Back to Journals » Neuropsychiatric Disease and Treatment » Volume 21
Impact of Emotional Blunting on Patient Social Function and Depressive Symptoms: A Post Hoc Analysis of a Web-Based Survey in Japanese Patients with Major Depressive Disorder
Authors Kikuchi T, Iga JI , Hattori A , Tokuda F, Moriguchi Y , Hoshino T
Received 5 September 2024
Accepted for publication 8 March 2025
Published 12 April 2025 Volume 2025:21 Pages 841—854
DOI https://doi.org/10.2147/NDT.S485109
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Taro Kishi
Toshiaki Kikuchi,1 Jun-ichi Iga,2 Atsushi Hattori,3 Fumie Tokuda,3 Yoshiya Moriguchi,4 Tatsuya Hoshino3
1Department of Neuropsychiatry, Keio University School of Medicine, Tokyo, Japan; 2Department of Neuropsychiatry, Ehime University Graduate School of Medicine, Ehime, Japan; 3Japan Medical Office, Takeda Pharmaceutical Company Ltd, Tokyo, Japan; 4Medical Affairs, Lundbeck Japan K.K., Tokyo, Japan
Correspondence: Tatsuya Hoshino, Japan Medical Office, Takeda Pharmaceutical Company Ltd, 1– 1, Nihonbashi-Honcho 2-Chome, Chuo-ku Tokyo, 103-8668, Japan, Tel +81-3-3278-2111, Email [email protected]
Background: Emotional blunting (EB), defined as a flattening of emotions and emotional indifference, is reported by many patients with major depressive disorder (MDD) taking antidepressants. Severity of EB correlates with depressive symptoms, as well as deficits in social function, anxiety and health-related quality of life. However, awareness and understanding of EB and its impact on treatment of MDD remain poorly understood.
Methods: This was a post hoc analysis of data from a web-based survey of 3376 adults with MDD in Japan. The primary endpoint was the correlation between total and subdomain scores of the Oxford Depression Questionnaire (ODQ; a validated instrument to assess EB) and total and individual domain/item scores of the Work and Social Adjustment Scale (WSAS) and Patient Health Questionnaire 9-item (PHQ-9). The secondary endpoint explored which patients had a discrepancy between EB symptoms (assessed by the ODQ) and their own evaluation of EB (using a validated screening question).
Results: There was a moderate correlation between the ODQ total score and the WSAS total score (Spearman’s rank correlation coefficient [rs] = 0.578) and a strong correlation between the ODQ total score and PHQ-9 total score (rs = 0.670). Multiple regression analyses showed that the ODQ subdomains “not caring” (NC) and “reduction in positive emotions” (PR) had the greatest impact on both the WSAS total score (partial regression coefficients = 1.034 and 0.501, respectively) and PHQ-9 total score (partial regression coefficients = 0.548 and 0.592, respectively). A higher proportion of men (versus women) and unemployed individuals (versus employed individuals) underestimated their EB severity compared with their ODQ score.
Conclusion: The ODQ subdomains of NC and PR are important factors when evaluating the impact of EB on social function and severity of depressive symptoms in patients with MDD. Physicians should assess EB symptoms for each patient, considering the patient’s background.
Keywords: health-related quality of life, natural language analysis, online survey, Oxford Depression Questionnaire, patient health questionnaire 9-item, work and social adjustment scale
Introduction
Major depressive disorder (MDD) is a common but serious mental illness with a substantial global health burden. In 2019, an estimated 280 million people worldwide were affected by depressive disorders (defined as MDD and dysthymia).1,2 MDD affects multiple aspects of health-related quality of life (HRQoL), including physical, cognitive, and emotional health, and can cause significant problems in work, school, family, and social life.3–7 Importantly, even if depressive symptoms are improved with treatment, patients with residual symptoms (such as decreased motivation, cognitive impairment, sleeping disorder, or anxiety) are more likely to experience disease recurrence or relapse.8–10 Therefore, in addition to improving psychological symptoms, treatment considerations for MDD should include addressing any residual symptoms, as well as improving patient function and social reintegration.11,12
In recent years, emotional blunting (EB) has been proposed as one of the symptoms experienced by patients with MDD. EB is defined as the “numbing” or “flattening” of emotions, as well as emotional indifference or reduced emotional responsiveness (such as not caring, being emotionally detached, or having a reduction in positive emotions or emotions generally).13 EB describes a state in which both positive and negative emotions are toned down and there is an inability to experience expected emotional responses.14 EB has significant effects on the treatment of MDD; it is associated with reduced HRQoL and daily function,15,16 decreased quality of remission,14 and the discontinuation of antidepressant treatment.17
The reported prevalence of EB in patients taking antidepressants ranges from 46% to 71%.14,18,19 We recently published results from a survey conducted in Japan, which found that 67.1% of patients with MDD taking antidepressant medication reported symptoms of EB, and that there was a correlation between the severity of EB (as assessed by the Oxford Depression Questionnaire [ODQ]) and depressive symptoms, social function, anxiety, and HRQoL.20 These results highlighted the need to increase awareness of EB symptoms and to address EB in the treatment of MDD. However, EB in MDD treatment remains poorly understood.
The ODQ is a validated instrument for assessing EB in patients with MDD, including those treated with antidepressants.13,21 Questions cover five subdomains of EB;14 however, it is not clear how each subdomain relates to a patient’s social function and depressive symptoms. Although EB is a symptom observed in many patients with MDD, it is thought that it is difficult for physicians to notice EB symptoms and appropriately evaluate them during clinical practice. In fact, it has been reported that one-third of patients with EB do not tell their physicians about these symptoms,20 and that there is a gap in the evaluation of EB between patients and physicians.16 A better understanding of the background and characteristics of patients with EB is needed to help physicians identify the presence and severity of EB symptoms.
Here, we present a post hoc analysis of our previous survey of Japanese patients with MDD. We investigated which EB subdomains are associated with reduced social function and depressive symptoms, and which patients had a discrepancy between their EB symptoms (as assessed by the ODQ) and their overall evaluation of EB severity. We also explored the relationships between verbal expressions used by patients to describe their EB symptoms, patient awareness of EB, severity of EB, patient social function, and symptoms of depression.
Methods
Study Design
This was a post hoc analysis of data from a web-based survey (UMIN Clinical Trials Registry ID: UMIN000048497) that has been described previously.20 The survey was conducted between July 29, 2022 and August 9, 2022 via a monitored patient panel offered by Macromill Carenet, Inc. (www.macromillcarenet.jp). Potential participants were identified from the patient panel and invited to participate. Respondents were provided with information about the study before being screened for eligibility. Participants were informed that they could refuse to answer any question and could withdraw at any point. Data were collected using a self-completed online survey comprising a validated screening question,13,15 followed by validated Japanese translations of multiple questionnaires. These included the ODQ, which assesses EB,13,21 the Work and Social Adjustment Scale (WSAS),22 which measures social functional impairment, and the Patient Health Questionnaire 9-item (PHQ-9),23,24 which evaluates depression. For their participation, respondents received points from Macromill that could be redeemed for a variety of commercial services.25 Both the online survey20 and this post hoc analysis were conducted in accordance with the Declaration of Helsinki and were approved by the Research Institute of Healthcare Data Science Institutional Review Board (Tokyo, Japan).
Participants
Adults aged 18–59 years were eligible for participation in the survey if they had been diagnosed with MDD (self-reported by the participant); had been taking antidepressant medication for at least 3 months; had been visiting a hospital for more than 3 months; could use the internet with a personal computer, smartphone, or tablet; and could give informed consent after reading and understanding the study information provided in Japanese. Individuals who had been diagnosed with bipolar disorder or were not taking antidepressants were excluded from participation.
Assessments
The primary endpoint of this post hoc analysis was the correlation between ODQ scores (total score and each subdomain score) and the total and individual domain/item scores of the WSAS and PHQ-9. The ODQ comprises 26 questions about emotional experiences during the past week, and respondents are asked the extent to which they agree or disagree.13,21 Questions cover five subdomains of EB (general reduction in emotions [GR]; reduction in positive emotions [PR]; emotional detachment from others [ED]; not caring [NC]; antidepressant-as-cause [AC]). Responses for each question are scored on a 5-point scale ranging from 1 (disagree) to 5 (agree). The ODQ total score indicates the severity of EB and ranges from 26 to 130 points, with higher scores indicating more severe EB; scores for each subdomain provide information on EB symptom characteristics.13,21 The Japanese translated version is available online,26 and has been cross-culture validated in Japan.27 The WSAS is a self-reported scale of functional impairment that is associated with an identified problem.22 The five WSAS questions are rated on a scale from 0 (not at all) to 8 (very severely) and the total score ranges from 0 to 40. The PHQ-9 is a 9-item questionnaire designed to screen for the presence and severity of depression. PHQ-9 items are scored by the patient and range from 0 (not at all) to 3 (nearly every day). The PHQ-9 total score is a continuous outcome, ranging from 0 (absence of depression) to 27 (severe depression).23,24
The secondary endpoint of this post hoc analysis was the relationship between patient background characteristics and the presence of a gap between the patient’s overall assessment of their EB severity and their ODQ score. The overall presence and severity of patients’ EB symptoms were assessed using the following validated screening question:13,15 “To what extent have you had any of the following emotional experiences in the past 6 weeks?” This was qualified by the following explanation: “Feeling emotionally ‘numbed’ or ‘blunted’ in some way; lacking positive emotions or negative emotions; feeling detached from the world around you; or ‘just not caring’ about things that you used to care about.”
The respondent was required to select one option from the EB assessment scale (never, almost none, mildly, moderately, or severely) to determine the severity of their EB symptoms. Patients who responded “mildly”, “moderately”, or “severely” to this question were considered to have EB.
Exploratory endpoints included the relationship between the expressions used by patients to describe EB and scores on the EB assessment scale, ODQ, WSAS, and PHQ-9. Participants were asked the following open-ended questions about how they expressed concerns about EB when consulting with a clinician and what daily problems they experienced due to EB. Q1: “How did you describe your EB symptoms to your physician?” and Q2: “In what aspects of your daily life do you have trouble with feeling EB symptoms?” Natural language analysis was used to identify trends in the content of the responses.
Statistical Analysis
The population for this analysis comprised all patients who met the inclusion criteria and completed the online survey. Data were presented descriptively using mean and standard deviation (SD) for continuous variables, and frequency and/or percentage for categorical variables.
For analysis of the primary endpoint, we calculated correlation coefficients between questionnaire scores and examined the influence of ODQ subdomains on WSAS and PHQ-9 total scores using multiple regression analysis. Because the questions included in the WSAS and PHQ-9 are also considered to represent factors that make up social function and depressive symptoms, respectively, we also analyzed these sub-scores in the same way. Spearman’s rank correlation coefficients (rs) and p values were calculated for the ODQ total score and subdomains (GR, PR, ED, NC, and AC), as well as the total score and domain/item scores of the WSAS (5 domains) and PHQ-9 (9 items). For the multiple regression analysis, the subdomains of the ODQ were explanatory variables and the total score and domains/items of WSAS and PHQ were dependent variables. In this case, we corrected for multiple testing using the Bonferroni method. For the assessment of categorical variables, we conducted a chi-square test.
For analysis of the secondary endpoint, we calculated the mean (± SD) ODQ total score for the patients in each EB assessment scale category. Patients were then divided into three groups. The EB accurate group included patients with a ODQ total score within the mean ± SD ODQ total score for their EB assessment scale category. The EB overestimation group included patients with a ODQ total score below the mean – SD ODQ total score for their EB assessment scale category. The EB underestimation group included patients with a ODQ total score higher than the mean + SD ODQ total score for their EB assessment scale category. We then compared the background characteristics of patients in these three groups using the following variables: sex, household income, personal income, age, family status, whether they lived with a spouse, employment status, and highest educational attainment.
For analysis of the exploratory endpoint, we conducted topic clustering on the responses obtained from each question using BERTopic. We used Uniform Manifold Approximation and Projection for dimension reduction and K-means for clustering, with a cluster number of 20, and examined the relationship between the distribution of topics obtained by clustering and the distribution of the EB assessment scale, ODQ, WSAS, and PHQ-9 scores. For the purpose of this analysis, we divided ODQ and WSAS scores into three equal groups (ODQ: 26–81, 82–94, and 95–130; WSAS: 0–9, 10–18, and 19–40) and compared the distribution of topics between these groups. For the EB assessment scale and PHQ-9, we compared the distribution of topics by severity scores (EB assessment scale: mildly, moderately, severely; PHQ-9: 0–4, 5–9, 10–14, 15–19, and 20–27). We used Python 3.10 for natural language analysis and R version 4.1.2 (R Core Team and R Foundation for Statistical Computing, Vienna, Austria) for other analyses.
Results
Patient Characteristics
Data for this post hoc analysis were available for 3376 patients who completed our previously reported survey on EB in Japan.20 Patient characteristics have been described previously,20 and are shown in Table 1.
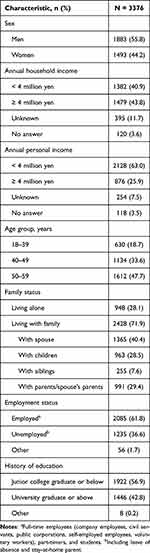 |
Table 1 Patient Characteristics |
Relationship Between ODQ Scores and WSAS and PHQ-9 Scores
Summary statistics for ODQ, WSAS, and PHQ-9 scores are shown in Supplementary Table 1. There were moderate correlations between the ODQ total score and the WSAS total score (rs = 0.578), as well as the ODQ total score and individual WSAS domain scores (domain 1: rs = 0.466; domain 2: rs = 0.491; domain 3: rs = 0.514; domain 4: rs = 0.507; domain 5: rs = 0.545) (Table 2). There were strong correlations between the ODQ PR and NC subdomain scores and the WSAS total score (rs = 0.606 and 0.639, respectively), and a weak correlation between the ODQ AC subdomain score and the WSAS total score (rs = 0.277). The ODQ PR and NC subdomain scores also showed moderate correlations with all domains of the WSAS (Table 2). In the multiple regression analysis, the ODQ NC subdomain score had the greatest impact on the WSAS total score (partial regression coefficient: 1.034), followed by the PR score (partial regression coefficient: 0.501) (Table 3). Similar trends were also observed when the objective variable was replaced by each of the domains of the WSAS (data not shown).
 |
Table 2 Correlation Between ODQ Score and WSAS Score (Spearman’s Rank Correlation Coefficient) |
 |
Table 3 Correlation Between ODQ Score and WSAS Score (Multiple Regression Analysis) |
There were strong correlations between the ODQ total score and the PHQ-9 total score (rs = 0.670) and moderate or strong correlations between all ODQ subdomain scores, except AC, and the PHQ-9 total score (Table 4). Moderate or strong correlations were also found between the ODQ total score and all PHQ-9 items, except for item 3 (Trouble falling or staying asleep, or sleeping too much), which showed a weak correlation (Table 4). Multiple regression analysis showed that the ODQ PR subdomain score had the greatest impact on the PHQ-9 total score (partial regression coefficient: 0.592), followed by the NC subdomain score (partial regression coefficient: 0.548) (Table 5). A similar trend was seen when the objective variable was replaced by each of the PHQ-9 items (data not shown).
 |
Table 4 Correlation Between ODQ Score and PHQ-9 Score (Spearman’s Rank Correlation Coefficient) |
 |
Table 5 Correlation Between ODQ Score and PHQ-9 Score (Multiple Regression Analysis) |
Patient Background Characteristics and EB Assessment Discrepancies
EB assessment scale results and ODQ total scores are shown in Supplementary Table 2. Table 6 shows the background characteristics of the EB accurate group, EB overestimation group, and EB underestimation group. There were significant distribution differences between the three groups for sex (p < 0.001) and employment status (p = 0.014). The EB underestimation group had proportionally more men and unemployed respondents (63.3% men; 43.4% unemployed) than either the EB accurate group (55.0% men; 35.7% unemployed) or the EB overestimation group (52.2% men; 34.2% unemployed). In the EB underestimation group, 45.1% of patients had a household income of less than 4 million yen, a higher proportion than in either the EB accurate (40.8%) or EB overestimation (37.8%) groups. For the EB overestimation group, a higher percentage of patients lived with their spouse (44.7%) than in either the EB accurate (39.9%) or the EB underestimation (37.9%) groups. However, there was no significant difference in the inter-group distribution when considering household income (p = 0.169) or whether the patient lived with a spouse (p = 0.057).
 |
Table 6 Patient Background Characteristics and Discrepancy Between EB Assessment Scalea and ODQ Total Score Assessment of EB |
Relationship Between Expressions Used by Patients in Communicating About EB Symptoms and EB Assessment Scale, ODQ, WSAS, and PHQ-9 Scores
We obtained 1468 free descriptions for Q1 (“How did you describe your EB symptoms to your physician?”) and 2128 free descriptions for Q2 (“In what aspects of your daily life do you have trouble with feeling EB symptoms?”). For both questions, the free descriptions were clustered into different topics using natural language analysis.
Figure 1 shows the distribution of a) EB assessment scale category, b) ODQ total score, c) WSAS total score, and d) PHQ-9 total score associated with the top 10 topics for Q1. There was a tendency for patients who selected “severely” on the EB assessment scale to mention “suicidal thoughts” (topic 10). Patients with intermediate (82–94) or high (95–130) ODQ total scores were more likely to use expressions related to “decreased motivation” (topic 2) and “loss of fun” (topic 3) than patients with low (26–81) ODQ total scores. The topics “loss of fun” (topic 3), “sense of isolation” (topic 4), and “suicidal thoughts” (topic 10) were also frequently mentioned by patients with intermediate (10–18) or high (19–40) WSAS total scores. Patients with severe depressive symptoms (as shown by PHQ-9 total score) were the most likely to mention “suicidal thoughts” (topic 10).
Figure 2 shows the distribution of a) EB assessment scale category, b) ODQ total score, c) WSAS total score, and d) PHQ-9 total score associated with the top 10 topics for Q2. Patients with high ODQ total scores were the most likely to use expressions related to “lethargy” (topic 1). The topics “loss of fun” (topic 3) and “household chores” (topic 10) were frequently mentioned by patients with high WSAS total scores. There were no notable patterns observed for Q2 topics and EB assessment scale categories or PHQ-9 total scores.
Discussion
In this post hoc analysis of our survey of Japanese patients with MDD, we found that patients with symptoms of not caring or having a reduction in positive emotions (as assessed by the ODQ) had reduced social function, and that a patient’s social environment may influence their awareness of EB symptoms. We also identified patterns in the expressions used by patients to describe EB that may be related to their EB symptoms, social function, and severity of depression.
We found that the NC subdomain of the ODQ had the greatest impact on the WSAS total score, followed by the PR subdomain. While previous studies have shown moderate to strong correlations between ODQ and social function scores,16,20,27,28 there has been limited reporting on the relationships between the subdomains of EB and social functioning.16 To our knowledge, this is the first study to describe in detail the relationship between the ODQ subdomains and WSAS domains. Our results are consistent with a study that showed positive correlations between all ODQ subdomains and the Functioning Assessment Short Test (FAST) total score, with the strongest correlations observed for the NC and PR subdomains.16 Moreover, the ODQ total score was moderately correlated with all WSAS domains, which is consistent with a previous study showing that the ODQ total score was correlated with all domains of the Sheehan Disability Scale (SDS).27,28 It is important to note that these previous studies included different social functioning scales and patient populations. Overall, considering the differing impact individual EB subdomains have on social function, our results suggest that it is important for physicians to focus not only on whether EB is present, but also which specific symptoms the patient is experiencing. In particular, it is important to consider the NC and PR subdomains from the perspective of declining social function.
For the PHQ-9, a subjective evaluation of depression severity, some items related to psychological symptoms (such as a loss of interest, feelings of depression, and low self-worth) showed moderate to strong correlations with the ODQ total score, whereas other items related to physical symptoms (such as challenges with sleep or appetite and low energy) showed weak to moderate correlations with the ODQ total score. These results suggest that the emotional symptoms assessed by the ODQ, in particular the PR and NC subdomains, are similar to the psychological symptoms of depression assessed by the PHQ-9. Conversely, a previous study examining the relationship between the Montgomery-Åsberg Depression Rating Scale (MADRS; an objective evaluation of depression severity) and the ODQ total score suggested that not only “concentration” and “inability to feel”, but also “reduced sleep” are predictors of ODQ total score.27 The reason for this discrepancy in results is unclear; however, it could potentially be attributed to the methodological difference between the patient-assessed PHQ-9 and the clinician-assessed MADRS. We found that the PR and NC subdomains of the ODQ had the greatest impact on the PHQ-9 total score. These findings are consistent with other studies that examined the relationship between the ODQ subdomains and the Beck Depression Inventory (BDI) score (an objective evaluation of depression severity). Specifically, in one study the NC and PR subdomains were correlated with dimensions of the BDI dominated by so-called “cognitive items” such as “past failure”, “worthlessness”, “pessimism”, and “self-dislike”, rather than “somatic items” such as “changes in appetite”, “changes in sleep pattern”, and “tiredness or fatigue”.13 Moreover, in a Chinese study, the BDI total score showed a stronger correlation with the PR and NC subdomains than the GR, AC, or ED subdomains.29 Overall, these consistent findings suggest that across a range of depression scales (including the PHQ-9, MADRS, and BDI), and for different populations, patients with MDD who report symptoms of PR and NC may also be experiencing more severe depressive symptoms, particularly psychological symptoms. Similarly, patients with MDD reporting severe depressive symptoms may also be experiencing EB symptoms such as PR and NC.
Our analysis found that there was a higher proportion of male and unemployed individuals in the EB underestimation group than in the EB accurate group and the EB overestimation group. In the EB overestimation group, a higher proportion of patients lived with a spouse than in the EB accurate group and the EB underestimation group. These results suggest that differences in the patients’ social environment may influence their awareness of EB symptoms. A common theme identified in the characteristics of the patients may be the opportunity for communication. A 2017 survey in Japan showed that middle-aged and elderly men tended to report less supportive friendships, and that individuals who are unemployed or do not live with a spouse may have fewer communication opportunities through either work or family life.30,31 Therefore, patients with these background characteristics may be less aware of their own emotional fluctuations or of any changes in how they are interacting with others in their surroundings, which are both characteristics of EB. While it has been reported that younger patients are more likely to experience feelings of EB,19,32 our analysis found no age-related differences in the EB overestimation, accurate, or underestimation groups. Overall, our findings indicate that a patient’s background characteristics may be important to consider when identifying the presence of EB.
The natural language analysis suggested that topics related to decreased motivation, loss of fun, sense of isolation, suicidal thoughts, and lethargy may be related to a patient’s EB symptoms, social function, and severity of depressive symptoms. Regarding topics relating to suicidal thoughts, Goldsmith et al reported an increase in suicidal thoughts among patients with EB,33 and Price et al reported that EB may also be linked to suicidal ideation through reducing normal inhibitions.15 Although these reports are not based on natural language analysis, they align with our finding of the tendency for patients who selected “severely” on the EB assessment scale to mention “suicidal thoughts”. However, it is important to note that the results in our study were based on answers to specific questions regarding EB and therefore cannot be generalized. As the verbal expressions used by a patient may reflect their EB symptoms, social function, and depressive symptoms, physicians should carefully monitor any statements made by the patient regarding EB symptoms over the course of treatment.
One limitation of this study was that results were based on responses from patients with a self-reported diagnosis of MDD; diagnoses of MDD or EB were not confirmed by a physician. Therefore, responses may have included patients without MDD. Another limitation is the lack of detailed analysis of MDD treatments, including antidepressant use and dose, and other potential confounders such as medical disorders, medical treatments, and personality disorders, which could have affected EB symptoms. An additional limitation is that the answers used for the linguistic analysis were based on the patient’s recollection of what was said and do not necessarily reflect exactly what was explained to their physician. Moreover, as this is a cross-sectional analysis of survey data, it is not possible to determine causal relationships due to the reciprocal and interrelated nature of the ODQ, PHQ-9, and WSAS. Future work could utilize a mediation analysis to investigate the causal relationships of these three domains. Furthermore, while the ODQ was developed specifically for assessing EB related to antidepressant treatment, our study cannot distinguish between EB caused by antidepressants and EB caused by depression itself.
Conclusion
When treating patients with MDD, physicians should focus on the EB subdomains of NC and PR from the perspective of declining social function. Furthermore, given that the awareness of EB differs between patients, physicians should check for EB symptoms on an individual basis and consider the patient’s background. Finally, because the verbal expressions used by patients may reflect symptoms of EB, social function, and severity of depression, physicians should carefully monitor patients’ statements regarding EB during treatment.
Data Sharing Statement
Takeda does not plan to share data supporting the results reported in this article because the study is part of a co-development program agreement which prevents Takeda from data sharing. The raw data cannot be shared for reasons of personal data protection, as informed consent was only obtained for the analysis and external publication of survey results, not for providing raw data to parties other than the study sponsor.
Acknowledgments
The authors would like to thank all study participants and contributors inside Takeda for their cooperation in conducting the study and preparing the manuscript. The authors also wish to thank Hiromi Mizutani (Medical Affairs, Lundbeck Japan K.K.) for her contribution to planning, analysis of results, and advice regarding this study. Medical writing support was provided by Ruby Oberin PhD and Sarah Graham PhD of Oxford PharmaGenesis, Melbourne, Australia and funded by Takeda Pharmaceutical Company Limited and Lundbeck Japan K.K. in accordance with Good Publication Practice (GPP 2022) guidelines (www.ismpp.org/gpp-2022).
Funding
This study was funded by Takeda Pharmaceutical Company Limited and Lundbeck Japan K.K.
Disclosure
TK has received consultant fees and speaker’s honoraria from Lundbeck Japan K.K and Takeda Pharmaceutical Co., Ltd., and speaker’s honoraria from Mochida Pharmaceutical Co., Ltd., MSD K.K., Otsuka Pharmaceutical Co., Ltd., Sumitomo Pharma, and Viatris Inc. JI has received grant funding from the Japan Society for the Promotion of Science and speaker’s honoraria from Daiichi Sankyo, Eisai, Eli Lilly, Janssen Pharmaceuticals, Kowa Company, Kyowa Pharmaceutical Industry, Lundbeck Japan, Meiji Seika Pharma, Mochida Pharmaceutical, Mylan, MSD K.K., Nobelpharma, Novartis Pharma K.K., Nippon Boehringer Ingelheim, Ono Pharmaceutical, Otsuka, Sanofi K.K., Sawai Pharmaceutical, Shionogi, Sumitomo Dainippon Pharma, Takeda Pharmaceutical, Viatris, Yonyaku, and Yoshitomi Yakuhin. AH, FT, and TH are employees of Takeda Pharmaceutical Company Limited. YM is an employee of Lundbeck Japan K.K. The authors report no other conflicts of interest in this work.
References
1. World Health Organization. Depressive disorder (depression). Available from: https://www.who.int/news-room/fact-sheets/detail/depression.
2. D GB. Mental disorders collaborators. global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. 2022;9(2):137–150.
3. Evans-Lacko S, Knapp M. Global patterns of workplace productivity for people with depression: absenteeism and presenteeism costs across eight diverse countries. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1525–1537.
4. Marazziti D, Consoli G, Picchetti M, Carlini M, Faravelli L. Cognitive impairment in major depression. Eur J Pharmacol. 2010;626(1):83–86. doi:10.1016/j.ejphar.2009.08.046
5. Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. 2016;69:313–332. doi:10.1016/j.neubiorev.2016.07.002
6. IsHak WW, Mirocha J, James D, et al. Quality of life in major depressive disorder before/after multiple steps of treatment and one-year follow-up. Acta Psychiatr Scand. 2015;131(1):51–60. doi:10.1111/acps.12301
7. Hammar A, Ardal G. Cognitive functioning in major depression--a summary. Front Hum Neurosci. 2009;3:26. doi:10.3389/neuro.09.026.2009
8. Nierenberg AA, Husain MM, Trivedi MH, et al. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR*D report. Psychol Med. 2010;40(1):41–50. doi:10.1017/S0033291709006011
9. Saragoussi D, Touya M, Haro JM, et al. Factors associated with failure to achieve remission and with relapse after remission in patients with major depressive disorder in the PERFORM study. Neuropsychiatr Dis Treat. 2017;13:2151–2165. doi:10.2147/NDT.S136343
10. Verhoeven FEA, Wardenaar KJ, Ruhe HGE, Conradi HJ, de Jonge P. Seeing the signs: using the course of residual depressive symptomatology to predict patterns of relapse and recurrence of major depressive disorder. Depress Anxiety. 2018;35(2):148–159. doi:10.1002/da.22695
11. Oluboka OJ, Katzman MA, Habert J, et al. Functional recovery in major depressive disorder: providing early optimal treatment for the individual patient. Int J Neuropsychopharmacol. 2018;21(2):128–144. doi:10.1093/ijnp/pyx081
12. Lam RW, McIntosh D, Wang J, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 1. disease burden and principles of care. Can J Psychiatry. 2016;61(9):510–523. doi:10.1177/0706743716659416
13. Price J, Cole V, Doll H, Goodwin GM. The Oxford questionnaire on the emotional side-effects of antidepressants (OQuESA): development, validity, reliability and sensitivity to change. J Affect Disord. 2012;140(1):66–74. doi:10.1016/j.jad.2012.01.030
14. Goodwin GM, Price J, De Bodinat C, Laredo J. Emotional blunting with antidepressant treatments: a survey among depressed patients. J Affect Disord. 2017;221:31–35. doi:10.1016/j.jad.2017.05.048
15. Price J, Cole V, Goodwin GM. Emotional side-effects of selective serotonin reuptake inhibitors: qualitative study. Br J Psychiatry. 2009;195(3):211–217. doi:10.1192/bjp.bp.108.051110
16. Christensen MC, Ren H, Fagiolini A. Emotional blunting in patients with depression. Part II: relationship with functioning, well-being, and quality of life. Ann Gen Psychiatry. 2022;21(1):20. doi:10.1186/s12991-022-00392-4
17. Rosenblat JD, Simon GE, Sachs GS, et al. Treatment effectiveness and tolerability outcomes that are most important to individuals with bipolar and unipolar depression. J Affect Disord. 2019;243:116–120. doi:10.1016/j.jad.2018.09.027
18. Read J, Williams J. Adverse effects of antidepressants reported by a large international cohort: emotional blunting, suicidality, and withdrawal effects. Curr Drug Saf. 2018;13(3):176–186. doi:10.2174/1574886313666180605095130
19. Read J, Cartwright C, Gibson K. Adverse emotional and interpersonal effects reported by 1829 New Zealanders while taking antidepressants. Psychiatry Res. 2014;216(1):67–73. doi:10.1016/j.psychres.2014.01.042
20. Kikuchi T, Iga JI, Oosawa M, Hoshino T, Moriguchi Y, Izutsu M. A web-based survey on the occurrence of emotional blunting in patients with major depressive disorder in Japan: patient perceptions and attitudes. Neuropsychopharmacol Rep. 2024;44(2):321–332. doi:10.1002/npr2.12417
21. Christensen MC, Fagiolini A, Florea I, Loft H, Cuomo A, Goodwin GM. Validation of the Oxford depression questionnaire: sensitivity to change, minimal clinically important difference, and response threshold for the assessment of emotional blunting. J Affect Disord. 2021;294:924–931. doi:10.1016/j.jad.2021.07.099
22. Mundt JC, Marks IM, Shear MK, Greist JM. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180(5):461–464. doi:10.1192/bjp.180.5.461
23. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
24. Muramatsu K, Miyaoka H, Kamijima K, et al. Performance of the Japanese version of the patient health questionnaire-9 (J-PHQ-9) for depression in primary care. Gen Hosp Psychiatry. 2018;52:64–69. doi:10.1016/j.genhosppsych.2018.03.007
25. Macromill Inc. Corporate profile. Macromill, Inc. Available from: https://www.macromill.com/company/profile.html.
26. Oxford University Innovation Limited. Oxford depression symptoms questionnaire. Japanese for Japan; 2011. Available from: https://innovation.ox.ac.uk/wp-content/uploads/2014/09/Final_ODQ_Japanese_Japan_SAMPLE.pdf.
27. Kato M, Kikuchi T, Watanabe K, et al. Assessing reliability and validity of the Oxford depression questionnaire (ODQ) in a Japanese clinical population. Neuropsychiatr Dis Treat. 2023;19:2401–2412. doi:10.2147/NDT.S428443
28. Fagiolini A, Florea I, Loft H, Christensen MC. Effectiveness of vortioxetine on emotional blunting in patients with major depressive disorder with inadequate response to SSRI/SNRI treatment. J Affect Disord. 2021;283:472–479. doi:10.1016/j.jad.2020.11.106
29. Chen J, Chen W, Zhang H, et al. Reliability and validity of the Chinese version of the Oxford Depression Questionnaire (ODQ-Chinese). J Affect Disord. 2022;313:278–282. doi:10.1016/j.jad.2022.06.044
30. Murata H. Middle-aged and elderly men who have few friendships - Japanese relationships as seen from a survey ISSP international comparative survey “social networks and social resources 2017” [Results from Japan]. Broadcast Res invest. 2018;68(6):78–94.
31. Murata H. Middle-aged and elderly men have shallow friendships: looking into personal relationships of the Japanese; 2018. Available from: https://www.nhk.or.jp/bunken/english/research/yoron/20180601_7.html.
32. Hughes S, Lacasse J, Fuller RR, Spaulding-Givens J. Adverse effects and treatment satisfaction among online users of four antidepressants. Psychiatry Res. 2017;255:78–86. doi:10.1016/j.psychres.2017.05.021
33. Goldsmith L, Moncrieff J. The psychoactive effects of antidepressants and their association with suicidality. Curr Drug Saf. 2011;6(2):115–121. doi:10.2174/157488611795684622
 © 2025 The Takeda Pharmaceutical Company Limited. This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Takeda Pharmaceutical Company Limited. This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



