Back to Journals » Journal of Pain Research » Volume 18
Impact of Carotid Interventions on Headache Relief in Patients with Carotid Stenosis: a Retrospective Analysis of Carotid Endarterectomy Versus Stenting
Authors Arslanturk O , Gur AK, Ada F , Keskin E
Received 9 December 2024
Accepted for publication 20 March 2025
Published 24 March 2025 Volume 2025:18 Pages 1587—1596
DOI https://doi.org/10.2147/JPR.S511101
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rune Häckert Christensen
Oguz Arslanturk,1 Ali Kemal Gur,1 Fatih Ada,2 Emrah Keskin3
1Department of Cardiovascular Surgery, Zonguldak Bülent Ecevit University, Faculty of Medicine, Zonguldak, Turkey; 2Department of Cardiovascular Surgery, Sivas Cumhuriyet University, Faculty of Medicine, Sivas, Turkey; 3Department of Neurosurgery, Zonguldak Bülent Ecevit University, Faculty of Medicine, Zonguldak, Turkey
Correspondence: Oguz Arslanturk, Department of Cardiovascular Surgery, Zonguldak Bülent Ecevit University, Faculty of Medicine, Zonguldak, Turkey, Tel +90 539 5613887, Email [email protected]
Objective: To evaluate the impact of carotid endarterectomy (CEA) and carotid artery stenting (CAS) on postoperative headache outcomes in patients with carotid artery stenosis, comparing changes in pre-existing headache intensity and the incidence of new-onset headaches.
Materials and Methods: We conducted a retrospective cohort analysis on 284 patients who underwent CEA (n=167) or CAS (n=117) between January 2018 and December 2023. Pre- and postoperative headache characteristics were documented at baseline and 24 h, 1 month, and 6 months after the intervention. We evaluated headache frequency, intensity (using the Numeric Rating Scale [NRS]), and duration while focusing on changes in pre-existing headaches and the incidence of new headaches.
Results: Patients who underwent CEA had a greater reduction in headache intensity at 24 h (NRS median 4, Interquartile range [IQR]: 2– 6) compared with those who underwent CAS (NRS median 6, IQR: 2– 7; p=0.038). At 1 month, the CEA group continued to show lower headache scores (median 2, IQR: 1– 3) compared with the CAS group (median 3, IQR 2– 4; p=0.045). At 6 months, both groups had similar levels of headache resolution (p=0.785). Patients who underwent CAS had higher incidences of new-onset headache than those with CEA at 24 h (34.1% vs 20.3%; p=0.033) and 1 month (26.4% vs 13.1%; p=0.018), but converged by 6 months.
Conclusion: This study highlights the differential impacts of CEA and CAS on headache outcomes, with CEA showing a lower incidence and intensity of postoperative headaches. These findings underscore the need to consider patient-reported symptoms in treatment planning to enhance the quality of life. Further prospective research is essential to corroborate these observations and explore the mechanisms underlying headache outcomes after carotid interventions.
Keywords: carotid artery stenosis, carotid endarterectomy, carotid artery stenting, headache
Introduction
Carotid artery stenosis is an important risk factor for stroke,1 and carotid revascularization is important for reducing stroke risk in patients with moderate-to-severe carotid stenosis. The North American Symptomatic Carotid Endarterectomy Trial showed a definitive benefit of carotid endarterectomy (CEA) in patients with symptomatic 70–99% internal carotid artery (ICA) stenosis.2 There are two techniques used for carotid revascularization: CEA, which involves the surgical removal of atherosclerotic plaques, and carotid artery stenting (CAS), which involves placing a stent to widen the narrowed artery. Both methods effectively reduce the incidence of stroke, but have different procedural characteristics and effects.3,4 The late 20th century Carotid and Vertebral Artery Transluminal Angioplasty Trial reported an incidence of death or stroke in the first 3 years.5 Similarly, in the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study, the adverse events between the two groups did not differ at the 2-year follow-up.6 Notably, studies comparing CAS and CEA have focused primarily on major adverse events, including myocardial infarction, stroke, and mortality.5–7 However, headaches are a common symptom of ischemic cerebrovascular diseases. Fisher8 observed headache occurrence in 31% of individuals with ICA disease. Edmeads and Barnett9 reported a similar prevalence, with 35% of patients with carotid artery disease experiencing headache. Major adverse events are commonly studied, but post-procedural symptom management, such as headache relief, is less well explored. Limited research has explored post-procedural headache, yet, to date,10–12 no direct comparison of headache outcomes following CAS and CEA exists in the literature. In this retrospective study, we aimed to address this gap by comparing the incidence and severity of postprocedural headaches in patients with carotid artery stenosis who underwent CAS or CEA, offering insights into symptom relief outcomes following revascularization.
Materials and Methods
Study Design and Population
This retrospective monocentric study was conducted at Zonguldak Bülent Ecevit University, Faculty of Medicine, between January 2018 and December 2023. All procedures were performed by multiple experienced cardiovascular and neurosurgeons following standardized institutional protocols to ensure consistency in patient management. This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and received ethical approval from the Zonguldak Bulent Ecevit University Clinical Research Ethics Committee (Approval Number: 2024/23). Given the retrospective nature of the study, the requirement for informed consent was formally waived by the Ethics Committee. To protect participant privacy, all data were fully anonymized, and only de-identified information was made available for analysis by the research team.
We included patients who met the specific eligibility requirements for assessing preoperative headache status and postoperative headache outcomes. The inclusion criteria were adults aged ≥ 18 years with documented symptomatic carotid artery stenosis on one side (unilateral stenosis). Eligible patients underwent either CEA or CAS for revascularization, and procedural consistency was ensured by using a patch for only those receiving CEA with closure, without using a shunt. Documentation of headache symptoms before the intervention was required to allow for a comparative analysis of headache frequency and intensity before and after the procedure. In addition, patients were evaluated for new-onset headaches after the intervention.
Inclusion and Exclusion Criteria
These exclusion criteria further refined the study sample. Patients with incomplete or insufficient medical records and those with primary headache disorders (chronic migraine) or unrelated neurological conditions that could confound headache outcomes were excluded. We also excluded cases of bilateral carotid stenosis to focus on unilateral intervention outcomes. Patients who received CEA and underwent closure without a patch or with shunting were excluded to maintain consistency with the specified patch closure protocol. Finally, we excluded patients with asymptomatic stenosis lacking documented preoperative headaches or ischemic symptoms.
Operative Techniques
Carotid Endarterectomy (CEA)
CEA procedures were performed under either general or local anesthesia, depending on the patient and surgical considerations. A longitudinal incision was made to access the carotid artery, and careful dissection exposed the area of atherosclerotic plaque. After complete plaque removal, the artery was reconstructed using patch angioplasty patch angioplasty with a synthetic or autologous patch to ensure sufficient vessel diameter and reduce the risk of future narrowing. Consistent with this protocol, no routine intraoperative shunting was performed, Postoperatively, the patients were observed closely for any immediate complications, and their headache status was evaluated at designated follow-up times.
Carotid Artery Stenting (CAS)
CAS was performed under local anesthesia with light sedation to allow patient feedback during the procedure. Access was obtained through the femoral artery, and a guiding catheter was advanced to the stenotic segment of the carotid artery. The embolic risk was minimized using a distal embolic protection device (EPD) in all cases. Cerebral protection was ensured utilizing either the Emboshield NAV (Abbott Vascular, Santa Clara, CA, USA) or the SpiderFX (Medtronic, Plymouth, MN, USA). Balloon angioplasty was performed to pre-dilate the stenosis, after which a self-expanding nitinol stent was placed to maintain vessel patency. Post-deployment, the embolic protection device was retrieved, and completion angiography was performed to confirm revascularization success. The patients were monitored postoperatively, and headache assessments were conducted according to the study’s follow-up schedule.
CEA and CAS were performed by specialists with extensive experience in carotid interventions, who adhered to standardized institutional protocols to maintain consistency across cases.
Postoperative Care and Monitoring
After both procedures, the patients were monitored in the intensive care unit for 24 h. Intravenous heparin administration commenced 3 h after the procedure and was continued for 24 h to maintain anticoagulation. Crucial parameters, including arterial blood pressure, heart rate, and any neurological changes, were recorded throughout the perioperative period. Observations included monitoring for neurological complications, transient ischemic events, and signs of hyperperfusion syndrome such as headache, seizures, confusion, neurological deficits, and elevated blood pressure (systolic >150 mmHg and/or diastolic >90 mmHg). To ensure comprehensive postoperative evaluation, all patients underwent routine follow-up assessments, including carotid Duplex ultrasound (DUS) at 1 and 6 months, as per institutional protocols. While this study primarily focuses on headache outcomes rather than vascular patency, DUS findings were reviewed to rule out significant hemodynamic changes that could contribute to postoperative symptoms. In cases where patients reported persistent or worsening headaches with neurological symptoms, computed tomography angiography (CTA) was selectively performed to exclude vascular complications.
Data Collection
Data were extracted from medical records at four designated time points: preoperative (baseline) and 24 h, 1 month, and 6 months postoperatively. Patients’ baseline demographic and clinical information, including age, sex, comorbidities (such as hypertension and diabetes), degree of carotid stenosis, and characteristics of any pre-existing headaches (frequency, intensity, and duration) were documented to provide a reference for comparing the pre- and post-procedural headache outcomes.
Postoperative headache assessments were based on the patient-reported outcomes in the medical records. For each procedure, new-onset headaches were evaluated according to the International Classification of Headache Disorders, 3rd edition (ICHD-3).13
The criteria for diagnosing post-endarterectomy headache (ICHD-3 section 6.5.2)13 for patients who underwent CEA are as follows: a new headache must develop within 1 week of the procedure, be localized to the side of the surgery, and exhibit specific characteristics such as diffuse mild pain, cluster-like attacks, or severe pulsating pain.
The criteria for diagnosing headache attributed to carotid or vertebral angioplasty or stenting (ICHD-3 section 6.5.3)13 for patients who received CAS are as follows: the headache must develop within 1 week post-procedure, be on the same side as the stenting, and resolve within 1 month if related to the intervention.
The classification of post-procedural headaches followed the International Classification of Headache Disorders, 3rd edition (ICHD-3), ensuring standardized diagnostic criteria for Post-Endarterectomy Headache and Headache Attributed to Stenting.13
At each follow-up (24 h, 1 month, and 6 months), headache characteristics, including frequency, intensity (measured using the Numeric Rating Scale [NRS] from 0, indicating no pain, to 10, indicating the most severe pain), and duration were retrospectively recorded. Patients with migraines were excluded from the postoperative NRS scoring to avoid skewed results. This systematic data collection enabled consistent tracking of changes in the characteristics of pre-existing headaches and the identification of new-onset headaches based on the ICHD-3 criteria.
Outcome Measures
The primary outcome measures were changes in the characteristics of pre-existing headaches before and after the procedure, including frequency, intensity, and duration. In addition, the persistence or resolution of these pre-existing headaches at each follow-up interval was assessed.
The secondary outcome measures were the occurrence and characterization of new-onset headaches following the intervention. These new-onset headaches were identified and characterized using the ICHD-3 criteria.13 This standardized approach facilitated the objective evaluation of postprocedural headache outcomes specific to each intervention type (CEA or CAS).
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows version 25 (IBM Corp., Armonk, NY, USA). The normality of the quantitative variables was checked using the Kolmogorov–Smirnov test. For comparisons between groups, independent sample t-tests were applied to normally distributed data, whereas the Mann–Whitney U-test was used for non-normal data. The relationships between categorical variables were examined using Chi-square tests. Descriptive statistics are shown as mean ± standard deviation for normal data and median (25th-75th percentile) for non-normal data. Categorical data are presented as frequencies (%). Statistical significance was set at p < 0.05.
Results
Patient Demographics and Clinical Features
Of the 284 patients analyzed, 117 underwent CAS, and 167 underwent CEA. No significant differences were observed in the patient’s demographic or clinical variables, including age (CAS: 69.26 ± 8.26, CEA: 67.4 ± 9.2, p=0.082) and body mass index (CAS: 71.6 ± 5.23, CEA: 68.2 ± 4.9, p=0.819). Notably, both groups had similar proportions of patients with hypertension (p=0.421), diabetes mellitus (p=0.519), and dyslipidemia (p=0.241). A greater percentage of severe ICA stenosis (≥ 90%) was noted in patients who underwent CAS (50.5%) compared to those who underwent CEA (49.5%), though not significantly different (p=0.397) (Table 1).
 |
Table 1 Demographic and Clinical Characteristics of Patients |
Preoperative Headache Characteristics
When comparing headache data between the CAS and CEA groups, headache types, average durations, and pain localization were analyzed individually. All variables showed a similar distribution across both groups with no statistically significant differences (p > 0.05) (Table 2). Additionally, preoperative monthly headache days were comparable between the two groups, with a median of 11 days (IQR: 6–15) in the CAS group and 12 days (IQR: 5–16) in the CEA group (p=0.241).
 |
Table 2 Preoperative Headache Characteristics |
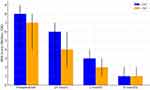
Postoperative Changes in Pre-Existing Headache Outcomes
The patients with pre-existing headaches in both groups experienced significant reductions in headache intensity after the procedure (Figure 1). At 24 h, the CEA group had a lower median NRS score (median 4, IQR: 2–6) than the CAS group (median 6, IQR: 2–7; p=0.038). At 1 month, the CEA group had a more favorable reduction in headache intensity (CEA: median 2, IQR: 1–3 vs CAS: median 3, IQR: 2–4, p=0.045). At 6 months, both groups showed similar outcomes, with a median NRS score of 1 (IQR: 1–2) (p=0.785) (Table 3). Moreover, postoperative monthly headache days at 6 months were lower in both groups compared to preoperative values, with a median of 5 days (IQR: 3–10) in the CAS group (down from 11 days [IQR: 6–15] preoperatively) and 4 days (IQR: 2–9) in the CEA group (down from 12 days [IQR: 5–16] preoperatively). While this represents a notable reduction in headache frequency over time in both groups, the comparison between CAS and CEA groups at 6 months showed no significant difference (p=0.372) (Table 3).
 |
Table 3 Changes in Pre-Existing Headache Outcomes Post-Procedure |
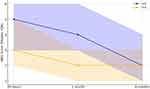
New-Onset Headache in Patients Without Pre-Existing Headaches
New-onset headaches were documented in 26% of the patients within 24 h after the procedure, with a higher frequency in the CAS group (34.1%) than in the CEA group (20.3%; p=0.033) (Table 4). The incidence of new-onset headaches at 1 month decreased to 18.6% across both groups, with the CAS group still presenting a higher frequency (26.4%) than the CEA groups (13.1%; p=0.018). At 6 months, this incidence further decreased to 10.2%, with no significant difference between the groups (p=0.272). Initial headache intensity, measured by NRS, was higher in patients who received CAS at 24 h (median 5, IQR: 3–6) than in those who received CEA (median 3, IQR: 2–5; p=0.045), with convergence in scores by 1 month (p=0.072) (Figure 2)
 |
Table 4 New-Onset Headache Outcomes Post-Procedure in Patients Without Pre-Existing Headaches |
Procedure-Related Headache Outcomes Based on ICHD-3
Based on the ICHD-3 criteria, headaches specifically attributed to the procedures were reported exclusively within their respective groups: 5.1% of patients in the CAS cohort experienced headaches attributed to stenting and 4.1% of patients in the CEA cohort reported post-endarterectomy headache. This indicated a specific postoperative headache type related to each intervention but without a notable difference in occurrence between the two techniques (Table 4).
Patients with a history of prior myocardial infarction (MI) or stroke were excluded from the study to ensure a more homogeneous cohort for headache assessment. Additionally, there was no statistically significant difference in postoperative stroke rates, perioperative mortality, or acute myocardial infarction (AMI) between the CEA and CAS groups (p > 0.05).
Discussion
Carotid artery stenosis is one of the most important causes of ischemic stroke.14,15 CEA or CAS has been established as an effective treatment for symptomatic and asymptomatic patients.7 The most common sites of headache in ICA stenosis or occlusion are the ipsilateral orbit and its surroundings.16 Revascularization aims to restore cerebral blood flow and prevent stroke; however, its impact on post-procedural symptoms, specifically headaches, warrants further exploration due to the observed variability in outcomes. Ipsilateral headaches may occur after CEA due to cerebral hyperperfusion syndrome (CHS). Reportedly, the incidence of CHS after CEA is 0–3%.17 Studies have shown that maximum blood flow after carotid stenting, with hyperperfusion symptom onset at the 6th postoperative hour, can occur within 3–4 d and stabilize on the 7th d.18–21 Postoperative CHS is a potential complication of CEA and is known to trigger headaches in approximately 20% of patients.20,22,23 Wagner et al investigated hyperperfusion syndrome after CEA in 1602 patients and reported that six patients (0.4%) developed hyperperfusion symptoms within 2 weeks post-surgery, and it caused three of five perioperative strokes (60%) and two of seven deaths (29%).24 In this study, we observed that the incidence of new-onset headache after CEA was 20% at 24 h, 13% at 1 month, and 7% at 6 months postoperatively. This study’s retrospective design did not allow for a direct assessment of hyperperfusion syndrome as a specific cause; however, our findings suggest that CEA is associated with a lower incidence of postoperative headache than CAS. The initially higher headache rates observed with CAS could be attributed to the mechanical effects of the stent pressing against the baroreceptor regions and displacing the vessel wall outward, as it addresses the stenotic area. This investigation serves as an important contribution to the comparative understanding of CEA and CAS, highlighting the advantage of CEA in terms of reducing headaches as a postoperative complication. Our findings provide a foundation for further prospective research to clarify the underlying mechanisms and confirm the symptomatic benefits of CEA over CAS in the context of headache outcomes.
Gündüz et al reported that headache was observed after CAS (39.1%) and angiography (21.9%).10 In our study, the incidence of headache within the first 24 h after CAS was 34%, which aligns with the findings of Gündüz et al. However, at the 1-month and 6-month mark, we observed a decline in the rate of new-onset headaches to 26% and 13%, respectively. These findings provide a unique perspective to the current literature, as this is the first study to document an extended trajectory of headache incidence after CAS beyond the immediate postoperative period.
Headaches occurring after cerebral angiography and endovascular procedures are rare, but they represent an important type of headache.11 Marti et al documented that after CAS, 21.4% of patients reported headaches typically occurring within the first 6 h post-procedure and lasting for an average of 2 h.12 The headaches were generally described as oppressive, mild-to-moderate in intensity, and localized unilaterally in the frontotemporal area. However, they did not provide further insight into whether these headaches recurred or diminished over time. Our study addresses this gap by demonstrating that 13% of patients who underwent CAS and 7% of those who underwent CEA experienced persistent headaches at 6 months post-procedure, although with a marked reduction in intensity.
The Carotid Revascularization Endarterectomy versus Stenting Trial reported a higher risk of stroke with stenting but a higher risk of myocardial infarction with endarterectomy.7 The SPACE study emphasizes that the risk of stroke or death increased significantly with age in the CAS group but not in the CEA group.25 However, no study has addressed whether existing headache patterns change post-procedure.8,9 Notably, some studies have noted the presence of headaches before intervention in patients who underwent CAS. However, none have provided details on the types of post-procedure headaches or intensity reduction. Our study demonstrated that pre-existing migraine-type headaches persisted post-intervention, indicating that carotid revascularization does not affect migraine-type headaches.
Tehindrazanarivelo et al reported that 31 (62%) out of 50 patients who underwent CEA had headaches, and only five of them had post-endarterectomy headaches according to the International Headache Society’s criteria.26 In our study, 20% of patients who underwent CEA reported headaches, with 4% meeting the ICHD-3 criteria, whereas 5% of patients who underwent CAS experienced headaches attributed to stenting. This variation may be influenced by differences in diagnostic criteria, as the ICHD-3 offers refined definitions that have evolved to improve the accuracy in classifying post-procedural headaches. The evolution of headache criteria highlights the importance of standardized definitions for evaluating the outcomes following carotid interventions. Our study aligns with prior findings on the incidence of post-CEA headaches; however, the lower rates of ICHD-3-defined post-endarterectomy headaches in our cohort suggest that the refined criteria may yield more precise assessments of the procedural impact.
This study contributes to a deeper understanding of the nuanced impact of carotid revascularization on post-procedural headache, an area often overlooked in clinical research. By directly comparing headache outcomes in patients undergoing CAS versus CEA, our findings revealed distinct differences in the persistence and intensity of headaches over time, providing valuable insights into patient-centered outcomes beyond stroke prevention. The observed variations in headache patterns underscore the importance of considering the procedural effects on symptom relief, helping guide clinical decisions in selecting the most appropriate intervention. This study fills a gap in the literature regarding long-term headache outcomes after carotid interventions and sets a foundation for future research aimed at improving patient quality of life post-revascularization.
Limitation
This study’s retrospective design restricted the ability to ascertain causal relationships between the intervention type and headache outcomes. In addition, reliance on medical records for headache assessment may introduce reporting bias, particularly for headache characteristics that are not consistently documented. Excluding patients with bilateral carotid stenosis limits the generalizability of our findings. Prospective studies with larger and more diverse populations, as well as standardized headache assessments, are necessary to further validate these results.
Conclusions
This study provides valuable insights into the differential effects of CEA and CAS on post-procedural headache outcomes. While both interventions effectively reduce stroke risk, CEA is associated with a lower incidence and intensity of persistent headaches compared to CAS. These findings highlight the importance of considering patient-reported symptoms when selecting treatment strategies. Given the retrospective nature of the study, further prospective research is warranted to validate these findings and explore the underlying mechanisms influencing post-procedural headache outcomes.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. Due to the retrospective nature of the study and the inclusion of patient-specific information, data sharing is subject to ethical and privacy restrictions as outlined by the Institutional Review Board.
Acknowledgments
We extend our gratitude to the medical team at the Zonguldak Bulent Ecevit University Hospital for their assistance with data collection and patient care. We are grateful to the patients whose participation was vital to this study. We thank our research staff for their careful handling of and analysis of data. This study was conducted without any external funding.
Funding
This research did not receive any specific funding from public, commercial, or nonprofit organizations.
Disclosure
The authors report no competing interest in this work.
References
1. Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 2000;342(23):1693–1700. doi:10.1056/nejm200006083422302
2. Moneta GL, Edwards JM, Chitwood RW, et al. Correlation of North American Symptomatic Carotid Endarterectomy Trial (NASCET) angiographic definition of 70% to 99% internal carotid artery stenosis with duplex scanning. Journal of Vascular Surgery. 1993;17(1):152–159. doi:10.1016/0741-5214(93)90019-I
3. Rothwell PM, Eliasziw M, Gutnikov S, et al. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. The Lancet. 2003;361(9352):107–116. doi:10.1016/S0140-6736(03)12228-3
4. Yadav JS, Wholey MH, Kuntz RE, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. New England Journal of Medicine. 2004;351(15):1493–1501. doi:10.1056/NEJMoa040127
5. Brown MM, Rogers J, Bland JM, et al. Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001;357(9270):1729–1737. doi:10.1016/S0140-6736(00)04893-5
6. Eckstein -H-H, Ringleb P, Allenberg J-R, et al. Results of the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study to treat symptomatic stenoses at 2 years: a multinational, prospective, randomised trial. The Lancet Neurology. 2008;7(10):893–902. doi:10.1016/S1474-4422(08)70196-0
7. Brott TG, Hobson RW, Howard G, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. New England Journal of Medicine. 2010;363(1):11–23. doi:10.1056/NEJMoa0912321
8. Fisher C. Headache in cerebrovascular disease. Handbook of Clinical Neurology. 1968:124–156.
9. Edmeads J, Barnett H. La cefales en les afecciones cerebrovasculares oclusivas. Cefaleas y Jaquecas Eudeba Editorial Universitaria de Buenos Aires. Spanish. 1973.
10. Gündüz A, Göksan B, Koçer N, Karaali-Savrun F. Headache in carotid artery stenting and angiography. Headache: The Journal of Head and Face Pain. 2012;52(4):544–549. doi:10.1111/j.1526-4610.2012.02096.x
11. Gil-Gouveia R, Fernandes Sousa R, Lopes L, Campos J, Pavão Martins I. Headaches during angiography and endovascular procedures. Journal of Neurology. 2007;254(5):591–596. doi:10.1007/s00415-006-0330-9
12. Suller Marti A, Bellosta Diago E, Velázquez Benito A, Tejero Juste C, Santos Lasaosa S. Headache after carotid artery stenting. Neurología. 2019;34(7):445–450. doi:10.1016/j.nrleng.2017.02.010
13. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. doi:10.1177/0333102417738202
14. Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes. Stroke. 1999;30(12):2513–2516. doi:10.1161/01.STR.30.12.2513
15. Touzé E, Trinquart L, Chatellier G, et al. A comparative analysis and results of carotid interventions regarding endovascular stenting and open endarterectomy: a real-life study. Italian Journal of Vascular and Endovascular Surgery. 2023;30(4):135–141. doi:10.23736/S1824-4777.23.01615-7
16. Edmeads J. Complicated migraine and headache on cerebrovascular disease. Neurologic Clinics. 1983;1(2):385–397. doi:10.1016/S0733-8619(18)31152-6
17. van Mook WNKA, Rennenberg RJMW, Schurink GW, et al. Cerebral hyperperfusion syndrome. The Lancet Neurology. 2005;4(12):877–888. doi:10.1016/S1474-4422(05)70251-9
18. Ogasawara K, Sakai N, Kuroiwa T, et al. Intracranial hemorrhage associated with cerebral hyperperfusion syndrome following carotid endarterectomy and carotid artery stenting: retrospective review of 4494 patients. Journal of Neurosurgery. 2007;107(6):1130–1136. doi:10.3171/JNS-07/12/1130
19. Abou-Chebl A, Yadav JS, Reginelli JP, Bajzer C, Bhatt D, Krieger DW. Intracranial hemorrhage and hyperperfusion syndrome following carotid artery stenting: risk factors, prevention, and treatment. Journal of the American College of Cardiology. 2004;43(9):1596–1601. doi:10.1016/j.jacc.2003.12.039
20. Naylor A, Whyman M, Wildsmith J, et al. Factors influencing the hyperaemic response after carotid endarterectomy. Journal of British Surgery. 1993;80(12):1523–1527. doi:10.1002/bjs.1800801209
21. Jorgensen LG, Schroeder TV. Defective cerebrovascular autoregulation after carotid endarterectomy. European Journal of Vascular Surgery. 1993;7(4):370–379. doi:10.1016/S0950-821X(05)80252-X
22. Rippy EE, Wolfe JHN. Cerebral hyperperfusion syndrome: a case report and literature review. Vascular and Endovascular Surgery. 2002;36(4):291–295. doi:10.1177/153857440203600407
23. Naylor AR, Ruckley CV. The post-carotid endarterectomy hyperperfusion syndrome. Eur J Vasc Endovasc Surg. 1995;9(4):365–367. doi:10.1016/s1078-5884(05)80001-2
24. Wagner WH, Cossman DV, Farber A, Levin PM, Cohen JL. Hyperperfusion syndrome after carotid endarterectomy. Annals of Vascular Surgery. 2005;19(4):479–486. doi:10.1007/s10016-005-4644-3
25. Stingele R, Berger J, Alfke K, et al. Clinical and angiographic risk factors for stroke and death within 30 days after carotid endarterectomy and stent-protected angioplasty: a subanalysis of the SPACE study. The Lancet Neurology. 2008;7(3):216–222. doi:10.1016/S1474-4422(08)70024-3
26. Tehindrazanarivelo AD, Lutz G, Petitjean C, Bousser M-G. Headache following carotid endarterectomy: a prospective study. Cephalalgia. 1992;12(6):380–382. doi:10.1111/j.1468-2982.1992.00380.x
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.