Back to Journals » ClinicoEconomics and Outcomes Research » Volume 16
Improving Adherence and Reducing Health Care Costs Through Blister-Packaging: An Economic Model for a Commercially Insured Health Plan
Authors Borrelli EP , Saad P, Barnes NE , Dumitru D, Lucaci JD
Received 25 June 2024
Accepted for publication 25 September 2024
Published 3 October 2024 Volume 2024:16 Pages 733—745
DOI https://doi.org/10.2147/CEOR.S480890
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Eric P Borrelli,1 Peter Saad,2 Nathan E Barnes,2 Doina Dumitru,3 Julia D Lucaci4
1Health Economics & Outcomes Research (HEOR), Becton, Dickinson and Company, San Diego, CA, USA; 2Medical Affairs, Becton, Dickinson and Company, Durham, NC, USA; 3Medical Affairs, Becton, Dickinson and Company, San Diego, CA, USA; 4Health Economics & Outcomes Research (HEOR), Becton, Dickinson and Company, Franklin Lakes, NJ, USA
Correspondence: Eric P Borrelli, Health Economics & Outcomes Research (HEOR), Becton, Dickinson and Company, 3750 Torrey View Ct, San Diego, CA, 92130, USA, Email [email protected]
Purpose: To model the potential clinical and economic impact of blister-packaging medications for chronic conditions on medication adherence and healthcare costs in a commercially insured population.
Methods: A health economic model was developed to evaluate the potential impact of blister-packaging chronic medications for a commercially insured population. The chronic medication classes assessed were renin-angiotensin-system (RAS) antagonists, statins, non-insulin oral antidiabetics, and direct oral anticoagulants (DOACs). The model was designed to reflect the perspective of a hypothetical commercially insured health plan with 100,000 members, over a one-year time horizon. Literature-based or best available epidemiologic references were used to inform the number of patients utilizing each medication class, the impact of blister-packaging on the number of patients who become adherent, as well as the impact of medication adherence in a commercially insured population on healthcare costs for each medication class assessed. Impact on costs was measured in total net healthcare costs, as well as being stratified by medical costs and medication costs.
Results: Following the blister-packaging intervention, there were an additional 591 patients adherent to RAS antagonists, 1196 patients adherent to statins, 169 patients adherent to oral antidiabetics, and 25 patients adherent to DOACs. While pharmacy costs increased, these costs were more than offset by the reduction in medical costs. Overall, the increase in patients adherent to therapy due to blister-packaging led to a reduction in total healthcare costs of $879,312 for RAS antagonists (-$0.73 per-member per-month (PMPM)), $343,322 for statins (-$0.29 PMPM), $78,917 for oral antidiabetics (-$0.07 PMPM), and $120,793 for DOACs (-$0.10 PMPM).
Conclusion: Blister-packaging chronic medications in a commercially insured population has the potential to reduce healthcare costs. Future research is needed to confirm these findings in real-world settings and to fully understand the clinical and economic implications of blister-packaging chronic medications.
Plain Language Summary: Patients not taking their medications as prescribed is common in the United States, leading to disease progression, increased healthcare visits, and increased healthcare costs. Blister-packaging medications is an intervention shown to increase medication adherence, or patients taking their medication as prescribed, and has been around for several decades. While there is research and literature available that shows the impact that blister-packaging medications has on improving adherence, and there is literature available that shows patients taking their medications as prescribed reduces healthcare costs, there is minimal literature available that directly ties these two concepts together. As a result, we modeled from a hypothetical commercial insurance health plan perspective what the impact would be of blister-packaging chronic medications on healthcare costs using the best available peer-reviewed literature and epidemiologic data. This analysis found that for a commercially insured health plan with 100,000 members, 591 additional patients would become adherent to their renin-angiotensin-system (RAS) antagonists blood pressure medications, 1196 additional patients would become adherent to their statins, 169 additional patients would become adherent to their oral antidiabetics, and 25 additional patients would become adherent to their direct oral anticoagulants (DOACs). Additionally, this would lead to a reduction in healthcare costs for the health plan of $879,312 for RAS antagonists (-$0.73 per-member per-month (PMPM)), $343,322 for statins (-$0.29 PMPM), $78,917 for oral antidiabetics (-$0.07 PMPM), and $120,793 for DOACs (-$0.10 PMPM).
Keywords: medication adherence, medical cost offsets, healthcare costs, total cost of care, medication adherence packaging, blister-packaging, blister-packing, self-insured
Introduction
Chronic disease prevalence in the adult population in the United States (US) remains significant, with data from 2018 indicating that 27.4% of adults aged 18–44, 63.4% of adults aged 45–64, and 87.6% of adults 65 years or older had at least one chronic condition.1 Notably, 27.2% of the adult population had at least two chronic conditions, with prevalence increasing with age.1 Managing these conditions can be burdensome, and while numerous treatments are available, adherence to medication regimens is a significant factor in treatment success.2–4
Nonadherence to medications for chronic conditions has been linked to treatment failure, poor health outcomes, increased healthcare resource utilization (HCRU), and greater healthcare costs.5 Several studies have shown that in both commercially insured populations and Medicare populations, patients adherent to medications for chronic conditions have lower HCRU and healthcare costs.6–15 Rates of nonadherence for chronic medications in the US have been reported to vary in the literature, ranging from 20% to at least 32% for antihypertensives, 25% to 38% for statins, 20% to 35% for noninsulin antidiabetics, and 24% to 46% for oral anticoagulants.6–12 Medication nonadherence, a pervasive challenge, negatively impacts both patients and the healthcare system in the U.S.16,17 Consequently, payers are intensifying the scrutiny of medication adherence metrics for different chronic conditions to enhance performance evaluation and provide better healthcare quality.18 Different quality measures exist for payers to use to assess their own performance as well as for individuals to assess different public health plans.18 The Pharmacy Quality Alliance (PQA) is an organization that has created several validated quality measures of health plan performance, including measures for medication adherence.19
Contributing factors of medication nonadherence include the complexity of the medication regimen, patient forgetfulness, patients not understanding their condition and/or how their medication impacts their condition, running out of refills and not being able to have their prescription filled by their pharmacy, forgetting to refill their prescription at the pharmacy, high medication costs and many more.20 Considering the impact that medication adherence can have on patient outcomes and healthcare costs, several initiatives have been developed to help promote adherence among patients.20–22 Some of the interventions available that are tailored to help promote different factors associated with medication nonadherence and have been shown to be successful in improving medication adherence include medication adherence packaging such as blister-packaging or calendar packing medications, patient outreach initiatives by the pharmacy or payer, prescriber outreach by the pharmacy or payer, medication therapy management (MTM) or medication reconciliation, 90-day prescription fills, and pharmacist counseling.20–28 Typically, multiple adherence interventions may be implemented at the same time to help increase the odds of patients becoming adherent.
Blister-packaging or calendar packing medications is an intervention long-recognized for promoting medication adherence, aiding patients in remembering to take their medication and reducing the complexity of medication regimens. Studies have shown blister-packaging medications has led to increases in adherence rates and patients becoming adherent.22,23,29,30 For instance, one study by Zedler et al, a retrospective analysis of pharmacy dispensing data at over 3700 Walmart pharmacies in 49 states across the US from December 2006 through July 2009 of patients utilizing angiotensin-converting enzyme inhibitors (ACEi) used a propensity-score matched analysis to assess the odds of patients becoming adherent – defined as the proportion of days covered (PDC) greater than or equal to 80%. This study found that prevalent users of ACEi who had their medications blister-packaged had 12% higher odds of being adherent compared to those without blister-packaged medications (adjusted odds ratio (aOR): 1.12, 95% confidence interval (CI): 1.08–1.16).23
While there are studies that correlated blister-packaging with improved medication adherence for chronic conditions, there is a gap in the literature regarding the economic impact of such packaging on HCRU. Therefore, the aim of this study was to model the potential clinical and economic impact of blister-packaging medications for chronic conditions on medication adherence and healthcare costs in a commercially insured population.
Materials and Methods
Study Design
An economic model was developed to assess the potential impact of blister-packaging chronic medications for a commercially insured population. The model took the perspective of a hypothetical commercially insured health plan with 100,000 members, and the time horizon of the analysis was 1 year. Medication adherence was defined using the PDC of 80% or greater,31 which is the definition used by the PQA for their medication adherence quality measures.19 Discount rates were not applied to healthcare costs due to the short time horizon of the analysis.32 This economic model followed best practices for building and reporting economic analyses.33–36
Medication Classes Assessed
This model’s objective was to evaluate medication adherence to chronically utilized medications in this population. A thorough literature review revealed the impact of medication adherence on healthcare costs for the different oral medication classes that the PQA has medication adherence measures for, with the exception of antiretrovirals that have a different definition of adherence: PDC greater than or equal to 90%, and medications that are filled through specialty pharmacy, specifically non-infused medications to treat rheumatoid arthritis and non-infused disease modifying therapies for multiple sclerosis.19 After reviewing the literature available that was published within the last fifteen years, studies were identified that allowed us to measure the impact of adherence on healthcare costs for renin-angiotensin-system (RAS) antagonists,7 statins,8 non-insulin antidiabetics,9 and direct oral anticoagulants (DOACs).10 All studies examined the impact of adherence to the medication of interest to healthcare costs, using an adherence definition of greater than or equal to 80% PDC.7–10
Population
Epidemiologic data of a commercially insured population was used to analyze the percentage of patients on each medication class assessed. For patients utilizing RAS antagonists, we first identified the number of patients in the population diagnosed with hypertension using antihypertensive therapy from the prevalence of hypertension by patient age.37 This approach estimated that 31.2% of patients would have hypertension in a commercial health plan (Figure 1).38 Subsequently, the percentage of hypertension patients who utilize RAS antagonists (50%)39 was identified to calculate the number of patients in the health plan who would be utilizing RAS antagonists (15.6%).
Since statins are used for numerous conditions in addition to hyperlipidemia, the number of patients on statins was directly determined. Starting with the prevalence of statin utilization in the United States and focusing on those with private/commercial insurance (53% of 92 million),40 the prevalence of statin users within the commercially insured population38 was calculated to be 26.15%.
For patients utilizing oral antidiabetics for type II diabetes mellitus (T2DM), the prevalence of adults aged 18–44 with T2DM was 3%, while 14.5% for patients aged 45–64 had T2DM.41 The prevalence of T2DM was matched by the mean breakdown of age per commercial health plan38 to determine that 6% of the health plan has a diagnosis of T2DM. The percent of T2DM patients who utilize antidiabetic therapy was identified (82.7%)42 as well as the percent who do not utilize monotherapy insulin (84.6%).43 This led to 4.04% of the health plan utilizing non-insulin antidiabetic therapy.
In estimating the prevalence of DOACs use, the model focused on patients with atrial fibrillation (AFib) and patients with venous thromboembolism (VTE). While DOACs are indicated in additional conditions,44–47 we were unable to identify the epidemiological data to analyze their utilization in those other conditions. Although this may lead to an underestimation in this model, AFib and VTE are likely the two most indicated conditions of DOAC use. For patients with AFib, the estimated prevalence of working aged patients 18–64 with AFib was 0.83%.48 After age distribution adjustments for the health plan,38 it led to a prevalence of 0.63% of the entire health plan population. Considering that half of patients with AFib are on DOACs (50%),49 this suggests that 0.315% of the population received DOACs for AFib. The incidence of VTE within the commercial population was established at 0.214% for patients aged 25–64.50 Adjusting this to represent the incidence for the entire health plan population (0.163%), this was multiplied by the percent of patients with VTE who utilize DOACs (92%),51 to get the percent incidence of the population utilizing DOACs for VTE (0.150%). Incidence was used instead of prevalence for VTE because secondary treatment is initiated after an event and while some patients may continue anticoagulation therapy indefinitely, others are treated for only a set time.52 Combining these figures, the total utilization rate of DOACs for both AFib and VTE in the health plan was calculated at 0.465%.
Adherence Rates and Impact of Intervention
This model examines the effect of blister-packaging chronic medications. The impact of the intervention is a 12% increase in patients becoming adherent based upon the Zedler et al retrospective pharmacoepidemiology study which analyzed data from a national pharmacy chain from December 2006 through July 2009.23 The baseline rates of adherence in the model for each medication was taken from the average rates of patients being adherent to said medication class in the studies utilized to assess impact of adherence on healthcare costs. This equated to adherence rates of 68.4% for RAS antagonists,7 61.9% for statins,8 65.2% for oral antidiabetics,9 and 54.4% for DOACs.10
Healthcare Costs
Regarding costs, the model evaluated the impact of medication adherence on medical costs, pharmacy costs, and total healthcare costs for all four medication classes. For RAS antagonists, adherent patients had a reduction in monthly medical costs of $162, an increase in monthly pharmacy costs of $42, and a net reduction in monthly total healthcare costs of $124 per patient.7 For statins, adherent patients had a reduction in medical costs of $73 per month, an increase in pharmacy costs of $50 per month, and a net reduction in total healthcare costs of $24 per month per patient.8 Patients adherent to oral antidiabetics saw a monthly decrease in medical costs of $53 per patient, a monthly increase in pharmacy costs of $32, and a net decrease in total monthly healthcare costs of $39 per patient.9 Lastly, adherent patients on DOACs saw a monthly reduction in medical costs of $711 per patient, a monthly increase in pharmacy costs of $344 per patient, and a net monthly decrease in total healthcare costs of $396 per patient.10 All costs in the model were adjusted to 2024 US dollars using the US medical Consumer Price Index (CPI).53
Sensitivity and Scenario Analyses
Model sensitivity and uncertainty was assessed via sensitivity and scenario analyses. One-way sensitivity analyses were conducted for all input parameters, with the upper and lower bounds of the analysis being supported by peer-reviewed literature where applicable, or plus/minus 20% where peer-reviewed literature was not able to be identified for upper and lower bounds. The inputs for the one-way sensitivity analyses are available in Supplemental Table 1. Scenario analyses were performed to examine the impact of varying health plan sizes on the net impact of total healthcare costs for plans with member sizes of 10,000 members, 25,000 members, 50,000 members, 75,000 members, and 150,000 members.
Results
In the model, prior to blister-packaging there were an estimated 10,660 patients adherent to RAS antagonists, 16,187 adherent to statins, 2633 adherent to oral antidiabetics, and 253 adherent to DOACs. Following the initiation of blister-packaging for these medications, there were an additional 591 patients adherent to RAS antagonists, 1196 patients adherent to statins, 169 patients adherent to oral antidiabetics, and 25 patients adherent to DOACs.
Annual pharmacy costs increased by $298,848 for patients on RAS antagonists, $717,634 for patients on statins, $65,562 for patients on oral antidiabetics, and $105,019 for patients on DOACs (Table 1). Conversely, annual medical costs decreased by $1,151,850 for patients on RAS antagonists, $1,042,448 for patients on statins, $107,125 for patients on oral antidiabetics, and $216,815 for patients on DOACs. Overall, the increase in patients adherent to therapy due to blister-packaging led to a reduction in total healthcare costs of $879,312 or $0.73 per-member per-month (PMPM) for patients on RAS antagonists, $343,322 or $0.29 PMPM for patients on statins, $78,917 or $0.07 PMPM for patients on oral antidiabetics, and $120,793 or $0.10 PMPM for patients on DOACs (Figure 2).
 |
Table 1 Impact of Blister-Packaging Medications on Healthcare Costs |
 |
Figure 2 Impact of Blister-Packaging on Per-Member Per-Month (PMPM) Healthcare Costs. Abbreviations: DOACs, Direct Oral Anticoagulants; PMPM, Per-Member Per-Month; RAS, Renin-Angiotensin-System. |
The model input that demonstrated the largest sensitivity was the impact of blister-packaging on patients becoming adherent (RAS antagonists: -$0.42 PMPM to -$1.05 PMPM; statins: -$0.19 PMPM to -$0.38 PMPM; oral antidiabetics: -$0.04 PMPM to -$0,09 PMPM; DOACs: -$0.08 PMPM to -$0.12 PMPM) (Table 2). The percent of health plan on each medication class, as well as the reduction in total health care costs per adherent patient, and the percent of patients adherent pre-implementing blister-packaging varied between medication class for second through fourth most sensitive inputs.
 |
Table 2 Variability of the Model per-Member per-Month Results Assessed in the One-Way Sensitivity Analyses |
The scenario analysis of varying health plan sizes showed variations in reductions in healthcare costs for plans from 10,000 members to 150,000 members ranging from $87,931 to $1,318,968 for RAS antagonists, $34,332 to $514,983 for statins, $7892 to $118,376 for oral antidiabetics, and $12,079 to $181,190 for DOACs (Table 3).
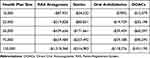 |
Table 3 Scenario Analysis Assessing Impact of Varying Health Plan Size on Total Healthcare Costs |
Discussion
This economic analysis modeled the potential impact of increased adherence for a commercial population for several chronic medications on healthcare costs based on peer-reviewed literature. The intervention led to adherence gains and showed a significant reduction in annual health care costs for major drug classes, filling a gap in the literature underscoring the potential impact of blister-packaging chronic medications on healthcare costs for commercially insured patients.
While not modeled in this study due to missing background rates of HCRU, the four studies included in the analysis of impact of medication adherence on healthcare costs also showed significant reductions in HCRU. In the analysis of RAS antagonist utilization, they found that after adjusting for demographic and clinical covariates, patients adherent to RAS antagonists had a significant reduction in inpatient use (adjusted risk ratio (aRR): 0.612, 95% CI: 0.607–0.617) and a statistically significant but minimal clinically meaningful impact on outpatient use (aRR: 0.995, 95% CI: 0.994–0.997).7 In the analysis of statin utilization, it was noted that patients adherent to statins had a significant reduction in inpatient utilization (aRR: 0.756, 95% CI: 0.749–0.762) and a statistically significant increase but minimal clinically meaningful impact on outpatient use (aRR: 1.009, 95% CI: 1.007–1.010).8 The analysis of oral antidiabetics found that adherent patients had a significant reduction in inpatient utilization (aRR: 0.834, 95% CI: 0.819–0.850) but a significant increase in outpatient use (aRR: 1.036, 95% CI: 1.032–1.039), although the cost ratio for outpatient expenditures had a significant reduction (adjusted cost ratio (aCR): 0.974, 95% CI: 0.970–0.978).9 Included in a publication separate from the one assessing impact of adherence on healthcare costs, the authors of the study evaluating DOAC adherence showed that nonadherence to DOACs had a significant increase in ischemic stroke at 6 and 12 months (adjusted hazards ratio (aHR): 1.818, 95% CI: 1.240–2.667; aHR: 2.077, 95% CI: 1.112–3.879) and a significant increase in VTE (deep-vein thrombosis and pulmonary embolism) at 6 and 12 months (aHR: 2.120, 95% CI: 1.189–3.780; aHR: 5.386, 95% CI: 1.780–16.296), while having nonsignificant impact on major bleeding at 6 and 12 months (aHR: 1.056, 95% CI: 0.815–1.368; aHR: 0.883, 95% CI: 0.574–1.358).11
Assessing the potential impact of medication adherence packaging with blister-packaging medications for chronic utilization, this model primarily focuses on the health plan payer perspective. However, health plans generally do not directly fund such interventions. A practical approach is through self-insured integrated delivery networks (IDN)/health system.54 In this scenario, the health plan is also the health system that could implement blister-packaging medications in their outpatient pharmacy for both employees who fill their prescriptions at the health system, as well as patients in the system. For a self-insured employer, unused healthcare costs would be able to be reinvested back into the company.55 Additionally, by providing an intervention for employees to help promote adherence, employers could potentially see an improvement in quality of life and productivity from employees as research has shown that patients with improved adherence not only results in improved health outcomes,7–11,56 but also improvements in quality of life (QoL) and productivity.57–60 Another potential option is for retail pharmacies engaging in value-based contracts with pharmacy benefits managers (PBMs) potentially pursuing blister-packaging medications to help improve adherence rates for their patients, leading to higher reimbursement rates. An additional opportunity is for self-insured retail pharmacies or self-insured PBMs with mail-order pharmacies, who could pursue blister-packaging chronic medications for their employees as well as their patients.
Self-insured IDNs or health systems that implement blister-packaging chronic medications may also see health benefits for their patients not seen in this specific model which may lead to reduction in health care costs and/or reduction in lost reimbursement due to value-based contracting for health outcomes. Value-based contracting (VBC) has increased in recent years tying reimbursement for medical and pharmacy costs to outcomes.61–63 The Centers for Medicare & Medicaid Services (CMS) has a Hospital Readmissions Reduction Program (HRRP), which is an initiative to improve quality of care for Medicare patients and reduces reimbursement to hospitals for patients who are readmitted within 30 days for the conditions or procedures of acute myocardial infarction (AMI), chronic obstructive pulmonary disease (COPD), heart failure (HF), pneumonia, coronary artery bypass graft surgery, and/or elective hip or knee arthroplasty.62 Several studies have shown that medication nonadherence is a contributing factor to rehospitalization in some patients.64–66 While no studies were able to be identified showing the impact of blister-packaging on 30-day or 90-day rehospitalization in these conditions, blister-packaging has been seen to help promote improved medication adherence which makes it plausible that blister-packaging may have a potential impact on reducing readmissions, although future studies would need to study this possibility.
One important limitation exists in the study used in the model evaluating the impact of adherence to oral antidiabetics, which is that the study was conducted before some newer antidiabetic agents came to market (sodium-glucose cotransporter-2 (SGLT2) inhibitors, glucagon-like peptide 1 (GLP-1) agonists) or were very new to market and had low adoption rates during the study period (dipeptidyl peptidase 4 (DPP-4) inhibitors).8 These medications are now included as potential first-line options in the treatment of T2DM.67 Additionally, these medications have shown to have significant clinical benefits on cardiovascular outcomes68,69 and are recommended as first-line treatment options for cardiovascular patients both with T2DM70 and without T2DM.71,72 Due to the superiority of these newer agents, specifically SGLT2 inhibitors and GLP-1 antagonists, on diabetes and cardiovascular outcomes,68,69 it is plausible that the increasing adherence to these agents would result in an even larger reduction HCRU and healthcare costs. However, all of the agents in the three newer classes of medications as of now are brand name medications compared to the generic alternatives of the older classes of oral antidiabetics included in the study and would likely lead to an increase in pharmacy costs with increased adherence. Additionally, specific medications within each of the three newer classes have agents that have been among the largest price increases of medications in the US over the last 5 years.73–77 It is difficult to determine what the overall impact of increased adherence to these newer medications would mean on total healthcare costs with the likely reduction in medical costs and increase in pharmacy costs, as future studies needed to assess this impact. In addition, newer policies and regulations such as the Inflation Reduction Act and the California drug price transparency law among others may affect the overall healthcare cost by influencing pricing and access. However, the exact direction and full impact of these initiatives remain unknown at this time.
While blister-packaging is a highly effective intervention at promoting medication adherence, other interventions co-exist, such as patient outreach initiatives by the pharmacy or payer, prescriber outreach by the pharmacy or payer, medication therapy management (MTM) or medication reconciliation, 90-day prescription fills, pharmacist counseling. Although these interventions have demonstrated varying rates of improvement in medication adherence, there is limited data on their impact on economic outcomes.21 Future studies, such as cost-effectiveness analyses and/or budget impact analyses are needed to assess the financial implications of implementing these differing initiatives.
When interpreting the results, it is important to use caution when estimating the overall impact for increased adherence to all four classes of medications evaluated in this model. The conditions for which these medications are indicated have some overlap in populations as all four classes have cardiovascular impacts. The most prevalently used risk calculators are the 10-year American College of Cardiology (ACC)/American Heart Association (AHA) cardiovascular risk assessment in adults;78 CHADS2 predicting risk of stroke and thromboembolism in AFib;79 CHA2DS2-VASc for risk of stroke and thromboembolism in AFib.80 Factors determining risk of cardiovascular events include impact of cholesterol, blood pressure, diabetes, and prior events. Statins are the standard therapy for patients with T2DM even in patients without hyperlipidemia as primary prevention of cardiovascular events.70 Additionally, statin utilization in T2DM is a quality measure by PQA for appropriate medication use.19 Moreover, for those patients with T2DM and chronic kidney disease, RAS antagonists are recommended as treatment to prevent progression of disease and reduce cardiovascular events.81 An analysis of the Quintiles Electronic Medical Record research database from July 2014 through June 2015 found that among patients with T2DM, 82.1% had hypertension, 77.2% had hyperlipidemia, and 67.5% of patients had both hypertension and hyperlipidemia.82 In the study examining DOAC utilization, 49% of patients were on statins, and 48% of patients were on RAS antagonists.10 It is expected that patients with these comorbid conditions becoming adherent to their pharmacologic treatment would receive a greater benefit in health outcomes and costs impact than a patient with a single condition would receive; however, it likely would not be the same as combining the effects of multiple classes together.
Limitations
This analysis has several limitations exist beyond those already mentioned. One limitation relates to the impact of blister-packaging medications as it was assessed in a study conducted of only ACEi. While this analysis assessed RAS antagonists which includes ACEi, it also includes RAS antagonists consisting of angiotensin-II receptor blockers (ARBS), statins, oral antidiabetics, and DOACs. While these remaining medications were not evaluated in the study, it seems reasonable to assume the impact would carry over to most medications that are dosed once daily. For medications dosed twice daily, the specific impact remains uncertain. The one-way sensitivity analysis attempted to highlight the level of variability and uncertainty in this input by varying the potential impact. As with all economic models, there is uncertainty in the actual impact of the intervention on the outcomes modeled in the analysis, and future studies are needed to examine the impact in real-world settings. However, this model shows the potential impact based upon the best available peer-reviewed literature tying the impact of blister-packaging on increasing patients becoming adherent to the impact on adherent patients reducing healthcare costs. An additional limitation, which is seen in all pharmacoepidemiology adherence studies, is that the measure of adherence is based upon prescription dispensing claims, without verifying correct medication use or timing.83 Despite this limitation, the studies in the analysis used a validated definition of adherence of 80% PDC, and showed reduction in healthcare costs and HCRU with this definition.7–10 An additional limitation of the study is that it used a 1-year time horizon. While this time horizon helps demonstrate the short-term impact on healthcare costs, which is most relevant to commercial payers due to the potential of beneficiaries switching plans in the commercial market, it does not fully capture the potential long-term benefits and/or impacts. Another limitation of this analysis was that it only included the impact of blister-packaging four different medication classes (RAS antagonists, statins, oral antidiabetics, and DOACs). We were unable to find data in the literature to model the potential impact of blister-packaging other chronic medications, and therefore the results of this analysis are only generalizable to the medication classes assessed.
Conclusion
Blister-packaging medications has been shown to improve medication adherence, and adherence to medications for chronic conditions has also been shown to reduce HCRU and healthcare costs. This economic analysis estimated the potential impact of blister-packaging chronic medications on adherence and healthcare costs in a commercially insured population, indicating reductions of $0.73 PMPM for RAS antagonists, $0.29 PMPM for statins, $0.07 PMPM for oral antidiabetics, and $0.10 PMPM for DOACs. Future research is needed to confirm these findings in real-world settings and fully understand the economic implications of blister-packaging chronic medications.
Abbreviations
ACC, American College of Cardiology; ACEi, angiotensin-converting enzyme inhibitor; aCR, Adjusted Cost Ratio; AFib, Atrial Fibrillation; AHA, American Heart Association; aHR, Adjusted Hazards Ratio; AMI, Acute Myocardial Infarction; aOR, Adjusted Odds Ratio; ARB, Angiotensin-II Receptor Blocker; aRR, Adjusted Risk Ratio; CI, Confidence Interval; CMS, Centers for Medicare & Medicaid Services; COPD, Chronic Obstructive Pulmonary Disease; DOAC, Direct Oral Anticoagulant; DPP-4, Dipeptidyl Peptidase 4; GLP-1, Glucagon-Like Peptide 1; HCRU, Healthcare Resource Utilization; HF, Heart Failure; HRRP, Hospital Readmissions Reduction Program; IDN, Integrated Delivery Network; MTM, Medication Therapy Management; PBM, Pharmacy Benefits Manager; PDC, Proportion of Days Covered; PMPM, Per-Member Per-Month; PQA, Pharmacy Quality Alliance; QoL, Quality of Life; RAS, Renin-Angiotensin-System; SGLT2, Sodium-Glucose Cotransporter-2; T2DM, Type II Diabetes Mellitus; US, United States; VBC, Value Based Contracting; VTE, Venous Thromboembolism.
Acknowledgments
The authors would like to thank Ashley Taneja, PharmD and Mia Weiss, MPH, for their review of the model.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
Saad, Dumitru, and Lucaci are employees and shareholders of Becton, Dickinson and Company. Borrelli and Barnes are employees of Becton, Dickinson and Company. Barnes is a shareholder of BioMérieux. No other conflicts of interest to report.
References
1. Boersma P, Black LI, Ward BW. Prevalence of multiple chronic conditions among US adults, 2018. Prev Chronic Dis. 2020;17:E106. doi:10.5888/pcd17.200130
2. Aremu TO, Oluwole OE, Adeyinka KO, Schommer JC. Medication adherence and compliance: recipe for improving patient outcomes. Pharmacy. 2022;10(5):106. doi:10.3390/pharmacy10050106
3. Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155–159. doi:10.5001/omj.2011.38
4. Unni E. Medicine Use in Chronic Diseases. Pharmacy. 2023;11(3):100. doi:10.3390/pharmacy11030100
5. Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. doi:10.1136/bmjopen-2017-016982
6. Campbell PJ, Axon DR, Taylor AM, et al. Hypertension, cholesterol and diabetes medication adherence, health care utilization and expenditure in a medicare supplemental sample. Medicine. 2021;100(35):e27143. doi:10.1097/MD.0000000000027143
7. Campbell PJ, Axon DR, Taylor AM, et al. Associations of renin-angiotensin system antagonist medication adherence and economic outcomes among commercially insured us adults: a retrospective cohort study. J Am Heart Assoc. 2020;9(17):e016094. doi:10.1161/JAHA.119.016094
8. Chinthammit C, Axon DR, Anderson S, et al. A retrospective cohort study evaluating the relationship between statin medication adherence and economic outcomes in commercial health plans. J Clin Lipidol. 2020;14(6):791–798. doi:10.1016/j.jacl.2020.09.005
9. Chinthammit C, Axon DR, Mollon L, et al. Evaluating the relationship between quality measure adherence definitions and economic outcomes in commercial health plans: a retrospective diabetes cohort study. J Manag Care Spec Pharm. 2021;27(1):64–72. doi:10.18553/jmcp.2021.27.1.064
10. Deshpande CG, Kogut S, Willey C. Real-world health care costs based on medication adherence and risk of stroke and bleeding in patients treated with novel anticoagulant therapy. J Manag Care Spec Pharm. 2018;24(5):430–439. doi:10.18553/jmcp.2018.24.5.430
11. Deshpande CG, Kogut S, Laforge R, Willey C. Impact of medication adherence on risk of ischemic stroke, major bleeding and deep vein thrombosis in atrial fibrillation patients using novel oral anticoagulants. Curr Med Res Opin. 2018;34(7):1285–1292. doi:10.1080/03007995.2018.1428543
12. Axon DR, Vaffis S, Chinthammit C, et al. Assessing the association between medication adherence, as defined in quality measures, and disease-state control, health care utilization, and costs in a retrospective database analysis of Medicare supplemental beneficiaries using statin medications. J Manag Care Spec Pharm. 2020;26(12):1529–1537. doi:10.18553/jmcp.2020.26.12.1529
13. Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff. 2011;30(1):91–99. doi:10.1377/hlthaff.2009.1087
14. Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. doi:10.1097/01.mlr.0000163641.86870.af
15. Zhang Y, Flory JH, Bao Y. Chronic medication nonadherence and potentially preventable healthcare utilization and spending among medicare patients. J Gen Intern Med. 2022;37(14):3645–3652. doi:10.1007/s11606-021-07334-y
16. Foley L, Larkin J, Lombard-Vance R, et al. Prevalence and predictors of medication non-adherence among people living with multimorbidity: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e044987. doi:10.1136/bmjopen-2020-044987
17. Stewart SF, Moon Z, Horne R. Medication nonadherence: health impact, prevalence, correlates and interventions. Psychol Health. 2023;38(6):726–765. doi:10.1080/08870446.2022.2144923
18. Kogut SJ. A primer on quality measurement and reporting in pharmacy benefit plans. J Manag Care Spec Pharm. 2024;30(4):386–396. doi:10.18553/jmcp.2024.23240
19. Pharmacy Quality Alliance. PQA Measure Overview. Pharmacy Quality Alliance; 2022. Available from: https://www.pqaalliance.org/assets/Measures/PQA_Measures_Overview.pdf.
20. Hugtenburg JG, Timmers L, Elders PJ, Vervloet M, van Dijk L. Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Patient Prefer Adherence. 2013;7:675–682. doi:10.2147/PPA.S29549
21. Ágh T, Hiligsmann M, Borah B, et al. Systematic review of outcomes for assessment of medication adherence enhancing interventions: an ISPOR special interest group report. Value Health. 2024;27(2):133–142. doi:10.1016/j.jval.2023.10.016
22. Conn VS, Ruppar TM, Chan KC, Dunbar-Jacob J, Pepper GA, De Geest S. Packaging interventions to increase medication adherence: systematic review and meta-analysis. Curr Med Res Opin. 2015;31(1):145–160. doi:10.1185/03007995.2014.978939
23. Zedler BK, Joyce A, Murrelle L, Kakad P, Harpe SE. A pharmacoepidemiologic analysis of the impact of calendar packaging on adherence to self-administered medications for long-term use. Clin Ther. 2011;33(5):581–597. doi:10.1016/j.clinthera.2011.04.020
24. Leslie RS, Gilmer T, Natarajan L, Hovell M. A multichannel medication adherence intervention influences patient and prescriber behavior. J Manag Care Spec Pharm. 2016;22(5):526e538. doi:10.18553/jmcp.2016.22.5.526
25. Leslie RS, Tirado B, Patel BV, Rein PJ. Evaluation of an integrated adherence program aimed to increase Medicare part D star rating measures. J Manag Care Spec Pharm. 2014;20(12):1193e1203. doi:10.18553/jmcp.2014.20.12.1193
26. Hale G, Moreau C, Joseph T, et al. Improving medication adherence in an ACO primary care office with a pharmacist-led clinic: a report from the ACORN SEED. J Pharm Pract. 2021;34(6):888e893. doi:10.1177/0897190020934271
27. Hong M, Esse T, Vadhariya A, et al. Evaluating success factors of a medication adherence tracker pilot program in improving part D medication adherence metrics in a medicare advantage plan: importance of provider engagement. J Manag Care Spec Pharm. 2020;26(5):662e667. doi:10.18553/jmcp.2020.26.5.662
28. Daly CJ, Verrall K, Jacobs DM. Impact of community pharmacist interventions with managed care to improve medication adherence. J Pharm Pract. 2021;34(5):694e702. doi:10.1177/0897190019896505
29. Gutierrez PM, Wortzel HS, Forster JE, Leitner RA, Hostetter TA, Brenner LA. Blister packaging medication increases treatment adherence in psychiatric patients. J Psychiatr Pract. 2017;23(5):320–327. doi:10.1097/PRA.0000000000000252
30. Navin LS. Blister packaging medications for adherence for American Indians/Alaska natives in the outpatient setting. J Pharm Pract. 2021;34(1):97–102. doi:10.1177/0897190019851357
31. Leslie SR, Gwadry-Sridhar F, Thiebaud P, Patel BV. Calculating medication compliance, adherence and persistence in administrative pharmacy claims databases. Pharmaceutical Programming. 2008;1(1):13–19. doi:10.1179/175709208X334614
32. Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 budget impact analysis good practice ii task force. Value Health. 2014;17(1):5–14. doi:10.1016/j.jval.2013.08.2291
33. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford university press; 2015.
34. Caro JJ, Briggs AH, Siebert U, Kuntz KM. ISPOR-SMDM modeling good research practices task force. modeling good research practices - overview: a report of the ISPOR-SMDM modeling good research practices task force-1. Value Health. 2012;15(5):796–803. doi:10.1016/j.jval.2012.06.012
35. McIntosh E, Clarke PM, Frew EJ, Louviere JJ. Applied Methods of Cost-Benefit Analysis in Health Care.
36. Husereau D, Drummond M, Augustovski F, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II good practices task force. Value Health. 2022;25(1):10–31. doi:10.1016/j.jval.2021.10.008
37. Chobufo MD, Gayam V, Soluny J, et al. Prevalence and control rates of hypertension in the USA: 2017-2018. Int J Cardiol Hypertens. 2020;6:100044. doi:10.1016/j.ijchy.2020.100044
38. SHADAC: State Health Compare. Health Insurance Coverage Type. SHADAC; 2024. Available from: https://statehealthcompare.shadac.org/table/4/health-insurance-coverage-type-by-age#1/5,4,1,10,86,9,8,6,3,12,13,20,25,14,21,22,23,24,11/42/7,8.
39. Shah SJ, Stafford RS. Current trends of hypertension treatment in the United States. Am J Hypertens. 2017;30(10):1008–1014. doi:10.1093/ajh/hpx085
40. Matyori A, Brown CP, Ali A, Sherbeny F. Statins utilization trends and expenditures in the U.S. before and after the implementation of the 2013 ACC/AHA guidelines. Saudi Pharm J. 2023;31(6):795–800. doi:10.1016/j.jsps.2023.04.002
41. Centers for Disease Control and Prevention. national diabetes statistics report: estimates of diabetes and its burden in the United States. Centers for Disease Control; 2023. Available from: https://www.cdc.gov/diabetes/data/statistics-report/index.html.
42. Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med. 2021;384(23):2219–2228. doi:10.1056/NEJMsa2032271
43. Raval AD, Vyas A. National trends in diabetes medication use in the United States: 2008 to 2015. J Pharm Pract. 2020;33(4):433–442. doi:10.1177/0897190018815048
44. Pradaxa (dabigatran etexilate) [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals Inc; 2023. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=ba74e3cd-b06f-4145-b284-5fd6b84ff3c9.
45. Xarelto (rivaroxaban) [package insert]. Titusville, NJ: Janssen Pharmaceutical, Inc; 2023. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=10db92f9-2300-4a80-836b-673e1ae91610.
46. Eliquis (apixaban) [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2021. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e9481622-7cc6-418a-acb6-c5450daae9b0.
47. Savaysa (edoxaban tosylate) [package insert]. Basking Ridge, NJ: Daiichi Sankyo, Inc; 2024. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e77d3400-56ad-11e3-949a-0800200c9a66.
48. Turakhia MP, Shafrin J, Bognar K, et al. Estimated prevalence of undiagnosed atrial fibrillation in the United States. PLoS One. 2018;13(4):e0195088. doi:10.1371/journal.pone.0195088
49. Navar AM, Kolkailah AA, Overton R, et al. Trends in oral anticoagulant use among 436 864 patients with atrial fibrillation in community practice, 2011 to 2020. J Am Heart Assoc. 2022;11(22):e026723. doi:10.1161/JAHA.122.026723
50. Weller SC, Porterfield L, Davis J, Wilkinson GS, Chen L, Baillargeon J. Incidence of venous thrombotic events and events of special interest in a retrospective cohort of commercially insured US patients. BMJ Open. 2022;12(2):e054669. doi:10.1136/bmjopen-2021-054669
51. Iyer GS, Tesfaye H, Khan NF, Zakoul H, Bykov K. Trends in the Use of Oral Anticoagulants for Adults With Venous Thromboembolism in the US, 2010-2020. JAMA Netw Open. 2023;6(3):e234059. doi:10.1001/jamanetworkopen.2023.4059
52. Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 2020;4(19):4693–4738. doi:10.1182/bloodadvances.2020001830
53. US Inflation Calculator. Health care inflation in the United States (1948-2024). US Inflation Calculator; Available from: https://www.usinflationcalculator.com/inflation/health-care-inflation-in-the-united-states/.
54. Crimmel BL. Changes in self-insured coverage for employer-sponsored health insurance: private sector, by firm size, 2001-2011. In: Statistical Brief (Medical Expenditure Panel Survey (US)) [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2001. STATISTICAL BRIEF #412.
55. Kaiser Family Foundation. 2023 Employer Health Benefits Survey. Kaiser Family Foundation; 2023. Available from: https://www.kff.org/report-section/ehbs-2023-section-10-plan-funding/.
56. Evans M, Engberg S, Faurby M, Fernandes JDDR, Hudson P, Polonsky W. Adherence to and persistence with antidiabetic medications and associations with clinical and economic outcomes in people with type 2 diabetes mellitus: a systematic literature review. Diabetes Obes Metab. 2022;24(3):377–390. doi:10.1111/dom.14603
57. Majeed A, Rehman M, Hussain I, et al. The impact of treatment adherence on quality of life among type 2 diabetes mellitus patients - findings from a cross-sectional study. Patient Prefer Adherence. 2021;15:475–481. doi:10.2147/PPA.S295012
58. Brook RA, Beren IA, Drnach AA, et al. POSB138 medication adherence impacts lost time, productivity costs and emergency room visits in employees with diabetes. Value in Health. 2022;25(1):S87. doi:10.1016/j.jval.2021.11.1271
59. Chantzaras A, Yfantopoulos J. Association between medication adherence and health-related quality of life of patients with diabetes. Hormones. 2022;21(4):691–705. doi:10.1007/s42000-022-00400-y
60. Giffords B, Geppert P, Zayance R, Lin R The impact of medication adherence on workplace productivity outcomes: a review of the scientific evidence and example for calculating savings from improved adherence. Integrated Benefits Institute; 2018. Available from: https://www.ibiweb.org/resources/the-impact-of-medication-adherence-on-workplace-productivity-outcomes.
61. Branning G, Lynch M, Hayes K. Value-Based Agreements in Healthcare: willingness versus Ability. Am Health Drug Benefits. 2019;12(5):232–234. doi:10.1377/hblog20161104.057443/full/
62. Centers for Medicare & Medicaid Services. Hospital readmissions reduction program (HRRP). Centers for Medicare & Medicaid Services. 2023. Available from: https://www.cms.gov/medicare/payment/prospective-payment-systems/acute-inpatient-pps/hospital-readmissions-reduction-program-hrrp.
63. Kee A, Maio V. Value-based contracting: challenges and opportunities. Am J Med Qual. 2019;34(6):615–617. doi:10.1177/1062860619862756
64. Uitvlugt EB, Janssen MJA, Siegert CEH, et al. Medication-related hospital readmissions within 30 days of discharge: prevalence, preventability, type of medication errors and risk factors. Front Pharmacol. 2021;12:567424. doi:10.3389/fphar.2021.567424
65. Carnicelli AP, Li Z, Greiner MA, et al. Sacubitril/valsartan adherence and postdischarge outcomes among patients hospitalized for heart failure with reduced ejection fraction. JACC Heart Fail. 2021;9(12):876–886. doi:10.1016/j.jchf.2021.06.018
66. Rosen OZ, Fridman R, Rosen BT, Shane R, Pevnick JM. Medication adherence as a predictor of 30-day hospital readmissions. Patient Prefer Adherence. 2017;11:801–810. doi:10.2147/PPA.S125672
67. ElSayed NA, Aleppo G, Bannuru RR, American Diabetes Association Professional Practice Committee. Pharmacologic approaches to glycemic treatment: standards of care in Diabetes—2024. Diabetes Care. 2024;47(Suppl 1):S158–S178. doi:10.2337/dc24-S009
68. Rind D, Guzauskas G, Fazioli K, et al. Oral semaglutide for type 2 diabetes: effectiveness and value. Institute for Clinical and Economic Review. 2021. Available from: https://icer-review.org/material/diabetes-finalevidence-report-and-meeting-summary/.
69. Fazioli KT, Rind DM, Guzauskas GF, Hansen RN, Pearson SD. The effectiveness and value of oral semaglutide for type 2 diabetes mellitus. J Manag Care Spec Pharm. 2020;26(9):1072–1076. doi:10.18553/jmcp.2020.26.9.1072
70. American Diabetes Association Professional Practice Committee. Cardiovascular disease and risk management: standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S179–S218. doi:10.2337/dc24-S010
71. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: executive summary: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2022;145(18):e876–e894. doi:10.1161/CIR.0000000000001062
72. Elendu C, Elendu RC, Enyong JM, et al. Comprehensive review of current management guidelines of chronic kidney disease. Medicine. 2023;102(23):e33984. doi:10.1097/MD.0000000000033984
73. Rind DM, Agboola F, Kumar VM, Borrelli E, Pearson SD Unsupported Price Increase Report: 2019 Assessment. Institute for Clinical and Economic Review. 2019. Available from: https://icer.org/wp-content/uploads/2020/10/ICER_UPI_Final_Report_and_Assessment_110619.pdf.
74. Rind DM, Agboola F, Chapman R, Borrelli E, McKenna A, Pearson SD Unsupported price increase report: 2020 assessment. Institute for Clinical and Economic Review. 2021. Available from: https://icer.org/assessment/unsupported-price-increase-2021/.
75. Rind DM, Agboola F, Nikitin D, et al. Unsupported price increase report: unsupported price increases occurring in 2020. Institute for Clinical and Economic Review. 2021. Available from: https://icer.org/assessment/unsupported-price-increase-2020/.
76. Rind DM, Agboola F, Campbell J, Nikitin D, McKenna A, Pearson SD Unsupported PRICE INCREASE REPORT: UNSUPPORTED PRICE INCREASES OCCURRING in 2021. Institute for Clinical and Economic Review. 2022. Available from: https://icer.org/assessment/upi-2022/.
77. Rind DM, Agboola F, Nikitin D, et al. Unsupported price increase report: unsupported price increases occurring in 2022. Institute for Clinical and Economic Review. 2023. Available from: https://icer.org/wp-content/uploads/2023/12/UPI_2023_Report_121123.pdf.
78. DC G Jr, Lloyd-Jones DM, Bennett G, et al. American college of cardiology/American heart association task force on practice guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S49–73. doi:10.1161/01.cir.0000437741.48606.98
79. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi:10.1378/chest.09-1584
80. Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish atrial fibrillation cohort study. Eur Heart J. 2012;33(12):1500–1510. doi:10.1093/eurheartj/ehr488
81. ElSayed NA, Aleppo G, Bannuru RR, American Diabetes Association Professional Practice Committee. Chronic kidney disease and risk management: standards of care in Diabetes—2024. Diabetes Care. 2024;47(Suppl 1):S219–S230. doi:10.2337/dc24-S011
82. Iglay K, Hannachi H, Joseph Howie P, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243–1252. doi:10.1185/03007995.2016.1168291
83. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Enhancing Outcomes in Opioid Use Disorder Treatment: An Economic Evaluation of Improving Medication Adherence for Buprenorphine Through Blister-Packaging
Borrelli EP, Saad P, Barnes NE, Nelkin H, Dumitru D, Lucaci JD
Substance Abuse and Rehabilitation 2024, 15:209-222
Published Date: 22 October 2024


