Back to Journals » Infection and Drug Resistance » Volume 17
Impact of Jordanian Pharmacists’ Knowledge of the Human Microbiome: Has the Practice of Antibiotics and Probiotics Dispensing Been Affected? A Cross-Sectional Study
Authors Sawan HM , Shroukh W, Abutaima R , Al Omari SM , Abdel-Qader DH, Binsuwaidan R
Received 4 September 2024
Accepted for publication 19 November 2024
Published 26 November 2024 Volume 2024:17 Pages 5203—5214
DOI https://doi.org/10.2147/IDR.S494714
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Hana M Sawan,1 Wejdan Shroukh,2 Rana Abutaima,3 Shatha M Al Omari,1 Derar H Abdel-Qader,4 Reem Binsuwaidan5
1Pharmaceutical Sciences Department, Faculty of Pharmacy, Zarqa University, Zqrqa, Jordan; 2Faculty of Pharmacy, Middle East University, Amman, Jordan; 3Faculty of Pharmacy, Zarqa Private University, Zarqa, Jordan; 4Faculty of Pharmacy and Medical Sciences, University of Petra, Amman, Jordan; 5Department of Pharmaceutical Sciences, College of Pharmacy, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia
Correspondence: Hana M Sawan, Email [email protected]
Objective: This study aimed to assess Jordanian pharmacists’ knowledge of the human microbiome and the impact of their knowledge on their attitudes and practices toward antibiotics and probiotics.
Methods: A self-administered survey was designed after reviewing the literature. Participants’ demographics were collected, and questions to evaluate pharmacists’ knowledge, attitudes, and practices toward antibiotic and probiotic dispensing were asked. The data were analyzed using the Statistical Package for the Social Sciences V.26. Pearson correlations and one-way ANOVA were employed to calculate the significance of knowledge, attitudes, and practices. Statistical significance was considered at p < 0.05.
Results: Of the 333 respondents, around 75% (n=250) had a high level of general knowledge regarding the human gut microbiome. Almost equal proportions of participants had either intermediate or high levels of knowledge about the role of gut bacteria in health (n=164, 49.2%) (n=166, 49.8%), respectively, while almost two-thirds had an intermediate level of knowledge of the role of gut bacteria in disease (n=197, 59.2%). More than half of the participants had a positive attitude toward antibiotics, probiotics, and the human microbiome (n=179, 53.8%), and the majority (n=239, 71.8%) had an intermediate level of practice with them. There was a significant positive correlation between pharmacists’ general knowledge of the human microbiome and their positive attitudes (r=0.306, p < 0.01) and practices (r=0.331, p < 0.01) toward antibiotics and probiotics.
Conclusion: Study results raise the importance of interventional educational measures to promote healthcare professionals’ knowledge of the human microbiome and their potential beneficence on pharmacists’ attitudes and practices regarding antibiotics and probiotics dispensing. The results also denote the urgent need for probiotics’ clinical guidelines to ensure practice uniformity.
Keywords: human microbiome, antibiotics, probiotics
Introduction
The role of the human microbiome in health and disease keeps unraveling and public awareness of the topic is widely spreading,1 so healthcare professional’s knowledge of microbiome aspects, factors, and interactions has become a necessity in practice.2 Antibiotic resistance, as a global health threat, has mainly been attributed to the misuse and overuse of antibiotics. Pharmacists’ attitudes and practices toward antibiotics greatly impact antibiotic resistance, as they are responsible for dispensing antibiotics and educating the public about their appropriate use.
Many studies have investigated the contributing factors behind public and healthcare professionals’ attitudes and practices leading to antibiotic resistance, including antibiotics-self-medication and antibiotic dispensing without a prescription, which are widely disseminated within Arab countries, including Jordan,3 the United Arab Emirates (UAE),4 and Saudi Arabia.5
One of the proposed, yet controversial, mechanisms to improve health is the consumption of probiotics; however, there is extensive debate around their safety, efficacy, and suitability for certain groups of people (eg, children, the elderly, and pregnant women), in addition to the absence of clinical and practice guidelines and regulations (ie, target population, dosing, and counseling).6 Therefore, public acceptability and over-The-counter dispensing of probiotics fall on physicians and pharmacists; hence, pharmacists’ knowledge of probiotics is considered crucial in shaping the public understanding of probiotic efficacy and safety. In order to demonstrate the influence of pharmacists in the dispensation of laxatives and probiotics, a study conducted in Spain have found that over 90% of the patients followed the advice of the pharmacist over the advice of their doctors.7
In this study, we propose knowledge of the human microbiome as a novel predictor factor contributing to pharmacists’ attitudes and behaviors regarding antibiotics and probiotics, and show that providing pharmacists with satisfactory orientation regarding the human microbiome and its role in health and disease could be crucial in our battle against attitudes and practices contributing to antibiotic resistance. An example of knowledge gaps affecting pharmacists’ practices is the misconception by some pharmacists that probiotics are primarily intended for gastrointestinal health, as was shown in a recent study conducted in the UAE assessing pharmacists’ knowledge, perception, and prescribing practice of probiotics.8
Methods
Survey Development
A literature review was performed in preparation for the cross-sectional assessment of community and hospital pharmacists’ knowledge, attitudes, and practices toward antibiotic and probiotic dispensing based on their knowledge of the human microbiome. The questionnaire was designed using Google® forms and in paper format both in Arabic (the official language of Jordan) and English. Two academics, fluent in both languages, translated the questionnaire from Arabic to English to ensure similarity and content validity.9 Content and face validity of the questionnaire were ensured by consulting experts in the field who reviewed the questionnaire and took part in finalizing it. The questionnaire was then piloted on 10 individuals, academics, and non-academics to account for face validity. Their feedback and comments were considered for any unclear questions or jargon, which were removed accordingly. The responses of the pilot samples were not included in the final statistical analyses. The number of registered pharmacists in Jordan was obtained from the Jordanian Pharmacists Syndicate records, and the sample size was calculated using an online calculator with a 95% confidence interval and a 5% margin of error.10 The target group was all registered pharmacists in Jordan who worked in either a community or a hospital pharmacy. Data collection was performed from June to September 2022 by disseminating the questionnaire either online across different social media groups with member pharmacists or in paper format by visiting pharmacists’ workplaces with the aim of manually responding to the questionnaire.
Survey Sections
The questionnaire consisted of four main sections. The first part explored participants’ demographics, such as age, gender, place of residence, educational level, the facility sector where they worked (ie, public or private), practice settings (community or hospital pharmacist), and years of experience. The second section evaluated pharmacists’ knowledge of bacteria, the human microbiome, and antibiotics in general. Questions about the human microbiome were designed on a 2 point Likert scale, with answers divided between agree and disagree, in which a knowledge score based on a comprehensive literature review was established (see Appendix 1).
Questions in the third section were constructed in three parts and in the first part examined whether pharmacists were able to recognize the role of the microbiome in health and disease based on an agree or disagree scale and a predesigned knowledge score. The role of the microbiome in digestion, nutrient production, activation of immune response, cognitive skills, response to medications, wound healing, fertility, food preferences, physical exercise endurance, and aging was also investigated. The second part of this section asked pharmacists to describe the imbalance of the gut microbiome and the factors that promote its progression using a checkbox of different relevant factors, such as smoking, unhealthy lifestyle, antibiotic misuse, pollution, and hormonal imbalance. The third part of this section evaluated the participants’ knowledge of the microbiome’s role in disease states and possible methods to reverse this imbalance.
The last section was designed based on a Likert scale of five degrees ranging from strongly disagree to strongly agree to investigate pharmacists’ attitudes and practices regarding antibiotic and probiotic use and their influence on the human microbiome.
Ethics Approval
Research ethics approval was obtained from the Ethics Committee for Scientific Research at Zarqa University, with approval number (Zu-2023/7/5306/37) prior to conducting the study. Informed consent was collected from participants before they recorded their responses to the questionnaire, while ensuring that participant’s identities were anonymously maintained. Their responses were treated confidentially, and they were informed that they could withdraw from responding at any time while filling out the questionnaire.
Statistical Analyses
The data were cleared and analyzed using the Statistical Package for the Social Sciences (SPSS) version 26. Simple descriptive statistics were used to present the general characteristics of the research participants and their levels of knowledge, attitudes, and practice. Knowledge questions were scored so that one option was considered the correct answer to yield a score of either11 for a correct answer or11 for a wrong answer. Attitudes and practices questions were scored in the direction that implies a positive attitude or practice towards each question. Pearson’s correlation coefficient was calculated to detect any significant correlations between knowledge, attitudes, and practices scores at the p < 0.05 level. One-way ANOVA and post hoc analysis were used to detect any significant differences between knowledge, attitudes, and practices scores at the p < 0.05 level.
Results
An average of 100 electronic responses and 233 paper responses were obtained and statistically analyzed (it was not feasible to calculate the response rate, as the questionnaire link was distributed through social media platforms). The general characteristics of the research participants are listed in Table 1. Around two-thirds of the study participants were in the age group of 25–49 years (n=220, 66.1%). Female respondents comprised 78.4% (n=261) of the study sample. The highest participation rate was from Amman (n=122, 36.6%), followed by Zarqa (n= 91, 27.3%).
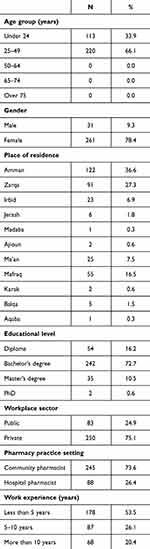 |
Table 1 General Characteristics of the Research Participants |
As shown in Table 2, more than two-thirds of participants (n=257, 77.2%) considered themselves familiar with the term “human microbiome”, and an even higher percentage answered the “most likely description of the human microbiome” question correctly (n=301, 90.4%). When study participants were asked about the factors affecting the composition of the microbiome, the most prevalent answer (n=265, 79.6%) was antibiotics, followed by probiotics (eg, Activia yogurt) (n= 231, 69.4%) and genetics (n= 208, 62.5%). Scores of participants regarding general knowledge of the human microbiome, the role of the human microbiome in health, and the role of the human microbiome in disease are presented in Supplementary Tables 1-3, respectively.
 |
Table 2 Participants’ Responses to Microbiome Knowledge Questions |
According to study participants, the most frequent descriptions of imbalance in gut bacteria were “the decrease in number of beneficial bacteria” (n= 207, 62.2%) and “the increase in number of harmful bacteria” (n= 201, 60.4%). When asked about the leading causes of imbalance in gut bacteria, the most frequent answers were “smoking” and “adopting an unhealthy lifestyle” (equally, 80.5%), followed by “excessive and misuse of antibiotics” (n= 266, 79.9%). “Eating healthy food” was the most prevalent answer to the question on methods for fixing the imbalance in gut bacteria (n=269, 80.8%), followed by “taking pills of beneficial bacteria probiotics” (n=266, 79.9%).
One-way ANOVA test was applied to detect any differences between knowledge, attitude, and practice scores based on the characteristics of the study sample. Participants who were 24 years or less scored significantly lower than participants in the age group of 25 to 49 years in the following scores: general knowledge scores F(1331)=17.5, p=0.00; mean knowledge score on the role of gut bacteria in health F(1331)=4.1, p=0.04; and mean score on attitudes regarding antibiotics, probiotics, and the human microbiome F(1331)=5.1, p=0.02. Also, there was a statistically significant difference between male and female participants in general knowledge scores, F(3329)=3.8, p=0.01, as it was observed that male participants scored significantly higher than female participants.
Furthermore, a statistically significant difference was observed among residents in the different provinces in scores on practices regarding antibiotics, probiotics, and the human microbiome F(10,322)=2.3, p=0.01; however, post hoc analysis could not be executed due to the low number of respondents from some of the included provinces.
Regarding respondents’ attitudes regarding antibiotics, probiotics, and the human gut microbiome, most respondents agreed that it was important to consider the impact of antibiotics on the patient’s microbiome (whether it was a short-term (n=281, 84.3%) or long-term effect (n=257, 77.1%)), and the majority believed in the importance of the human microbiome knowledge for pharmacists and healthcare providers (n=281, 84.4%); however, only 60.9% (n=203) considered themselves well informed regarding the significance of the human microbiome with respect to medical practice, a similar percentage (n=212, 63.6%) felt confident in their knowledge discussing the human microbiome with patients, and more than two-thirds of the respondents (n=249, 74.7%) thought that the human microbiome was too “new” as a field for them to consider how it affected patients’ health. Most respondents agreed that probiotics (n=266, 79.8%) and healthy lifestyle modifications (n=270, 81%) helped restore the balance of “good” and “bad” bacteria in the gut, and 74.7% (n=249) of respondents agreed that they would take probiotic pills after completing an antibiotic course (Figure 1).
 |
Figure 1 Participants’ responses to attitude questions. |
The responses regarding the respondents’ practices regarding antibiotics are shown in Figure 2. Around two-thirds of respondents (n=232, 69.6%) never dispended antibiotics without a prescription, around one-third (n=119, 35.7%), on the other hand, would recommend and dispense antibiotics to patients, friends, and family (without a prescription), and 30.6% (n=102) of respondents would take antibiotics as a precaution so they would not get sick. With respect to respondents’ practices regarding probiotics, over half of those surveyed (n=194, 58.2%) indicated that they would recommend probiotics to patients, friends, and family members (without a prescription), (n= 200, 60%) would give probiotics to their child, (n=211, 63.3%) would give probiotics to an elderly family member, and an even higher percentage (n=227, 68.1%) would personally take probiotics’ pills or consume yogurt to improve their health. Knowledge of the human microbiome was reported to influence respondents’ use and practices toward antibiotics and respondents’ food and lifestyle choices (eg, exercise and sleep habits) by 73.3% (n= 244), 65.1% (n= 217), and 63% (n= 210) of respondents, respectively.
 |
Figure 2 Participants’ responses to practice questions. |
With respect to the levels of knowledge, attitude, and practice scores among the research participants, around 75% (n=250) had a high level of general knowledge regarding the human microbiome (Supplementary Table 4). Almost equal proportions of research participants had either intermediate or high levels of knowledge about the role of gut bacteria in health (n=164, 49.2%) (n=166, 49.8%) respectively, while almost two-thirds had an intermediate level of knowledge of the role of gut bacteria in disease (n=197, 59.2%) (Supplementary Table 4). More than half of the research participants had a positive attitude toward antibiotics, probiotics, and the human microbiome (n=179, 53.8%), and the majority (n=239, 71.8%) had an intermediate level of practice toward the same.
A significant weak positive correlation was found between participants’ knowledge of the role of gut bacteria in health and their attitudes regarding antibiotics, probiotics, and the human microbiome (r=0.186, p < 0.01). Also, a weak positive correlation was found between participants’ knowledge of the role of gut bacteria in disease and their practices regarding antibiotics, probiotics, and the human microbiome (r=0.188, p < 0.01). A significant moderate positive correlation was found between participants’ general knowledge and each of the following: participants’ knowledge of the role of gut bacteria in health (r=0.317, p < 0.01) and attitudes (r=0.306, p < 0.01) and practices (r=0.331, p < 0.01) regarding antibiotics, probiotics, and the human microbiome. Also, a significant moderate positive correlation was found between participants’ knowledge of the role of gut bacteria in health and their practices regarding antibiotics, probiotics, and the human microbiome (r=0.321, p<0.01). Furthermore, a significant strong positive correlation was found between participants’ knowledge of the role of gut bacteria in health and their knowledge of the role of gut bacteria in disease (r=0.591, p<0.01) and between participants’ attitudes regarding antibiotics, probiotics, and the human microbiome and their practices regarding the same (r=0.539. p < 0.01) (Supplementary Table 5).
Discussion
The study provides unique and valuable insights into the impact of pharmacists’ knowledge of the human microbiome and its role in health and disease as an influential factor driving their attitudes and practices regarding antibiotics and probiotics. Here, we present knowledge of the human microbiome as a powerful tool to modulate public and healthcare professionals’ mind-sets regarding their attitudes and practices regarding antibiotics and probiotics. Our results show that the prevalence of self-medication with antibiotics and the propensity to dispense antibiotics without a medical prescription was lower among pharmacists with a higher knowledge score of the human microbiome. Also, pharmacists with higher knowledge scores were also more likely to take or recommend probiotics to patients, friends, and family members (without a prescription).
In addition, the study results show that the higher the score of participants’ knowledge (either general or specific knowledge), the less likely they were to take or dispense antibiotics without a prescription, and the more likely they were to take and recommend probiotics to patients, friends, and family members (without a prescription). Despite the high or intermediate levels of knowledge (either general or specific knowledge) of participants of the human microbiome, correlations of knowledge (either general or specific knowledge) with either pharmacists’ attitudes or practices were either moderately or weakly significant, which might be attributed to a number of impediments, such as the lack of clinical and practice guidelines and regulations (ie, target population, dosing, and counseling) regarding the use of probiotics.
Two of the major behaviors contributing to antibiotic resistance are self-medicating with antibiotics and the propensity to dispense antibiotics without a medical prescription,12,13 especially with the high prevalence rates of self‐medication with antibiotics in Jordan.3 The results of this study indicated that of the 333 participants, around one-third (n=119, 35.7%) would recommend and dispense antibiotics to patients, friends, and family (without a prescription), and a similar proportion (n=102, 30.6%) would take antibiotics as a precaution so they would not get sick. In a study conducted in Jordan in 2021 evaluating community pharmacists’ knowledge of and attitudes toward antibiotic use, resistance, and self-medication, almost all respondents (97%) agreed that community pharmacists were qualified to prescribe antibiotics to patients with bacterial infections, and most respondents (95.2%) practiced antibiotic self-medication.14 Another study conducted in Portugal to investigate factors associated with a propensity to dispense antibiotics without a medical prescription found that agreement with the dispensing of antibiotics without a medical prescription was highest in cases of dental diseases, followed by urinary tract infections.15
Probiotics are still considered over-The-counter medications;16–18 therefore, pharmacists play a great role in dispensing probiotics and shaping public knowledge and awareness regarding them. In the present study, it was found that the higher the score of participants’ knowledge, the more likely they were to take probiotic pills or recommend them to others. This is similar to a study conducted in Jordan in 2019 to evaluate Jordanian healthcare providers’ knowledge, attitudes, and practice patterns toward probiotics, which reported that half of the healthcare professionals included in the study (51.5%) had fair knowledge about probiotics (pediatricians were more knowledgeable), and around 59% of healthcare professionals had positive attitudes toward probiotics. However, only 41% had ever recommended or prescribed them to patients.19 Another regional study conducted in Muscat, Oman, showed that pharmacists have a good background knowledge of probiotics.20
However, these results contrast with the results of other studies conducted earlier in other countries. For example, a study from Nigeria reported limited knowledge of probiotics by healthcare professionals (pharmacists were more knowledgeable).21 Two other studies have also reported limited knowledge of probiotics by healthcare professionals in Lagos State22 and Pakistan.23 Furthermore, in an online international survey that included 1066 health professionals from 30 countries, most respondents evaluated their knowledge of probiotics as medium (36.4%) or good (36.2%), and only 8.9% of respondents rated it as excellent.24 As good knowledge is frequently correlated with positive attitudes and good practices, according to our results, we propose knowledge of the human microbiome as a predictor factor of healthcare professionals’ attitudes and practices regarding antibiotics and probiotics.
Linking healthcare professionals’ knowledge of the human microbiome with their attitudes and clinical practice has been addressed in a few studies in the literature. An online survey distributed in Rhode Island, US, to address the knowledge and opinions of antibiotic prescribing regarding the importance of the human microbiome and its relation to antibiotics and the immune system, found that clinicians considered the health of the human microbiome when prescribing antibiotics; however, they did not feel well informed or confident in their knowledge about the microbiome or its relevance to patient health.25 The study also reported that a higher level of knowledge of the microbiome was associated with the increased importance placed on the microbiome and its relevance to medical practice. Likewise, in this study, most of the participants (n=281, 84.4%) believed in the importance of pharmacists and healthcare providers learning about the human microbiome. However, although a significant proportion of the participants (n=249, 74.7%) believed that the human microbiome was too “new” as a field for them to consider how it affected patients’ health 60.9% (n=203), they considered themselves well informed regarding the significance of the human microbiome with respect to medical practice, and a similar percentage (n=212, 63.6%) felt confident in their knowledge discussing the human microbiome with patients.
Regarding the link between participants’ attitudes and practices regarding antibiotics, probiotics, and the human microbiome, a significant positive strong correlation was found (r=0.539. p < 0.01). This alignment of a high level of knowledge with positive attitudes and practices is not always the case in the literature. Another knowledge, attitude and practices (KAP) survey in Jordan regarding probiotics reported fair knowledge and a positive attitude that did not reflect a positive practice.19
To the best of our knowledge, this study is the first of its kind in Jordan linking pharmacists’ knowledge of the human microbiome to their attitudes and practices regarding antibiotics and probiotics. However, the study had a number of caveats that needed to be noted, including convenience sampling and the low number of respondents from some of the included provinces. Despite convenient sampling, the sample was fairly representative, given that, gender-wise, there are more female pharmacists in Jordan (more females were included in the study sample (78.4%) than males). Also, residency-wise, more pharmacists are situated in the middle governorates compared to north and south (63.9% of respondents were from the middle governorates). In addition, more pharmacists work in the private sector than in the public sector (75.1% of respondents were from the private sector).26 Another limitation of our study is that the data were self-reported and that healthcare professionals may admit less negative attitudes and practices than in which they really engage.
Conclusion
This study highlighted the importance of knowledge of the human microbiome and its role in health and disease for pharmacists, in their attitudes and practices toward antibiotics and probiotics, and in their personal lives regarding food and lifestyle choices, which ultimately reflected positively on knowledge of the general population of the human microbiome, which in turn might help rectify public behaviors leading to antibiotic resistance. Future directions include interventional studies to assess the effect of educating pharmacists (or pharmacy students) of the human microbiome on their attitudes and practices regarding antibiotics and probiotics.
Data Sharing Statement
All data were provided within the manuscript and supplementary tables.
Ethical Approval
Research ethics approval was obtained from the Ethics Committee for Scientific Research at Zarqa University, with approval number (Zu-2023/7/5306/37) prior to conducting the study. Informed consent was collected from participants before they recorded their responses to the questionnaire, while ensuring that participant’s identities were anonymously maintained.
Acknowledgments
The authors would like to thank Zarqa University in Jordan and Princess Nourah bint Abdulrahman University for supporting this research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project was funded by Zarqa University in Jordan and Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R304), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Disclosure
The authors state no conflicts of interest in this work.
References
1. Prados-Bo A, Casino G. How have quality newspapers covered the microbiome? A content analysis of The New York Times, The Times, and El País. Journalism. 2022;14648849211067858.
2. Collier SP, Weldon AJ, Johnson JL. More Than Our Enemy: making Space for the Microbiome in Pharmacy Education. Innova Pharm. 2022;13(1):9. doi:10.24926/iip.v13i1.4553
3. Nusair MB, Al‐azzam S, Alhamad H, et al. The prevalence and patterns of self‐medication with antibiotics in Jordan: a community‐based study. Int J Clin Pract. 2021;75(1):e13665. doi:10.1111/ijcp.13665
4. Abduelkarem AR, Othman AM, Abuelkhair ZR, et al. Prevalence of self-medication with antibiotics among residents in United Arab Emirates. Infect Drug Resist. 2019. 3445–3453. doi:10.2147/IDR.S224720
5. Alghadeer S, Aljuaydi K, Babelghaith S, et al. Self-medication with antibiotics in Saudi Arabia. Saudi Pharm J. 2018;26(5):719–724. doi:10.1016/j.jsps.2018.02.018
6. Merenstein D, Pot B, Leyer G, et al. Emerging issues in probiotic safety: 2023 perspectives. Gut Microbes. 2023;15(1):2185034. doi:10.1080/19490976.2023.2185034
7. González PLVJB, Peinado II. Importance of the Pharmaceutical Council in the Dispensation of Laxants and Probiotics. J Pharm Pharmacol. 2018;6:742–751.
8. Abbas MO, Ahmed H, Hamid E, et al. Pharmacists’ Knowledge, Perception, and Prescribing Practice of Probiotics in the UAE: a Cross-Sectional Study. Antibiotics. 2024;13(10):967. doi:10.3390/antibiotics13100967
9. Sperber AD. Translation and validation of study instruments for cross-cultural research. Gastroenterology. 2004;126:S124–S128. doi:10.1053/j.gastro.2003.10.016
10. Raosoft I, Sample size calculator. Available from: wwwwraosoftcom/samplesize.
11. Tan CC, Moir M, Tegally H, et al. No evidence for a common blood microbiome based on a population study of 9,770 healthy humans. Nature Microbiology. 2023;8:1–13. doi:10.1038/s41564-022-01276-9
12. Bert F, Previti C, Calabrese F, et al. Antibiotics self medication among children: a systematic review. Antibiotics. 2022;11(11):1583. doi:10.3390/antibiotics11111583
13. Machowska A, Stålsby Lundborg C. Drivers of irrational use of antibiotics in Europe. Int J Environ Res Public Health. 2019;16(1):27. doi:10.3390/ijerph16010027
14. Abdel-Qader DH, Albassam A, Ismael NS, et al. Community pharmacists’ knowledge of and attitudes toward antibiotic use, resistance, and self-medication in Jordan. Drugs Therapy Perspect. 2021;37:44–53. doi:10.1007/s40267-020-00797-9
15. Roque F, Soares S, Breitenfeld L, et al. Influence of community pharmacists׳ attitudes on antibiotic dispensing behavior: a cross-sectional study in Portugal. Clin. Ther. 2015;37(1):168–177. doi:10.1016/j.clinthera.2014.11.006
16. Goldstein EJ, Citron DM, Claros MC, et al. Bacterial counts from five over-The-counter probiotics: are you getting what you paid for? Anaerobe. 2014;25:1–4. doi:10.1016/j.anaerobe.2013.10.005
17. Zitvogel L, Derosa L, Kroemer G. Modulation of cancer immunotherapy by dietary fibers and over-The-counter probiotics. Cell Metab. 2022;34(3):350–352. doi:10.1016/j.cmet.2022.02.004
18. Ujaoney S. In vitro effect of over-The-counter probiotics on the ability of Candida albicans to form biofilm on denture strips. American Dental Hygienists’. Association. 2014;88(3):183–189.
19. Ababneh M, Elrashed N, Al-Azayzih A. Evaluation of Jordanian healthcare providers’ knowledge, attitudes, and practice patterns towards probiotics. Expert Rev Pharmac Outc Res. 2020;20(1):93–97. doi:10.1080/14737167.2019.1609354
20. Al-Qysi L, Mohammad M, Al-iedani A, et al. Investigating the characteristics of probiotics marketed in the Middle East and pharmacists’ perception of use in Muscat. Oman PharmaNutrition. 2020;13:100202. doi:10.1016/j.phanu.2020.100202
21. Amarauche CO. Assessing the awareness and knowledge on the use of probiotics by healthcare professionals in Nigeria. J Young Pharm. 2015;8(1):53. doi:10.5530/jyp.2016.1.12
22. Chukwu EE, Nwaokorie F, Yisau J, et al. Assessment of the knowledge and perception of probiotics among medical science students and practitioners in Lagos state. Br J Med Med Res. 2015;5(10):1239. doi:10.9734/BJMMR/2015/13676
23. Arshad MS, Saqlain M, Majeed A, et al. Cross-sectional study to assess the healthcare professionals’ knowledge, attitude and practices about probiotics use in Pakistan. BMJ open. 2021;11(7):e047494. doi:10.1136/bmjopen-2020-047494
24. Fijan S, Frauwallner A, Varga L, et al. Health professionals’ knowledge of probiotics: an international survey. Int J Environ Res Public Health. 2019;16(17):3128. doi:10.3390/ijerph16173128
25. Wilson MH, Mello MJ, Gruppuso PA. Antibiotics and the Human Microbiome: a Survey of Prescribing Clinicians’ Knowledge and Opinions Regarding the Link between Antibiotic-Induced Dysbiosis and Immune-Mediated Disease. Rhode Island Med J. 2021;104(7).
26. Jebreel S, Tarawneh M, Abu-Shaer M, National human resources for health observatory annual report; 2017 Availabe from: http://wwhhcgovjo/uploadedimages/340f3d689059-44d2-b328-1154896f9b8b.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

