Back to Journals » Risk Management and Healthcare Policy » Volume 17
Improving the Process of Managing Psychosocial Risks in Organizations
Authors Saik P, Tsopa V, Cheberyachko S, Deryugin O, Sokurenko S, Suima I, Lozynskyi V
Received 23 July 2024
Accepted for publication 28 November 2024
Published 5 December 2024 Volume 2024:17 Pages 2997—3016
DOI https://doi.org/10.2147/RMHP.S488263
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Pavlo Saik,1 Vitaliy Tsopa,2 Serhii Cheberyachko,3 Oleg Deryugin,3 Svitlana Sokurenko,3 Iryna Suima,3 Vasyl Lozynskyi1,3
1Belt and Road Initiative Center for Chinese-European Studies (BRICCES), Guangdong University of Petrochemical Technology, Maoming, People’s Republic of China; 2International Institute of Management, Kyiv, Ukraine; 3Dnipro University of Technology, Dnipro, Ukraine
Correspondence: Vasyl Lozynskyi, Email [email protected]
Introduction: Psychosocial risks (PSRs) are identified as one of the main modern occupational safety issues, primarily related to occupational stress, and need to be reduced to safe levels in accordance with international requirements. The research purpose is to improve the process of managing the PSRs in the occupational safety and health management systems of employees, taking into account the impact of psychosocial dangers in accordance with the requirements of ISO 45001:2018 and ISO 45003:2021 standards.
Methods: To develop the process of managing the PSRs, a system analysis method is applied, which allows determining the structural relationships between the variable elements of dangerous psychosocial factors described in the ISO 45003:2021 standard.
Results: The bow-tie model has been improved to determine the relationship between psychosocial dangers and the dangerous event occurrence – experiencing stress by an employee, taking into account the influence of various dangerous psychosocial factors, which provides for an additional risk level assessment for restoring the health of an employee who has experienced stress. The process of psychosocial risk management consisting of ten steps is proposed, which involves identifying the relationship between psychosocial dangers and consequences for human health, taking into account the impact of various dangerous psychosocial factors based on questionnaires, followed by analysis and processing of the duration and intensity of experiencing stress. To reduce the impact of subjective assessments of the duration and intensity of experiencing stress on the psychosocial risk level, it is proposed to take into account the value of individual perception of experiencing stress (stress resistance) and the employees’ health condition.
Discussion: The scientific novelty is to determine the psychosocial risk level as the sum of the risk values from the impact of each dangerous psychosocial factor, which are characteristic of aspects of work organization, social conditions at work, working environment, equipment, dangerous tasks and the level of employee health. The practical value is the development of scales for assessing the impact of dangerous psychosocial factors and a form for documenting the process of managing psychosocial risks with the indication of precautionary measures to control them.
Keywords: psychosocial risk, dangers, stress, psychosocial factor, managerial decisions
Introduction
Psychosocial risks (hereinafter referred to as PSRs) at work provoke diseases among employees.1 Exposure to stress reduces employees’ well-being and leads to significant economic and social losses, as well as is a dangerous factor of occupational risks.2 According to the estimates of various scientific studies,3–6 50–60% of all lost working days for the disease in the EU are associated with stress. This includes the development of occupational diseases (professional burnout, emotional exhaustion, symptoms of depression and musculoskeletal disorders, etc.7) and oncological diseases.8 This situation requires the top management of organizations to take appropriate precautionary measures to reduce psychosocial risks. For example, the development of the concept of a healthy and safe workplace,9 which includes not only a traditional safe physical environment, but also a healthy psychosocial environment, safe epidemic environment, safe infectious environment, and a healthy lifestyle of the employee. The development of such a concept is convenient based on the requirements of a number of international standards: ISO 45001, ISO 45002, ISO 45003, ISO 45004, ISO/PAS 45005 and ISO 45006 (Figure 1). It is based on the risk management process: that is, to identify dangers, dangerous external or internal factors that increase the probability of a dangerous event occurrence and the severity of consequences, as well as to justify precautionary/protective measures to avoid costs associated with work-related injuries, disabilities and diseases.10,11
 |
Figure 1 A contemporary vision of a healthy and safe workplace based on a number of international standards ISO 4500Х. |
Of the components of the safe and healthy workplace concept listed, the most questions regarding the consistency of risk management procedures arise precisely in relation to the definition of psychosocial risks. Since they are characterized by “the interaction of the working environment, work organization”, etc. with the abilities, needs and concerns of employees, which affects the health condition through the influence of stress.12 There is a difference between physical dangers and psychosocial dangers – stress. Physical dangers are characterized by specific circumstances that can lead to injury or deterioration of employees’ health. Psychosocial dangers (dangerous factors), as defined by the ISO 45003:2021 standard Occupational Health and Safety Management – Psychological Health and Safety at Work – Guidelines for Managing Psychosocial Risks, are specific events that are related to work organization, aspects of working environment and can cause psychological, social or physical harm to employees. In other words, the term “psychosocial danger” is defined as a dangerous factor in the interaction between psychological, physiological and working environment factors.13 In addition, their impact is related to the individual susceptibility of employees, which necessitates the assessment of psychosocial risks.14 It is also difficult to identify the severity of the consequences of psychosocial risks. For example, according to WHO (World Health Organization), a negative reaction in employees experiencing stress occurs when job demands and pressures do not correspond to the employees’ abilities.12 Some people are known to be more susceptible to the effects of stress, depression and anxiety15,16 with long-term consequences on the quality of their professional life. At the same time, the impact of physical or chemical dangers is often characterized by a linear relationship between the values of harm and danger, rather than psychosocial danger – stress.17
Note that many organizations have legal obligations to conduct occupational risk assessments for all workplaces and activities to protect the health of employees and prevent accidents or other harmful effects of employees’ work.18 For this purpose, an occupational safety and health management system is often implemented in accordance with the requirements of ISO 45001:2018 «Occupational health and safety management systems – Requirements with guidance for use». Hence, there is an urgent task to develop a process for managing not only occupational risks, but also the PSRs, which can be easily integrated with other risk management processes (physical, chemical, infectious, and others).
The analysis of studies has shown that the priority direction of research on this issue is aimed primarily at studying the PSR impact on the effectiveness of the organization’s activities,18 since their presence increases the number of days of inability to work19,20 and accidents, medical care costs and staff turnover.21 The demand for such research is understandable, as there is a need for financial support of precautionary measures to reduce the level of occupational stress.22 At the same time, more interesting are studies on determining the relationship between long-term exposure to occupational stress and the emergence of distress, which depends, among other things, on the health condition, including, for example, mental disorders, cardiovascular diseases.23 In addition, of interest are studies on counterproductive behavior, sabotage, interpersonal conflicts with colleagues, subordinates or managers due to the presence of stressful tension, which ultimately worsens the effectiveness and efficiency of the organization’s activities,24 the quality of products (services).3,25,26 Also important are studies on the negative impact of occupational stress on employee well-being due to the exhaustion of personal resources.27 However, all of the above research papers do not describe the process of managing the PSRs. Some of them only indicate their importance.28,29 Unfortunately, the number of such studies is not significant. This may be due to the complexity of determining risk as the product of the probability of a dangerous event occurrence and the severity of the consequences, which in this case significantly depends on the individual characteristics of a person, his/her stress resistance, religious beliefs, and family circumstances.30 There are studies31–34 on the development of questionnaires to identify psychosocial factors (stressors) in the workplace, and then a qualitative description of the impact on mental health of working conditions is conducted, which is difficult to compare in the conditions of one organization, not to mention the conditions at different enterprises. There is also a problem with the interpretation of conclusions by different experts: psychologists, psychotherapists, psychoanalysts and ordinary occupational safety engineers who are responsible for reducing the PSRs.35 In addition, there is a significant difference between psychological and social dangers, which require the development of various measures to reduce the impact on the health of employees.36
The conducted analysis of scientific research suggests the existence of certain gaps in the substantiation of PSR management process in the organization’s occupational health and safety management system. This requires conducting appropriate research to find answers to questions about the consistency of the process of managing psychosocial risks in occupational safety and health management systems in specific settings, as well as to identify not only occupational risks but also psychosocial risks and assess their level, as well as develop appropriate precautionary measures to reduce them to an acceptable level.
The purpose of the research is to improve the process of managing the PSRs in the occupational health and safety management systems of employees in accordance with the requirements of ISO 45001:2018 and ISO 45003:2021 standards.
Materials and Methods
A system analysis method is used to develop the PSR management process.37 It allows determining the structural relationships between the variable elements of dangerous psychosocial factors described in ISO 45003:2021 standard, and the probability of a dangerous event occurrence (experiencing stress by an employee) and the severity of consequences (development of occupational diseases).
To assess psychosocial risks, the bow-tie method is used, which is described in IEC 31010:2019 Risk Management – Risk Assessment Techniques (Figure 2). This method is quite common and is used in many industries.38–40 It is a composition of a fault tree and an event tree, taking into account the impact of a dangerous event occurrence on the root causes of various dangerous psychosocial factors. Its use allows for a good visualization of the chain between the root cause, a dangerous event and its consequences, thereby identifying not only protective barriers, but also dangerous factors that increase the probability or severity of consequences.35
 |
Figure 2 Model of psychosocial risk management based on the ISO 45003 standard requirements using the bow-tie method. |
The choice of the bow-tie method for psychosocial risk assessment is related to the possibility of implementing all the steps: from identifying the dangers to monitoring the effectiveness of precautionary measures, as specified in the IEC 31010:2019 standard. The bow-tie method is based on a cause-and-effect relationship: psychosocial danger – stress that can lead to a dangerous event – experiencing stress by an employee under the influence of several groups of dangerous psychosocial factors (aspects of work organization, social factors at work, working environment, equipment, dangerous tasks, employee’s health level, etc). Using a system analysis, it is supposed to identify the impact of potentially dangerous psychosocial factors, as well as to analyze the ability of available resources, such as support, feedback, dedication, and good physical and mental health, to reduce the severity of consequences. The selection of these groups of dangerous psychosocial factors is primarily due to the recommendations of ISO 45003:2021 standard. The identification of these groups of dangerous psychosocial factors has also been confirmed by various scientific studies. They indicate the existing relationship between the employee’s experience of stress and the impact of work organization41,42 lack of support from management or coworkers,43,44 performing dangerous tasks.45,46 The impact of dangerous tasks on the employee’s experience of stress is associated with high demands for performing such tasks, which lead to the need to take appropriate measures and strategies to actively respond to these demands.47 It is believed that this disrupts a person’s internal state of stability, which can lead to stress.48
Questionnaires are used to determine the impact of psychosocial dangerous factors. Their analysis is supposed to identify not only dangerous psychosocial factors, but also indicators of the intensity and duration of experiencing stress. The practice of using questionnaires is quite widespread.49,50 There are a significant number of such developments.49 Thus, to reduce the influence of subjectivity and increase the reliability of such approaches, it is recommended to use a combination of several different questionnaires,51 to use exploratory factor analysis (EFA),52 for example, through the use of the Gonzaga’s School of Business online application (https://analytics.gonzaga.edu/parallelengine/).
Research Results
Based on the bow-tie method model, an improved model has been developed for managing the PSRs in accordance with ISO 45003:2021 standard, which provides for consideration of additional psychosocial risk, taking into account the employee’s health recovery (Figure 3). Its development arises from the need to create appropriate safe working conditions for employees who restore their mental health after experiencing occupational stress and their adaptation when returning to work.
 |
Figure 3 Proposed model for managing psychosocial risk of stress. |
This will allow, at least, the organization’s managers to develop measures for psychological support (recovery) of employees upon returning to work, as well as to ensure the level of occupational physical and psychological load in accordance with the individual capabilities of such an employee.
Hence, there is a need to identify dangerous psychosocial factors that negatively affect the recovery of mental health and adaptation of an employee when returning to work. In particular, protection of violated rights of employees, especially in moments of greatest vulnerability, avoidance of forced execution of dangerous tasks, bullying, lack of support, etc.53
The difference of the proposed bow-tie method model for managing PSRs is also the consideration of physical and mental individual characteristics of a person as an additional factor influencing psychosocial risk.
Based on the proposed bow-tie method model (Figure 4), a PSR management process has been developed that includes eleven steps aimed at identifying the relationship between psychosocial danger – stress and human health consequences, taking into account the influence of various dangerous psychosocial factors on the level of psychosocial risk of stress.
 |
Figure 4 Process of psychosocial risk management. |
The first step is to identify the psychosocial danger – stress, the dangerous event – experiencing stress and possible consequences, based on a study of the production environment with its characteristic dangerous factors. It is convenient to use different models for this step.54 For example, the JD-R model, linking the demands to employees with their available capabilities, which makes it possible to identify psychosocial dangers that lead to experiencing stress.55
It is also convenient to apply the Job Demands – Control – Support model, illustrating how job demands can cause stress for employees, such as heavy workload, role ambiguity, and work-related stress.56 Using these models, determine the relationships between psychosocial dangers and dangerous events, the probability of which is increased by dangerous psychosocial factors and the severity of consequences – injuries or the development of occupational diseases. We document all the information, and, as an example, you can see Table 1.
 |
Table 1 Form of the Register of Dangerous Psychosocial Factors |
The second step is to identify the dangerous psychosocial factors that affect the psychosocial risk level based on the use of a questionnaire. Various well-known questionnaires, such as Copenhagen Psychosocial Questionnaire (COPSOQ; COPSOQ II, COPSOQ III), can be used.57 However, there is a need to process and revise them to assess dangerous psychosocial factors in accordance with the working environment and the mentality of employees. An example of a fragment of such a questionnaire, developed in accordance with the groups of dangerous factors specified in the ISO 45003:2021 standard for one of the mining enterprises, is given in Table 2. To form it, a combination of various existing approaches was used to determine the level of perceived PSS-1058 or to measure GAD-7 anxiety symptoms.59 The peculiarities of the proposed questionnaire include determining the duration and intensity of experiencing stress from the specified dangerous psychosocial factor using the Sten scale, where 1 means no stress, and 10 means significant intensity and duration of stress.60 It is believed that the severity of health consequences can be determined based on the intensity and duration of experiencing stress.61–63
 |
Table 2 Questionnaire to Identify Dangerous Psychosocial Factors (Fragment) |
The third step involves surveying employees about the intensity and duration of experiencing stress and the frequency of experiencing stress from various dangerous psychosocial factors. In this case, statistical analysis reveals significant dangerous psychosocial factors. For example, with the help of STATISTICA (Dell Technologies, Round-Rock, Texas, USA) software, which conveniently uses the Mann–Whitney U-test to assess differences in stress experience and its perception.64 Based on the identified significant dangerous psychosocial factors, it is necessary to form their register. This will make it possible to clarify the impact of dangerous psychosocial factors at specific time intervals. Having a register of dangerous psychosocial factors will help identify the effectiveness of precautionary measures to reduce the experience of stress.
At the fourth step, determine the level of total PSR at the employee’s workplace by the sum of all identified psychosocial risks from the impact of each dangerous psychosocial factor - i
where R – is the psychosocial risk value; Ri – is the psychosocial risk value from the impact of each dangerous psychosocial factor – i.
For example, two approaches are proposed for determining the PSR value depending on the influence of each psychosocial factor. The first approach is based on the understanding that the PSR level from exposure to i – a dangerous psychosocial factor is determined by the formula as a combination of the probability (frequency) of occurrence of a work-related psychosocial danger and the severity of consequences in terms of health deterioration, as specified in ISO 45003:2021 standard:
where, Fri – is the frequency of stress experience; Si – is the severity of stress experience consequences.
In this case, the probability of experiencing stress by an employee is convenient to determine by the frequency of occurrence of a stressful situation. The ten-score scale for determining the frequency of stress experience occurrence is shown in Table 3. It was formed based on the relationship between the frequency of experiencing stress by employees and the possible development of mental disorders (depression, anxiety, sleep disturbances, deterioration of the immune and cardiovascular systems, etc).65–67
 |
Table 3 Frequency Scale of the Stress Experience Occurrence (Fr) |
Table 2 is based on the assumption that the more often a person is exposed to stress, the more the psychosocial risk level increases.68–70 However, there is a significant number of publications indicating that the deterioration of mental health from the frequency of stress experience is ambiguous, the dependence is quite complex71 and requires taking into account individual characteristics of a person (for example, stress resistance).72 At the same time, the proposed scale allows for a qualitative comparison of the number of stressful situations experienced by an employee in the production environment. At least, this approach makes it possible to identify psychosocial dangerous factors. Of course, it needs to be improved based on the analysis of a significant amount of accumulated research. At the same time, the method for determining psychosocial risk should not be too complicated. Otherwise, it will be impossible to involve employees in enterprises for its implementation, which is required by ISO 45001 standard. It should be noted that the involvement of employees in the process of managing the PSRs is one of the important aspects of the successful management system operation in organizations, which is confirmed by scientific evidence.73,74
To create the scale of severity of stress experience consequences (Table 3), we use the recommendations from.75,76 More details about the development of frequency scales (or probability) of a dangerous event occurrence and the scale of severity of consequences are disclosed in the paper.77 By combining the scales of frequency of stress experience occurrence (Table 2) and severity of consequences of experiencing it (Table 3), a simple matrix can be constructed to determine the PSR level (Table 4). It is a two-dimensional grid. On one axis, there are categories of severity of consequences, and on the other, there are categories of frequency of stress experience occurrence. The cells within the grid determine the psychosocial risk level. A difficult point in constructing such risk assessment matrices is determining the number of cells with an unacceptable risk.76,78 For this purpose, it is recommended to use the method based on the iso-risk contour.7 Low-risk cells are located below and to the right of the 30 iso-risk line, and highest-risk cells are located above and to the left of the 60 iso-risk line.
 |
Table 4 Severity of Stress Experience Consequences (Si) |
Thus, the unacceptable psychosocial risk level is in the range of 60 to 100 scores, and the acceptable psychosocial risk level is from 1 to 27. The range from 27 to 60 scores refers to acceptable risk level with control. However, the proposed risk assessment matrix is an example (Table 5) and needs improvement, based on the conditions of use in a particular organization.
 |
Table 5 PSR Assessment Matrix |
Given that the relationship between the frequency of stress experience and the psychosocial risk level is complex and often depends on the individual level of physical health of the employee, as well as his/her stress resistance, a second approach is proposed. Determination of the PSR level takes into account the employee’s stress resistance, intensity and duration of stress experience, the employee’s health condition through the use of appropriate coefficients. Then, formula (1) will be transformed into:
where ICi - is the intensity of stress experience; ISR - is index of stress resistance, from 0 to 1, in this case 0 – absolutely stress-resistant employee, 1 – absolutely stress-susceptible employee; DEi - is duration of stress experience; IHC - is index of employee’s health condition, from 0 to 1, in this case 0 – absolutely healthy, 1 – severely ill.
To determine the intensity and duration of stress experience, the following scales are proposed, given in Tables 6 and 7. For their construction, similar approaches are used, described in,60,65,66 as well as in.7
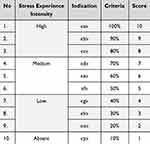 |
Table 6 Scale of Stress Experience Intensity (IC) |
 |
Table 7 Scale of the Stress Experience Duration (DE) |
There is a difficulty, both in constructing three-dimensional matrices for determining risk based on three criteria, and in its use in organizations. In this approach, the following indicators are used to determine the psychosocial risk level: frequency of occurrence, intensity and duration of stress experience.54,79 To avoid creating such a three-dimensional matrix, we develop a matrix for determining the severity of consequences based on a grid between intensity and duration. The possibility of its development stems from the revealed dependence of the deterioration of a person’s physical and mental health on the intensity and duration of stress experience.28,32,80,81
Using the stress intensity (Table 6) and duration (Table 7) scales, we construct a matrix for assessing the severity of the consequences, which is shown in Table 8. These values of the severity of consequences have been reduced by a factor of ten so that they can be compared with the data for the PSR matrix assessment (Table 5).
 |
Table 8 Matrix for Assessing the Severity of Stress Intensity and Duration Consequences |
To do this, we use the recommendations given in,76,82 which provide a specific peculiarity of scaling discrete categories of stress intensity and duration.
The well-known Connor-Davidson Resilience Scale (CD-RISC),83 Resilience Scale for Adults (RSA),84 or Resilience Scale for Mexicans (RESI-M) can also be used to determine the employee’s stress resistance coefficient.85 These scales are based on assessing employees’ ability to cope with stress/change, self-esteem/confidence level, social problem-solving skills, sense of humor, etc. At the same time, their direct use to determine the psychosocial risk level, in particular the severity of stress consequences, is impossible, due to the difference in the estimated indicators in the above scales. Using their principles of construction, which are based on a quantitative indicator that determines a person’s resistance to stress based on a physiological response, a scale is proposed (Table 9) that is compatible with the proposed approach to assessing PSR. Description of stress resistance coefficients is made in accordance with the data described in the studies of physiological recovery after experienced stressful situation based on the analysis of electrocardiography, electromyography, electrocutaneous activity and respiration to assess the physiological characteristics of stress resistance.86–88 It is proposed to set a scale for determining the coefficient of the employee’s physical health condition from the medical history of employees or from determining their physical activity.89 In this case, the scale is based on the assessment of a person’s cardio fitness from 0.1 to 1, where 0.1 characterizes poor health, and 1 – good physical condition (Table 10). The approach described in90 can also be used.
 |
Table 9 Employee’s Stress Resistance Coefficient (ISR) |
 |
Table 10 Employee’s Physical Health Condition Coefficient (IHC) |
In the fifth step, assess the PSRs in accordance with the risk matrix (Table 5) as acceptable, acceptable with control, or not acceptable Risk acceptance criteria for each organization are determined based on the well-known ALARP approach (that is, as low as is practicable).91
In the sixth step, determine the actions to control the total PSR, if the risk is determined to be acceptable with control. To do this, additional and unscheduled conversations, surveys, etc. are conducted with employees to determine whether they experience stress, how often, and of what intensity and duration, and primarily with employees with low stress resistance and health condition.
The seventh step is the processing of psychosocial risk, where precautionary and protective measures are determined to reduce the probability, intensity and duration of stress experience. For this purpose, a plan is developed to reduce dangerous psychosocial factors (Table 11), which includes the following:
 |
Table 11 An Example of a Plan to Reduce Dangerous Psychosocial Factors |
1) precautionary and protective measures to prevent or reduce the frequency, intensity, and duration of stress experience through additional breaks, changes in technology, equipment, workplace, use of fitness trackers, etc.92,93 (first level);
2) training employees to cope with the stress experience (meditation, mindfulness, cognitive-behavioral therapy94,95), to increase stress resistance (mobile applications are used to implement this approach96) (second level);
3) measures to restore the health level of employees affected by stress experience and their adaptation to work, as well as providing the necessary services and resources to support them at the initial stage of returning to the workplace97,98 (third level).
To provide support to employees at the initial stage of returning to the workplace, it is necessary to determine the risk of their health recovery. This is due to the continued experience of negative effects of the disease (including pain, fatigue, and bad mood) after the main treatment.53,97–99
Taking into account changes in the psychosocial risk level from the initial level to an unacceptable level, which caused the employee’s disease and partial recovery of his/her health, it is necessary to take into account changes in the stress resistance coefficient – ISR and the employee’s health condition – IHC, which are not fully restored after stress-related diseases. This means that such employees will have a relatively high initial psychosocial risk level (Figure 5). When such employees experience a stressful event, they are more likely to exceed the acceptable risk level. This leads to a relapse of the disease. Therefore, such employees need to be given more attention when returning to work and providing support during work.
To calculate the risk of health recovery, we propose to replace the health condition coefficient IHC in formula 3 with the employee’s health recovery rate (IRC):
To determine the health recovery rate, we suggest using the Self-Assessment Revised Version (RSA-R) recovery scale developed by the Yale School of Medicine.20,100 Its authors note that it will be useful for developing plans to improve care for people recovering from mental diseases. The questionnaire consists of 32 questions to which the person answers. Each answer is rated on a scale of 1 to 5.20 A higher score means that the person’s health is recovered.20,101
The health recovery rate values are given in Table 12.
 |
Table 12 Employee’s Health Recovery Rate (IRC) |
In the eighth step, document all the information received on the identification of psychosocial risks, for example, according to the proposed form (Table 13).
 |
Table 13 Form for PSR Management Report |
In the ninth step, the organization’s management approves a register of psychosocial risks and precautionary measures to reduce their impact on employees. We also develop a plan to monitor the effectiveness of measures to reduce psychosocial risk level with appropriate deadlines and necessary resources. In the last step, it is planned to review the register of dangerous psychosocial factors and the effectiveness of measures to control them, or in case of changes in production activities at least once a year: new products or services; modernization, reconstruction, changes in equipment or processes; conditions of martial law, etc.
Discussion
Management of PSRs is one of the main challenges in the field of occupational safety due to their potential impact on stress related to occupational safety, health protection and well-being of employees in the workplace.102 The need to create a process for managing PSRs will also allow managers of organizations to respond quickly to changes in technology, equipment or the organization of the production process.7,24,103 It is also important, in order to achieve effectiveness, that the process of managing the PSRs is integrated with other processes that already operate in organizations.104 Therefore, the proposal to use a model for assessing the PSRs based on the bow-tie method will allow combining the procedures for assessing different types of risks in the occupational safety and health management system of employees, since it is most often used in organizations.13,16,105 It is clear that whatever the nature of precautionary and protective measures developed to reduce the risks of stress in the workplace, they should be evidence-based, adaptable to existing workplaces, comprehensive and timely. The implementation of measures should be well planned and resourced and involve those affected or potentially affected by stress.
The management of PSRs has certain peculiarities that are associated with an additional assessment of the risk level of an employee’s health recovery. This will ensure a quick employee’s health recovery, reducing the impact of various dangerous factors that are somehow present in the workplace.23 At the same time, there is a need to improve the process of managing the PSRs by developing appropriate procedures: identifying dangerous psychosocial factors, assessing individual stress resistance, etc. In this case, it is important to use the existing theory of stress,106 as well as tested empirical relationships between the development of diseases and the level of stress experience, to ensure the reliability of PSR assessment.
The proposed process of PSR management involves time control and type of dangerous psychosocial factors. This allows you to find out the level of stress impact on a person’s health condition. It will also help to determine the effectiveness of the measures: whether the threat has actually been reduced. Time control involves long-term monitoring of exposure to dangerous psychosocial factors in order to record different variations and compare them with real health complaints,103,107 thereby minimizing subjective assessments, such as short-term biases in responses due to mood or recall of previous responses.
In addition, to increase the reliability of the described process of managing PSRs, it is necessary to constantly monitor the conditions of the working environment in which employees perform their duties in order to better understand the influence of certain types of dangerous psychosocial factors.
This research has identified and reviewed three main groups of precautionary measures that meet the specified criteria for reducing stress exposure. The research classified the measures into those that had an organizational, systemic and individual focus. Focusing on only one direction will not allow achieving the desired result.108
Work-related stress is closely related to the way work is planned, managed and organized. In the literature, several sources of stress are often distinguished (often referred to as “psychosocial dangers”):2 they include work-related stressors, organizational roles, work relationships, career development, organizational structure and team psychological climate. The stress process can be generalized through sources of stress, stress responses, long-term consequences of stress and individual characteristics of employees, as well as their interrelationships (Figure 6).
 |
Figure 6 Model of the cause-and-effect chain “source of stress – stress – individual characteristics of the employee’s perception of stress – stress response – stress response consequences”. |
A growing body of evidence suggests that when stress responses last for a long period of time, it can lead to more persistent, less reversible health consequences: such as chronic fatigue, exhaustion, musculoskeletal problems, or cardiovascular diseases. Individual characteristics, such as personality, values, goals, age, gender, education level and family situation, can influence a person’s ability to cope. These characteristics can either enhance or mitigate the effects of risk factors in the workplace and, in turn, stress experience. In particular, an inadequate psychosocial working environment that influences productivity and, moreover, the health of the organization: namely, job satisfaction, morale, productivity, turnover, absence, presentability and organizational commitment.
Conclusions
The bow-tie method model has been improved to determine the relationship between psychosocial danger – stress and the dangerous event occurrence – experiencing stress by an employee, taking into account the influence of various dangerous psychosocial factors, which provides for an additional assessment of the psychosocial risk level for recovering the health of an employee who has experienced stress.
A psychosocial risk management process consisting of ten steps is proposed, which involves determining the relationship between psychosocial danger and human health consequences, taking into account the influence of various psychosocial dangerous factors using questionnaires, followed by analysis and study of the duration and intensity of stress experience.
It is proposed to determine the psychosocial risk level as the sum of the risk values from the influence of each dangerous psychosocial factor, which are characteristic of the following groups of dangerous factors: aspects of work organization, social conditions in the workplace, working environment, equipment, dangerous tasks and the employee’s health level.
To reduce the impact of subjective assessments of the duration and intensity of stress experience on the psychosocial risk level, it is proposed to take into account the value of individual perception of stress experience (stress resistance) and the employees’ health condition.
Scales for assessing the impact of dangerous psychosocial factors and a form for documenting the process of managing psychosocial risks with the indication of precautionary measures to control them are proposed.
Acknowledgments
The authors would like to thank the anonymous reviewers and editor for their valuable comments and recommendations concerning the improvement of the paper.
Funding
This study was carried out as part of the project “Belt and Road Initiative Center for Chinese-European studies (BRICCES)” and was funded by the Guangdong University of Petrochemical Technology.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Official site European Agency for Safety and Health at Work. European survey of Enterprises on New and Emerging Risks (ESENER). Available from: https://osha.europa.eu/en/facts-and-figures/esener.
2. Ren F, Zhang J. Job stressors, organizational innovation climate, and employees’ innovative behaviour. Creat Res J. 2015;27(1):16–23. doi:10.1080/10400419.2015.992659
3. Bani-Melhem S, Zeffane R, Albaity M. Determinants of employees’ innovative behaviour. Int J Contemp Hosp Manag. 2018;30(3):1601–1620. doi:10.1108/IJCHM-02-2017-0079
4. Martín P, Salanova M, Peiró JM. Job demands, job resources and individual innovation at work: going beyond Karasek’s model? Psicothema. 2007;19(4):621–626.
5. Liu C, Liu Y, Mills MJ, Fan J. Job stressors, job performance, job dedication, and the moderating effect of conscientiousness: a mixed-method approach. Int J Stress Manage. 2013;20(4):336–363. doi:10.1037/a0034841
6. Astorquiza Bustos BA, Castillo Caicedo M, Gomez Mejia A. Measuring the job stress of the employed population: the case of labor market in Cali-Colombia. Revista de Métodos Cuantitativos para la Economía y la Empresa. 2018;25:272–294.
7. Cannizzaro E, Ramaci T, Cirrincione L, Plescia F. Work-related stress, physio-pathological mechanisms, and the influence of environmental genetic factors. Int J Environ Res Public Health. 2019;16(20):4031. doi:10.3390/ijerph16204031
8. Halliday B, van der Laan L, Raineri A. Prioritizing work health, safety, and wellbeing in corporate strategies: an indicative framework. Safety. 2024;10(1):18. doi:10.3390/safety10010018
9. Alonso-Nuez M-J, Cañete-Lairla M-Á, García-Madurga M-Á, et al. Corporate social responsibility and workplace health promotion: a systematic review. Front Psychol. 2022;13:1011879. doi:10.3389/fpsyg.2022.1011879
10. Schulte PA, Iavicoli I, Fontana L, et al. Occupational safety and health staging framework for decent work. Int J Environ Res Public Health. 2022;19(17):10842. doi:10.3390/ijerph191710842
11. Rick J, Briner RB. Psychosocial risk assessment: problems and prospects. Occup Med. 2000;50(5):310–314. doi:10.1093/occmed/50.5.310
12. Roussos PL. The psychosocial risks and impacts in the workplace assessment tool: construction and psychometric evaluation. Behav Sci. 2023;13:104. doi:10.3390/bs13020104
13. Leka S, Jain A, Iavicoli S, Vartia M, Ertel M. The role of policy for the management of psychosocial risks at the workplace in the European Union. Saf Sci. 2011;49(4):558–564. doi:10.1539/joh.O10010
14. Stress at the workplace. Available from: https://www.who.int/publications/i/item/9241590475.
15. Brindle K, Moulding R, Bakker K, Nedeljkovic M. Is the relationship between sensory-processing sensitivity and negative affect mediated by emotional regulation? Aust J Psychol. 2015;67:214–221. doi:10.1111/ajpy.12084
16. Yano K, Oishi K. The relationships among daily exercise, sensory-processing sensitivity, and depressive tendency in Japanese university students. Pers Individ Differ. 2018;127:49–53. doi:10.1016/j.paid.2018.01.047
17. Frimpong S, Sunindijo RY, Wang CC, Boadu EF, Dansoh A, Fagbenro RK. Coping with psychosocial hazards: a systematic review of young construction workers’ practices and their determinants. Buildings. 2023;13(1):22. doi:10.3390/buildings13010022
18. Metzler YA, von Groeling-Müller G, Bellingrath S. Better safe than sorry: methods for risk assessment of psychosocial hazards. Saf Sci. 2019;114:122–139. doi:10.1016/j.ssci.2019.01.003
19. Albort-Morant G, Ariza-Montes A, Leal-Rodríguez A, Giorgi G. How does positive work-related stress affect the degree of innovation development? Int J Environ Res Public Health. 2020;17(2):520–535. doi:10.3390/ijerph17020520
20. Golinko V, Cheberyachko S, Deryugin O, Tretyak O, Dusmatova O. Assessment of the risks of occupational diseases of the passenger bus drivers. Saf Health Work. 2020;11(4):543–549. doi:10.1016/j.shaw.2020.07.005
21. Fukui S, Wu W, Salyers MP. Impact of supervisory support on turnover intention: the mediating role of burnout and job satisfaction in a longitudinal study. Adm Policy Ment Health Ment Health Serv Res. 2019;46(4):488–497. doi:10.1007/s10488-019-00927-0
22. Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep. 2015;17(9):1–9. doi:10.1007/s11886-015-0630-8
23. Carlotto MS, Câmara SG. Burnout syndrome in public servants: prevalence and association with occupational stressors. Psico-USF. 2019;24(3):425–435. doi:10.1590/1413-82712019240302
24. Martinez MC, Fischer FM. Psychosocial factors at hospital work: experienced conditions related to job strain and effort-reward imbalance. Revista Brasileira de Saúde Ocupacional. 2019;44:e12. doi:10.1590/2317-6369000025918
25. Kemajl Z, Stojance M, Gzim I, Ledi ML. Comprehensive analysis of the mining accident forecasting and risk assessment methodologies: case study – stanterg Mine. Min Miner Depos. 2024;18(2):11–17. doi:10.33271/mining18.02.011
26. Rysmendeyeva G. Development of mathematical models for an information system for decision-making in the asset management process. Eng J Satbayev Univ. 2021;143(3):65–75. doi:10.51301/vest.su.2021.i3.10
27. Abbas M, Raja U. Impact of psychological capital on innovative performance and job stress. Can J Adm Sci. 2015;32(3):128–138. doi:10.1002/cjas.1314
28. Di Marco D, Arenas A, Giorgi Arcangeli G, Mucci N. Be friendly, stay well: the effects of job resources on well-being in a discriminatory work environment. Front Psychol. 2018;9:413. doi:10.3389/fpsyg.2018.00413
29. Martinez MC, Fischer FM. Work ability as determinant of termination of employment: to resign or be dismissed? J Occup Environ Med. 2019;61(6):e272–e281. doi:10.1097/JOM.0000000000001599
30. Oenning NSX, Gelmini S, Brandao SS, Silva J. Workplace accidents in Brazil: analysis of physical and psychosocial stress and health-related factors. RAM Revista de Administração Mackenzie. 2018;19(3). doi:10.1590/1678-6971/eRAMG170131
31. Pulido Guerrero EG, Carrillo LJL, Ruiz LKJ. Work psychosocial conditions influencing on absenteeism: evaluation of an explicative model. Interdisciplinaria Revista de Psicología y Ciencias Afines. 2020;38(1):149–162. doi:10.16888/interd.2021.38.1.10
32. Oldham GR, Fried Y. Job design research and theory: past, present and future. Organ Behav Hum Decis Process. 2016;136:20–35. doi:10.1016/j.obhdp.2016.05.002
33. Tsopa V, Cheberiachko S, Yavorska O, Deryugin O, Bas I. Increasing the safety of the transport process by minimizing the professional risk of a dump truck driver. Min Miner Depos. 2022;16(3):101–108. doi:10.33271/mining16.03.101
34. Raj NA, Usman J, Khan SJ, Goh SL. The prevalence of lower limb musculoskeletal pain symptoms during stop and go driving. In: Usman J, Liew YM, Ahmad MY, Ibrahim F, editors.
35. Bazaluk O, Tsopa V, Cheberiachko S, et al. Ergonomic risk management process for safety and health at work. Front Public Health. 2023;11:1253141. doi:10.3389/fpubh.2023.1253141
36. Mogård EV, Rørstad OB, Bang H. The relationship between psychological safety and management team effectiveness: the mediating role of behavioral integration. Int J Environ Res Public Health. 2023;20:406. doi:10.3390/ijerph20010406
37. Bulat A, Dziuba S, Minieiev S, Koriashkina L, Us S. Solution of the problem to optimize two-stage allocation of the material flows. Min Miner Depos. 2020;14(1):27–35. doi:10.33271/mining14.01.027
38. Bernsmed K, Frøystad C, Meland PH, Nesheim DA, Rødseth ØJ. Visualizing cyber security risks with bow-tie diagrams. In:
39. Culwick MD, Merry AF, Clarke DM, Taraporewalla KJ, Gibbs NM. Bow-tie diagrams for risk management in anaesthesia. Anaesth Intensive Care. 2016;44:712–718. doi:10.1177/0310057x1604400615
40. Abdi Z, Ravaghi H, Abbasi M, Delgoshaei B, Esfandiari S. Application of Bow-tie methodology to improve patient safety. Int J Health Care Qual Assur. 2016;2(29):425–440. doi:10.1108/ijhcqa-10-2015-0121
41. Cendales BE, Gómez-Ortiz V, Useche SA, Cedillo L, Stephenson DWH, Landsbergis P. Mental health outcomes among urban public transport workers: a systematic literature review. J Transp Health. 2024;36:101804. doi:10.1016/j.jth.2024.101804
42. Knight C, Haslam SA. Your place or mine? Organizational identification and comfort as mediators of relationships between the managerial control of workspace and employees’ satisfaction and well-being. Br J Manag. 2010;21:717–735. doi:10.1111/j.1467-8551.2009.00683.x
43. Tobia L, Vittorini P, Di Battista G, et al. Study on psychological stress perceived among employees in an Italian University during mandatory and voluntary remote working during and after the COVID-19 pandemic. Int J Environ Res Public Health. 2024;21:403. doi:10.3390/ijerph21040403
44. Stasiła-Sieradzka M, Turska E. Sense of danger and stress–The mediating role of social bonds in the workplace on the example of mining rescuer profession. Medycyna Pracy. 2019;3:295–303. (in Polish). doi:10.13075/mp.5893.00779
45. Wu G, Hu Z, Zheng J. Role stress, job burnout, and job performance in construction project managers: the moderating role of career calling. Int J Environ Res Public Health. 2019;16(13):2394. doi:10.3390/ijerph16132394
46. Leung M, Chan Y-S, Yu J. Integrated model for stressors and stresses of construction project managers in Hong Kong. J Constr Eng Manage. 2009;135(2135):126–134. doi:10.1061/(ASCE)0733-9364(2009)135:2(126)
47. Schaufeli WB, Bakker AB. Job demands, job resources, and their relationship with burnout and engagement: a multi-sample study. J Organ Behav. 2004;25:293–315. doi:10.1002/job.248
48. Üngüren E, Onur N, Demirel H, Tekin ÖA. The effects of job stress on burnout and turnover intention: the moderating effects of job security and financial dependency. Behav Sci. 2024;14:322. doi:10.3390/bs14040322
49. Tabanelli MC, Depolo M, Cooke RMT, et al. Available instruments for measurement of psychological factors in the work environment. Int Arch Occup Environ Health. 2008;82:1–12. doi:10.1007/s00420-008-0312-6
50. Edwards JA, Webster S, Van Laar D, Easton S. Psychometric analysis of the UK health and safety executive’s management standards work-related stress indicator tool. Work Stress. 2008;22:96–107. doi:10.1080/02678370802166599
51. Topp CW, Østergaard SD, Søndergaard S, Bech P. WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. 2015;84:167–176. doi:10.1159/000376585
52. Velicer WF, Jackson DN. Component analysis versus common factor analysis: some further observations. Multivariate Behav Res. 1990;25:97–114. doi:10.1207/s15327906mbr2501_12
53. Figueredo J-M, García-Ael C, Gragnano A, Topa G. Well-being at work after return to work (RTW): a systematic review. Int J Environ Res Public Health. 2020;17:7490. doi:10.3390/ijerph17207490
54. Damsgaard JB, Angel S. Living a meaningful life while struggling with mental health: challenging aspects regarding personal recovery encountered in the mental health system. Int J Environ Res Public Health. 2021;18:2708. doi:10.3390/ijerph18052708
55. Tummers LG, Bakker AB. Leadership and job demands-resources theory: a systematic review. Front Psychol. 2021;12:722080. doi:10.3389/fpsyg.2021.722080
56. Snyder LA, Krauss AD, Chen PY, Finlinson S, Huang Y-H. Occupational safety: application of the job demand–control-support model. Accid Anal Prev. 2008;40(5):1713–1723. doi:10.1016/j.aap.2008.06.008
57. Kox JH, van der Zwan JS, Groenewoud JH, et al. Predicting late dropout from nursing education or early dropout from the profession. Sci Talks. 2023;5:100106. doi:10.1016/j.sctalk.2022.100106
58. Bejda G, Kułak-Bejda A, Waszkiewicz N, Krajewska-Kułak E. Type D personality, stress level, life satisfaction, and alcohol dependence in older men. Front Psychiatry. 2021;12:712508. doi:10.3389/fpsyt.2021.712508
59. Salimzadeh R, Hall NC, Saroyan A. Examining academics’ strategies for coping with stress and emotions: a review of research. Front Educ. 2021;6:660676. doi:10.3389/feduc.2021.660676
60. Wong SMY, Lam BYH, Wong CSM, et al. Measuring subjective stress among young people in Hong Kong: validation and predictive utility of the single-item subjective level of stress (SLS-1) in epidemiological and longitudinal community samples. Epidemiol Psychiatr Sci. 2021;8(30):e61. doi:10.1017/S2045796021000445
61. Burazeri G, Goda A, Sulo G, Stefa J, Kark JD. Financial loss in pyramid savings schemes, downward social mobility and acute coronary syndrome in transitional Albania. J Epidemiol Community Health. 2008;62(7):620–626. doi:10.1136/jech.2007.066001
62. Keller A, Litzelman K, Wisk LE, et al. Does the perception that stress affects health matter? The association with health and mortality. Health Psychol. 2012;31(5):677–684. doi:10.1037/a0026743
63. Shchaslyvyi AY, Antonenko SV, Telegeev GD. Comprehensive review of chronic stress pathways and the efficacy of behavioral stress reduction programs (BSRPs) in managing diseases. Int J Environ Res Public Health. 2024;21:1077. doi:10.3390/ijerph21081077
64. Meléndez R, Giraldo R, Leiva V. Sign, Wilcoxon and Mann-Whitney tests for functional data: an approach based on random projections. Mathematics. 2021;9:44. doi:10.3390/math9010044
65. Salleh MR. Life event, stress and illness. Malays J Med Sci. 2008;15(4):9–18.
66. Merrill RM. Mental health conditions according to stress and sleep disorders. Int J Environ Res Public Health. 2022;19(13):7957. doi:10.3390/ijerph19137957
67. Stoyanov D. The anxious brain: the influence of stress on the nervous system. Brain Sci. 2024;14(6):597. doi:10.3390/brainsci14060597
68. Sebastião R, Neto DD, Costa V. Understanding differential stress and mental health reactions to COVID-19-related events. Int J Environ Res Public Health. 2023;20:5819. doi:10.3390/ijerph20105819
69. Yöyen E, Barış TG, Bal F. Depression, anxiety, and psychological resilience in healthcare workers during the pandemic (COVID-19). Healthcare. 2024;12(19):1946. doi:10.3390/healthcare12191946
70. Tsopa V, Cheberiachko S, Cheberiachko Y, et al. Development of a new ergonomic risks management algorithm on the example of drivers. East Eur J Enterp Technol. 2024;2(3 (128):38–49. doi:10.15587/1729-4061.2024.302886
71. Schetter E, Schwinger M. What triggers mental disorders? Examining the role of increasing relationships between self-regulatory efficacy expectations and behavioral intensity. Psychiatry Int. 2024;5:672–696. doi:10.3390/psychiatryint5040048
72. Cybulska AM, Rachubińska K, Stanisławska M, Grochans S, Cymbaluk-Płoska A, Grochans E. Analysis of factors related to mental health, suppression of emotions, and personality influencing coping with stress among nurses. Int J Environ Res Public Health. 2022;19:9777. doi:10.3390/ijerph19169777
73. Di Tecco C, Ronchetti M, Ghelli M, Russo S, Persechino B, Iavicoli S. Do Italian companies manage work-related stress effectively? A process evaluation in implementing the INAIL methodology. Biomed Res Int. 2015;2015:197156. doi:10.1155/2015/197156
74. Nielsen K, Randall R, Holten AL, González ER. Conducting organizational-level occupational health interventions: what works? Work Stress. 2010;24(3):234–259. doi:10.1080/02678373.2010.515393
75. Lynch W, Platt ML, Pardes A. Development of a severity score and comparison with validated measures for depression and anxiety: validation study. JMIR Format Res. 2021;5(11):e30313. doi:10.2196/30313
76. König H, König HH, Gallinat J, et al. Excess costs of mental disorders by level of severity. Social Psychiatry Psychiatric Epidemiol. 2023;58(6):973–985. doi:10.1007/s00127-022-02298-8
77. Kaya GK, Ward J, Clarkson J. A review of risk matrices used in acute hospitals in England. Risk Anal. 2019;39:1060–1070. doi:10.1111/risa.13221
78. Bao C, Wu D, Wan J, Li J, Chen J. Comparison of different methods to design risk matrices from the perspective of applicability. Procedia Comput Sci. 2017;122:455–462. doi:10.1016/j.procs.2017.11.393
79. Alderman BL, Arent SM, Landers DM, Rogers TJ. Aerobic exercise intensity and time of stressor administration influence cardiovascular responses to psychological stress. Psychophysiology. 2007;44(5):759–766. doi:10.1111/j.1469-8986.2007.00548.x
80. Wicker P, Frick B. The relationship between intensity and duration of physical activity and subjective well-being. Eur J Public Health. 2015;25(5):868–872. doi:10.1093/eurpub/ckv131
81. Shannon S, Shevlin M, Brick N, Breslin G. Frequency, intensity and duration of muscle strengthening activity and associations with mental health. J Affect Disord. 2023;325:41–47. doi:10.1016/j.jad.2022.12.063
82. Curyło M, Czerw A, Rynkiewicz-Andryśkiewicz M, et al. Measuring the intensity of stress experienced and its impact on life in patients with diagnosed alcohol use disorder. J Clin Med. 2024;13:572. doi:10.3390/jcm13020572
83. DeTienne KB, Agle BR, Phillips JC, Ingerson M-C. Frequency and intensity of stress scales [Database record]. APA PsycTests. 2012. doi:10.1037/t35248-000
84. Duijm NJ. Recommendations on the use and design of risk matrices. Saf Sci. 2015;76:21–31. doi:10.1016/j.ssci.2015.02.014
85. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depression Anxiety. 2003;18:76–82. doi:10.1002/da.10113
86. Hjemdal O, Friborg O, Braun S, Kempenaers C, Linkowski P, Fossion P. The Resilience Scale for Adults: construct validity and measurement in a Belgian sample. Int J Test. 2011;11(1):53–70. doi:10.1080/15305058.2010.508570
87. Deryugin OV, Cheberiachko SI. Substatiation of truck selection in terms of minimizing psychophysiological stress on a driver. East Eur J Enterp Technol. 2015;3(3(75):15–22. (In Ukrainian). doi:10.15587/1729-4061.2015.42127
88. Šarlija M, Popović S, Jagodić M, et al. Prediction of task performance from physiological features of stress resilience. IEEE J Biomed Health Inform. 2021;25:2150–2161.
89. Lü W, Wang Z, You X. Physiological responses to repeated stress in individuals with high and low trait resilience. Biol Psychol. 2016;120:46–52. doi:10.1016/j.biopsycho.2016.08.005
90. Diaz-Ramos RE, Gomez-Cravioto DA, Trejo LA, López CF, Medina-Pérez MA. Towards a resilience to stress index based on physiological response: a machine learning approach. Sensors. 2021;21:8293. doi:10.3390/s21248293
91. Nesticò A, He S, De Mare G, Benintendi R, Maselli G. The ALARP Principle in the Cost-Benefit Analysis for the Acceptability of Investment Risk. Sustainability. 2018;10:4668. doi:10.3390/su10124668
92. Jerath R, Syam M, Ahmed S. The future of stress management: integration of Smartwatches and HRV technology. Sensors. 2023;23:7314. doi:10.3390/s23177314
93. Du Y, Shahiri H, Wei X. I’m stressed!”: the work effect of process innovation on mental health. SSM Popul Health. 2023;21:101347. doi:10.1016/j.ssmph.2023.101347
94. Song Y, Lindquist R. Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Educ Today. 2015;35(1):86–90. doi:10.1016/j.nedt.2014.06.010
95. Arch JJ, Ayers CR, Baker A, Almklov E, Dean DJ, Craske MG. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behav Res Ther. 2013;51:185–196. doi:10.1016/j.brat.2013.01.003
96. Can YS, Iles-Smith H, Chalabianloo N, et al. How to relax in stressful situations: a smart stress reduction system. Healthcare. 2020;8:100. doi:10.3390/healthcare8020100
97. Froberg DG, Kane RL. Methodology for measuring health-state preferences—II: scaling methods. J Clin Epidemiol. 1989;42(5):459–471. doi:10.1016/0895-4356(89)90136-4
98. Cox T, Griffiths A. The nature and measurement of work-related stress: theory and practice. Psychology. 2005. doi:10.1201/9781420055948.ch19
99. Sánchez-Guarnido AJ, Ruiz-Granados MI, Garrido-Cervera JA, Herruzo J, Herruzo C. Implementation of the recovery model and its outcomes in patients with severe mental disorder. Healthcare. 2024;12(9):952. doi:10.3390/healthcare12090952
100. O’Connell M, Tondora J, Croog G, Evans A, Davidson L. From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatr Rehabil J. 2005;28(4):378–386. doi:10.2975/28.2005.378.386
101. McNaught M, Caputi P, Oades LG, Deane FP. Testing the validity of the recovery assessment scale using an Australian sample. Aust N Z J Psychiatry. 2007;41(5):450–457. doi:10.1080/00048670701264792
102. Nielsen K, Randall R, Holten A-L, González ER. Conducting organizational-level occupational health interventions: what works? Work Stress. 2010;24(3):234–259. doi:10.1080/02678373.2010.515393
103. Di Tecco C, Nielsen K, Ghelli M, et al. Improving working conditions and job satisfaction in healthcare: a study concept design on a participatory organizational level intervention in psychosocial risks management. Int J Environ Res Public Health. 2020;17(10):3677. doi:10.3390/ijerph17103677
104. Iavicoli S, Di Tecco C. The management of psychosocial risks at work: state of the art and future perspectives. La Medicina del lavoro. 2020;111(5):335–350. doi:10.23749/mdl.v111i5.10679
105. Barbaranelli C, Ghezzi V, Di Tecco C, et al. Assessing objective and verifiable indicators associated with work-related stress: validation of a structured checklist for the assessment and management of work-related stress. Front Psychol. 2018;9:2424. doi:10.3389/fpsyg.2018.02424
106. Bazaluk O, Pavlychenko A, Yavorska O, et al. Improving the risk management process in quality management systems of higher education. Sci Rep. 2024;14:3977. doi:10.1038/s41598-024-53455-9
107. Schulte PA, Delclos G, Felknor SA, Chosewood LC. Toward an expanded focus for occupational safety and health: a commentary. Int J Environ Res Public Health. 2019;16:1–17. doi:10.3390/ijerph16244946
108. Podsakoff NP, LePine JA, LePine MA. Differential challenge stressor-hindrance stress relationships with job attitudes, turnover intentions, turnover, and withdrawal behavior: a meta-analysis. J Appl Psychol. 2007;92(2):438–454. doi:10.1037/0021-9010.92.2.438
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






