/s40120-024-00645-2
23. Gao J, Zhao Y, Du M, et al. Serum albumin levels and clinical outcomes among ischemic stroke patients treated with endovascular thrombectomy. Neuropsychiatr Dis Treat. 2021;17:401–411. doi:10.2147/NDT.S293771
24. Price CJ, Menon DK, Peters AM, et al. Cerebral neutrophil recruitment, histology, and outcome in acute ischemic stroke: an imaging-based study. Stroke. 2004;35(7):1659–1664. doi:10.1161/01.STR.0000130592.71028.92
25. Perez-de-Puig I, Miró-Mur F, Ferrer-Ferrer M, et al. Neutrophil recruitment to the brain in mouse and human ischemic stroke. Acta Neuropathol. 2015;129(2):239–257. doi:10.1007/s00401-014-1381-0
26. Gidday JM, Gasche YG, Copin JC, et al. Leukocyte-derived matrix metalloproteinase-9 mediates blood-brain barrier breakdown and is proinflammatory after transient focal cerebral ischemia. Am J Physiol Heart Circ Physiol. 2005;289(2):H558–68. doi:10.1152/ajpheart.01275.2004
27. Maestrini I, Strbian D, Gautier S, et al. Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes. Neurology. 2015;85(16):1408–1416. doi:10.1212/WNL.0000000000002029
28. Döring Y, Soehnlein O, Weber C. Neutrophil extracellular traps in atherosclerosis and atherothrombosis. Circ Res. 2017;120(4):736–743. doi:10.1161/CIRCRESAHA.116.309692
29. Warnatsch A, Ioannou M, Wang Q, Papayannopoulos V. Inflammation. Neutrophil extracellular traps license macrophages for cytokine production in atherosclerosis. Science. 2015;349(6245):316–320. doi:10.1126/science.aaa8064
30. Rocha M, Jovin TG. Fast versus slow progressors of infarct growth in large vessel occlusion stroke: clinical and research implications. Stroke. 2017;48(9):2621–2627. doi:10.1161/STROKEAHA.117.017673
31. Löwhagen Hendén P, Rentzos A, Karlsson JE, et al. Hypotension during endovascular treatment of ischemic stroke is a risk factor for poor neurological outcome. Stroke. 2015;46(9):2678–2680. doi:10.1161/STROKEAHA.115.009808
32. Reinhart WH, Nagy C. Albumin affects erythrocyte aggregation and sedimentation. Eur J Clin Invest. 1995;25(7):523–528. doi:10.1111/j.1365-2362.1995.tb01739.x
33. Maalej N, Albrecht R, Loscalzo J, Folts JD. The potent platelet inhibitory effects of S-nitrosated albumin coating of artificial surfaces. J Am Coll Cardiol. 1999;33(5):1408–1414. doi:10.1016/S0735-1097(98)00687-1
34. Grigoriadis G, Stewart AG. Albumin inhibits platelet-activating factor (PAF)-induced responses in platelets and macrophages: implications for the biologically active form of PAF. Br J Pharmacol. 1992;107(1):73–77. doi:10.1111/j.1476-5381.1992.tb14465.x
35. Ishizaka N, Ishizaka Y, Nagai R, Toda E, Hashimoto H, Yamakado M. Association between serum albumin, carotid atherosclerosis, and metabolic syndrome in Japanese individuals. Atherosclerosis. 2007;193(2):373–379. doi:10.1016/j.atherosclerosis.2006.06.031
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

