Back to Journals » Cancer Management and Research » Volume 17
Impact of the Basic Mandatory Health Insurance “AMO-Tadamon” on Continuity of Care Among Breast Cancer Patients Treated at the Oncology Center of the CHU Mohammed VI in Tangier: A Mixed Longitudinal Cohort Study
Authors Bouzini G , Amzerin M, Mahdi Z, Sammoud K, Chahbar A, Najdi A, El m’rabet FZ
Received 1 January 2025
Accepted for publication 22 March 2025
Published 21 April 2025 Volume 2025:17 Pages 851—861
DOI https://doi.org/10.2147/CMAR.S514238
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Ghizlan Bouzini,1 Mounia Amzerin,2 Zaynab Mahdi,3 Karima Sammoud,3 Abdelaziz Chahbar,2 Adil Najdi,3 Fatima Zahra El m’rabet2
1Life and Health Science Laboratory, Faculty of Medicine and Pharmacy of Tangier, Center for Doctoral Studies in Sciences and Techniques and Medical Sciences (CED-STSM), Abdelmalek Essaadi University (UAE), Tangier, Morocco; 2Oncology Center of the Mohammed VI University Hospital of Tangier, Faculty of Medicine and Pharmacy of Tangier, Abdelmalek Essaadi University (UAE), Tangier, Morocco; 3Laboratory of Epidemiology and Public Health, Faculty of Medicine and Pharmacy of Tangier, Abdelmalek Essaadi University (UAE), Tangier, Morocco
Correspondence: Ghizlan Bouzini, Oncology Center of the Mohammed VI University Hospital of Tangier, Faculty of Medicine and Pharmacy of Tangier, Abdelmalek Essaadi University, Tangier, 90080, Morocco, Email [email protected]
Introduction: In Morocco, AMO-Tadamon is a basic mandatory health insurance scheme designed to ensure right to health for all. Implementation of this reform is advantageous for access to healthcare services. However, its impact on continuity of care needs to be assessed. In this study, we aimed to evaluate its impact on continuity of care for breast cancer patients at the Oncology Center of CHU Mohammed VI-Tangier between September 2022 and September 2023.
Methods: This was a mixed longitudinal cohort study. Follow-up information was collected over 13 months. December 1, 2022 was the index-event. Continuity of care was measured using “Bice-Boxerman Continuity of Care Index” and “Usual Provider Continuity” over three chronological sequences.
Results/Discussion: We recorded 74 cases in total, 16/74 were lost to follow-up (21.6%). Significant association (p=0.001; CI (0.01– 0.04)) was observed between AMO-Tadamon generalization and continuity of care in our patients. For both indicators (UPC and COCI), mean continuity of care scores ranged from 0.25 to 0.75 over the three reference periods. This indicates a moderate overall continuity of care. During the first 4 months of this reform, significant positive associations were found between Therapy postponement and its implementation (p=0.003; CI (0.01--0.04)). Moreover, access to expensive drugs was significantly higher in the postgeneralization period (p=0.027; CI (0.01– 0.04)).
Conclusion: Our study suggests a negative impact of this reform on patient care during the period of its generalization and a positive effect on access to expensive drugs after its generalization. A long-term follow-up study is planned. This will assess the impact of this reform on survival.
Keywords: continuity of care, breast cancer, basic mandatory health insurance, medical coverage
Introduction
Background
The usage and definition of the concept of continuity of care varies considerably in the medical literature, but the consensus is that continuity of care is the uninterrupted provision of care for a given patient either in time or between care providers.1–3
In their review of the multidisciplinary literature, Haggerty et al divided the concept of continuity of care into three main dimensions: informational continuity, relational continuity, and management continuity. Depending on the type and context of care, the meaning and use of each of these three concepts may vary.1 Continuity of care in specialty care, including oncology, means continuity of management, according to Haggerty et al. This is reflected in the ability of multiple health care providers involved in a patient’s care to provide coordinated and complementary care within a reasonable time frame, in agreement with a protocol of care and a shared management plan.1 Nevertheless, in 2012, the Cochrane review combined the three dimensions of continuity of care in the disciplinary field of oncology. Therefore, continuity of care for a patient with cancer is the combination of good information transfer, good relational and interpersonal skills and good care coordination.2 It is the way in which a cancer patient experiences care over time, as being coherent and linked.2
Continuity of care is an indispensable dimension of the quality and organization of healthcare services. Numerous studies have demonstrated its association with increased health system efficiency, improved health outcomes and lower health system costs. Furthermore, reduced risk of hospital admission, readmission to hospital, multi-morbidity and mortality are associated with good continuity of care. It also contributes to better therapeutic compliance, patient satisfaction and quality of life.4–19
Ensuring continuity of care is a key issue for all stakeholders in the healthcare system. It therefore needs to be regularly assessed and improved. Obviously, assessing continuity of care is fundamental for evaluating the impact of structural and organizational changes in health care delivery and their consequences. As established by Saultz in 20033 and Jee and Cabana in 2006,20 several indicators have been developed to measure continuity of care. These indicators are generally related to longitudinal continuity. Depending on their use and purpose, they are grouped into five categories. These include measures based on the duration of the patient-provider relationship, the density of medical visits, the dispersion of providers, the sequence of visits to providers, or simply the patient’s subjective perception of continuity of care.20 In the context of chronic pathologies and long-term diseases, the indicators used by researchers to measure continuity of care are still not agreed upon, as there is considerable methodological heterogeneity among published studies and no standard indicator has been developed for this measurement.2,20
In Morocco, the health system has achieved considerable advancements, evidenced by better survival rates, health indicators and reforms designed to enlarge the scope of health insurance coverage. Additionally, as in many other countries around the world, the succession of health crises that shook the world made it necessary to reform the health system at every levels of the Moroccan government. In this quest for improved service quality and universal health coverage, the “AMO Tadamon” project was born. The aim of this reform is to provide universal health coverage. In the same direction, in order to participate effectively in achieving the objectives of this reform with the help of the other actors, the Moroccan Ministry of Health has accelerated the implementation of the structuring projects included in the “AMO Tadamon” support strategy.21–23
Instituted by law 27--22, which completes and amends law n°68--00 on medical insurance, this reform is one of the main pillars of the project to universalize social protection for Moroccans. It guarantees medical coverage for the poor and vulnerable. In fact, as of December 1, 2022, all beneficiaries of the medical assistance scheme for the economically underprivileged - RAMED (a system of free public access to health care for the underprivileged who lack health insurance, which has proven to be limited by the inability of public hospitals to meet the needs of most patients) will be enrolled in the mandatory basic health insurance (AMO-Tadamon) (dedicated to the insured and their dependent family members). Contributions are based on income. For those unable to pay, the monthly contributions are paid by the state, while the rest of the population pays according to their income. The AMO-Tadamon system allows patients to receive treatment in private health facilities rather than being restricted to public facilities as it was with RAMED. This health insurance offers insured persons and their dependents the possibility of using the services of public health facilities free of charge, in addition to access to care provided by the private sector.24–28 This new reform aims to both reduce the burden on public health facilities and ensure equal access to health resources.
In terms of access to health care, the implementation of such structural reform is advantageous. Nonetheless, its impact on continuity of care needs to be assessed, particularly for cancer patients, for whom compliance with dose intensity is essential.
Objective
In this context, we aim to assess the impact of the basic mandatory health insurance AMO Tadamon on the continuity of care among breast cancer patients, covered by this health insurance and treated at the Oncology Center of the CHU Mohammed VI in Tangier.
Materials and Methods
Study Design and Setting
We conducted a mixed longitudinal cohort study using the medical-administrative database of the Oncology Center of the CHU Mohammed VI of Tangier, which is managed by ENOVA software and supplied with all patient data (sociodemographic, clinical, therapeutic and evolutionary).
Study Population
Our cohort is exhaustive and includes all patients with confirmed breast cancer (localized and/or metastatic), who received at least two courses of chemotherapy or hormonal therapy before the implementation of AMO-Tadamon. These patients continued their treatment between September 1, 2022, and the end of September 2023. They were beneficiaries of the former RAMED medical assistance scheme and had experienced the switch of their scheme to AMO-Tadamon since December 1, 2022. Patients under 18 years of age, patients on tamoxifen and not candidates for switching to antiaromatases (AAs) or adding LH‒RH analogs (aLHRHs), patients under posttherapeutic monitoring and patients with incomplete identification and clinical data were excluded from our study.
Data Collection
The follow-up period is staggered over a 13 months from September 1, 2022, to the end of September 2023. We collected follow-up information using a data collection sheet (3 items related to sociodemographic, clinical and therapeutic data) designed and completed by the research team from the patients’ electronic medical records managed by ENOVA software. The study’s “index event” corresponds to December 1, 2022 (AMO-Tadamon scheme launch date). Continuity of care (COC) was measured over 3 chronological sequences using the Bice-Boxerman index (COCI=care dispersion indicator) and the usual provider index (UPC=care density indicator). The first sequence corresponds to the pre-intervention period, which is spread over 3 months before the index event. The second sequence corresponds to the intermediate period (intervention period), characterized by the entry into force of the reform and the generalization of the AMO-Tadamon (index event), which we spread over 4 months. The third sequence corresponds to the post-intervention period (post-generalization of AMO-Tadamon), which we spread over 6 months from April 1, 2023, to September 30, 2023 (Figure 1).
 |
Figure 1 Study design. |
For each period, information on chemotherapy and/or hormonal therapy treatments refers to whether the therapeutic protocols were fully administered or not, and how they were acquired (in-hospital treatment or treatment purchased by the patient). It is noteworthy that all the postponements of the treatment for clinical or biological reasons have been eliminated.
Variables
Continuity of care is our dependent variable. Based on corpus data, we have adopted the Bice–Boxerman index29 and the usual provider continuity (UPC) index30 as measurement indicators. Our selection criteria are measurability, validity, reliability, relevance, interpretability and availability of medical-administrative data:
- The Bice-Boxerman Index (COCI) is an indicator that measures the dispersion of care in terms of whether or not therapeutic protocols are complete and in terms of their acquisition (in-hospital treatment or purchased by the patient)26 (Table 1).
- The Usual Provider Continuity Index (UPCI) is an indicator used to measure the density of care. It is calculated with reference to the available in-hospital treatments. This is done by dividing the number of in-hospital treatments to the total number of treatments administered in each chronological sequence27 (Table 1).
 |
Table 1 Indicators for Measuring Continuity of Care |
Possible scores for both indicators range from 0 to 1. Continuity of care is considered low if it approaches 0 and high if it approaches 1. We have classified continuity of care into three levels according to the value of the scores: the low continuity level refers to scores below the first quartile of 0.25, the moderate level refers to scores between 0.25 and 0.75, and the high level refers to scores above the third quartile of 0.75 to 1.00.
Independent Variable
Entry into force of the generalization of the basic mandatory health insurance “AMO Tadamon”.
Covariates
Sociodemographic, clinical, therapeutic and evolutionary data.
Statistical Analysis
The data collected were entered into Excel and then analyzed using IBM SPSS software (IBM SPSS Statistics Version 25). The first step was a descriptive analysis:
- For quantitative variables, means were calculated.
- For categorical variables, percentages were calculated.
Second, a univariate analysis was performed using the Chi-square test to compare percentages. We then calculated the mean ranks of the two continuity of care indexes and prioritized them according to the three levels of continuity of care. We then tested our results using Friedman’s nonparametric test for matched samples.
Ethics Approval and Consent to Participate
This study has been approved by the University Hospital Ethics Committee of Tangier (CEHUT) (IRB approval number: AC75FV/2024), which waived the requirement for informed consent to participate, because it is a retrospective study for which formal consent may be unnecessary.
However, it was conducted in compliance with the Helsinki Declaration and all elements of ethics are considered. We ensure that the confidentiality and privacy of every patient’s information are maintained, treating personal health data with the highest integrity and following applicable legal and regulatory standards, and insuring that individual identities will remain anonymous during both the collection of data and the final report of study results.
Results
Study Population Characteristics
After excluding ineligible cases, we identified a total of 74 cases to be processed, of which 16/74 (21.6%) were patients lost to follow-up during the reform period. The mean age of our study population was 53.35 years (σ= 11.97). The majority were from Tétouan and Tangier and lived in urban areas (Table 2).
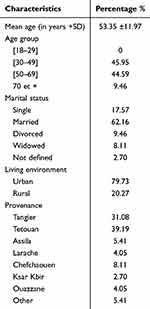 |
Table 2 Study Population Characteristics: Sociodemographic Characteristics |
Moreover, 81.1% of our patients are initially diagnosed at a localized stage, with SBR grade III in more than half. 83.78% received a curative treatment strategy including chemotherapy, surgery, radiotherapy, and hormonal therapy. At 62.2%, luminal B carcinoma is the most common molecular type (Table 3).
 |
Table 3 Study Population Characteristics: Clinical, Therapeutic and Evolutionary Characteristics |
Outcome Data and Main results
A significant association was observed between the generalization of AMO-Tadamon and the continuity of care for our patients (p=0.001 and IC (0.01–0.04)). On the one hand, the implementation of this reform had a negative impact on patient care during the period of its generalization by postponing therapeutic sessions and incomplete administration of therapeutic protocols. On the other hand, after it became generalized, the reform favored patient access to expensive drugs (Figure 2).
 |
Figure 2 Patient access to treatment by sequential period. |
The mean continuity of care scores obtained over the three reference periods for both indicators (UPC and COCI) ranged from 0.25 to 0.75 (0.62 before, 0.47 during, and 0.44 after the generalization of AMO-Tadamon). This indicates an overall moderate continuity of care at the Oncology Center of CHU Mohammed VI in Tangier. However, this continuity of care tends to be higher before the transition from RAMED to AMO-Tadamon (mean=0,62) and lower during the period of its implementation (mean=0.47 and 0.44, respectively) (Table 4).
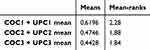 |
Table 4 Continuity of Care Mean Scores for the Three Reference Periods |
After comparing the mean ranks of the scores of the two indicators within the three linked series, a significant positive association (p=0.003 and CI (0.01–0.04) was found between treatment postponement and the implementation of AMO-Tadamon during the first four months after its introduction. In addition, access to expensive drugs was significantly higher among patients in the post-generalization period (p=0.027 and CI (0.01–0.04)). However, there was no significant difference between the AMO-Tadamon generalization period and the post-generalization period regarding the continuity of chemotherapy and/or hormonal therapy with in-hospital drugs (p=0.027 and CI (0.01–0.04)) (Table 5).
 |
Table 5 Comparison of the Mean Ranks of the Scores for the Two Indicators within the Three Linked Series |
Discussion
Key Results and Interpretation
Recommendations for the management of patients with breast cancer provided by clinical practice guidelines and algorithms confirm that adherence to treatment options and follow-up procedures reduces the relative risk of recurrence and improves survival, and that any undue delay would reduce the efficacy of therapy.31–34 In this study, we examined the impact of the reform of the basic mandatory health insurance “AMO-Tadamon” on the continuity of care among patients with breast cancer (breast cancer patients’ follow-up).
For all visits to the oncology service, we calculated the COCI (visit dispersion) and UPCI (visit density), based on observations reported by the treating physicians. These observations relate to whether or not the therapeutic protocols were fully administered and how they were acquired (in-hospital treatment or purchased by the patient). Overall, we observed that switching from RAMED (the medical assistance program for the economically disadvantaged) to AMO-Tadamon was associated with decreased continuity of care as a result of postponement of therapeutic sessions and incomplete administration of therapeutic protocols. But, once generalized, this reform promoted patient access to expensive drugs.
Before the switch from RAMED to AMO-Tadamon, stock-outs of anticancer drugs available free of charge at the oncology center were the main reason for the moderate level of continuity of care (index 0.62) and treatment postponement. This is combined with the financial impossibility of external purchase by patients. During the period of AMO-Tadamon implementation (intervention period), we found that treatment deferrals and low continuity of care (index 0.47) were mainly due to administrative barriers to accessing care, associated with the continued inability of patients to purchase expensive drugs. The overall percentage of patients lost to follow-up (21.6%) was also occurred during this timeframe, coinciding with the emergence of administrative barriers reported by healthcare providers. In the AMO-Tadamon post-generalisation period, the low continuity of care (index 0.44) is due to the high percentage of patients lost to follow-up, which occurred entirely during the AMO-Tadamon generalisation period. This period is also marked by the clear emergence of the possibility for patients to access expensive drugs externally, due to their coverage and/or reimbursement by the AMO-Tadamon Management Organisation. These current findings reveal gaps in cooperation and coordination between all parties involved, which can be attributed to the distinct aspects of health services, funding systems, management approaches, organizational dynamics, and the digital systems for managing patients’ medical records.
Our results support those of similar studies carried out in other countries, which reported that a lack of coordination and communication between different stakeholders, different levels of care, and different patients can be a major problem for continuity of patient care in health care reform.35–38 However, due to differences in the health care system and the nature of the reforms studied, the effects of the reform on continuity of care observed in this study may not be directly comparable to studies conducted in other countries.
Generalizability and Research Limitations
Some limitations are evident in the results of our study. First, even if exhaustive, our sample size was small (74 cases) because of the narrow inclusion and exclusion criteria. Consequently, we probably cannot presume that generalizability is applicable. Second, we measured the COCI and UPCI based on observations reported by treating physicians, referring to the complete administration or not of the therapeutic protocols and how they are acquired (in-hospital treatment or purchased by the patient). This is because we do not have data obtained directly from patient statements. Additionally, as our study was simple and quantitative, it lacked qualitative knowledge that could help us comprehend the perceived difficulties. It is also important to note that we did not perform a multivariate analysis of patient sociodemographic, clinical, therapeutic, and evolutionary characteristics that may simultaneously affect continuity of care.
However, despite these limitations, our first-of-its-kind study offers insightful information. It makes a significant contribution to the continuity of care for cancer patients and to the health policy debate. In addition, the results demonstrated a negative impact of the reform of the basic mandatory health insurance on patient care, which could compromise patient survival. These findings show gaps in cooperation and coordination between all parties involved, which can be attributed to the distinct aspects of health services, funding systems, management approaches, organizational dynamics, and the electronic medical record systems of patients.
Conclusion
The implementation of the basic mandatory health insurance AMO-Tadamon has explicitly influenced the continuity of care among breast cancer patients followed-up at the Oncology Center of the CHU Mohammed VI of Tangier between September 2022 and September 2023. In fact, our study suggests a negative impact on patient care during the reform’s implementation period, but also a positive impact on access to expensive drugs after the reform’s implementation. This negative impact on patient care represents a survival risk. Therefore, it will be important to ensure adequate monitoring and support, to take into account the specificities of health services, the coordination and cooperation of the various actors involved, and the contextualization of the measures taken in accordance with the limited adaptability of traditional service structures and operations. These are essential tools for achieving the objectives of reform strategies and preventing certain adverse effects on patients’ health.
Abbreviations
AA, Anti-aromatase; AMO, basic mandatory health insurance (assurance maladie obligation); CHU, University Hospital Center; CMT, Chemotherapy; COCI, Continuity of Care Index (Bice–Boxerman index); CRC, Concomitant Radiochemotherapy; HER, Human epidermal growth factor receptor; IRB, Institutional Review Board; LH-RH, Luteinizing Hormone - Releasing Hormone; NOS, Not otherwise specified; RAMED, Medical assistance scheme (Régime d’assistance médicale); RH, Releasing hormone; RTH, Radiotherapy; SBR grade, Scarff, Bloom and Richardson grade; SD, Standard deviation; TNBC, triple-negative breast cancer; UPC, Usual provider continuity index.
Data Sharing Statement
The data that support the findings of this study are available from the Oncology Center of the Mohammed VI University Hospital of Tangier, but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from the Oncology Center of the Mohammed VI University Hospital of Tangier.
Acknowledgments
This study used the medical-administrative database of the Oncology Center of the CHU Mohammed VI of Tangier (ENOVA software). The analysis of these data and the results deduced are the sole responsibility of the authors. We acknowledge the Oncology Center of the CHU Mohammed VI of Tangier for providing access to the data.
Funding
The authors would like to acknowledge the financial support provided by Institut de Recherche sur le Cancer (IRC). www.irc.ma under the Scientific Publication Grant Program (Ref: 1796/2024) for the publication of this article.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327:1219–1221. doi:10.1136/bmj.327.7425.1219
2. Aubin M, Giguère A, Martin M, et al. Interventions to improve continuity of care in the follow-up of patients with cancer. Cochrane Database Syst Rev. 2012;2012:CD007672. doi:10.1002/14651858.CD007672.pub2
3. Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1:134–143. doi:10.1370/afm.23
4. Chau E, Rosella LC, Mondor L, Wodchis WP. Association between continuity of care and subsequent diagnosis of multimorbidity in Ontario, Canada from 2001–2015: a retrospective cohort study. PLoS One. 2021;16:e0245193. doi:10.1371/journal.pone.0245193
5. DuGoff EH, Bandeen-Roche K, Anderson GF. Relationship between continuity of care and adverse outcomes varies by number of chronic conditions among older adults with diabetes. J Comorb. 2016;6:65–72. doi:10.15256/joc.2016.6.76
6. Leleu H, Minvielle E. Relationship between longitudinal continuity of primary care and likelihood of death: analysis of national insurance data. PLoS One. 2013;8:e71669. doi:10.1371/journal.pone.0071669
7. Chan K-S, Wan EY-F, Chin W-Y, et al. Effects of continuity of care on health outcomes among patients with diabetes mellitus and/or hypertension: a systematic review. BMC Family Practice. 2021;22:145. doi:10.1186/s12875-021-01493-x
8. Christakis D, Kazak A, Wright J, Zimmerman F, Bassett A, Connell F. What factors are associated with achieving high continuity of care? Family Medicine. 2004;36:55–60.
9. Cheng S-H, Chen -C-C, Hou Y-F. A longitudinal examination of continuity of care and avoidable hospitalization: evidence from a universal coverage health care system. Archives of Internal Medicine. 2010;170:1671–1677. doi:10.1001/archinternmed.2010.340
10. Romaire MA, Haber SG, Wensky SG, McCall N. Primary care and specialty providers: an assessment of continuity of care, utilization, and expenditures. Med Care. 2014;52:1042. doi:10.1097/MLR.0000000000000246
11. Cheng S-H, Hou Y-F, Chen -C-C. Does continuity of care matter in a health care system that lacks referral arrangements? Health Policy Plann. 2011;26:157–162. doi:10.1093/heapol/czq035
12. Hoertel N, Limosin F, Leleu H. Poor longitudinal continuity of care is associated with an increased mortality rate among patients with mental disorders: results from the French national health insurance reimbursement database. Eur Psychiatry. 2014;29:358–364. doi:10.1016/j.eurpsy.2013.12.001
13. Maeseneer JMD, Prins LD, Gosset C, Heyerick J. Provider continuity in family medicine: does it make a difference for total health care costs? Anna Family Med. 2003;1:144–148. doi:10.1370/afm.75
14. Shin DW, Cho J, Yang HK, et al. Impact of continuity of care on mortality and health care costs: a nationwide Cohort Study in Korea. Anna Family Med. 2014;12:534–541. doi:10.1370/afm.1685
15. Chen -C-C, Tseng C-H, Cheng S-H. Continuity of care, medication adherence, and health care outcomes among patients with newly diagnosed type 2 diabetes: a longitudinal analysis. Med Care. 2013;51:231. doi:10.1097/MLR.0b013e31827da5b9
16. Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304:1287–1290. doi:10.1136/bmj.304.6837.1287
17. Jayadevappa R, Guzzo T, Vapiwala N, Malkowicz S, Gallo J, Chhatre S. Continuity of care and advanced prostate cancer. Cancer Med. 2023;12. doi:10.1002/cam4.5845
18. Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors-a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;
19. van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16:947–956. doi:10.1111/j.1365-2753.2009.01235.x
20. Jee SH, Cabana MD. Indexes for continuity of care: a systematic review of the literature. Med Care Res Rev. 2006;63:158–188. doi:10.1177/1077558705285294
21. Ruger JP, Kress D. Health financing and insurance reform in Morocco. Health Aff. 2007;26(4):1009–1016. doi:10.1377/hlthaff.26.4.1009
22. Bouzaidi TD, Ragbi A. An analysis of the trend towards universal health coverage and access to healthcare in Morocco. Health Econ Rev. 2024;14(1):5. doi:10.1186/s13561-023-00477-0
23. Zahidi K, Moustatraf A, Zahidi A, Naji S, Obtel M. Universal health coverage in Morocco: the way to reduce inequalities: a cross-sectional study. [cited March 7, 2025]. Available from: https://openpublichealthjournal.com/VOLUME/15/ELOCATOR/e187494452212220/FULLTEXT/.
24. Dahir n° 1-14-141 portant promulgation de la loi n° 120-13 modifiant et complétant la loi n° 65-00 portant Code de la couverture médicale de base. BO N° 6292 de 18 septembre 2014. 2014.
25. Dahir n° 1-21-30 portant promulgation de la loi cadre n°09.21 relative à la protection sociale. BO N° 7132 de 6 octobre 2022. 2021.
26. Décret n° 2-22-797 d’application de la loi n° 65-00 portant code de la couverture médicale de base, concernant le régime d’assurance maladie obligatoire de base au profit des personnes incapables de s’acquitter des cotisations. BO N° 7147 bis de 30 novembre 2022. 2022.
27. Décret n°2-22-923 de 30 novembre 2022, fixant le seuil d’éligibilité pour le régime d’assurance maladie obligatoire de base au profit des personnes incapables de s’acquitter des cotisations promulgé. 2022.
28. CNSS. Guide de l’Assurance Maladie Obligatoire pour les personnes dans l’incapacité de s’acquitter des cotisations. 2023.
29. Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care. 1977;15:347–349. doi:10.1097/00005650-197704000-00010
30. Steinwachs DM. Measuring provider continuity in ambulatory care: an assessment of alternative approaches. Med Care. 1979;17:551–565. doi:10.1097/00005650-197906000-00001
31. Loibl S, André F, Bachelot T, et al. Early breast cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up☆. Ann Oncol. 2024;35:159–182. doi:10.1016/j.annonc.2023.11.016
32. Denduluri N, Somerfield MR, Chavez-MacGregor M, et al. Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO guideline update. JCO. 2021;39:685–693. doi:10.1200/JCO.20.02510
33. Burstein HJ, Somerfield MR, Barton DL, et al. Endocrine treatment and targeted therapy for hormone receptor-positive, human epidermal growth factor Receptor 2-negative metastatic breast cancer: ASCO guideline update. J Clin Oncol. 2021;39:3959–3977. doi:10.1200/JCO.21.01392
34. Al Sukhun S, Temin S, Barrios CH, et al. Systemic treatment of patients with metastatic breast cancer: ASCO resource–stratified guideline. JCO Glob Oncol. 2024:e2300285. doi:10.1200/GO.23.00285
35. Geng J, Li R, Wang X, et al. Exploring the lack of continuity of care in older cancer patients under China’s “integrated health system” reform. Age Ageing. 2024:53. doi:10.1093/ageing/afae213
36. Nystrøm V, Ohinmaa A, Leonardsen A-CL. Patient pathways in primary health care – an interview study across various health care personnel in a Canadian and a Norwegian county. BMC Health Serv Res. 2024;24. doi:10.1186/s12913-024-11985-y
37. Osei Afriyie D, Loo PS, Kuwawenaruwa A, et al. Understanding the role of the Tanzania national health insurance fund in improving service coverage and quality of care. Soc Sci Med. 2024;347:116714. doi:10.1016/j.socscimed.2024.116714
38. Stylianidis S. The blind spots of psychiatric reform in Greece. Psychiatrike = Psychiatriki. 2024;35:99–102. doi:10.22365/jpsych.2024.009
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

