Back to Journals » Clinical Interventions in Aging » Volume 20
Impacts of Prior Anti-Osteoporosis Treatments on Sequential Denosumab Responses in BMD Changes Among Postmenopausal Osteoporosis Women in East China: Real-World Data Analysis
Authors Guan G, Du Y , Tang W, Chen M, Yu W, Li H, Cheng Q
Received 11 December 2024
Accepted for publication 23 April 2025
Published 8 May 2025 Volume 2025:20 Pages 573—586
DOI https://doi.org/10.2147/CIA.S511622
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Guoyu Guan,1 Yanping Du,2,* Wenjing Tang,2 Minmin Chen,2 Weijia Yu,2 Huilin Li,2 Qun Cheng2,*
1Department of Geriatrics, Huadong Hospital, Fudan University, Shanghai, People’s Republic of China; 2Department of Osteoporosis and Bone Disease, Huadong Hospital, Fudan University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qun Cheng, Department of Osteoporosis and Bone Disease, Huadong Hospital, Fudan University, No. 221, Yan’an West Road, Shanghai, 200040, People’s Republic of China, Email [email protected] Yanping Du, Department of Osteoporosis and Bone Disease, Huadong Hospital, Fudan University, No. 221, Yan’an West Road, Shanghai, 200040, People’s Republic of China, Email [email protected]
Purpose: This study aimed to investigate the impacts of prior anti-osteoporosis treatments on bone mineral density (BMD) changes in Chinese postmenopausal women with osteoporosis following 1-year Denosumab (Dmab) therapy.
Patients and Methods: This retrospective cohort study enrolled 381 postmenopausal women, all receiving a 1-year Dmab treatment. Participants were stratified into five groups based on prior anti-osteoporosis treatments: no treatment (NT), alendronate (ALN), zoledronic acid (ZOL), teriparatide (TPT), and raloxifene (RAL). Potential factors influencing BMD changes were screened using least absolute shrinkage and selection operator (LASSO). The selected variables were then incorporated into a multivariate regression model to identify independent risk factors. Finally, after adjusting for confounders, the impacts of prior anti-osteoporosis treatment on sequential Dmab responses were evaluated.
Results: 1) Further BMD increases were observed after sequential 1-year Dmab with prior use of other anti-osteoporosis drugs; 2) Compared to the NT group, ZOL significantly reduced BMD changes at the lumbar spine (LS), femoral neck (FN), and total hip (TH) (LS: β = − 0.01, P = 0.016; FN: β = − 0.01, P = 0.010; TH: β = − 0.01, P = 0.011); Significant negative associations with FN BMD changes were observed for the ALN group (β = − 0.01, P< 0.001), and the RAL group (β = − 0.01, P = 0.010) compared to the NT group; TPT showed no significant differences with the NT group at all sites; 3) Multiple analysis revealed baseline BMD were independently associated with changes in BMD (LS: β = − 0.04, P = 0.009; FN: β = − 0.19, P < 0.001; TH: β = − 0.14, P < 0.001).
Conclusion: These findings indicated that prior anti-osteoporosis treatments differentially influenced BMD responses to 1-year Dmab therapy. While patients who had previously been treated with ZOL had limited subsequent BMD improvement, patients who had previously used TPT and had lower baseline BMD benefited more.
Keywords: denosumab, alendronate, zoledronic acid, teriparatide, raloxifene, sequential treatment, bone mineral density, postmenopausal osteoporosis
Introduction
Osteoporosis is characterized by progressive decline of bone mass and bone quality, leading to increased bone fragility and risk of fracture. It is a significant public health issue worldwide due to its high prevalence and the serious consequences of fractures. The overall prevalence of osteoporosis in older men and women in the world was reported to be 12.5% and 35.3%, respectively. Also, the highest prevalence of osteoporosis in the elders was reported in Asia with 24.3%.1 It is estimated an osteoporotic fracture occurs every three seconds worldwide.2 Osteoporosis and osteoporotic fractures can lead to decreased quality of life, hospitalization, disability and increased mortality.3 Moreover, osteoporosis can impose a high medical cost on the global economy.4 Thus, management of osteoporosis is necessary to improve quality of life and reduce economic burden on the health care system.
Fortunately, researches have demonstrated that pharmaceutical interventions for osteoporosis can effectively help improve bone density and reduce the risk of fractures.5 Osteoporosis stems from an imbalance in the bone remodeling process, where bone resorption by osteoclasts exceeds bone formation by osteoblasts. Thus, anti-osteoporosis drugs are classified by mechanism as anti-resorptive drugs and anabolic drugs. Anti-resorptive drugs include bisphosphonates (BPs), selective estrogen receptor modulators (SERMs), Denosumab (Dmab), and so on. BPs have a strong affinity for hydroxyapatite, the main mineral component of bone. They bind to the bone surface, particularly in areas of active bone resorption. When osteoclasts encounter bisphosphonate-bound bone, they internalize the bisphosphonate. Bisphosphonates like alendronate (ALN) and zoledronic (ZOL) can inhibit farnesyl diphosphate synthase in osteoclasts, which prevent the synthesis of isoprenoid compounds needed for osteoclast function.6 SERMs, exemplified by raloxifene (RAL), bind to estrogen receptors (ERs) in various tissues. Depending on the tissue, they can act as either agonists or antagonists. In bone tissue, they act as agonists, inhibiting bone resorption, helping to maintain bone density and prevent osteoporosis.7 Dmab is a fully humanised monoclonal antibody against Receptor Activator of Nuclear factor Kappa B Ligand (RANKL), a major regulator of osteoclast development and activity.8 Anabolic drugs include teriparatide (TPT) and abaloparatide. TPT is recombinant human parathyroid hormone 1–34. When administered intermittently, TPT has anabolic skeletal effects which are most marked in trabecular bone.9 All these medications can increase bone density and lower the risk of fractures, according to numerous studies.7,10–14 However, it is important to note that the majority of clinical trials are carried out on treatment-naive patients or on patients who have gone through a drug washout period. Nevertheless, the clinical scenario in the real world is far more complicated.
Osteoporosis is a chronic condition that needs long-term treatment, thus sequential therapy is highly popular and recommended by many guidelines.15–18 Dmab, the first monoclonal drug to be marketed for the treatment of osteoporosis, has been widely used in the clinic for the last decades. It has been shown to increase BMD and reduce the incidence of vertebral, non-vertebral and hip fractures in postmenopausal women with osteoporosis and safety and efficacy are maintained over 10 years of treatment in the Phase 3 randomised FREEDOM trial and open-label extension.19 In addition, subcutaneous Dmab given twice yearly would ensure adherence for 6 months after each dose, which is critical in the treatment of chronic disorders. But all the subjects in the FREEDOM trial were treatment-naive. However, In the real world, Dmab is not only for patients who have never been treated previously. For reasons of effectiveness, safety, convenience, and cost, many patients who have previously used TPT, BPs, or SERMs frequently consider switching to Dmab. There is a gap between clinical trials and clinical practice. Thus, a concern for clinicians is whether the sequential use of Dmab in patients who have been treated with other anti-osteoporosis medications would gain the same benefits as in treatment-naive patients. The majority of studies on sequential Dmab therapy have focused on compared the difference in efficacy between sequential Dmab after the use of a prior anti-osteoporosis drug and continuous prior drugs (eg, BPs or PTH), and there have been no analyses comparing the impacts of prior anti-osteoporosis drugs with different mechanisms including ALN, ZOL, RAL, and TPT on the efficacy of sequential Dmab in one study at the same time.20–22 Thus, the study aims to use real-world data to analyze the impacts of prior anti-osteoporosis treatments including ALN, ZOL, RAL, and TPT on sequential 1-year Dmab responses in BMD changes among postmenopausal osteoporosis women in east China.
Materials and Methods
Study Design and Participants
This study adopted a retrospective design primarily to efficiently analyze the prior treatment’s efficacy on following 1-year Dmab therapy among Chinese PMOP patients, while avoiding the ethical concerns associated with randomized controlled trials (RCTs) and the time and resource constraints of prospective studies, thereby better reflecting treatment outcomes in clinical practice. Thus, the data for this retrospective observational cohort study were sourced from the outpatient department of Huadong Hospital in Shanghai, targeting postmenopausal women residing in eastern China. A total of 381 patients were enrolled in this study from July 2021 to June 2024 (Figure 1). The inclusion criteria are as follows: a) Age ≥ 50 years; b) Patients with a definitive diagnosis of postmenopausal osteoporosis according to clinical consensus;23 c) Patients who had previously used at least 12 months of antiresorptive drugs (ALN, ZOL, RAL), at least 6 months of TPT, or who had never received therapy. They had subsequently used Dmab treatment every 6 months for at least 12 months; d) Adherence: ≥80% for prior treatments and 100% for Dmab treatment. Patients were excluded if they were male; they had secondary osteoporosis; they had an incomplete prior medication history; they had missing data on bone mineral density and bone metabolism markers both at baseline and after 12 months of Dmab treatment; they suffered from chronic metabolic disorders or malignancies, including but not restricted to hyperthyroidism, significantly impaired renal function (creatinine clearance ≤ 35 mL/min as estimated by the Cockcroft and Gault method), multiple myeloma, and leukemia; they had idiopathic bone diseases; they were currently receiving medications known to potentially impact bone or soft tissue metabolism, including but not limited to glucocorticoids, heparin, warfarin, and thyroxine. This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and was approved by the Biomedical Research Ethics Committee of Huadong Hospital Affiliated to Fudan University (No. 2024K181). Informed consent from patients was waived due to the anonymity and confidential analysis of results.
Basic Information Collection and Anthropometric Measurements
This study collected patients’ basic information, encompassing age (years), height (cm), weight (kg), body mass index (BMI), history of fractures, as well as details of prior medications, including medication names and durations. Height was accurately determined to the nearest 0.01 m using a stadiometer, while body weight was precisely measured to the nearest 0.01 kg with a standard balance beam scale. Subsequently, BMI was calculated by dividing the body weight by the square of the height, expressed in kg/m².
Laboratory Measurements
Blood samples were collected in the morning following a 10-hour overnight fast and promptly stored at −80°C immediately for subsequent analysis. Key serum biomarkers indicative of bone and renal function were assayed, encompassing GFR (glomerular filtration rate, mL/min), Scr (serum creatinine, μmol/L), Ca (serum calcium, mmol/L), UA (uric acid, µmol/L), P (serum inorganic phosphorus, mmol/L), AKP (alkaline phosphatase, U/L), PINP (propeptide of type I procollagen, ng/mL), PTH (parathyroid hormone, pg/mL), 25-OH-D (25-hydroxy-vitamin D, ng/mL), OCN (osteocalcin, ng/mL), and CTX (C-telopeptide collagen crosslinks, pg/mL). All biomarkers were measured twice in two tubes with the final results averaged. Utilizing the electrochemical luminescence method (Roche Diagnostics, Boston, MA, USA), PINP, CTX, and 25-OH-D were precisely quantified, with intra-assay and inter-assay CVs (coefficients of variance) maintained below 3.5% and 8.4% for CTX, 2.6% and 4.1% for PINP, and 7.8% and 10.7% for 25-OH-D, respectively, ensuring the reliability and reproducibility of the measurements.
Measurement of Bone Mineral Density and the Definition of Osteoporosis
In this study, bone mineral density (BMD) assessments of the lumbar spine (L2-4 vertebrae) and left total hip were conducted using a dual-energy X-ray absorptiometry (DXA) device, specifically the Hologic Delphi A model manufactured by Hologic Inc. (Methuen, MA, USA). Our laboratory achieved precision errors of 0.8% for lumbar spine measurements, 1.05% for the femoral neck, and 0.97% for the total hip. Prior to each measurement, the DXA machine was standardized utilizing a standard phantom to ensure consistency and accuracy in the obtained data.
To assure the accuracy of the measurements, all BMD measurements in this investigation were performed by two technicians, and all BMD for the same patient were performed by the same technician throughout the trial. Both technicians were certified by International Society for Clinical Densitometry (ISCD).The intraclass correlation coefficient (ICC) values demonstrated excellent agreement between the two technicians for measurements at the FN (0.991), TH (0.992), and LS (0.995) in Supplementary Table 1. According to the World Health Organization (WHO) definition,23 osteoporosis was defined as T-score of BMD ≤ −2.5 for either site of vertebral, femur neck or total hip, or having experienced a low-trauma hip or vertebral fracture, or having osteopenia by BMD who sustain a low-trauma proximal humerus, pelvis, or distal forearm fracture. BMD were performed at the time of switching from the preceding treatment to Dmab and after 12 months of consecutive Dmab.
Statistical Analysis
In this study, continuous variables were presented as means (standard deviations) or medians (interquartile ranges), while categorical variables were expressed through frequencies (proportions). To compare differences among groups for continuous variables, we employed Analysis of Variance (ANOVA) for normally distributed data or the Kruskal–Wallis test for non-parametric data. For categorical variable comparisons, the χ²-test was applied. Potential factors influencing BMD changes following 1-year Dmab treatment were screened using least absolute shrinkage and selection operator (LASSO) with 10-fold cross-validation. The selected variables were then incorporated into a multivariate regression model to identify independent risk factors. Three models were established to evaluate the impact of prior anti-osteoporosis treatment on BMD changes following 1-year Dmab therapy. Model 1 was unadjusted for any variables, Model 2 was adjusted for age, BMI, and fracture history, and Model 3 was adjusted for independent risk factors. All statistical tests were conducted as two-tailed, with a P value of less than 0.05 considered statistically significant. Finally, all statistical analyses were performed using R software (version 4.3.2). Key packages, including stats, glmnet, and rms, were employed for analysis.
Results
Patient Characteristics
This study enrolled 381 postmenopausal female patients with osteoporosis, all of whom completed a 1-year treatment with denosumab. Patients were stratified into five groups based on their prior anti-osteoporotic medication usage: the no-treatment group (NT, n=169), the alendronate group (ALN, n=89, duration year: 3.3 ±2.1), the zoledronic acid group (ZOL, n=39, duration year: 2.7±1.2), the teriparatide group (TPT, n=42, duration year: 0.9 ±0.3), and the raloxifene group (RAL, n=42, duration year: 2.4 ±1.2). The detailed baseline demographic characteristics and clinical indicators of patients in each group were presented in Table 1. No significant differences (P>0.05) were observed baseline serum PTH levels among the five groups. However, statistically significant differences (P<0.05) were found among the groups in age, baseline BMI, fracture history, PINP, 25-OH-D, CTX, OCN, and the baseline BMD at the LS, FN, and TH. Among all patients, the previous fracture rate was 34.38%, and the thoracolumbar spine was the most common site of previous fractures, accounting for 24.15%.
 |
Table 1 Baseline Characteristics of the Study Patients |
LASSO Regression and Multivariate Analysis of Factors Influencing BMD Changes
After 1-year sequential Dmab, LS BMD increased in all groups (0.022–0.060g/cm2, all P<0.001), whereas FN and TH BMD increased only in the NO, ALN, and TPT groups (FN: 0.010–0.025g/cm2, all P<0.01; TH:0.009–0.015g/cm2, all P<0.05). However, increases in BMD were also observed in the ZOL group and the RAL group, but they were not statistically significant (Table 2).
 |
Table 2 Changes in BMD Following 1-year Dmab in Five Groups |
Among the 11 correlated variables from the baseline characteristics analyzed, LASSO regression identified 9 baseline factors significantly associated with LS BMD changes: age, fracture history, serum PINP levels, serum PTH levels, serum 25-OH-D levels, serum CTX levels, serum OCN levels, LS BMD, and TH BMD (Figure 2). Furthermore, the analysis revealed 10 factors demonstrating non-zero coefficients for FN and TH BMD changes: age, BMI, fracture history, serum PINP levels, serum PTH levels, serum 25-OH-D levels, serum OCN levels, LS BMD, FN BMD, and TH BMD (Figures 3 and 4).
Additionally, multivariate analysis revealed three distinct sets of independent associations (Table 3): (1) femoral fracture history, serum 25-OH-D levels, and both baseline LS and TH BMD values were significantly associated with LS BMD changes; (2) age, humeral fracture history, and both baseline FN and TH BMD values were independently associated with FN BMD changes; and (3) age, BMI, and baseline FN and TH BMD values showed independent associations with TH BMD changes.
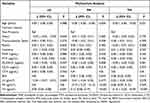 |
Table 3 Multivariate Analysis of BMD Changes at the LS, FN, and TH |
Impact of Prior Treatment on BMD Changes Following 1-year Dmab Therapy
As presented in Table 4, in the unadjusted Model 1, only the ZOL group demonstrated a significant negative association with LS BMD changes compared to the NT group (β = −0.01, 95% CI: −0.02 to −0.00, P = 0.014). This negative association persisted in Model 2 after adjusting for age, fracture history, and BMI (β = −0.01, 95% CI: −0.02 to −0.00, P = 0.019). In addition, in Model 3 after adjusting for independent risk factors, including fracture history, serum 25-OH-D levels, baseline TH BMD, and baseline LS BMD, this negative associations also remained (β = −0.01, 95% CI: −0.02 to −0.00, P = 0.016).
 |
Table 4 Impact of Prior Treatment on BMD Changes with 1-year Dmab Therapy at the LS |
As shown in Table 5, significant negative associations with FN BMD changes were observed for the ALN group (β = −0.01, 95% CI: −0.02 to −0.01, P< 0.001), the ZOL group (β = −0.02, 95% CI: −0.03 to −0.01, P < 0.001), and the RAL group (β = −0.01, 95% CI: −0.03 to −0.00, P = 0.010) compared to the NT group. These associations remained significant in Model 2 after adjusting for age, fracture history, and BMI (ALN: β = −0.01, 95% CI: −0.02 to −0.01, P < 0.001; ZOL: β = −0.02, 95% CI: −0.03 to −0.01, P = 0.002; RAL: β = −0.02, 95% CI: −0.03 to −0.00, P = 0.006). Additionally, after adjusting for independent risk factors in Model 3 also maintained these negative associations (ALN: β = −0.01, 95% CI: −0.02 to −0.01, P = 0.002; ZOL: β = −0.01, 95% CI: −0.03 to −0.00, P = 0.010; RAL: β = −0.01, 95% CI: −0.02 to −0.00, P = 0.045), including age, fracture history, baseline FN BMD, and baseline TH BMD.
 |
Table 5 Impact of Prior Treatment on BMD Changes with 1-year Dmab Therapy at the FN |
As displayed in Table 6, in the unadjusted Model 1, only the ZOL group showed a significant negative association with TH BMD changes compared to the NT group (β = −0.01, 95% CI: −0.02 to −0.00, P = 0.014). This negative association persisted in Model 2 after adjustment for age, fracture history, and BMI (β = −0.01, 95% CI: −0.02 to −0.00, P = 0.019). Furthermore, the association remained significant in Model 3 after adjusting for independent risk factors, including age, BMI, baseline FN BMD, and baseline TH BMD (β = −0.01, 95% CI: −0.02 to −0.00, P = 0.011).
 |
Table 6 Impact of Prior Treatment on BMD Changes with 1-year Dmab Therapy at the TH |
Changes in Bone Turnover Marker After 1-year Dmab Therapy
The results of this study indicated that, compared to baseline, serum PINP, CTX, and OCN levels significantly decreased in all five treatment groups. In terms of serum PTH, only the RAL group showed an increase (Before: 41.56±12.02pg/mL, After: 46.85±13.55pg/mL, P=0.030), while the other four groups did not exhibit significant changes from baseline (Supplementary Table 2).
Discussion
In this study, we used real-world data to compare the impacts of different prior anti-osteoporosis treatments on the efficacy of sequential Dmab among the postmenopausal osteoporosis. Our findings indicated that that increases in BMD were still observed after the use of anti-osteoporosis drugs followed by 1-year sequential Dmab; however, the choice of different prior medications had a variable impact on the effectiveness of sequential Dmab. TPT had the least impact on subsequent Dmab efficacy, and its increase in BMD was comparable to that of the NT group. ZOL, on the contrary, had the greatest impact on subsequent Dmab efficacy and resulted in a less increase in BMD. Furthermore, among three BMD sites, prior treatment had the greatest impact on changes in BMD at FN, with ALN, ZOL, and RAL leading in a significantly smaller improvement in FN BMD than the NT group after sequential 1-year Dmab. In addition, the lower the BMD at the moment of conversion to Dmab, the greater the following BMD improvement.
Osteoporosis is a chronic disease that requires long-term or even lifelong treatment. Sequential therapy is often required during long-term treatment to maintain or increase efficacy, reduce adverse effects, and promote patient compliance. Currently, exploratory investigations on the sequential treatment of osteoporosis medications have focused on RCTs.22,24–26 While RCTs remain the gold standard for assessing efficacy, they do not replicate real-world settings. There is a gap between clinical trials and clinical practice. In RCTs about drug sequencing, subjects are often randomised into groups, given a different initial study drug, then sequenced to a second study drug after a certain period of time, followed by a comparison of efficacy between the groups. The problem, however, is that in the real world, the administration of the initial drug is not randomised. Patients are often stratified clinically based on risk factors to select an initial treatment drug, and thereafter some patients are considered for switching to another drug because of efficacy, safety, economic factors, or convenience.15 And this is the real clinic settings what clinicians encounter more often. Whereas theoretically possible, it is unlikely that an RCT will ever be conducted for this question.
While data from real-world studies are closer to clinical reality, the challenge is that the subjects receiving anti-osteoporosis therapy are heterogeneous. Medication is selected based on the severity of the patient’s disease. Those who have “high fracture risk” (for example, postmenopausal women with no prior fractures and moderately low T-scores) can be started on oral agents such as ALN or RAL. Injectable agents such as TPT, ZOL or Dmab can be considered as initial therapy for those who are at very high fracture risk (for example, older women who have had multiple vertebral fractures or hip fractures, or who have very low T-scores).15 In order to assess the impact of these different anti-osteoporosis drugs on the efficacy of sequential Dmab, a key point is to balance the various confounding factors among treatment groups. In this study, several rigorous methods were applied to reduce bias and confounding in data analysis. First, we used LASSO binary logistic regression model to select for potential variables influencing BMD changes (Figures 2–4). All the variables were from baseline characteristics. Second, the selected variables were then incorporated into a multivariate regression model to identify independent risk factors (Table 3). Finally, three models adjusted for confounders were constructed to assess the impact of prior anti-osteoporosis treatment on BMD changes after sequential Dmab (Tables 4–6).
With the above statistical processing, after adjusting for numerous confounding factors, the results of our study demonstrated that the use of anti-osteoporosis medications with different mechanisms had different impacts on later treatment with Dmab. Bone remodeling is a continuous process involving bone resorption by osteoclasts and bone formation by osteoblasts. In osteoporosis, the balance is disrupted, with increased bone resorption exceeding bone formation. This leads to bone loss and microarchitectural deterioration.27 Thus, the two main targets of current drugs for osteoporosis are the promotion of bone formation and the inhibition of bone resorption. Our results have shown that in postmenopausal osteoporosis, switching therapy from TPT to Dmab further increases bone mineral density at all measured sites, suggesting that this sequential treatment can fully utilise the mechanism of the two different drugs to intervene in the bone remodelling process and further increase BMD. Previous study has confirmed that TPT sequential Dmab therapy significantly enhanced BMD in hip and vertebrae, with particularly notable improvements observed in vertebral bone density.20,22 However, our study further revealed that prior use of TPT did not reduce the increase in BMD after later sequential Dmab compared with the treatment-naive group. In fact, sequential Dmab at the end of TPT treatment is one of the currently recommended sequential treatment strategies.15,22
Our results also showed that the efficacy of sequential Dmab was differentially attenuated by the prior use of ALN, ZOL, and RAL, all of which were antiresorptive agents. Patients who had previously received ZOL experienced significantly smaller gains in BMD at all three sites following sequential Dmab treatment than the NT group. Patients with prior ALN or RAL gained similar increases in BMD at LS and TH following sequential Dmab as the NT group, but exhibited smaller increases at FN. This finding implied that the prior use of drugs that inhibit bone resorption through similar mechanisms to Dmab impacted the efficacy of sequential Dmab. The degree of impact was related to the capacity of prior drugs to suppress bone resorption. Partial overlap in the mechanisms of action of BPs and Dmab could be one explanation for this phenomena. BPs target their action on osteoclasts. They can bind with high affinity to bone and are subsequently taken up by osteoclasts, resulting to impairment of bone-resorbing capabilities and osteoclast death. Whereas Dmab targets osteoclast precursor cells, preventing osteoclasts from maturing and activating before they attach to the bone matrix, resulting in greater inhibition of bone remodeling and more effective anti-bone resorption.28–32 Thus, the total remodeling space had already been reduced during treatment with BPs. Therefore, the stronger the BPs used, the more the bone remodeling space reduces and the less effective sequential Dmab gains. Both ZOL and ALN are nitrogen-containing BPs. The antiresorptive effects of the nitrogen-containing BPs appear to result from their inhibition of the enzyme farnesyl pyrophosphate synthase (FPPS) in osteoclasts. FPPS is a key enzyme in the mevalonate pathway, which generates isoprenoid lipids utilized for the post-translational modification of small GTP-binding proteins that are essential for osteoclast function.6 However, ZOL has an additional ring heterocyclic structure, allowing it to stabilize conformational changes that magnify its inhibitory potency in addition to inhibiting the FPPS enzyme. The rank order for inhibiting FPPS and antiresorptive potency was pamidronate < ALN < ibandronate < risedronate < ZOL.6 Moreover, it was well-established that BPs were the only anti-osteoporotic drugs that could remain in bone matrix.33 Bisphosphonates are retained in the bone for a longer period, and drugs exposed to the bone surface dissociate and return to circulation and reattach to the bone to inhibit bone resorption.34 Bisphosphonates can be retained in the circulation for up to 10 years after discontinuation.34 Nancollas used a constant composition potentiostatic method, to demonstrate significant differences in the kinetic binding affinity of several BPs to hydroxyapatite that established a rank order of clodronate < etidronate < risedronate < ibandronate < ALN < pamidronate < ZOL.35 Therefore, the differences in mineral binding and inhibitory potency for FPPS would both be predicted to affect the duration of action of BPs. ZOL exhibit stronger binding affinity to hydroxyapatite and longer residual time in bone compared to ALN, leading to a more pronounced reduction in bone remodeling space. This explained why switching from ZOL to Dmab resulted in poor BMD improvement compared to ALN. However, Fraser did not observe a significant difference in change in BMD between patients previously on iv ZOL compared to oral BPs, although there was a trend in the TH and FN where the response to Dmab was less in patients on previous iv ZOL transitioning to Dmab.36 Nevertheless, more than one-third of the subjects in that study suffered from secondary osteoporosis and nearly 20% were renally impaired, making the sample less representative. Several studies showed that sequential treatment with BPs–Dmab was associated with higher BMD gain than continuous BPs treatment. None of them, however, examined how the effectiveness of sequential Dmab was affected by prior, different BPs with varying capacities to inhibit bone resorption.24–26
There were limited and inconsistent researches on the effects of transitioning from RAL to Dmab on the changes of BMD.37,38 Although RAL primarily exerts its anti-resorptive effects through selective estrogen receptor modulation and by reducing osteoclast activity and number,39 studies have shown that it can also involve in RANKL/Osteoprotegerin(OPG) pathway by modulating estrogen receptor.40,41 RAL stimulates the production of OPG from osteoblasts, as demonstrated in vitro, carring out their antiresorption activity, at least in part, as means of the OPG/RANK/RANKL system.42,43 In vivo, Messalli reported RAL treatment in postmenopausal women showed a significant increase in OPG levels after 6 months of therapy.44 Both Dmab and OPG can bind to RANKL, negatively regulating osteoclast differentiation and activation by blocking the RANKL-RANK interaction. The overlapping mechanisms of action via the same pathway between RAL and Dmab resulted in a lack of synergistic effects, which might explain the less-than-expected BMD increase in low bone turnover regions (FN sites) observed in this study. Additionally, elevated PTH levels observed in the RAL group emerged as another prominent factor contributing to the insignificant increase in the BMD of cortical bone compared to the notable increase in BMD of trabecular bone.
Another concern is that, among three BMD sites, prior therapy had the greatest impact on changes in BMD at FN, with ALN, ZOL, and RAL resulting in much lesser increases than the NT group after sequential 1-year Dmab. Fraser observed decreased responses in the TH and FN when switching from ZOL to Dmab.36 A meta-analysis of 4RCTs suggest that sequential therapy with BPs and Dmab have just positive effects on lumbar spine bone density in patients with postmenopausal osteoporosis.45 The LS is composed of cancellous (spongy) bone, which has a higher rate of bone turnover and responsive to treatments that promote bone formation or inhibit resorption. In contrast, the FN is primarily composed of cortical bone, which is less metabolically active and may respond differently to the same treatments. And the cortical-cancellous ratio in the TH is lower than in the FN.46,47 Drugs that affect bone remodeling may have a more pronounced effect on areas with higher turnover rates, leading to greater changes in LS BMD.48 This resulted in differences in FN and LS BMD changes throughout the drug sequencing strategy. In this study, the change in BMD was only observed after 1-year sequential Dmab. An increase in FN BMD might have been found after several years of sequential Dmab.
This study revealed an independent negative correlation between baseline BMD and the increase in BMD one year after Dmab treatment. This finding indicated that Dmab may be particularly suitable for patients with lower baseline BMD. Of particular importance, for patients whose BMD remained at a low level despite having received other anti-osteoporotic therapies, switching to or sequentially using Dmab resulted in a more significant increase in BMD. Dmab demonstrated remarkable efficacy in preventing bone loss, decreasing cortical bone porosity, and increasing cortical bone thicking, owing to its ability to significantly inhibit the generation rate of systemic bone remodeling units.49
Bone turnover markers have been widely recognized as effective surrogate indicators for assessing bone turnover rates and predicting fracture risk.50 This study demonstrated that switching to Dmab significantly suppressed bone metabolism marker levels in all five observed groups, notably, an increase in serum PTH levels observed only in the RAL group, suggesting that the patients of this group might require additional vitamin D supplementation to prevent hypocalcemia after transitioning to Dmab Therefore, it is hypothesized that insufficient vitamin D supplementation may be a reason for the limited BMD increase at the hip in the RAL groups.
The strengths of this study include the authenticity and practicality of the data, which are derived from real-world clinical practice and provide valuable insights for guiding actual treatment decisions. In addition, to reduce bias and confounding in data analysis, several statistical approaches were used, including the LASSO binary logistic regression mode and a multivariate regression model. Moreover, the study highlighted differences in treatment efficacy among patients with varying baseline medication histories, providing crucial references for developing personalized treatment plans aimed at enhancing therapeutic outcomes. However, the study also has several limitations. The diversity and complexity of real-world data may lead to sample bias, affecting the generalizability of the results. Unlike an RCT, which has the ability to balance both measured and unmeasured confounders, statistical methods can only be used to balance the measured confounders in our investigation. Unmeasured confounding such as lifestyle factors may create bias. In addition, the subjects were from a real-world clinical setting and it was also impossible to require the subjects to complete the measurements precisely in accordance with the treatment protocol. As a result, some biomarkers were missing, such as vitamin D levels after sequential. Moreover, the limited observation period of one-year makes it difficult to fully assess the long-term efficacy such as fracture risk and safety of Dmab. Lastly, while preliminary mechanistic explorations were performed, further in-depth studies such as long-term fracture risk reduction, optimal treatment duration, and molecular mechanisms are needed to elucidate the specific pathways and interactions between Dmab and other medications.
Conclusion
In summary, this study compare the treatment effects of transitioning to Dmab from different prior treatments using real-world clinical data in Chinese women. According to our research, further BMD increases were observed after sequential 1-year Dmab even with prior use of other anti-osteoporosis drugs (LS: 0.022–0.060g/cm2; FN: 0.005–0.025g/cm2; TH: 0.003–0.015g/cm2). Nevertheless, the effectiveness of subsequent consecutive Dmab treatment are impacted by prior anti-osteoporosis treatment regimens. While patients who had previously been treated with ZOL had limited subsequent BMD improvement(LS: β = −0.01, 95% CI: −0.02 to −0.00, P = 0.016; FN: β = −0.01, 95% CI: −0.03 to −0.00, P = 0.010;; TH: β = −0.01, 95% CI: −0.02 to −0.00, P = 0.011), patients who had previously used TPT and had lower BMD at the beginning of the sequential Dmab benefited more. The results of this study will help clinicians make therapeutic decisions with reasonable expectations of the consequences of sequential therapy, which is quite common in the real world when treating osteoporosis. Increased BMD from effective treatments with sequential Dmab can reduce fracture risks and help prevent the pain and disability. Moreover, a more effective treatment plan can help patients gain confidence in treatment and increase patient compliance, leading to better bone health, fewer fractures and disability, and a more active and fulfilling lifestyle, further enhancing quality of life.
Acknowledgments
We deeply appreciate the contributions and dedication of everyone involved in bringing this study to completion.
Funding
This study was supported by the Health Development Promotion Project - Osteoporosis Scientific Research Project of the Xinge Bureau (Project No. XGJ-005), the National Natural Science Foundation of China (NSFC; Grant No. 81471089), the Shanghai Key Laboratory of Clinical Geriatric Medicine (Grant No. 13dz2260700), and the National Key Research and Development Program of China (Grant No. 2018YFC2000201 and No. 2018YFC2000203).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Salari N, Darvishi N, Bartina Y, et al. Global prevalence of osteoporosis among the world older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):669. doi:10.1186/s13018-021-02821-8
2. Johnston CB, Dagar M. Osteoporosis in older adults. Med Clin North Am. 2020;104(5):873–884. doi:10.1016/j.mcna.2020.06.004
3. Cauley JA. Public health impact of osteoporosis. J Gerontol Ser A Biomed Sci Med Sci. 2013;68(10):1243–1251. doi:10.1093/gerona/glt093
4. Cui Z, Meng X, Feng H, et al. Estimation and projection about the standardized prevalence of osteoporosis in mainland China. Arch Osteoporos. 2019;15(1):2. doi:10.1007/s11657-019-0670-6
5. Ensrud KE, Crandall CJ. Osteoporosis. Ann Intern Med. 2018;168(4):306–307. doi:10.7326/L17-0587
6. Russell RG, Watts NB, Ebetino FH, et al. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int. 2008;19:733–759. doi:10.1007/s00198-007-0540-8
7. Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–645. doi:10.1001/jama.282.7.637
8. Cummings SR, San Martin J, Mcclung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–765. doi:10.1056/NEJMoa0809493
9. Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–1441. doi:10.1056/NEJM200105103441904
10. Bone HG, Hosking D, Devogelaer JP, et al. Ten years’experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004;350:1189–1199. doi:10.1056/NEJMoa030897
11. Lyles KW, Colón-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after Hip fracture. N Engl J Med. 2007;357:1799–1809. doi:10.1056/NEJMoa074941
12. Jiang Y, Zhao JJ, Mitlak BH, et al. Recombinant human parathyroid hormone (1-34) [teriparatide] improves both cortical and cancellous bone structure. J Bone Miner Res. 2003;18:1932–1941. doi:10.1359/jbmr.2003.18.11.1932
13. Kendler DL, Cosman F, Stad RK, Ferrari S. Denosumab in the treatment of osteoporosis: 10 years later: a narrative review. Adv Ther. 2022;39(1):58–74. doi:10.1007/s12325-021-01936-y
14. Ferrari S, Libanati C, Lin CJF, et al. Relationship between bone mineral density T-score and nonvertebral fracture risk over 10 years of denosumab treatment. J Bone Miner Res. 2019;34(6):1033–1040. doi:10.1002/jbmr.3722
15. Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract. 2020;26(Suppl 1):1–46. doi:10.4158/GL-2020-0524SUPPL
16. Gregson CL, Armstrong DJ, Bowden J, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2022;17(1):58. doi:10.1007/s11657-022-01061-5
17. Subarajan P, Arceo-Mendoza RM, Camacho PM. Postmenopausal osteoporosis: a review of latest guidelines. Endocrinol Metab Clin North Am. 2024;53(4):497–512. doi:10.1016/j.ecl.2024.08.008
18. Cortet B, Guañabens N, Brandi ML, Siggelkow H. Similarities and differences between European guidelines for the management of postmenopausal osteoporosis. Arch Osteoporos. 2024;19(1):84. doi:10.1007/s11657-024-01441-z
19. Bone HG, Wagman RB, Brandi ML, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open label extension. Lancet Diabetes Endocrinol. 2017;5(7):513–523. doi:10.1016/S2213-8587(17)30138-9
20. Shane E, Shiau S, Recker RR, et al. Denosumab after teriparatide in premenopausal women with idiopathic osteoporosis. J Clin Endocrinol Metab. 2022;107(4):e1528–e1540. doi:10.1210/clinem/dgab850
21. Kendler DL, Roux C, Benhamou CL, et al. Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res. 2010;25(1):72–81. doi:10.1359/jbmr.090716
22. Leder BZ, Tsai JN, Uihlein AV, et al. Denosumab and teriparatide transitions in postmenopausal osteoporosis (the DATA-Switch study): extension of a randomised controlled trial. Lancet. 2015;386(9999):1147–1155. doi:10.1016/S0140-6736(15)61120-5
23. Lorentzon M, Cummings SR, Sahlgrenska A, et al. Osteoporosis: the evolution of a diagnosis. J Intern Med. 2015;277(6):650–661. doi:10.1111/joim.12369
24. Anastasilakis AD, Polyzos SA, Gkiomisi A, et al. Denosumab versus zoledronic acid in patients previously treated with zoledronic acid. Osteoporos Int. 2015;26(10):2521–2527. doi:10.1007/s00198-015-3174-2
25. Miller PD, Pannacciulli N, Brown JP, et al. Denosumab or zoledronic acid in postmenopausal women with osteoporosis previously treated with oral bisphosphonates. J Clin Endocrinol Metab. 2016;101(8):3163–3170. doi:10.1210/jc.2016-1801
26. Recknor C, Czerwinski E, Bone HG, et al. Denosumab compared with ibandronate in postmenopausal women previously treated with bisphosphonate therapy. Obstet Gynecol. 2013;121(6):1291–1299. doi:10.1097/AOG.0b013e318291718c
27. Raisz LG. Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest. 2005;115(12):3318–3325. doi:10.1172/JCI27071
28. Burgess TL, Qian Y, Kaufman S, et al. The ligand for osteoprotegerin (OPGL) directly activates mature osteoclasts. J Cell Biol. 1999;145(3):527–538. doi:10.1083/jcb.145.3.527
29. Lacey DL, Tan HL, Lu J, et al. Osteoprotegerin ligand modulates murine osteoclast survival in vitro and in vivo. Am J Pathol. 2000;157(2):435–448. doi:10.1016/S0002-9440(10)64556-7
30. Lacey DL, Timms E, Tan HL, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93(2):165–176. doi:10.1016/s0092-8674(00)81569-x
31. Udagawa N, Takahashi N, Yasuda H, et al. Osteoprotegerin produced by osteoblasts is an important regulator in osteoclast development and function. Endocrinology. 2000;141(9):3478–3484. doi:10.1210/endo.141.9.7634
32. Yasuda H, Shima N, Nakagawa N, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A. 1998;95(7):3597–3602. doi:10.1073/pnas.95.7.3597
33. Diab DL, Watts NB. Bisphosphonate drug holiday: who, when and how long. Ther Adv Musculoskelet Dis. 2013;5(3):107–111. doi:10.1177/1759720X13477714
34. Licata AA. Discovery, clinical development, and therapeutic uses of bisphosphonates. Ann Pharmacother. 2005;39(4):668–677. doi:10.1345/aph.1E357
35. Nancollas GH, Tang R, Phipps RJ, et al. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone. 2006;38(5):617–627. doi:10.1016/j.bone.2005.05.003
36. Fraser TR, Flogaitis I, Moore AE, et al. The effect of previous treatment with bisphosphonate and renal impairment on the response to denosumab in osteoporosis: a ‘real-life’ study. J Endocrinol Invest. 2020;43(4):469–475. doi:10.1007/s40618-019-01131-5
37. Nakatoh S. Bone turnover rate and bone formation/resorption balance during the early stage after switching from a bone resorption inhibitor to denosumab are predictive factors of bone mineral density change. Osteoporos Sarcopenia. 2017;3(1):45–52. doi:10.1016/j.afos.2016.12.001
38. Miyoshi A, Kameda H, Nagai S, et al. Beneficial effects of switching to denosumab from bisphosphonates or selective estrogen receptor modulators in postmenopausal women with type 2 diabetes and osteopenia/osteoporosis. J Diabetes Investig. 2021;12(7):1293–1300.
39. Nelson ER, Wardell SE, McDonnell DP. The molecular mechanisms underlying the pharmacological actions of estrogens, SERMs and oxysterols: implications for the treatment and prevention of osteoporosis. Bone. 2013;53(1):42–50. doi:10.1016/j.bone.2012.11.011
40. Cheung J, Mak YT, Papaioannou S, et al. Interleukin-6 (IL-6), IL-1, receptor activator of nuclear factor kappaB ligand (RANKL) and osteoprotegerin production by human osteoblastic cells: comparison of the effects of 17-beta oestradiol and raloxifene. J Endocrinol. 2003;177(3):423–433. doi:10.1677/joe.0.1770423
41. Fernández-García D, Muñoz-Torres M, Mezquita-Raya P, et al. Effects of raloxifene therapy on circulating osteoprotegerin and RANK ligand levels in post-menopausal osteoporosis. J Endocrinol Invest. 2008;31(5):416–421. doi:10.1007/BF03346385
42. Viereck V, Grundker C, Blaschke S, et al. Raloxifene concurrently stimulates osteoprotegerin and inhibits interleukin-6 production by human trabecular osteoblasts. J Clin Endocrinol Metab. 2003;88(9):4206–4213. doi:10.1210/jc.2002-021877
43. Taranta A, Brama M, Teti A, et al. The selective estrogen receptor modulator raloxifene regulates osteoclast and osteoblast activity in vitro. Bone. 2002;30(2):368–376. doi:10.1016/s8756-3282(01)00685-8
44. Messalli EM, Mainini G, Scaffa C, et al. Raloxifene therapy interacts with serum osteoprotegerin in postmenopausal women. Maturitas. 2007;56(1):38–44. doi:10.1016/j.maturitas.2006.05.007
45. Jiang X, Hou S, Xiaolei Deng X, et al. Sequential treatment from bisphosphonate to denosumab improves lumbar spine bone mineral density in postmenopausal osteoporosis patients: a meta-analysis of randomized controlled trials. Medicine. 2024;103(46):e40594. doi:10.1097/MD.0000000000040594
46. Odeh K, Rosinski A, Leasure J, et al. Pedicle screws challenged: lumbar cortical density and thickness are greater in the posterior elements than in the pedicles. Global Spine J. 2019;11(1):34–43. doi:10.1177/2192568219889361
47. Kochetkova T, Hanke MS, Indermaur M, et al. Composition and micromechanical properties of the femoral neck compact bone in relation to patient age, sex and Hip fracture occurrence. Bone. 2023;177:116920. doi:10.1016/j.bone.2023.116920
48. Yoon BH, Kim DY. Discordance between hip and spine bone mineral density: a point of care. J Bone Metab. 2021;28(4):249–251. doi:10.11005/jbm.2021.28.4.249
49. Ramchand SK, Ghasem-Zadeh A, Hoermann R, et al. Denosumab prevents bone loss and microarchitectural deterioration in premenopausal women with breast cancer receiving estradiol suppression therapy: a randomized controlled trial. J Clin Oncol. 2024;42:3466–3477. doi:10.1200/JCO.23.02309
50. Miller PD, Hochberg MC, Wehren LE, Ross PD, Wasnich RD. How useful are measures of BMD and bone turnover? Curr Med Res Opin. 2005;21(4):545–554. doi:10.1185/030079905x41390
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





