Back to Journals » Nature and Science of Sleep » Volume 17
Impact of Gender, Age, and Obesity on Childhood Obstructive Sleep Apnea: A Cross-Sectional Study of 4,668 Children
Authors Huang G , Wang Q , Chang L, Ye S, Liu J, Lu Y, Li T, Zhan X, Liang J, Cheng Y, Gu Q
Received 5 March 2025
Accepted for publication 20 May 2025
Published 17 June 2025 Volume 2025:17 Pages 1391—1404
DOI https://doi.org/10.2147/NSS.S521415
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sarah L Appleton
Guimin Huang,1,* Qian Wang,2,3,* Li Chang,4 Siyu Ye,2 Junting Liu,1 Yingxia Lu,2 Tao Li,1 Xiaojun Zhan,2 Jieqiong Liang,2 Yijing Cheng,1 Qinglong Gu2,3
1Child Health Big Data Research Center, Capital Institute of Pediatrics, Beijing, People’s Republic of China; 2Department of Otolaryngology-Head and Neck Surgery, Capital Institute of Pediatrics, Beijing, People’s Republic of China; 3Graduate School of Peking Union Medical College, Beijing, People’s Republic of China; 4Department of Respiratory Medicine, Capital Institute of Pediatrics, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qinglong Gu, Department of Otolaryngology-Head and Neck Surgery, Children’s Hospital, Capital Institute of Pediatrics, Beijing, People’s Republic of China, Email [email protected]
Purpose: Obstructive sleep apnea (OSA) is a common condition in children, linked to significant health risks. However, the impact of gender, age, and obesity on OSA severity remains poorly understood. This study aimed to explore how these factors influence OSA in pediatric patients.
Patients and Methods: This cross-sectional study was conducted at the Sleep Center of the Children’s Hospital Affiliated with the Capital Institute of Pediatrics from January 2017 to May 2023. We included children aged 0 to 15 years diagnosed with OSA via overnight polysomnography (PSG). Demographic data, including gender, age, and body measurements, were collected. The apnea-hypopnea index (AHI) and oxygen desaturation index (ODI) were recorded. Data analysis included one-way ANOVA for continuous variables, chi-square tests for proportions, linear trend analysis for changes across age and OSA severity, and Pearson/partial correlations for associations between BMI, AHI, and other variables.
Results: The study involved 4668 children, with a mean age of 5.3 years, 62.3% of whom were boys. Boys had the highest Apnea-Hypopnea Index (AHI) (8.8 ± 7.9). The 0– 2 years age group exhibited the highest AHI (10.7 ± 9.8), while the obese group had the highest AHI (13.9 ± 19.8). Logistic regression analysis revealed that male gender (OR = 1.2, 95% CI: 1.11– 1.43), age 0– 2 years (OR = 1.49, 95% CI: 1.09– 2.04), and obesity (OR = 1.29, 95% CI: 1.09– 1.52) were significantly associated with moderate to severe OSA.
Conclusion: This study underscores the complex roles of gender, age, and obesity in pediatric OSA severity. Boys, especially those in the 0– 2 years age group, had more severe OSA than girls, and obesity exacerbated OSA severity. These findings may guide improved screening and management strategies for pediatric OSA.
Keywords: pediatric obstructive sleep apnea, age, gender, obesity, severity
Introduction
Pediatric obstructive sleep apnea (OSA) is a respiratory disorder characterized by the partial or complete blockage of airways during sleep.1 The development of OSA in children is influenced by both systemic and local factors. Systemic contributors include obesity, neuromuscular diseases, and genetic syndromes. However, local anatomical abnormalities—such as adenotonsillar hypertrophy and craniofacial deformities (eg, mandibular retrognathia, maxillary constriction, and high-arched palate)—play a pivotal role in airway obstruction. Recent studies have demonstrated that craniofacial abnormalities significantly increase the risk of pediatric OSA.2,3 The prevalence of pediatric OSA is estimated to range from 1.2% to 5.7%.4–6 Clinicians often rely on a constellation of observable signs and symptoms—including snoring, intermittent nocturnal oxygen desaturation, and disrupted sleep patterns—to identify children at risk.5 Nonetheless, the gold standard for definitive diagnosis remains overnight polysomnography, which offers comprehensive monitoring of sleep architecture and respiratory function.7
Pediatric OSA has been associated with a wide spectrum of adverse health outcomes, including behavioral problems, cognitive impairments,8 growth disturbances, and cardiovascular complications such as hypertension and endothelial dysfunction.9 Moreover, metabolic and neurodevelopmental impacts have gained attention in recent studies. For instance, the neuronal PAS domain protein 2 (NPAS2) may be linked to metabolic dysregulation in patients with OSA,10 calcium imbalance due to sleep fragmentation, and increased uric acid levels correlating with higher apnea-hypopnea index (AHI) scores have all been reported.11 Inappropriate sleep patterns have also been found to increase the number of cariogenic bacteria and reduce salivary PH and buffering capacity.12 Adenotonsillectomy remains the first-line treatment for pediatric OSA and has been shown not only to improve upper airway obstruction but also to enhance cognitive performance and quality of life in children diagnosed with OSA.13 Given the potentially severe consequences of untreated OSA, early recognition and targeted intervention are essential. A thorough understanding of OSA’s epidemiological and clinical characteristics is crucial for improving screening and management in high-risk pediatric populations.
While male sex and obesity are well-established risk factors for OSA in adults,14,15 their influence in children appears more complex and age-dependent. Previous studies have shown that boys tend to experience more severe OSA symptoms than girls,16–18 potentially due to anatomical and hormonal differences.17–20 Additionally, obesity in children is independently associated with OSA and correlates with its severity.21,22 Although younger children (particularly those aged ≤3 years) are often diagnosed with moderate to severe OSA, findings across age groups remain inconsistent, and recent data suggest a rising prevalence of OSA among preschool-aged children.23,24
Despite growing awareness of pediatric OSA, few studies have systematically explored how age, sex, and obesity interact to influence disease severity. In particular, there is a lack of large-scale, real-world data from Asian pediatric populations to thoroughly assess these relationships. This study aims to address this gap by investigating a large inpatient assessment of children with OSA, with a focus on stratified analyses based on age, sex, and BMI categories. By examining PSG-derived parameters across subgroups defined by sex, age, and BMI, this study seeks to clarify how these factors impact the clinical characteristics of pediatric OSA and to provide valuable insights for risk stratification and individualized treatment strategies.
Materials and Methods
Study Design and Participants
This retrospective cross-sectional study was conducted at the Sleep Center of the Children’s Hospital Affiliated with the Capital Institute of Pediatrics. Clinical data were retrospectively collected from electronic medical records between January 2017 and May 2023. The study was approved by the Ethics Committee of the Capital Institute of Pediatrics (reference number: SHERLL2021034), and all procedures were conducted in accordance with the Declaration of Helsinki. For patients included after the initiation of the study, informed consent was obtained from the participants and their guardians. For data collected prior to the initiation, a waiver of informed consent was granted by the ethics committee for the use of de-identified retrospective data. We retrospectively selected children aged 0 to 15 years by retrieving data from electronic medical records between January 2017 and May 2023. A total of 4,668 patients were included. Data extraction and analysis were conducted from June 2023 to March 2024. As this study employed a cross-sectional design, it is important to note that causal relationships cannot be inferred from the observed associations.
Outcomes
The patients in our study were referred to the sleep laboratory for polysomnography (PSG) examinations by pediatricians and otolaryngologists from the Children’s Hospital affiliated with the Capital Institute of Pediatrics. Informed consent was obtained from all study participants and their legal guardians/parents prior to the initiation of the study. All participants underwent overnight polysomnography examination (Alice 6, Philips Respironics Inc., Murrysville, Pennsylvania).25 Sleep stages were meticulously scored by an experienced polysomnographic technician throughout the study, in accordance with the guidelines set by the American Academy of Sleep Medicine (AASM).26 Additionally, the scoring data were reviewed by pediatric sleep physicians to ensure the accuracy and consistency of the results. All PSG data were collected by two designated doctors and researchers.
Various variables were continuously monitored and recorded using computerized PSG, including a 6-channel electroencephalogram (with bilateral frontal, central, and occipital leads), electrocardiogram, airflow (measured via both nasal pressure cannula and thermistor), and respiratory effort (assessed using thoracic and abdominal inductive plethysmography. Oxygen saturation was monitored using pulse oximetry with a finger probe. Certified technicians manually scored the PSG according to the AASM manual.25 Sleep position was manually determined for each 30-second epoch. The AHI was defined as the total number of apneas and hypopneas per hour of sleep, while the oxygen desaturation index (ODI) was defined as the number of oxygen desaturations (≥ 3%) per hour of sleep. Children were diagnosed with OSA if their AHI was≥ 1, as determined by nocturnal PSG. The severity of OSA was classified as mild (AHI ≥ 1 and < 5), moderate (AHI ≥ 5 and < 10), or severe (AHI ≥ 10).27 All children do not have genetic syndrome. The exclusion criteria included: (1) neurological and muscular disorders, (2) children with AHI < 1, and (3) the presence of craniofacial anomalies, prematurity, or a prior history of adenotonsillectomy. The screening flow chart is shown in Figure 1. Body mass index (BMI) was calculated by dividing a child’s body weight (in kilograms) by the square of their height (in meters). Overweight and obesity were defined according to the Chinese national standard, “WS/T 586–2018: Screening for Overweight and Obesity Among School-Aged Children and Adolescents”, published by the National Health Commission of the People’s Republic of China.28 In this standard, BMI-for-age percentiles are used to classify weight status, thereby accounting for developmental differences across age groups. The BMI-for-age approach is consistent with international practices and provides an age- and sex-specific assessment of overweight, obesity, and undernutrition in children.29
 |
Figure 1 The screening flow chart. |
Statistical Analysis
Continuous data for normal distribution were expressed as mean ± standard deviation (SD), while categorical data were presented as frequency and percentage. ODI for skew distribution was displayed as median (P25, P75). Nonparametric statistical methods Mann–Whitney test were used for skewness distribution data. For continuous variables in demographic data and AHI values among different age groups, a one-way analysis of variance (ANOVA) was used. The chi-square test was used to assess differences in proportions among these age groups. Differences in the AHI between boys vs girls and obesity vs non-obesity were evaluated using independent sample t-tests. Linear trend analysis was applied to assess the statistical significance of changes in age, OSA severity, and obesity status. The Pearson linear correlation and partial correlation were used to evaluate the association between BMI and AHI, Min SpO2, rapid eye movement sleep (REM) period, non-rapid eye movement sleep (NREM) period. Using Pearson linear regression and mixed effect logistic regression models, we explored the relationship between AHI/ OSA severity and gender, age, BMI. In addition to controlling for age and gender, we also adjusted for BMI categories (underweight, normal weight, overweight, and obesity) to account for potential confounding effects. The level of statistical significance was set at P < 0.05. Statistical analyses were conducted using R (version 4.2.1).
Results
Basic Characteristics of the Participants
Our analysis included 4,668 children diagnosed with OSA, of which 1,758 (37.7%) were girls and 2,910 (62.3%) were boys. The mean age of the participants was 5.3 ± 2.7 years (range: 0–15 years). The mean BMI was 16.8 ± 3.7 kg/m², and the mean AHI was 8.4 ± 7.5 events per hour. Significant differences were observed between boys and girls in several parameters, including AHI, NREM AHI, %minimum SpO2, REM period, and ODI (Table 1). Boys had a higher mean BMI (17.1 ± 3.8 kg/m²) compared to girls (16.3 ± 3.4 kg/m²). However, no difference was found in REM sleep duration between the groups. Boys exhibited a significantly higher AHI during total sleep (8.8 ± 7.9 events per hour) compared to girls (7.7 ± 6.7 events per hour), with pronounced differences also observed in both REM sleep (boys: 14.8 ± 16.9 events per hour; girls: 13.6 ± 14.1 events per hour) and NREM sleep stages (boys: 7.6 ± 7.0 events per hour; girls: 6.6 ± 6.0 events per hour). Additionally, boys had a higher ODI 4.1(2.4,7.2) compared to girls 3.7(2.1,6.6) (P < 0.01). However, no significant difference was observed in the lowest oxygen saturation levels.
 |
Table 1 Characteristics of Patients with Obstructive Sleep Apnea According to Age |
Sleep Characteristics of Children with OSA in Various Age Groups
Children with OSA were categorized into different age groups: 0–2 years (7.6%), 3–5 years (55.1%), 6–8 years (24.9%), 9–11 years (8.5%), and 12–15 years (3.9%). BMI increased with age, reaching its peak in the 12–15-year group. Both total sleep time and REM sleep time showed significant variations across age groups. AHI during total sleep decreased notably with age, with the highest values observed in the 0-2-year group (10.7 ± 9.8) and the lowest in the 12–15-year group (7.7 ± 9.6). Both REM and NREM AHI also decreased significantly with age, peaking in the 0-2-year group. Minimum SpO2 during sleep did not show significant variation across age groups. However, ODI decreased significantly with age, with the highest values recorded in the 0-2-year group (Table 2).
 |
Table 2 Characteristics of Patients with OSA According to Different Age Groups |
Sleep and Respiratory Characteristics of Patients with Mild, Moderate, and Severe Obstructive Sleep Apnea
Significant variations in the distribution of OSA severity were observed across different age groups and genders (Figure 2). The age of patients varied significantly across mild, moderate, and severe OSA groups, with severe OSA patients being the youngest. Among children aged 0–2 years, boys had the highest proportion of severe OSA, whereas girls had the highest proportion of moderate OSA. Overall, as children aged, the proportion of mild OSA gradually increased, while the proportions of moderate and severe OSA tended to decrease.
 |
Figure 2 Age and Gender-Specific Distribution of OSA Severity. |
BMI consistently increased with OSA severity, with patients in the severe OSA category having the highest BMI (Table 3). The total sleep time (TST) varied across the different OSA severity groups. Both the moderate and severe OSA groups had longer TST compared to the mild group, with the moderate group showing the longest sleep duration overall. Regarding the REM period, moderate OSA patients had the longest duration, while mild OSA patients had the shortest. Additionally, both REM and NREM AHI increased significantly from mild to severe OSA. % minimum SpO2 levels were lowest in severe OSA patients, and the oxygen desaturation index (ODI) increased markedly with OSA severity, with the highest ODI observed in severe OSA and the lowest in mild OSA.
 |
Table 3 Sleep and Respiratory Characteristics of Patients with Mild, Moderate, and Severe Obstructive Sleep Apnea |
Obesity and Sleep in OSA Children
TST varied significantly across different BMI groups, with obese patients displaying the shortest TST and those with a normal BMI the longest (Table 4). Significant differences were also observed in AHI, REM AHI, and NREM AHI, with obese patients exhibiting the highest values, while the lowest values were found in patients with low BMI. Additionally, obese patients had the highest ODI, whereas those with low BMI had the lowest. However, there were no significant differences in % minimum SpO2 levels among the BMI groups. After controlling for age and gender, BMI remained significantly positively correlated with AHI, REM AHI, and NREM AHI, while it was negatively correlated with total sleep time and % minimum SpO2 (Table 5).
 |
Table 4 Sleep and Respiratory Characteristics During Different Obesity Statuses in Obstructive Sleep Apnea Children |
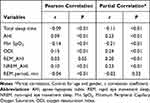 |
Table 5 Relationship Between BMI and Respiratory Characteristics in Obstructive Sleep Apnea Children |
Table 6 represents the univariate linear regression and multiple linear regression analyses for associations among AHI, age, gender and BMI. In the results of multiple linear regression analysis, the association between AHI and age (β=−0.30, P<0.001), BMI (β=0.25, P<0.001), gender (β=0.98, P<0.001) remained.
 |
Table 6 Linear Regression Analysis for Associations Between AHI and Related Factors |
Risk Factors Associated with Severity of OSA
The Univariate Logistic Regression showed that male (OR=1.27, 95% CI: 1.13–1.44), 0–2 years old (OR=2.59, 95% CI: 1.78–3.77), 3–5 years old (OR=1.54, 95% CI: 1.14–2.09), overweight (OR=1.27, 95% CI: 1.05–1.53) and obesity (OR=1.29, 95% CI: 1.10–1.52) were associated with the moderate to severe OSA. The multi-factor Logistic Regression revealed the similar results in Table 7, where the male (OR=1.2, 95% CI: 1.11–1.43), 0–2 years old (OR=1.49, 95% CI: 1.09–2.04), overweight (OR=1.25, 95% CI: 1.03–1.51) and obesity (OR=1.29, 95% CI: 1.09–1.52) were risk factors.
 |
Table 7 The Relationship Between Age Group, Gender and Obesity and OSA Severity in Children and Adolescents Using Logistic Regression Model Analysis |
Discussion
This cross-sectional study aims to analyze data from 4,668 children to investigate the impact of age, gender, and obesity on pediatric OSA. In contrast, our previously published study included 1,236 participants who underwent both PSG and completed sleep questionnaires. This earlier study primarily focused on examining the prevalence, risk factors, and clinical characteristics of positional obstructive sleep apnea (POSA) in children with OSA, and used propensity score matching (PSM) to control for confounding factors.30 In the current study, participants only underwent PSG without completing sleep questionnaires. With a larger sample size of 4,668 children, we employed statistical methods such as linear trend analysis, Pearson correlation, and partial correlation analysis. Unlike our previous study, which focused on POSA in OSA patients, the current research uniquely centers on the effects of gender, age, and obesity on pediatric OSA, making it distinct in both research objectives and methodology. The results highlighted significant differences in OSA based on gender, age, and BMI. While previous studies13 have explored the independent associations of age, gender, and obesity with pediatric OSA, these factors have rarely been examined in combination within a large, real-world clinical population. Our study offers novel contributions by analyzing the interactive effects of age, gender, and obesity on OSA severity in a substantial study of 4,668 children using objective PSG data. This approach allowed for the identification of distinct, developmentally relevant patterns, such as the highest AHI values observed in children aged 0–2 years, sex-based differences in OSA severity, and a clear trend of increasing severity with obesity. By integrating these variables within the same analytic framework and stratifying OSA severity based on PSG indices, our findings provide a more nuanced and clinically actionable understanding of risk stratification in pediatric OSA. This study therefore advances current knowledge beyond prior work that primarily examined these variables in isolation or used smaller sample sizes, offering new perspectives on how demographic and anthropometric factors interact to shape OSA severity during childhood.
Strengths and Limitations
This study offers several notable strengths. First, it included a large sample size of 4,688 pediatric patients with OSA, which helps to overcome the limitations of small sample sizes commonly seen in previous research. Second, all participants underwent nocturnal PSG, the gold standard for diagnosing OSA, ensuring consistent and accurate measurement of OSA severity across the entire study. Third, the study conducted a comprehensive analysis that simultaneously considered the effects of gender, age, and obesity on OSA. This multifactorial approach allowed the identification of key trends that provide valuable guidance for healthcare professionals involved in the diagnosis and management of pediatric OSA.
However, several limitations should also be acknowledged. First, as a single-center study conducted in mainland China, the findings may not be representative of the broader pediatric population, which limits their generalizability. Second, the cross-sectional design precludes the ability to establish definitive causal relationships between age, sex, obesity, and OSA severity. While the associations observed are statistically and clinically significant, longitudinal studies are needed to explore potential causal pathways and temporal dynamics. Third, the study population was ethnically homogenous, which may limit the applicability of the findings to other ethnic or regional groups. Future research involving multi-ethnic and multi-center cohorts is necessary to validate and extend these findings. Finally, due to limitations in extracting data from retrospective sleep study reports, T90 values were not consistently available for all patients and were therefore excluded from the analysis. To gain deeper insights into oxygen desaturation patterns, future studies should consider prospective cohort designs that systematically collect consistent T90 data.
Gender Differences
The research revealed notable gender differences in pediatric OSA.31 Boys exhibited higher AHI and ODI scores than girls, indicating a more severe manifestation of the disease. Several factors contribute to gender disparities in OSA severity among pediatric patients. Anatomical differences, such as the susceptibility of the anterior respiratory tract to nighttime collapse, play a significant role. For example, the retrusive movement of the mandible in boys has been shown to significantly reduce the cross-sectional area of the pharyngeal and oropharyngeal junctions, a change not observed in girls. Consequently, boys typically experience more severe OSA and are more reliant on changing body positions during sleep for relief.32–37 As the severity of OSA is associated with BMI,38 our study revealed that boys had significantly higher BMI than girls. To minimize bias, we conducted both univariate and multivariate analyses, which identified male gender as a risk factor for moderate to severe OSA. This finding further underscores that OSA tends to be more severe in boys compared to girls.
Age-Related Variations
In this study, we found significant variations in the prevalence and severity of OSA among different age groups of children. Firstly, the prevalence of OSA was highest in children aged 3–5 years, and the severity of OSA symptoms during this period was relatively severe, second only to that observed in children aged 0–2 years. The high prevalence of OSA in the 3–5 years age group may be closely related to the enlargement of the adenoids and tonsils during this period, particularly due to the widespread occurrence of lymphoid tissue hyperplasia, which increases the risk of airway obstruction.39 As children enter the 6–8 years age group, the adenoids typically reach a state of relative stability, resulting in a lower prevalence of OSA compared to the 3–5 years age group. The prevalence of OSA continues to decline with age, reaching its lowest point during adolescence (12–15 years). In adolescence, the role of the adenoids diminishes, and other factors come into play. For instance, hormonal changes associated with puberty may positively impact the tone and stability of the upper airway muscles, thereby reducing the severity of OSA.40 Moreover, research indicates that children under the age of three experience the most severe OSA, suggesting that this age group should be considered at high risk.41 This finding is consistent with our results that the AHI is highest in children aged 0–2 years and that children in this age group are a risk factor for the development of moderate to severe OSA. Possible reasons include: firstly, parents often become aware of the issue and seek medical help only when symptoms are more severe, which may lead to a concentration of severe cases in this age group. Secondly, younger children may have an underdeveloped nervous system, potentially leading to inadequate control of the upper airway and an increased frequency of breathing disorders.42 Thirdly, our results also showed that patients aged 0–2 years had the shortest REM sleep time, but the highest REM-AHI. This may be because infants and young children have reduced muscle tension during REM, especially the muscles of the upper airway, which may make upper airway obstruction more likely, thereby increasing the incidence of apnea. This may also explain why OSA is the most severe in patients at this stage. Studies have shown that REM% < 10% is a stronger predictor of more severe SDB in children.43 These findings underscore that age is a crucial factor affecting the prevalence and severity of OSA, especially during early childhood.
Impact of Obesity
Recent research had highlighted the significant impact of obesity on OSA across different age groups. Obesity, particularly central obesity, significantly increases the risk and severity of OSA among adults.44 This condition not only exacerbates the fragility of pharyngeal tissues and lung capacity due to mechanical forces but also disrupts airway neuromuscular control through activation of signaling proteins in the central nervous system.45 Research has been constrained by the neglect of OSA as a complex condition encompassing diverse subtypes, arising from varying contributions of anatomical, physiological, inflammatory, and obesity-linked risk factors, ultimately leading to distinct physiological aberrations.46 In recent years, the significance of childhood obesity and its correlation with OSA has garnered considerable attention in public health discussions. Childhood obesity rates are on the rise, accompanied by notable comorbidities such as OSA and increased cardiovascular morbidity.45 Evidence consistently indicates that childhood obesity substantially heightens the risk of OSA.47 Obesity was found to be a risk factor for moderate to severe OSA in our study. This finding aligns with previous research indicating that the severity of OSA in many children and adolescents correlates with the severity of obesity.38 The pathophysiological mechanisms underlying this association involve upper airway obstruction, altered chest wall dynamics, and aberrations in ventilatory control.48 However, despite these insights, there remains a gap in research directly comparing the severity of OSA in children with and without obesity across different age groups. The pathophysiological mechanisms underlying this association involve upper airway obstruction, altered chest wall dynamics, and disturbances in ventilatory control.49 Our results indicated that the obese group experienced the shortest duration of REM sleep, yet exhibited the highest REM-AHI. This is consistent with previous studies, which have shown that overweight and obese children tend to have reduced REM sleep and more severe obstructive sleep apnea. This may be due to the higher degree of sleep fragmentation common in obese patients, which shortens their REM sleep duration. Additionally, reduced sleep quality and frequent awakenings may contribute to an overall increase in AHI. More importantly, the elevated REM-AHI in obese children may be explained by pathophysiological mechanisms related to airway muscle tone and fat distribution. During REM sleep, there is a physiological reduction in muscle tone, including the pharyngeal dilator muscles, which makes the upper airway more susceptible to collapse. In obese children, this vulnerability is further exacerbated by increased fat deposition in the upper airway structures, such as the lateral pharyngeal walls and tongue base. These deposits increase airway collapsibility and narrow the airway lumen. The added mechanical load on the pharyngeal walls compromises airway patency during REM sleep, a stage already characterized by hypotonia, thereby resulting in more frequent and severe obstructive events. Thus, the combination of reduced neuromuscular compensation and structural narrowing due to obesity likely contributes to elevated REM-AHI in these patients.50–52 OSA also can impact obesity in children through several mechanisms. First, the positive correlation between leptin levels in the blood and the amount of adipose tissue means that obesity is associated with elevated leptin levels.53 However, while patients with OSA also have high leptin levels, they often exhibit decreased sensitivity to this hormone, a phenomenon known as leptin resistance.54 This reduced sensitivity leads to increased levels of ghrelin, the appetite-stimulating peptide.55 Consequently, this hormonal imbalance can result in greater food intake and weight gain, further contributing to obesity. Additionally, poor sleep quality and fragmented sleep often result in daytime sleepiness, which can reduce physical activity levels and further promote weight gain. Second, OSA can affect metabolic function, including glucose metabolism, leading to insulin resistance and an increased risk of obesity-related comorbidities. The sympathetic nervous system is often activated in response to the intermittent hypoxia seen in OSA, leading to increased cortisol levels, a stress hormone linked to abdominal fat deposition. These factors create a cycle where obesity worsens OSA, and OSA, in turn, exacerbates obesity, further complicating the management of both conditions. While our study cannot establish a causal relationship due to its cross-sectional design, the observed correlation between obesity and OSA severity in children suggests that these conditions may influence each other in a bidirectional manner.56–59 Future longitudinal studies are needed to better understand the temporal relationship and underlying mechanisms.
Implications
Notably, it is important to distinguish the differences in the characteristics of pediatric OSA across various ethnic groups. Some studies have shown that in Western populations, pediatric OSA is often more severe in early childhood and tends to improve during adolescence.60 Additionally, research suggests that differences in craniofacial morphology may contribute to boys having more severe OSA than girls in Western populations.61 A study from Spain reported a higher prevalence of obesity-related OSA in the general pediatric population, with childhood obesity identified as a predictor of severe OSA.62,63 These findings align with our results, which, based on a larger Asian sample, reflect similar trends observed in Western populations: boys, younger children, and those with obesity are more likely to experience severe OSA. This suggests that certain aspects of pediatric OSA may be similar between Asian and Western populations, though the specific pathophysiological mechanisms require further investigation.
Overall, the findings of this study suggest that healthcare providers should prioritize targeted OSA screening for boys, younger children (especially those aged 0–2 years), and children who are overweight or obese, as they are at higher risk of developing severe symptoms. Secondly, interventions should be tailored to meet the specific needs of these groups, such as emphasizing weight management strategies for children with obesity. Lastly, understanding how variables such as age, gender, and obesity interact may have prognostic implications. For example, children with both obesity and early-onset OSA may represent a subgroup with persistent or treatment-resistant disease. Recent evidence suggests that phenotype-driven approaches, including the use of drug-induced sleep endoscopy (DISE), can inform surgical planning and potentially improve outcomes. A systematic review64 showed that DISE-directed surgery led to changes in surgical strategy in over 50% of pediatric OSA cases and achieved meaningful reductions in AHI, indicating that individualized anatomical assessment may enhance treatment success. These findings underscore the importance of integrating clinical phenotypes and risk factors to guide prognosis and optimize intervention strategies.
Conclusion
In summary, this study confirms significant gender, age, and BMI disparities in pediatric OSA severity, revealing that boys, younger children (especially those aged 0–2 years), and obese individuals tend to experience more severe symptoms. Importantly, our study is one of the first to investigate these associations in a large pediatric examination in mainland China, providing region-specific data that can guide local clinical practice. These findings underscore the need for early screening and targeted interventions for high-risk groups. While the cross-sectional design limits causal inference, our results contribute to the growing body of evidence on pediatric OSA and highlight the necessity of future longitudinal and multicenter studies to validate these findings, explore causal mechanisms, and develop personalized treatment strategies.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, GQL, upon reasonable request.
Author Contributions
HGM - Formal analysis, Conceptualization, Software, Resources, Methodology, Validation, Supervision, Funding acquisition, Writing – original draft, Writing – review & editing. WQ - Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. CL - Conceptualization, Project administration, Resources, Supervision, Validation, Formal analysis, Writing – review & editing. YSY - Data curation, Methodology, Resources, Investigation, Writing – review & editing. LJT - Formal analysis, Methodology, Project administration, Validation, Software, Writing – review & editing. LYX - Conceptualization, Methodology, Supervision, Validation, Writing – review & editing. LT - Conceptualization, Data curation, Methodology, Project administration, Writing – review & editing. ZXJ-Data curation, Methodology, Supervision, Project administration, Writing – review & editing. LJQ - Data curation, Resources, Investigation, Writing – original draft. CYJ - Formal analysis, Methodology, Validation, Writing – review & editing. GQL - Conceptualization, Writing – review & editing, Methodology, Project administration, Funding acquisition, Supervision.
All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Capital’s Funds for Health Improvement and Research (CFH 2024-2G-1135), National Natural Science Foundation of China (Grant 72004142), Beijing Municipal Natural Science Foundation (7232010), and Key Program of Capital’s Funds for Health Improvement and Research (2022-1-2101). The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Disclosure
All authors report no conflicts of interest in this work.
References
1. Ersu R, Chen ML, Ehsan Z, Ishman SL, Redline S, Narang I. Persistent obstructive sleep apnoea in children: treatment options and management considerations. Lancet Respir Med. 2023;11(3):283–296. doi:10.1016/S2213-2600(22)00262-4
2. Tofangchiha M, Esfehani M, Eftetahi L, et al. Comparison of the pharyngeal airway in snoring and non-snoring patients based on the lateral cephalometric study: a case-control study. Dent Med Probl. 2023;60(1):121–126. doi:10.17219/dmp/154776
3. Dastan F, Ghaffari H, Shishvan HH, et al. Correlation between the upper airway volume and the hyoid bone position, palatal depth, nasal septum deviation, and concha bullosa in different types of malocclusion: a retrospective cone-beam computed tomography study. Dent Med Probl. 2021;58(4):509–514. doi:10.17219/dmp/130099
4. Bixler EO, Vgontzas AN, Lin H-M, et al. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep. 2009;32(6):731–736. doi:10.1093/sleep/32.6.731
5. Marcus CL, Brooks LJ, Ward SD, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714–e755. doi:10.1542/peds.2012-1671
6. Li AM, So HK, Au CT, et al. Epidemiology of obstructive sleep apnoea syndrome in Chinese children: a two-phase community study. Thorax. 2010;65(11):991–997. doi:10.1136/thx.2010.134858
7. Bitners AC, Arens RJL. Evaluation and management of children with obstructive sleep apnea syndrome. Lung. 2020;198(2):257–270. doi:10.1007/s00408-020-00342-5
8. Urbano GL, Tablizo BJ, Moufarrej Y, Tablizo MA, Chen ML, Witmans M. The link between pediatric obstructive sleep apnea (OSA) and attention deficit hyperactivity disorder (ADHD). Children. 2021;8(9):824. doi:10.3390/children8090824
9. Smith DF, Amin RS. OSA and cardiovascular risk in pediatrics. Chest. 2019;156(2):402–413. doi:10.1016/j.chest.2019.02.011
10. Karuga FF, Jaromirska J, Sochal M, Białasiewicz P, Gabryelska A, Problems M. Association between glucose metabolism, the circadian cycle and hypoxia: evaluation of the NPAS2 and Rev-Erb-α protein serum levels in obstructive sleep apnea patients-a pilot study. Dent Med Probl. 2024;61(3):465–469. doi:10.17219/dmp/185718
11. Kanclerska J, Wieckiewicz M, Nowacki D, et al. Sleep architecture and vitamin D in hypertensives with obstructive sleep apnea: a polysomnographic study. Dent Med Probl. 2024;61(1):43–52. doi:10.17219/dmp/172243
12. Mehdipour A, Fateh R, Fuladvand F, et al. Association between sleep pattern, salivary cariogenic bacteria and fungi populations, pH and buffering capacity in children: a comparative study. Dent Med Probl. 2024;61(2):217–224. doi:10.17219/dmp/167411
13. Di Mauro P, Cocuzza S, Maniaci A, et al. The effect of adenotonsillectomy on children’s behavior and cognitive performance with obstructive sleep apnea syndrome: state of the art. Children. 2021;8(10):921. doi:10.3390/children8100921
14. Forcelini CM, Buligon CM, Costa GJK, et al. Age-dependent influence of gender on symptoms of obstructive sleep apnea in adults. Sleep Sci. 2019;12(03):132–137. doi:10.5935/1984-0063.20190076
15. Bonsignore MR, Saaresranta T, Riha RL. Sex differences in obstructive sleep apnoea. Eur Respir Rev. 2019;28(154):190030. doi:10.1183/16000617.0030-2019
16. Dudley KA, Patel SR. Disparities and genetic risk factors in obstructive sleep apnea. Sleep Med. 2016;18:96–102. doi:10.1016/j.sleep.2015.01.015
17. Kang KT, Weng WC, Lee PL, Hsu WC. Age‐and gender‐related characteristics in pediatric obstructive sleep apnea. Pediatr Pulmonol. 2022;57(6):1520–1526. doi:10.1002/ppul.25900
18. Brockmann PE, Koren D, Kheirandish-Gozal L, Gozal D. Gender dimorphism in pediatric OSA: is it for real? Respir Physiol Neurobiol. 2017;245:83–88. doi:10.1016/j.resp.2016.11.010
19. Inoshita A, Kasai T, Matsuoka R, et al. Age-stratified sex differences in polysomnographic findings and pharyngeal morphology among children with obstructive sleep apnea. J Thorac Dis. 2018;10(12):6702. doi:10.21037/jtd.2018.11.09
20. Gabbay IE, Lavie P. Breathing. Age-and gender-related characteristics of obstructive sleep apnea. Sleep Breath. 2012;16:453–460. doi:10.1007/s11325-011-0523-z
21. Bachrach K, Danis DON, Cohen MB, Levi JR. The relationship between obstructive sleep apnea and pediatric obesity: a nationwide analysis. Ann Otol Rhinol Laryngol. 2022;131(5):520–526. doi:10.1177/00034894211028489
22. Narang I, Mathew JL. Childhood obesity and obstructive sleep apnea. J Nutr Metab. 2012;2012(1):134202. doi:10.1155/2012/134202
23. Selvadurai S, Voutsas G, Propst EJ, Wolter NE, Narang IJP, Health C. Obstructive sleep apnea in children aged 3 years and younger: rate and risk factors. Paediatr Child Health. 2020;25(7):432–438. doi:10.1093/pch/pxz097
24. Magnusdottir S, Hill EA. Prevalence of obstructive sleep apnea (OSA) among preschool aged children in the general population: a systematic review. Sleep Med Rev. 2024;73:101871. doi:10.1016/j.smrv.2023.101871
25. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events: deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi:10.5664/jcsm.2172
26. American Academy of Sleep Medicine and Others. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–689. PMID: 10450601. doi:10.1093/sleep/22.5.667
27. Hsu WC, Kang KT, Yao CCJ, et al. Evaluation of upper airway in children with obstructive sleep apnea using cone‐beam computed tomography. Laryngoscope. 2021;131(3):680–685. doi:10.1002/lary.28863
28. Wang L, Wang Z, Ma Q, et al. The development and reform of public health in China from 1949 to 2019. Global Health. 2019;15:1–21. doi:10.1186/s12992-019-0486-6
29. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240. doi:10.1136/bmj.320.7244.1240
30. Wang Q, Huang G, Wang R, et al. Evaluating positional obstructive sleep apnea in children: prevalence, characteristics, and risk factors. Nat Sci Sleep. 2024;16:1569–1581. doi:10.2147/NSS.S481742
31. Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164(4):406–418. doi:10.1001/archinte.164.4.406
32. Barsh LI. The origin of pharyngeal obstruction during sleep. Sleep Breath. 1999;3(01):017–022. doi:10.1007/s11325-999-0017-4
33. Mohsenin V. Effects of gender on upper airway collapsibility and severity of obstructive sleep apnea. Sleep Med. 2003;4(6):523–529. doi:10.1016/s1389-9457(03)00168-0
34. O’connor C, Thornley KS. Hanly PJJAjor, medicine cc. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161(5):1465–1472. doi:10.1164/ajrccm.161.5.9904121
35. PV T. Incidence of sleep-disordered breathing in an urban adult population. JAMA. 2003;289:2230–2237. doi:10.1001/jama.289.17.2230
36. Mohsenin V. Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest. 2001;120(5):1442–1447. doi:10.1378/chest.120.5.1442
37. Popovic RM. White DPJAjor, medicine cc. Influence of gender on waking genioglossal electromyogram and upper airway resistance. Am J Respir Crit Care Med. 1995;152(2):725–731. doi:10.1164/ajrccm.152.2.7633734
38. Mallory GB, Fiser DH, Jackson R. Sleep-associated breathing disorders in morbidly obese children and adolescents. J Pediatr. 1989;115(6):892–897. doi:10.1016/s0022-3476(89)80738-3
39. McNeill E, Houston R. Diseases of the adenoids and tonsils in children. Surgery. 2021;39(9):617–624. doi:10.1016/j.mpsur.2021.08.003
40. Lin CM, Davidson TM, Ancoli-Israel S. Gender differences in obstructive sleep apnea and treatment implications. Sleep Med Rev. 2008;12(6):481–496. doi:10.1016/j.smrv.2007.11.003
41. Don DM, Geller KA, Koempel JA, Ward SD. Age specific differences in pediatric obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 2009;73(7):1025–1028. doi:10.1016/j.ijporl.2009.04.003
42. Marcus CL. Pathophysiology of childhood obstructive sleep apnea: current concepts. Respir Physiol. 2000;119(2–3):143–154. doi:10.1016/s0034-5687(99)00109-7
43. Yang L, Huang Z, Zhong J, Qiu S, Liu D. The characteristics and clinical significance of REM< 10% in children with sleep-disordered breathing. Int J Pediatr Otorhinolaryngol. 2018;110:53–56. doi:10.1016/j.ijporl.2018.04.015
44. Ioan I, Mulier G, Taytard J, Césaire A, Beydon N. Evaluation of obesity and asthma as risk factors for moderate to severe obstructive sleep apnea in children. J Clin Sleep Med. 2022;18(6):1639–1648. doi:10.5664/jcsm.9948
45. Iyigun I, Alikasifoglu A, Gonc N, et al. Obstructive sleep apnea in children with hypothalamic obesity: evaluation of possible related factors. Pediatr Pulmonol. 2020;55(12):3532–3540. doi:10.1002/ppul.25097
46. Redline S, Azarbarzin A, Peker Y. Obstructive sleep apnoea heterogeneity and cardiovascular disease. Nat Rev Cardiol. 2023;20(8):560–573. doi:10.1038/s41569-023-00846-6
47. St‐Onge MP. Sleep–obesity relation: underlying mechanisms and consequences for treatment. Obes Rev. 2017;18:34–39. doi:10.1111/obr.12499
48. Thuler E, Rabelo FA, Yui M, Tominaga Q, Dos Santos V, Arap SS. Correlation between the transverse dimension of the maxilla, upper airway obstructive site, and OSA severity. J Clin Sleep Med. 2021;17(7):1465–1473. doi:10.5664/jcsm.9226
49. Gatt D, Ahmadiankalati M, Voutsas G, Katz S, Lu Z, Narang I. Identification of obstructive sleep apnea in children with obesity: a cluster analysis approach. Pediatr Pulmonol. 2024;59(1):81–88. doi:10.1002/ppul.26712
50. Sever O, Kezirian EJ, Gillett E, et al. Association between REM sleep and obstructive sleep apnea in obese and overweight adolescents. Sleep Breath. 2019;23:645–650. doi:10.1007/s11325-018-1768-6
51. Liu X, Forbes EE, Ryan ND, Rofey D, Hannon TS, Dahl RE. Rapid eye movement sleep in relation to overweight in children and adolescents. Arch Gen Psychiatry. 2008;65(8):924–932. doi:10.1001/archpsyc.65.8.924
52. Karamessinis L, Galster P, Schultz B, et al. Relationship between REM density, duty cycle, and obstructive sleep apnea in children. Sleep. 2007;30(7):837–843. doi:10.1093/sleep/30.7.837
53. Friedman JM. Leptin and the regulation of body weigh. Keio J Med. 2011;60(1):1–9. doi:10.2302/kjm.60.1
54. Marik PE. Leptin, obesity, and obstructive sleep apnea. Chest. 2000;118(3):569–571. doi:10.1378/chest.118.3.569
55. Ursavas A, Ilcol YO, Nalci N, Karadag M, Ege E. Ghrelin, leptin, adiponectin, and resistin levels in sleep apnea syndrome: role of obesity. Ann Thorac Med. 2010;5(3):161–165. doi:10.4103/1817-1737.65050
56. Ischander MM, Lloyd RD. Severe paediatric obesity and sleep: a mutual interactive relationship! J Sleep Res. 2021;30(3):e13162. doi:10.1111/jsr.13162
57. Ong CW, O’Driscoll DM, Truby H, Naughton MT, Hamilton GS. The reciprocal interaction between obesity and obstructive sleep apnoea. Sleep Med Rev. 2013;17(2):123–131. doi:10.1016/j.smrv.2012.05.002
58. Bonsignore MR. Obesity and obstructive sleep apnea. Lancet. In: From Obesity to Diabetes. Springer; 2021:181–201. doi:10.1016/S0140-6736(13)60734-5
59. Framnes SN, Arble DM. The bidirectional relationship between obstructive sleep apnea and metabolic disease. Front Endocrinol. 2018;9:440. doi:10.3389/fendo.2018.00440
60. Spilsbury JC, Storfer-Isser A, Rosen CL, Redline S. Remission and incidence of obstructive sleep apnea from middle childhood to late adolescence. Sleep. 2015;38(1):23–29. doi:10.5665/sleep.4318
61. Di Francesco R, Monteiro R, de Melo Paulo ML, Buranello F, Imamura R. Craniofacial morphology and sleep apnea in children with obstructed upper airways: differences between genders. Sleep Med. 2012;13(6):616–620. doi:10.1016/j.sleep.2011.12.011
62. Alonso-álvarez ML, Cordero-Guevara JA, Terán-Santos J. Obstructive sleep apnea in obese community-dwelling children: the NANOS study. J Sleep. 2014;37(5):943–949. doi:10.5665/sleep.3666
63. Narayanan A, Yogesh A, Mitchell RB, Johnson RF. Asthma and obesity as predictors of severe obstructive sleep apnea in an adolescent pediatric population. Laryngoscope. 2020;130(3):812–817. doi:10.1002/lary.28029
64. Wu Y, Zheng L, Cui G, Xu Z, Ni X. Subtypes of obstructive sleep apnea in children and related factors. J Clin Sleep Med. 2022;18(10):2397–2404. doi:10.5664/jcsm.10124
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Age and Gender, but Not Pain are Associated with Pressure Pain Thresholds in Patients with Temporomandibular Disorders: A Cross-Sectional Study
Zheng Y, Zhu R, Xiao C, Cheng Q, Long Y, Zhou X, Zhang S, Wang J, Xiong X
Journal of Pain Research 2023, 16:2205-2216
Published Date: 28 June 2023
What are the Main Risk Factors Associated with Erectile Dysfunction in the Elderly? A Cross-Sectional Study of 2436 Brazilian Elderly Men
Pitta RM, de Lima Queiroga L, Louzada ACS, Ritti-Dias RM, Kaufmann OG, Wolosker N
Clinical Interventions in Aging 2023, 18:1047-1054
Published Date: 8 July 2023
An Investigation into the Characteristics and Distribution Patterns of Diseases Detected via Gastroscopy in Northern Xinjiang, China
Wang FF, Li N, Wang JJ, Muyesai N, Fu H
Journal of Multidisciplinary Healthcare 2024, 17:229-235
Published Date: 16 January 2024
Modulation of Human Macrophages by Plasma from COVID-19 Patients Following BCG Vaccination: BATTLE Trial
Buosi K, Jalalizadeh M, Maia AR, Morari J, Velloso LA, Reis LO
International Journal of General Medicine 2024, 17:3107-3117
Published Date: 16 July 2024
Technostress Among Older Workers: A Central European Perspective
Rašticová M, Šácha J, Lakomý M, Mishra PK
Psychology Research and Behavior Management 2025, 18:1211-1225
Published Date: 24 May 2025

