Back to Journals » Cancer Management and Research » Volume 17
Impact of Social Determinants on Quality of Life in Socioeconomically Disadvantaged Cancer Survivors: A Mixed-Methods Study
Authors Almutairi M , Almutairi AA, Alodhialah AM
Received 5 January 2025
Accepted for publication 14 March 2025
Published 1 July 2025 Volume 2025:17 Pages 1271—1292
DOI https://doi.org/10.2147/CMAR.S515781
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chien-Feng Li
Mohammed Almutairi,1 Ashwaq A Almutairi,2 Abdulaziz M Alodhialah1
1College of Nursing, Department of Medical-Surgical Nursing, King Saud University, Riyadh, Saudi Arabia; 2School of Nursing & Midwifery, Monash University, Melbourne, Australia
Correspondence: Abdulaziz M Alodhialah, College of Nursing, Department of Medical-Surgical Nursing, King Saud University, Riyadh, Saudi Arabia, Email [email protected]
Background: Socioeconomic disparities significantly impact cancer survivorship, influencing quality of life (QoL) outcomes. This study investigates the role of social determinants of health (SDH) in shaping QoL among socioeconomically disadvantaged cancer survivors in Riyadh City, Saudi Arabia.
Methods: A mixed-methods design was employed, combining quantitative and qualitative approaches. The quantitative component included 200 participants who completed validated SDH and WHOQOL-BREF questionnaires. Pearson’s correlation and multiple regression analyses were conducted to explore relationships between SDH domains and QoL outcomes. The qualitative component involved in-depth interviews with 20 purposively selected participants. Thematic analysis was performed to capture survivors’ experiences and perceptions.
Results: Quantitative findings revealed significant negative correlations between financial instability and QoL domains, particularly physical health (r = − 0.45, p < 0.001). Multiple regression analysis identified financial instability (β = − 0.50, p < 0.001) and lack of social support (β = − 0.28, p < 0.05) as key predictors of reduced QoL. Qualitative findings highlighted three major themes: financial and structural barriers, psychological impacts, and coping mechanisms. Participants reported significant challenges related to healthcare access, fear of recurrence, and social isolation, while emphasizing the importance of family and community support.
Conclusion: SDH significantly influence QoL among socioeconomically disadvantaged cancer survivors. Addressing financial, structural, and social barriers through equity-driven and culturally sensitive interventions is essential to improving survivorship outcomes.
Keywords: social determinants of health, cancer survivorship, quality of life, socioeconomic disparities, Saudi Arabia, mixed-methods, healthcare access
Introduction
Cancer survivorship has emerged as a critical area of focus in contemporary public health and healthcare research.1 As advances in cancer diagnostics and treatments have contributed to increased survival rates, attention has shifted from solely improving survival to enhancing the quality of life (QoL) of survivors.2,3 Quality of life encompasses physical, psychological, social, and functional well-being, which are often disrupted during and after cancer treatment. Among survivors, those from socioeconomically disadvantaged backgrounds experience disproportionately poorer outcomes.4 This disparity highlights the necessity of examining the social determinants of health (SDH) that influence their QoL.5
Social determinants of health are the non-medical factors that influence health outcomes, including education, income, employment, social support, and access to healthcare.6 These determinants are interwoven with structural inequities, which exacerbate vulnerabilities among cancer survivors from lower socioeconomic strata.7 For instance, individuals with limited income or education may face barriers to accessing timely healthcare services, appropriate rehabilitation, or psychosocial support, which are essential for managing the multifaceted consequences of cancer and its treatment.8 These inequities underscore the importance of addressing SDH to improve QoL among socioeconomically disadvantaged populations.9
The association between socioeconomic status (SES) and health outcomes in cancer survivors is well-documented. Low SES is linked to increased risk of late-stage diagnosis, more aggressive cancer subtypes, and higher mortality rates.10 Additionally, survivors with lower SES often encounter financial toxicity, a term used to describe the economic burden of cancer care, which further diminishes their QoL.11 These financial strains are compounded by indirect costs such as loss of income, transportation expenses, and caregiving responsibilities. Consequently, understanding the intersection of SES and QoL is pivotal for designing equitable healthcare interventions.12,13
Psychosocial challenges are another dimension of concern for socioeconomically disadvantaged cancer survivors. Psychological distress, including anxiety, depression, and fear of recurrence, is more prevalent among this group due to compounded stressors such as economic instability and limited social support.14–16 Social isolation, often stemming from reduced mobility, stigma, or role changes within families and communities, further exacerbates these mental health challenges. Addressing these psychosocial barriers requires a multidimensional approach that integrates mental health support into survivorship care plans.17
Access to healthcare is a critical mediator of health disparities among cancer survivors. While advances in cancer care have improved outcomes for many, the unequal distribution of these advances perpetuates disparities.18 Socioeconomically disadvantaged survivors are less likely to receive follow-up care, surveillance for recurrence, or management of late effects. Geographic barriers, insurance coverage gaps, and health literacy also play significant roles in limiting access to essential services.19 The resultant disparities underscore the need for tailored interventions that account for the unique needs of this population.20
Physical well-being, a core component of QoL, is often compromised among socioeconomically disadvantaged cancer survivors. Treatment-related side effects, such as fatigue, pain, and lymphedema, are more likely to persist or worsen in the absence of adequate management.21 Furthermore, comorbidities such as diabetes, hypertension, and obesity are more prevalent in low-SES groups, compounding the physical challenges faced by survivors.22 Physical rehabilitation and lifestyle interventions, which could mitigate these effects, are frequently underutilized due to financial or logistical barriers.23,24
Nutrition and lifestyle factors are also pivotal in influencing QoL outcomes. Socioeconomically disadvantaged survivors often face dietary challenges due to limited access to affordable, nutritious food.25 This contributes to poor nutritional status, which can impair recovery and exacerbate treatment side effects. Similarly, opportunities for physical activity may be constrained by unsafe neighborhoods, lack of recreational spaces, or time demands related to work and caregiving. These lifestyle factors are critical targets for interventions aimed at improving overall well-being.26
From a policy perspective, addressing health inequities among cancer survivors requires a systemic approach. Policies that expand access to healthcare, provide financial support, and promote health literacy are essential for reducing disparities.27 Community-based programs that engage survivors in their care and connect them with social resources have shown promise in enhancing QoL. However, these initiatives must be tailored to the cultural and contextual needs of socioeconomically disadvantaged populations to ensure their effectiveness.28
Cultural factors play a crucial role in shaping social determinants of health (SDH) and survivorship experiences among cancer patients in Saudi Arabia. The strong emphasis on family support and collectivism often provides emotional and financial assistance to survivors, yet it can also lead to stigmatization and reluctance to seek external psychosocial support due to cultural norms surrounding illness disclosure and mental health concerns.7 Additionally, gender roles may impact healthcare access, as women, particularly those from lower socioeconomic backgrounds, may face mobility restrictions or limited decision-making autonomy in seeking medical care.29 Moreover, the centralized nature of specialized cancer care in major cities like Riyadh creates geographical and financial barriers for rural patients, exacerbating healthcare disparities.30 To mitigate these inequities, Saudi healthcare policies have introduced initiatives such as the National Cancer Control Program, which aims to expand oncology services to underserved regions, improve early detection, and integrate financial assistance programs for low-income patients.31 Further policy-driven interventions, including culturally tailored survivorship programs and community-based support networks, could enhance accessibility and address the unique sociocultural challenges faced by disadvantaged cancer survivors in Saudi Arabia.
This study aims to address these research gaps by investigating the social determinants of health and their influence on QoL outcomes among socioeconomically disadvantaged cancer survivors. Using a mixed-methods approach, this research seeks to identify key barriers and facilitators that shape survivors’ experiences and outcomes. By integrating quantitative and qualitative data, this study will provide a holistic understanding of the challenges faced by this population and inform targeted interventions.
Materials and Methods
Study Design
This study employed a convergent parallel mixed-methods design, in which quantitative and qualitative data were collected simultaneously, analyzed separately, and integrated during interpretation. The rationale for using this design was to provide a comprehensive understanding of the impact of social determinants of health (SDH) on quality of life (QoL) among socioeconomically disadvantaged cancer survivors by combining statistical associations with in-depth personal experiences. The quantitative component included survey-based assessments using validated tools (WHOQOL-BREF and SDH questionnaires), while the qualitative component involved semi-structured interviews to explore survivors’ lived experiences. After independent data analysis—statistical analysis for the quantitative data and thematic analysis for the qualitative data—the findings were merged in the discussion and integration phase to identify areas of convergence, divergence, and complementarity. This approach ensured that the qualitative insights provided contextual depth to the quantitative trends, reinforcing the validity of the findings and offering a holistic perspective on survivorship challenges.
Study Setting
The research was conducted in healthcare centers and hospitals affiliated with King Saud University in Riyadh City. These institutions were chosen due to their accessibility to diverse patient populations, including individuals from lower socioeconomic strata. The facilities provide a range of oncology and survivorship care services, making them ideal for recruiting participants who have experienced varying levels of socioeconomic challenges. Riyadh City, as a major urban center, offers a representative cross-section of Saudi Arabia’s socioeconomic diversity, enhancing the study’s relevance and generalizability.
Sampling and Sample Size
The study employed a purposive sampling technique for both the quantitative and qualitative components to ensure the inclusion of participants whose experiences and characteristics were relevant to the research objectives. This method allowed for the strategic selection of individuals who could provide valuable insights into the relationship between social determinants of health (SDH) and quality of life (QoL) outcomes among socioeconomically disadvantaged cancer survivors.
Quantitative Sample
The quantitative component aimed to enroll 200 participants, a sample size determined through statistical power calculations to ensure the study could detect significant associations between SDH and QoL. These calculations assumed a medium effect size, a significance level of 0.05, and a power of 80%, with adjustments made for potential attrition or incomplete data. This sample size was deemed sufficient to conduct multivariate analyses while accounting for the potential influence of confounding variables such as age, gender, cancer type, and duration of survivorship.
Recruitment Strategy
Participants were recruited during routine follow-up visits to hospitals and healthcare centers affiliated with King Saud University. Recruitment took place in oncology clinics, survivorship programs, and primary care units where cancer survivors regularly sought post-treatment care. The research team collaborated with healthcare providers to identify eligible participants who met the inclusion criteria. Eligible participants were approached in waiting areas or consultation rooms and provided with detailed information about the study’s purpose, procedures, and voluntary nature.
Inclusion Criteria
Adults aged 18 years or older.
- Diagnosed with any type of cancer and had completed primary treatment at least six months before participation.
- Self-identified as socioeconomically disadvantaged, based on income, education level, or self-reported financial hardship.
Fluent in Arabic.
Willingness to complete self-administered questionnaires.
Exclusion Criteria
Participants currently undergoing active cancer treatment.
- Individuals with severe cognitive impairments or mental health conditions that precluded informed consent or participation.
Sample Diversity
Efforts were made to ensure the sample was representative of the broader socioeconomically disadvantaged cancer survivor population in Riyadh. This included recruiting individuals from various demographic and clinical backgrounds, such as different age groups, cancer types, and treatment modalities. Participants were also selected from diverse geographic areas within Riyadh to capture potential variations in access to healthcare and support systems.
Qualitative Sample
The qualitative phase involved the purposive selection of 20 participants from the quantitative cohort. The sample size was guided by the principle of data saturation, which occurs when additional data no longer yield new themes or insights. This approach ensured the collection of rich, in-depth information while maintaining methodological rigor.
Selection Criteria
Participants for the qualitative interviews were selected based on the following criteria:
Diversity in socioeconomic characteristics, such as income level, education, and employment status.
- Variation in clinical factors, including cancer type, stage at diagnosis, and time since treatment completion.
Willingness to share detailed personal experiences regarding SDH and QoL.
- Representation of different responses to the quantitative survey, particularly those who reported higher or lower QoL scores, to explore a range of perspectives.
Recruitment Process
Potential participants were identified during the analysis of the quantitative data. Those meeting the selection criteria were contacted by phone or in person, depending on their preference, and invited to participate in the qualitative interviews. The research team explained the purpose of the interviews, the confidentiality measures in place, and the importance of their contributions to the study. Written consent was obtained from participants who agreed to take part.
Sample Diversity and Representativeness
The qualitative sample aimed to reflect the heterogeneity of the larger quantitative cohort. Participants were selected to capture a broad spectrum of experiences and challenges, including those related to financial barriers, social support systems, and healthcare access. Special attention was given to including individuals with unique or extreme cases, such as those facing significant financial hardship or those with exceptional resilience in the face of adversity, to enrich the dataset.
Data Saturation
Data saturation was monitored throughout the interview process. The research team conducted interviews iteratively, analyzing the data after each round to identify emerging themes and determine whether new interviews were adding unique insights. Saturation was achieved after 20 interviews, as no new themes or subthemes emerged from the data.
Justification of Sample Size
While 20 participants might seem modest, this number aligns with qualitative research standards, particularly for studies employing thematic analysis. The small, focused sample allowed for in-depth exploration of participants’ experiences while ensuring manageable data analysis. The insights gained from this sample size complemented the broader quantitative findings, providing a comprehensive understanding of the issues under investigation.
Data Collection Tools
Quantitative Component
Social Determinants of Health Questionnaire (SDHQ)
The Social Determinants of Health Questionnaire (SDHQ) was employed to comprehensively assess the socio-economic factors influencing participants’ quality of life (QoL). This tool evaluates domains such as income, education, employment status, housing, social support, and access to healthcare services.32 The questionnaire comprises 25 items designed to capture participants’ perceptions of how these factors impact their daily lives and health outcomes. Each item is scored on a 5-point Likert scale, where 1 indicates “Strongly Disagree” and 5 indicates “Strongly Agree”. Higher scores reflect greater perceived challenges related to the specific domains of social determinants.
The SDHQ was developed and validated through extensive testing in diverse populations, ensuring its reliability and applicability in capturing social determinants of health. The tool demonstrated robust psychometric properties, with a Cronbach’s alpha of 0.85 in pilot testing conducted with 20 participants from the target demographic. This indicates excellent internal consistency across the domains. Additionally, content validity was established by an expert panel comprising public health professionals, oncologists, and social scientists, who confirmed the relevance and comprehensiveness of the items.
For this study, the SDHQ was translated into Arabic and culturally adapted following established guidelines for cross-cultural research. The adaptation process included forward and backward translation, followed by pilot testing to ensure clarity and cultural appropriateness of the items. Minor modifications were made to contextualize specific terms related to healthcare access and social support within the Saudi Arabian setting. The Arabic version maintained the reliability of the original tool, with a Cronbach’s alpha of 0.87 in the adapted version.
Quality of Life Scale (WHOQOL-BREF)
The World Health Organization Quality of Life-BREF (WHOQOL-BREF) was used to evaluate participants’ QoL. This standardized instrument assesses four key domains: physical health, psychological well-being, social relationships, and environmental factors. The physical health domain examines aspects such as energy levels, mobility, and daily activities, while the psychological domain evaluates emotional well-being, self-esteem, and mental health. Social relationships encompass personal relationships and social support, whereas the environmental domain includes factors such as safety, financial resources, and access to healthcare.
The WHOQOL-BREF consists of 26 items, each rated on a 5-point Likert scale, where 1 indicates the lowest level of satisfaction or functionality and 5 indicates the highest. The scores for each domain are transformed into a scale ranging from 0 to 100, with higher scores reflecting better quality of life. The instrument has been widely used globally and is recognized for its robust psychometric properties.
The Arabic version of the WHOQOL-BREF, which has been validated in several Arabic-speaking populations, was employed in this study to ensure cultural and linguistic relevance. The translation and adaptation process followed the WHO guidelines for instrument adaptation, including expert review and field testing.33 The Arabic version demonstrated strong reliability, with Cronbach’s alpha values exceeding 0.80 for all domains in previous studies. Pilot testing with 20 participants from the current study yielded a Cronbach’s alpha of 0.82, further confirming its reliability in the local context.
Qualitative Component
Semi-Structured Interview Guide
The semi-structured interview guide was developed to explore participants’ lived experiences and perceptions of the impact of social determinants on their QoL. The guide was informed by an extensive review of the literature on social determinants of health and survivorship care, ensuring that the questions addressed relevant and context-specific issues.
The guide included open-ended questions and prompts designed to elicit detailed narratives about participants’ challenges and coping strategies. Examples of questions included:
“How have socioeconomic factors influenced your cancer care journey?”
“What challenges have you faced in maintaining your quality of life after cancer treatment?”
“Can you describe any support systems or resources that have helped you navigate these challenges?”
“What improvements in healthcare or social support systems would help enhance your quality of life?”
The guide was structured to allow flexibility, enabling interviewers to probe further based on participants’ responses. This approach ensured that the interviews captured rich, nuanced data while remaining focused on the study’s objectives.
The interview guide underwent expert review by a multidisciplinary panel, including healthcare providers, social scientists, and cancer survivors, to ensure its relevance and comprehensiveness. It was then pilot tested with five participants to refine the questions for clarity and cultural appropriateness. Feedback from the pilot study led to minor adjustments, such as rephrasing questions to align with local terminologies and sensitivities.
All interviews were conducted in Arabic to ensure participants’ comfort and ease of expression. Interviews were audio-recorded with participants’ consent and supplemented with field notes to capture non-verbal cues and contextual details. Transcripts were translated into English for analysis while retaining the original Arabic for validation purposes.
Data Collection Procedure
Quantitative Data Collection
Quantitative data collection took place over two months at King Saud University-affiliated hospitals and healthcare centers in Riyadh City. Before initiating the process, the research team conducted training sessions for research assistants to ensure a clear understanding of the study’s objectives, data collection tools, and ethical considerations. Research assistants practiced through mock sessions to simulate real-life scenarios. Arabic versions of the Social Determinants of Health Questionnaire and WHOQOL-BREF were prepared and piloted with five participants to ensure clarity and cultural relevance. Minor adjustments were made based on the pilot feedback.
Participants were recruited during routine visits to outpatient oncology clinics and survivorship care centers. Healthcare providers assisted in identifying eligible participants, who were then approached by the research team and briefed about the study’s purpose, confidentiality measures, and voluntary nature. After obtaining informed consent, participants completed the questionnaires in private rooms to ensure a quiet and confidential environment. Research assistants were available to assist participants with low literacy or physical impairments by reading questions aloud and recording their responses verbatim. Completing the questionnaires took approximately 20–30 minutes.
To maintain data quality, research assistants reviewed completed questionnaires to ensure clarity and completeness, addressing any missing or unclear responses immediately with the participant. The completed questionnaires were securely stored in locked cabinets, and data were later digitized and double-checked for accuracy during the electronic entry process. Participants were thanked for their involvement and provided with information about available support services if needed. This structured process ensured efficient and reliable quantitative data collection while respecting participant comfort and confidentiality.
Qualitative Data Collection
The qualitative phase commenced one week after the quantitative phase and lasted for two months. Twenty participants were purposively selected from the quantitative cohort based on their willingness to participate and diversity in socioeconomic and clinical characteristics. This approach ensured a broad range of perspectives and experiences. Participants were contacted via telephone to schedule interviews at their preferred time and location, with options for healthcare centers or their homes. Flexibility in scheduling aimed to accommodate participants’ comfort and convenience.
Interviews followed a semi-structured format, guided by an interview protocol developed from a review of relevant literature. Open-ended questions allowed participants to share their experiences freely, while follow-up prompts encouraged elaboration. Questions included, “Can you describe how financial challenges have impacted your quality of life after cancer treatment?” and “What support, if any, have you received from your community or family, and how has this influenced your recovery?” Interviews were conducted in Arabic and lasted 45–60 minutes, ensuring sufficient time for participants to articulate their thoughts.
All interviews were audio-recorded with participants’ consent, and detailed field notes were taken to capture non-verbal cues and contextual observations. Audio recordings were transcribed verbatim in Arabic and later translated into English for thematic analysis. Transcripts were reviewed against field notes to ensure accuracy. Pseudonyms were used, and identifying information was excluded to maintain confidentiality. The interviews continued until data saturation was achieved, which occurred after 20 interviews when no new themes emerged.
To ensure trustworthiness, member checking was performed by sharing summarized findings with a subset of participants to confirm the authenticity of the interpretations. This detailed and participant-centered approach ensured that the qualitative data collection was comprehensive, culturally sensitive, and ethically sound, providing rich insights into the lived experiences of socioeconomically disadvantaged cancer survivors.
Integration of Results
To ensure a comprehensive understanding of the relationship between social determinants of health (SDH) and quality of life (QoL) among socioeconomically disadvantaged cancer survivors, the study employed a convergent parallel mixed-methods approach, integrating both quantitative and qualitative findings. The quantitative results highlighted statistically significant associations between financial instability, lack of social support, and reduced QoL scores across physical, psychological, and social well-being domains. These numerical findings were complemented by qualitative insights, where participants described the emotional, social, and financial struggles that impacted their daily lives and ability to maintain post-treatment care. The integration of these data provided a richer, more nuanced perspective on survivorship challenges, bridging the gap between statistical correlations and lived experiences.
A key area of convergence was the strong correlation between financial instability and lower QoL, which was reinforced by qualitative narratives detailing survivors’ struggles with affording medical care, transportation, and daily necessities. Additionally, while the quantitative data demonstrated that low social support was a significant predictor of poor QoL, qualitative findings deepened this understanding, revealing cultural barriers that discouraged seeking external support and exacerbated social isolation. In contrast, areas of divergence emerged in psychological well-being—although quantitative scores indicated moderate psychological distress, qualitative interviews revealed heightened fear of recurrence, stigma-related stress, and emotional exhaustion, suggesting that standard survey measures may underestimate the depth of psychological burden. These complementary insights underscore the importance of integrating statistical patterns with patient narratives to develop culturally and contextually tailored interventions that address both the structural and personal dimensions of survivorship care.
Data Analysis
The analysis of data in this study followed a systematic and integrated approach to address the research objectives comprehensively. For the quantitative component, data from the Social Determinants of Health Questionnaire and the WHOQOL-BREF were analyzed using SPSS software (Version 26). The data underwent a rigorous cleaning process to identify and address missing or inconsistent entries. Missing data were handled using multiple imputation techniques, ensuring that the statistical analyses remained robust and unbiased. Descriptive statistics were calculated to summarize the demographic characteristics of the participants and the distribution of key variables, including income levels, educational attainment, employment status, and QoL scores across the physical, psychological, social, and environmental domains. Means, standard deviations, frequencies, and percentages were reported to provide a detailed overview of the dataset.
To explore the relationships between social determinants of health and quality of life outcomes, inferential statistical analyses were performed. Pearson’s correlation coefficient was used to examine the linear relationships between continuous variables, such as income levels and overall QoL scores. Chi-square tests were employed to assess associations between categorical variables, such as employment status and access to healthcare services. Multiple linear regression analysis was conducted to identify the most significant predictors of QoL among the study population. The regression model included key demographic and socioeconomic variables such as age, gender, educational attainment, income, and type of cancer, allowing for adjustments to control potential confounders. A p-value of less than 0.05 was considered statistically significant, and all results were interpreted with respect to the broader context of socioeconomically disadvantaged cancer survivors.
For the qualitative component, a thematic analysis was conducted to extract meaningful insights from the semi-structured interview data. The analysis began with a detailed familiarization process, where transcripts were read multiple times to immerse the research team in the content and context of the participants’ narratives. Initial coding involved highlighting key phrases, expressions, and concepts that captured participants’ experiences with social determinants of health and their perceived impacts on quality of life. Codes were systematically organized into categories, which were then grouped into broader themes that reflected recurring patterns and significant issues raised by participants. Examples of identified themes included “economic barriers to healthcare access”, “social support as a coping mechanism”, and “perceived inequities in healthcare delivery”.
Throughout the thematic analysis, the research team employed strategies to enhance the rigor and trustworthiness of the findings. Member checking was conducted by sharing preliminary interpretations with a subset of participants to validate the accuracy and resonance of the themes with their lived experiences. Peer debriefing sessions were held to discuss and refine the coding framework, ensuring consistency and alignment with the research objectives. An audit trail documented all analytical decisions, providing transparency and replicability in the qualitative analysis process. Data triangulation was achieved by comparing themes from qualitative interviews with patterns observed in the quantitative data, enriching the depth and validity of the overall findings.
The integration of quantitative and qualitative findings was performed during the interpretation phase. Quantitative results provided a broad overview of the relationships between social determinants of health and quality of life, while qualitative narratives offered nuanced explanations for these relationships. Together, these analyses generated a comprehensive understanding of the complex interplay between socioeconomic factors and QoL among cancer survivors, enabling the formulation of targeted recommendations for improving survivorship care in socioeconomically disadvantaged populations.
Rigour and Trustworthiness
Ensuring rigour and trustworthiness was a critical aspect of this study, particularly given the mixed-methods design. The principles of credibility, dependability, transferability, and confirmability guided the approach to enhancing the quality and reliability of both the quantitative and qualitative components.
Quantitative Component
Instrument Validity and Reliability
- The tools used for data collection, including the Social Determinants of Health Questionnaire and the WHOQOL-BREF, were validated instruments with demonstrated reliability in prior research. The Arabic versions of these tools were used to ensure cultural and linguistic appropriateness.
- A pilot study with 10 participants from the target population was conducted to test the clarity and applicability of the instruments. Feedback was used to refine the tools where necessary.
- Internal consistency of the instruments was assessed using Cronbach’s alpha. Both the Social Determinants of Health Questionnaire and the WHOQOL-BREF showed high reliability, with alpha values exceeding 0.85, indicating strong internal consistency.
Standardized Procedures
- Data collection protocols were standardized, with detailed instructions provided to research assistants to minimize variability in how questionnaires were administered.
- Training sessions for the research team emphasized ethical considerations, consistency in participant engagement, and thoroughness in data verification.
Data Verification
- Each completed questionnaire was reviewed for completeness and accuracy at the point of collection. Missing or unclear responses were addressed immediately with the participant where feasible.
- Double data entry was implemented to reduce the risk of errors during digitization. Discrepancies between entries were resolved by cross-referencing with the original questionnaires.
Qualitative Component
Credibility
- Prolonged engagement with participants was ensured by spending adequate time during interviews to build rapport and encourage open, honest sharing of experiences.
- Member checking was employed as part of the analysis process. Participants were invited to review preliminary interpretations of their interviews to confirm the accuracy and authenticity of the findings.
- Triangulation was achieved by integrating data from multiple sources, including interview transcripts, field notes, and observations, to strengthen the depth and breadth of insights.
Dependability
- An audit trail was maintained to document all methodological decisions, data collection procedures, and analysis processes. This ensured transparency and allowed for replication of the study by future researchers.
- A peer debriefing process involved discussing emerging themes and interpretations with colleagues and experts in qualitative research to ensure consistency and agreement on findings.
Transferability
- Detailed descriptions of the study context, participant demographics, and data collection settings were provided to enable other researchers to evaluate the applicability of the findings to similar populations or contexts.
- Purposive sampling ensured diverse perspectives within the qualitative sample, enhancing the richness of the data and its potential relevance across different subgroups of socioeconomically disadvantaged cancer survivors.
Confirmability
- Reflexivity was maintained throughout the study. The researchers kept reflexive journals to document their assumptions, biases, and potential influences on data interpretation. This practice helped minimize subjectivity and ensured that findings were grounded in the participants’ experiences.
- Independent coding was conducted by multiple researchers to ensure that the themes identified were not influenced by individual biases. Discrepancies in coding were resolved through consensus discussions.
Data Saturation
- Data saturation was reached when no new themes or insights emerged from the interviews, ensuring a comprehensive understanding of participants’ experiences. This was closely monitored by the research team, and additional interviews were conducted if required to achieve saturation.
Mixed-Methods Integration
Triangulation
- Triangulation of quantitative and qualitative findings provided a multidimensional understanding of the influence of social determinants on QoL. Themes from the qualitative analysis were cross-referenced with statistical patterns identified in the quantitative data to ensure coherence and complementarity.
Integration Workshops
- The research team conducted workshops to integrate and synthesize findings from both study components. This collaborative effort allowed for the reconciliation of discrepancies and the formulation of cohesive conclusions.
By employing these strategies, the study ensured the rigour and trustworthiness of its findings, offering robust evidence to inform policy and practice interventions aimed at improving QoL outcomes for socioeconomically disadvantaged cancer survivors.
Ethical Considerations
Ethical approval was obtained from the Institutional Review Board of King Saud University (IRB No. 24.971). Participants provided written informed consent and were assured of confidentiality and the right to withdraw at any time. Data were anonymized, securely stored, and used solely for research purposes. Participants received a debriefing at the study’s conclusion, offering resources for further support. All participants provided written informed consent, including consent for the publication of anonymized responses and direct quotes in the study.
Results
Demographic Characteristics
A total of 200 socioeconomically disadvantaged cancer survivors participated in the quantitative component of this study (Table 1). The sample included a wide age range, with a mean age of 54.7 years, reflecting the diverse age distribution of cancer survivors in Riyadh City. The majority of participants were female (68%), consistent with gender disparities often observed in cancer survivorship populations, where women are more likely to engage in follow-up care and participate in studies. Educational levels showed a predominance of participants with no formal education or secondary education, highlighting the socioeconomic challenges faced by this group. Employment data revealed a high prevalence of unemployment (78%), further emphasizing the financial hardships experienced by the participants. Income levels showed that more than half of the participants earned less than 5000 SAR per month, underscoring the financial vulnerability of this population.
 |
Table 1 Demographic Characteristics (n = 200) |
Social Determinants of Health Scores
Social determinants of health (SDH) were assessed using a validated questionnaire. Participants reported high levels of financial instability, healthcare access barriers, and social support deficits, with financial instability being the most significant challenge (mean = 30.1). These scores indicate systemic barriers faced by socioeconomically disadvantaged cancer survivors. The percentage of participants reporting high concern (≥4 on the Likert scale) for each subdomain was notable, particularly for financial instability (80%). These findings underscore the profound influence of financial and structural barriers on the well-being of cancer survivors (Table 2).
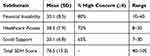 |
Table 2 Social Determinants of Health Scores (n = 200) |
Quality of Life Outcomes
Quality of life (QoL) was measured across four domains using the WHOQOL-BREF. The findings reveal substantial challenges in physical health, which scored the lowest among the domains, reflecting the lingering physical impacts of cancer and its treatment. Psychological health and social relationships also scored moderately low, suggesting the emotional toll and reduced social interactions associated with financial and healthcare access barriers. Interestingly, the environmental domain scored relatively higher, possibly indicating a better perception of the participants’ living environment compared to other aspects of their lives (Table 3).
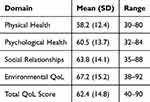 |
Table 3 Quality of Life Scores (n = 200) |
Correlation Analysis
The relationship between SDH and QoL was explored using Pearson’s correlation coefficient. Significant negative correlations were observed between SDH scores and QoL domains, particularly physical and psychological health. Financial instability demonstrated the strongest correlation with reduced QoL, emphasizing its pervasive impact. These correlations underscore the interconnectedness of socioeconomic barriers and QoL outcomes, highlighting the need for targeted interventions to address these challenges (Table 4).
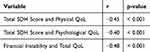 |
Table 4 Correlation Analysis (n = 200) |
Regression Analysis
A multiple linear regression model identified key predictors of QoL. The total SDH score was the strongest predictor, with higher scores associated with lower QoL. Income level and education emerged as significant positive predictors, suggesting that improving these factors could enhance QoL outcomes. Interestingly, age and gender were not significant predictors, indicating that socioeconomic factors may have a more direct influence on QoL in this population (Table 5).
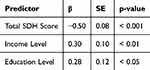 |
Table 5 Regression Analysis Predicting QoL (n = 200) |
Subgroup Analysis
Subgroup analysis revealed significant differences in QoL scores based on gender and income levels. Women reported lower QoL scores compared to men, reflecting additional challenges such as caregiving roles or gender-related barriers. Participants with low income also reported significantly lower QoL, emphasizing the financial burden as a key determinant of well-being. These findings highlight the heterogeneity within the population and the need for tailored interventions (Table 6).
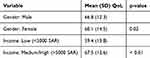 |
Table 6 Subgroup Analysis of QoL Scores |
Qualitative Findings
In-depth interviews revealed the complexities of socioeconomically disadvantaged cancer survivors’ experiences (Table 7). Three primary themes emerged: (i) financial and structural barriers, (ii) emotional and psychological impacts, and (iii) coping and support mechanisms. These themes illustrate the interplay of external and internal challenges faced by participants and their strategies to navigate survivorship.
 |
Table 7 Thematic Analysis of Qualitative Findings |
Financial and Structural Barriers
Participants described a range of financial and structural obstacles that exacerbated their difficulties in accessing healthcare and maintaining their quality of life. Two key subthemes were identified: cost of care and healthcare access barriers.
Cost of Care
Financial constraints emerged as a pervasive challenge, with participants expressing concerns over the affordability of routine check-ups, medications, and follow-up care. Many participants noted that their financial situation forced them to make difficult choices between healthcare and basic living expenses.
I have to think twice before scheduling a follow-up appointment because even the transportation cost is a burden. Medication is another story—I just can’t afford it all the time. (Participant 1)
Cancer is not just a disease; it’s a financial disaster. Sometimes I skip my appointments because I don’t have the money for the tests. (Participant 9)
Healthcare Access Barriers
Logistical issues, such as long travel distances and limited availability of specialized oncology services, were frequently cited as significant impediments. Participants living in underserved areas faced particular challenges in accessing timely care.
The hospital is far from my home, and I have to rely on someone to take me. Most times, they are busy, so I miss my appointments. (Participant 4)
The clinic near my house doesn’t provide the services I need. I have to go to the main hospital, which is a long and tiring journey. (Participant 7)
These financial and structural barriers not only delayed critical follow-ups but also contributed to feelings of frustration and helplessness among participants.
Emotional and Psychological Impacts
The psychological toll of cancer survivorship was another dominant theme. Participants shared their struggles with fear, anxiety, and emotional distress, which often compounded their physical and financial challenges.
Fear of Recurrence and Mortality
Participants expressed ongoing anxiety about the possibility of cancer recurrence or progression. This fear influenced their decisions to avoid or delay follow-ups, reflecting a protective but counterproductive behavior.
I am terrified every time I think about going to the hospital. What if they find something again? I don’t think I can go through it all over again. (Participant 3)
Sometimes, it feels like ignorance is bliss. If I don’t know, I don’t have to deal with the pain and worry. (Participant 10)
Emotional Exhaustion and Depression
Feelings of emotional fatigue and despair were prevalent, particularly among participants who lacked robust support systems. Survivors often described their cancer journey as isolating and mentally draining.
I feel like I’m carrying this burden alone. It’s exhausting, both physically and mentally. Some days, I don’t even want to get out of bed. (Participant 6)
The stress of thinking about my health and my finances is overwhelming. It feels like there’s no escape. (Participant 11)
These emotional and psychological impacts highlighted the need for integrated mental health support in survivorship care.
Coping and Support Mechanisms
Despite the challenges, participants demonstrated resilience through various coping strategies and sought support from family, friends, and community resources. Two subthemes emerged: family involvement and self-reliance.
Family Involvement
Participants who received consistent emotional and practical support from their families reported a better ability to cope with the aftermath of cancer treatment. However, the level of support varied widely.
My daughter helps me with everything—from managing my appointments to making sure I take my medicine on time. I don’t know what I’d do without her. (Participant 2)
I feel lucky to have my family around. They give me the strength to keep going, even on the bad days. (Participant 8)
Conversely, some participants noted a lack of family involvement, which exacerbated their sense of isolation.
My family doesn’t understand what I’m going through. They think everything is fine now that I’ve finished treatment, but it’s far from over. (Participant 12)
Self-Reliance and Community Resources
Several participants emphasized the importance of self-reliance and the use of community resources, such as support groups and non-profit organizations, in managing their post-treatment challenges.
I joined a local cancer support group, and it has made a big difference. Talking to people who understand what I’m going through is comforting. (Participant 5)
When I feel low, I try to focus on the things I can control, like eating healthy and walking every day. It’s not much, but it helps me stay positive. (Participant 9)
These coping mechanisms underscored the importance of fostering community-based interventions and creating accessible resources to empower survivors.
To enhance the integration of qualitative and quantitative findings, Table 8 and Figure 1 illustrates how qualitative themes support, complement, or explain the numerical trends identified in the quantitative analysis. This comparison reinforces the mixed-methods approach by contextualizing statistical associations with survivor narratives, offering a more holistic understanding of how social determinants impact cancer survivorship outcomes.
 |
Table 8 Integration of Quantitative and Qualitative Findings |
 |
Figure 1 Conceptual model to visualize how qualitative data contextualizes quantitative associations between SDH and QoL. |
Discussion
This study explored the influence of social determinants of health (SDH) on the quality of life (QoL) among socioeconomically disadvantaged cancer survivors in Riyadh City, Saudi Arabia, using a mixed-methods approach. The findings reveal significant associations between SDH and QoL domains, highlighting the compounded challenges faced by this population in navigating survivorship. These results underscore the critical need for integrated, equity-driven approaches to improve health outcomes and QoL among disadvantaged survivors.
The Influence of Financial Instability
Financial instability emerged as a predominant barrier, with participants reporting significant challenges in affording medical care, transportation, and basic needs.34 The quantitative findings demonstrated a strong negative correlation between financial instability and QoL, consistent with previous research indicating that economic strain adversely impacts cancer survivors’ physical and psychological well-being. Financial toxicity, defined as the economic burden associated with cancer care, has been widely documented as a critical factor influencing survivors’ ability to adhere to follow-up treatments and maintain overall health.35 These findings align with studies showing that financial distress exacerbates emotional exhaustion and reduces access to necessary healthcare services, further compounding disparities in outcomes.36
The qualitative data further contextualized these barriers, with participants describing the daily struggles of balancing medical expenses against household priorities. Participants noted that they often delayed or avoided follow-up care due to cost concerns, which is consistent with global evidence suggesting that financial strain leads to delayed diagnosis, poorer treatment adherence, and worsened outcomes.37 Addressing financial barriers requires not only systemic policy interventions but also targeted programs that provide financial assistance and facilitate access to affordable care.38
Healthcare Access Challenges
Barriers to accessing healthcare facilities were another prominent theme. Quantitative data indicated that healthcare access scores were significantly associated with QoL, emphasizing the critical role of accessibility in survivorship outcomes.39 Survivors in this study reported logistical challenges, including long distances to specialized oncology centers and limited availability of local services, which hinder their ability to receive timely care.
These findings are consistent with research demonstrating that geographic and structural barriers disproportionately affect socioeconomically disadvantaged populations.40 Limited access to comprehensive cancer care services often leads to reliance on emergency care or the postponement of necessary follow-ups, both of which can have deleterious effects on survivorship.41 Participants in the qualitative component shared similar concerns, with many highlighting the lack of nearby facilities equipped to manage their long-term care needs. These challenges reflect broader systemic inequities in healthcare delivery, necessitating a reconfiguration of service distribution to prioritize underserved areas.42
Emotional and Psychological Impacts
The emotional and psychological toll of cancer survivorship was another critical finding. Fear of recurrence, anxiety, and emotional exhaustion emerged as significant barriers to maintaining QoL.43 Quantitative data demonstrated significant associations between psychological health scores and SDH, particularly financial instability and lack of social support. This aligns with previous studies that underscore the heightened vulnerability of socioeconomically disadvantaged survivors to psychological distress due to the compounded burden of financial, social, and health-related challenges.44
Qualitative findings provided deeper insights into these psychological impacts, revealing the pervasive influence of fear and denial on survivors’ health-seeking behaviors. Many participants expressed reluctance to engage in follow-up care due to fear of receiving bad news, a phenomenon commonly reported in cancer survivorship literature. This avoidance behavior not only delays early detection of recurrence but also amplifies emotional distress, creating a vicious cycle that further compromises QoL.45 Effective psychological interventions, such as counseling and survivorship support programs, are essential to address these barriers and enhance mental well-being among disadvantaged survivors.46
The Role of Social Support
Social support emerged as a significant protective factor in QoL outcomes, with both quantitative and qualitative findings highlighting its critical role. Participants with robust familial and community support reported better coping mechanisms and a greater ability to navigate survivorship challenges. Conversely, the absence of social support was associated with feelings of isolation, depression, and reduced QoL. These findings echo existing research demonstrating that social networks and support systems play a pivotal role in mitigating the psychological and practical burdens of cancer survivorship.47
However, cultural attitudes and stigma surrounding illness and vulnerability emerged as significant barriers to seeking support.48,49 Participants described societal norms that discouraged open discussions about health challenges, leading to a lack of acknowledgment and understanding of their needs. Such cultural dynamics are well-documented in Middle Eastern contexts, where familial obligations and societal expectations often intersect to influence health behaviors.50 Community-based interventions that address cultural stigmas and foster supportive environments are crucial to bridging these gaps and enhancing survivorship care.51
Physical Health Challenges
Physical health was the most compromised QoL domain in this study, with survivors reporting persistent fatigue, pain, and treatment-related side effects. These findings align with previous research highlighting the long-term physical consequences of cancer and its treatment, particularly among socioeconomically disadvantaged populations who may have limited access to rehabilitation services52–55 The strong association between SDH and physical health underscores the interconnectedness of financial, logistical, and social barriers in shaping physical outcomes.56
Participants in the qualitative interviews emphasized the challenges of managing comorbidities and the limited availability of resources for physical rehabilitation. These findings are consistent with global evidence indicating that socioeconomically disadvantaged populations face a higher prevalence of comorbid conditions and reduced access to preventive and rehabilitative care.57 Addressing these challenges requires a holistic approach that integrates physical rehabilitation into survivorship care plans and ensures equitable access to these services.58
Systemic Inequities and Structural Barriers
The findings of this study underscore the systemic inequities that perpetuate disparities in cancer survivorship outcomes. Socioeconomically disadvantaged survivors face intersecting barriers that undermine their ability to achieve optimal health and QoL. Structural determinants, including inadequate healthcare infrastructure, financial inequities, and cultural stigmas, exacerbate these challenges, creating a cumulative burden that disproportionately affects this vulnerable population.59
These findings align with the Social Determinants of Health framework, which emphasizes the role of structural factors in shaping health outcomes. Addressing these systemic inequities requires a multifaceted approach that prioritizes health equity in policy and practice. Evidence-based strategies, such as expanding healthcare coverage, enhancing community-based care, and integrating social and psychological support into survivorship programs, are essential to addressing the root causes of these disparities.60
The findings of this study align with global research demonstrating the significant impact of social determinants of health (SDH) on cancer survivorship, particularly among socioeconomically disadvantaged populations. Similar to studies conducted in high-income countries like the United States and the United Kingdom, financial hardship and limited access to healthcare emerged as primary barriers to quality of life (QoL) for cancer survivors in Saudi Arabia.61 Research from the US highlights the concept of financial toxicity, where the high cost of cancer care leads to treatment delays, non-adherence to follow-ups, and increased psychological distress.62 This study similarly found that financial instability was a major predictor of lower QoL, reinforcing the broader notion that economic disparities exacerbate survivorship challenges regardless of geographic location. Additionally, the role of social support as a mitigating factor was consistent with global evidence, which has shown that strong family and community networks can buffer the negative effects of economic hardship and healthcare barriers.63 However, unlike Western settings where formal survivorship programs and social services are widely available, Saudi survivors often rely heavily on family-based support systems due to cultural norms, highlighting a gap in structured, long-term survivorship care.
Comparing these findings to lower- and middle-income countries (LMICs) reveals additional insights into how healthcare systems influence cancer survivorship outcomes. Studies from India and sub-Saharan Africa similarly report that limited healthcare infrastructure, long travel distances to specialized oncology centers, and lack of financial assistance programs significantly impact cancer survivors’ QoL.64 This mirrors the Saudi context, where centralized healthcare facilities in urban areas create geographic disparities in access to survivorship care. However, unlike many LMICs that struggle with basic oncology care availability, Saudi Arabia has a relatively well-resourced healthcare system with universal healthcare coverage for citizens, yet disparities persist due to systemic inefficiencies and socioeconomic divides.65 Addressing these gaps requires policy-driven interventions, such as decentralized oncology services, mobile health (mHealth) initiatives, and targeted financial assistance programs to ensure equitable survivorship care. By learning from international models that integrate comprehensive, patient-centered cancer survivorship programs, Saudi healthcare policymakers can develop tailored strategies to reduce disparities and enhance long-term survivorship outcomes.66
Structured Mixed-Methods Integration
The integration of quantitative and qualitative findings in this study provides a more comprehensive understanding of how social determinants of health (SDH) impact the quality of life (QoL) of socioeconomically disadvantaged cancer survivors. The quantitative results revealed strong correlations between financial instability, lack of social support, and lower QoL scores, with regression analysis confirming financial difficulties as the most significant predictor of reduced QoL. However, these findings alone do not fully capture the lived experiences and underlying mechanisms contributing to these disparities. The qualitative data added depth to these numerical trends, with participants describing the daily struggles of balancing medical expenses, emotional distress due to financial constraints, and the stigma surrounding their illness, which often led to delayed follow-ups or avoidance of care. By integrating both sets of data, it became evident that financial instability not only affects access to healthcare but also creates a psychological burden, reinforcing patterns of social withdrawal and anxiety that are not entirely captured through survey-based measures.
Moreover, the study found that low social support was a significant quantitative predictor of poor QoL, and qualitative findings further illuminated why this occurs. Participants expressed that while family and community support exist in Saudi culture, traditional gender roles and societal expectations often create barriers to seeking help. Women, in particular, noted that caregiving responsibilities limited their ability to prioritize their own health needs, an aspect not fully reflected in quantitative scores but strongly emphasized in the qualitative interviews. Additionally, while quantitative data showed that participants with lower education levels had poorer QoL, qualitative narratives revealed that health literacy barriers and difficulties in navigating the healthcare system played a crucial role in worsening health outcomes. These insights highlight the value of mixed-methods research, as the qualitative findings contextualize the statistical trends, ensuring that interventions target not only structural factors (eg, financial aid, access to care) but also culturally specific barriers (eg, stigma, gender norms, and health literacy challenges). Structuring the discussion around integrated findings rather than separate analyses reinforces the study’s contribution by demonstrating how a convergent mixed-methods approach provides a more holistic understanding of survivorship challenges in socioeconomically disadvantaged cancer patients.
Implications
The findings of this study have several important implications for clinical practice, public health policy, and future research. First, the significant influence of social determinants of health (SDH) on the quality of life (QoL) among cancer survivors highlights the need for holistic and equity-focused healthcare interventions. Policymakers and healthcare providers must prioritize programs that address financial and logistical barriers to care, such as subsidizing medical expenses, expanding transportation options, and establishing accessible oncology centers in underserved areas. Integrating social support services, such as counseling and community-based programs, into survivorship care plans can also help mitigate the psychological and emotional toll of cancer survivorship.
Second, the findings underscore the importance of culturally tailored interventions in addressing stigma and promoting health-seeking behaviors. Community awareness campaigns that normalize discussions about cancer and encourage early detection could significantly reduce fear, denial, and avoidance behaviors among survivors. Training healthcare providers to deliver culturally sensitive care and address the unique challenges faced by socioeconomically disadvantaged populations is also essential.
Finally, future research should focus on longitudinal studies to better understand the long-term impacts of SDH on cancer survivorship. Mixed-methods approaches, like the one used in this study, can provide comprehensive insights into the lived experiences of survivors and inform the development of targeted interventions that are both effective and contextually relevant.
Limitations
This study has several limitations that should be acknowledged. First, the cross-sectional design precludes the establishment of causal relationships between SDH and QoL. Longitudinal studies are needed to explore how these determinants evolve over time and influence survivorship outcomes.
Second, the study was conducted in Riyadh City, which may limit the generalizability of findings to other regions of Saudi Arabia or countries with different healthcare systems and sociocultural contexts. Future research should consider including participants from diverse geographic and cultural settings to enhance the applicability of results.
Third, while the study utilized validated instruments for data collection, self-reported measures are inherently subject to recall bias and social desirability bias. Participants may have underreported certain barriers or overemphasized others based on their perceptions or experiences. Incorporating objective measures, such as medical records or socioeconomic data, could provide a more comprehensive understanding of the factors influencing QoL.
Finally, the relatively small sample size for the qualitative component, while sufficient for achieving data saturation, may not fully capture the heterogeneity of experiences among cancer survivors. Expanding the qualitative sample and exploring specific subgroups, such as survivors of different cancer types or those in rural areas, could provide deeper insights.
Conclusions
This study highlights the profound impact of social determinants of health (SDH) on the quality of life (QoL) among socioeconomically disadvantaged cancer survivors in Riyadh, Saudi Arabia, using a convergent parallel mixed-methods approach. By integrating quantitative and qualitative findings, the study provides a comprehensive perspective on the financial, social, and psychological challenges that influence cancer survivorship outcomes. The quantitative results identified financial instability and lack of social support as the strongest predictors of lower QoL, while the qualitative findings offered deeper insights into how survivors experience and navigate these challenges within their sociocultural context. The integration of these findings enhances understanding beyond statistical associations, revealing how financial burden extends beyond healthcare costs to affect daily life decisions, psychological distress, and social relationships. Additionally, the study uncovered culturally specific barriers such as stigma, gender-related restrictions, and limited health literacy, which significantly shape survivors’ experiences and access to care.
The mixed-methods design strengthened the study’s contributions by demonstrating the value of combining numerical trends with personal narratives. Unlike studies that rely solely on quantitative measures, this research underscores the importance of integrating patient perspectives to develop targeted, culturally sensitive interventions. These findings emphasize the need for policy-driven solutions such as expanding financial aid programs, decentralizing oncology services, and implementing survivorship support networks that address both structural and cultural challenges. Future research should explore longitudinal mixed-methods approaches to assess how SDH influence survivorship over time and evaluate the effectiveness of interventions aimed at reducing disparities. By incorporating both statistical evidence and lived experiences, this study provides actionable insights for healthcare policymakers and practitioners working to enhance equity-driven survivorship care in Saudi Arabia and other comparable healthcare systems.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the King Saud University Institutional Review Board (IRB= IRB:24-971) 13 September 2024.
Data Sharing Statement
All data are available within the manuscript.
Acknowledgments
The authors acknowledge the financial support from the Ongoing Research Funding program, (ORF-2025-928), King Saud University, Riyadh, Saudi Arabia.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by the Ongoing Research Funding program, (ORF-2025-928), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors declare no conflicts of interest.
References
1. Harrop JP, Dean JA, Paskett ED. Cancer survivorship research: a review of the literature and summary of current NCI-designated cancer center projects. Cancer Epidemiol Biomarkers Prev. 2011;20(10):2042–2047. doi:10.1158/1055-9965.EPI-11-0673
2. Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(S11):2577–2592. doi:10.1002/cncr.23448
3. Osann K, Wenzel L, McKinney C, et al. Fear of recurrence, emotional well-being and quality of life among long-term advanced ovarian cancer survivors. Gynecol Oncol. 2023;171:151–158. doi:10.1016/j.ygyno.2023.02.015
4. Munoz AR, Kaiser K, Yanez B, et al. Cancer experiences and health-related quality of life among racial and ethnic minority survivors of young adult cancer: a mixed methods study. Support Care Cancer. 2016;24(12):4861–4870. doi:10.1007/s00520-016-3340-x
5. Llorens-Ortega R, Bertran-Noguer C, Juvinyà-Canals D, Garre-Olmo J, Bosch-Farré C. Influence of social determinants of health on the quality of life of older adults in Europe: a sex analysis. Res Square. 2023. doi:10.21203/rs.3.rs-3401316/v1
6. Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. Can Med Assoc J. 2016;188(17–18):E474–E483. doi:10.1503/cmaj.160177
7.. Coughlin SS. Social determinants of health and cancer survivorship. J Environ Heal Sci. 2021;7(1):11–15.
8. Bourgeois A, Horrill T, Mollison A, Stringer E, Lambert LK, Stajduhar K. Barriers to cancer treatment for people experiencing socioeconomic disadvantage in high-income countries: a scoping review. BMC Health Serv Res. 2024;24(1):670. doi:10.1186/s12913-024-11129-2
9. Novilla MLB, Goates MC, Leffler T, et al. Integrating social care into healthcare: a review on applying the social determinants of health in clinical settings. Int J Environ Res Public Health. 2023;20(19):6873. doi:10.3390/ijerph20196873
10. Bhattacharyya O, Li Y, Fisher JL, et al. Low neighborhood socioeconomic status is associated with higher mortality and increased surgery utilization among metastatic breast cancer patients. Breast. 2021;59:314–320. doi:10.1016/j.breast.2021.08.003
11. Scheidegger A, Bernhardsgrütter D, Kobleder A, et al. Financial toxicity among cancer survivors: a conceptual model based on a feedback perspective. Support Care Cancer. 2023;31(10):618. doi:10.1007/s00520-023-08066-x
12. Gillard PJ, Ganapathy V, Graham GD, DiBonaventura MD, Goren A, Zorowitz R. Caregiver burden, productivity loss, and indirect costs associated with caring for patients with poststroke spasticity. Clin Interv Aging. 2015;1793. doi:10.2147/CIA.S91123
13. Abdelaziz EM, Alsadaan N, Alqahtani M, et al. Effectiveness of cognitive behavioral therapy (CBT) on psychological distress among mothers of children with autism spectrum disorder: the role of problem-solving appraisal. Behav Sci. 2024;14(1):46. doi:10.3390/bs14010046
14. Mohamed AH, Shaban M, Mohammed HH, Abobaker RM, Alsaqri SH, Raem A. The impact of foot reflexology on fatigue and sleep quality in school-aged children undergoing hemodialysis. J Integr Nurs. 2024;6(2):76–82. doi:10.4103/jin.jin_3_24
15. Mohamed AAK, Shaban M. Age and expertise: the effects of ageism on professional recognition for senior nurses. Geriatr Nurs. 2024;60:70–78. doi:10.1016/j.gerinurse.2024.08.045
16. Więckiewicz G, Weber S, Florczyk I, Gorczyca P. Socioeconomic burden of psychiatric cancer patients: a narrative review. Cancers. 2024;16(6):1108. doi:10.3390/cancers16061108
17. Brandt L, Liu S, Heim C, Heinz A. The effects of social isolation stress and discrimination on mental health. Transl Psychiatry. 2022;12(1):398. doi:10.1038/s41398-022-02178-4
18. Vo J, Gillman A, Mitchell K, Nolan T. Health disparities: impact of health disparities and treatment decision-making biases on cancer adverse effects among black cancer survivors. Clin J Oncol Nurs. 2021;25(5):17–24. doi:10.1188/21.CJON.S1.17-24
19. DiMartino LD, Birken SA, Mayer DK. The relationship between cancer survivors’ socioeconomic status and reports of follow-up care discussions with providers. J Cancer Educ. 2017;32(4):749–755. doi:10.1007/s13187-016-1024-3
20. Hoagland A, Kipping S. Challenges in promoting health equity and reducing disparities in access across new and established technologies. Can J Cardiol. 2024;40(6):1154–1167. doi:10.1016/j.cjca.2024.02.014
21. K R, S L, B P, G S, Lp R. Psychosocial experiences of breast cancer survivors: a meta-review. J Cancer Surviv. 2024;18(1):84–123. doi:10.1007/s11764-023-01336-x
22. Ogden CL, Fakhouri TH, Carroll MD, et al. Prevalence of obesity among adults, by household income and education — United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2017;66(50):1369–1373. doi:10.15585/mmwr.mm6650a1
23. Ali SI, Elballah K, Sayed A, Shaban M. Abacus algorithms: a pure mathematical approach to ancient calculation tools. Abacus. 2023;26(2):1.
24. Zaree A, Dev S, Yaseen Khan I, et al. Cardiac rehabilitation in the modern era: optimizing recovery and reducing recurrence. Cureus. 2023;26. doi:10.7759/cureus.46006
25. Silva P, Araújo R, Lopes F, Ray S. Nutrition and food literacy: framing the challenges to health communication. Nutrients. 2023;15(22):4708. doi:10.3390/nu15224708
26. Park S, Zachary WW, Gittelsohn J, Quinn CC, Surkan PJ. Neighborhood influences on physical activity among low-income African American adults with type 2 diabetes mellitus. Diabetes Educ. 2020;46(2):181–190. doi:10.1177/0145721720906082
27. Patel MI, Lopez AM, Blackstock W, et al. Cancer disparities and health equity: a policy statement from the American society of clinical oncology. J Clin Oncol. 2020;38(29):3439–3448. doi:10.1200/JCO.20.00642
28. Singh H, Fulton J, Mirzazada S, Saragosa M, Uleryk EM, Nelson MLA. Community-based culturally tailored education programs for black communities with cardiovascular disease, diabetes, hypertension, and stroke: systematic review findings. J Racial Ethn Heal Disparities. 2023;10(6):2986–3006. doi:10.1007/s40615-022-01474-5
29. Idris IB, Hamis AA, Bukhori ABM, et al. Women’s autonomy in healthcare decision making: a systematic review. BMC Women's Health. 2023;23(1):643. doi:10.1186/s12905-023-02792-4
30. Mansour R, Abdel-Razeq H, Al-Hussaini M, et al. Systemic barriers to optimal cancer care in resource-limited countries: Jordanian healthcare as an example. Cancers. 2024;16(6):1117. doi:10.3390/cancers16061117
31. Bamodu OA, Chung CC. Cancer care disparities: overcoming barriers to cancer control in low- and middle-income countries. JCO Glob Oncol. 2024;(10). doi:10.1200/GO.23.00439
32. Sabo A, Kuan G, Abdullah S, Kuay HS, Goni MD, Kueh YC. Psychometric properties of the social determinants of health questionnaire (SDH-Q): development and validation. BMC Public Health. 2024;24(1):2507. doi:10.1186/s12889-024-19990-w
33. Dalky HF, Meininger JC, Al-Ali NM. The reliability and validity of the Arabic world health organization quality of life-BREF instrument among family caregivers of relatives with psychiatric illnesses in Jordan. J Nurs Res. 2017;25(3):224–230. doi:10.1097/jnr.0000000000000146
34. Schwarz T, Schmidt AE, Bobek J, Ladurner J. Barriers to accessing health care for people with chronic conditions: a qualitative interview study. BMC Health Serv Res. 2022;22(1):1037. doi:10.1186/s12913-022-08426-z
35. Mols F, Tomalin B, Pearce A, Kaambwa B, Koczwara B. Financial toxicity and employment status in cancer survivors. A systematic literature review. Support Care Cancer. 2020;28(12):5693–5708. doi:10.1007/s00520-020-05719-z
36. Biddell CB, Waters AR, Angove RSM, et al. Facing financial barriers to healthcare: patient-informed adaptation of a conceptual framework for adults with a history of cancer. Front Psychol. 2023:14. doi:10.3389/fpsyg.2023.1178517.
37. Rohatgi KW, Humble S, McQueen A, et al. Medication adherence and characteristics of patients who spend less on basic needs to afford medications. J Am Board Fam Med. 2021;34(3):561–570. doi:10.3122/jabfm.2021.03.200361
38. Kominski GF, Nonzee NJ, Sorensen A. The affordable care act’s impacts on access to insurance and health care for low-income populations. Annu Rev Public Health. 2017;38(1):489–505. doi:10.1146/annurev-publhealth-031816-044555
39. Erskine NA, Gandek B, Tran HV, et al. Barriers to healthcare access and to improvements in health-related quality of life after an acute coronary syndrome (From TRACE-CORE). Am J Cardiol. 2018;122(7):1121–1127. doi:10.1016/j.amjcard.2018.06.043
40. Egan L, Gardner LA, Newton NC, O’Dean S, Champion KE. Moderating effects of socioeconomic status and geographical location on the Health4Life school-based intervention. Prev Med Rep. 2024;46:102855. doi:10.1016/j.pmedr.2024.102855
41. Shelburne N, Simonds NI, Jensen RE, Brown J. Cancer-related emergency and urgent care: expanding the research agenda. Emerg Cancer Care. 2022;1(1):4. doi:10.1186/s44201-022-00005-6
42. Jindal M, Chaiyachati KH, Fung V, Manson SM, Mortensen K. Eliminating health care inequities through strengthening access to care. Health Serv Res. 2023;58(S3):300–310. doi:10.1111/1475-6773.14202
43. Antoni MH, Moreno PI, Penedo FJ. Stress management interventions to facilitate psychological and physiological adaptation and optimal health outcomes in cancer patients and survivors. Annu Rev Psychol. 2023;74(1):423–455. doi:10.1146/annurev-psych-030122-124119
44. Kirkbride JB, Anglin DM, Colman I, et al. The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry. 2024;23(1):58–90. doi:10.1002/wps.21160
45. Timmers I, Cwem Q, Hsu C, Heathcote LC, Rovnaghi CR, Simons LE. The interaction between stress and chronic pain through the lens of threat learning. Neurosci Biobehav Rev. 2019;107:641–655. doi:10.1016/j.neubiorev.2019.10.007
46. Yalcinoz-Ucan B, Zilney L, Zientarska-Kayko A, Ireland T, Browne DT. Examining the effectiveness of psychological interventions for marginalised and disadvantaged women and individuals who have experienced gender-based violence: protocol for a scoping review. BMJ Open. 2022;12(7):e060479. doi:10.1136/bmjopen-2021-060479
47. Vassilev I, Lin SX, Calman L, et al. The role of social networks in the self-management support for young women recently diagnosed with breast cancer. PLoS One. 2023;18(4):e0282183. doi:10.1371/journal.pone.0282183
48. Alruwaili M, Elsayed Ramadan OM, Shaban M, et al. An assessment of pediatric nurses awareness and perceived knowledge of autism spectrum disorders: a gulf state survey. Perspect Psychiatr Care. 2023;2023:1–9. doi:10.1155/2023/4815914
49. Alhumaidan NI, Alotaibi TA, Aloufi KS, et al. Barriers to seeking mental health help in Saudi Arabia: a systematic review. Cureus. 2024. doi:10.7759/cureus.60363
50. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Heal. 2018;6(11):e1196–e1252. doi:10.1016/S2214-109X(18)30386-3
51. Kale S, Vardhan S, Hirani S, et al. Addressing cancer disparities through community engagement: lessons and best practices. Cureus. 2023. doi:10.7759/cureus.43445
52. Shaban M, Mohammed HH, Amer FGM, Elsayed HH, Ali SI, Ibrahim AM. Psychometric evaluation of the translated Arabic version of the geriatrics health behavior questionnaire (GHBQ) for geriatric nurses: a cross-sectional study. BMC Nurs. 2024;23(1):552. doi:10.1186/s12912-024-02164-9
53. Shaban M, Mohammed HH, Gomaa Mohamed Amer F, Shaban MM, Abdel-Aziz HR, Ibrahim AM. Exploring the nurse-patient relationship in caring for the health priorities of older adults: qualitative study. BMC Nurs. 2024;23(1):480. doi:10.1186/s12912-024-02099-1
54. Mohamed Badawy WB, Shaban M. The role of nursing education in advancing sustainable development goals: a rapid review of current pedagogical strategies. Teach Learn Nurs. 2024. doi:10.1016/j.teln.2024.10.014
55. Lustberg MB, Kuderer NM, Desai A, Bergerot C, Lyman GH. Mitigating long-term and delayed adverse events associated with cancer treatment: implications for survivorship. Nat Rev Clin Oncol. 2023;20(8):527–542. doi:10.1038/s41571-023-00776-9
56. Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Heal Reports®. 2014;129(1_suppl2):19–31. doi:10.1177/00333549141291S206
57. Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic Status and Cardiovascular Outcomes. Circulation. 2018;137(20):2166–2178. doi:10.1161/CIRCULATIONAHA.117.029652
58. Song L, Dunlap KL, Tan X, et al. Enhancing survivorship care planning for patients with localized prostate cancer using a couple-focused mHealth symptom self-management program: protocol for a feasibility study. JMIR Res Protoc. 2018;7(2):e51. doi:10.2196/resprot.9118
59. Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic and structural racism: definitions, examples, health damages, and approaches to dismantling. Health Aff. 2022;41(2):171–178. doi:10.1377/hlthaff.2021.01394
60. Lee Smith J, Hall IJ. Advancing health equity in cancer survivorship. Am J Prev Med. 2015;49(6):S477–S482. doi:10.1016/j.amepre.2015.08.008
61. Peitz J, Zhong M, Adebamowo C, Adebamowo SN. Impact of social determinants of health on health-related quality of life among cancer survivors in the United States. Res Square. 2024. doi:10.21203/rs.3.rs-4797703/v1
62. Smith GL, Lopez-Olivo MA, Advani PG, et al. Financial burdens of cancer treatment: a systematic review of risk factors and outcomes. J Natl Compr Cancer Netw. 2019;17(10):1184–1192. doi:10.6004/jnccn.2019.7305
63. Lara-Morales A, Soto-Ruiz N, Agudelo-Suárez AA, García-Vivar C. Social determinants of health in post-treatment cancer survivors: scoping review. Eur J Oncol Nurs. 2024;70:102614. doi:10.1016/j.ejon.2024.102614
64. Gbenonsi G, Boucham M, Belrhiti Z, Nejjari C, Huybrechts I, Khalis M. Health system factors that influence diagnostic and treatment intervals in women with breast cancer in sub-Saharan Africa: a systematic review. BMC Public Health. 2021;21(1):1325. doi:10.1186/s12889-021-11296-5
65. Almalki M, Fitzgerald G, Clark M. Health care system in Saudi Arabia: an overview. East Mediterr Heal J. 2011;17(10):784–793. doi:10.26719/2011.17.10.784
66. Melhem SJ, Nabhani-Gebara S, Kayyali R. Leveraging e-health for enhanced cancer care service models in middle-income contexts: qualitative insights from oncology care providers. Digit Heal. 2024;10. doi:10.1177/20552076241237668
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Quality of Life and the Presence of Depression Among Adults with Hair Loss in the South of Saudi Arabia
Alomaish AR, Gosadi IM, Dallak FH, Darraj AI, Jaafari SM, Alshamakhy AE, Mleeh NT
Psychology Research and Behavior Management 2022, 15:1989-1996
Published Date: 4 August 2022
Assessment of Health-Related Quality of Life Among Patients with Chronic Diseases and Its Relationship with Multimorbidity: A Cross-Sectional Study from Saudi Arabia
Alzarea AI, Khan YH, Alzarea SI, Alanazi AS, Alsaidan OA, Alrowily MJ, Al-Shammari M, Almalki ZS, Algarni MA, Mallhi TH
Patient Preference and Adherence 2024, 18:1077-1094
Published Date: 4 June 2024
Unheard Struggles: Exploring Health-Related Quality of Life Determinants and Coping Mechanisms Among Children with Hearing Loss from Parents and Caregivers Perspective
Lone A
Risk Management and Healthcare Policy 2025, 18:1241-1255
Published Date: 8 April 2025
Assessing Quality of Life in Patients with Epidermolysis Bullosa in the Saudi Population: Validation of the QOLEB Questionnaire
Shehata N, Mahmoud SA, Abdulghani S, Alghamdi Y, Awan ZA, Alshahrani NZ, Algethami MR, Bamimore MA
Clinical, Cosmetic and Investigational Dermatology 2025, 18:1529-1539
Published Date: 20 June 2025

