Back to Journals » Cancer Management and Research » Volume 17
Interventional Treatment Strategies for Carotid Blowout Syndrome After Radiotherapy for Nasopharyngeal Carcinoma
Authors Lin Z, Chen J, Zou X, Zhang J, Huang D
Received 5 December 2024
Accepted for publication 25 March 2025
Published 3 April 2025 Volume 2025:17 Pages 757—765
DOI https://doi.org/10.2147/CMAR.S509063
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bilikere Dwarakanath
Treatment Strategies for Carotid Blowout Syndrome After Radiotherapy – Video abstract [509063]
Views: 106
Zhipeng Lin,* Jianqiao Chen,* Xugong Zou, Jian Zhang, Dabei Huang
Department of Interventional Medicine, Zhongshan People’s Hospital, Zhongshan, Guangdong Province, 528400, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dabei Huang, Department of Interventional Medicine, Zhongshan People’s Hospital, No. 2 Sunwen East Road, Zhongshan, Guangdong Province, 528400, People’s Republic of China, Email [email protected]
Background: Carotid blowout syndrome (CBS) is a life-threatening complication that can occur after radiotherapy in nasopharyngeal carcinoma (NPC) patients, resulting in catastrophic hemorrhage. Endovascular treatments, including coil embolization and stent grafting, have become standard options for managing CBS. Recent studies suggest that individualized approaches based on aneurysm location and vascular condition may further reduce recurrence and complications. This study aims to evaluate the efficacy, safety, and outcomes of these treatments in NPC patients with CBS.
Methods: A retrospective analysis was conducted on 46 NPC patients who developed CBS following radiotherapy and underwent endovascular intervention at Zhongshan People’s Hospital between January 2016 and July 2023. Outcomes such as immediate hemostasis, rebleeding rates, complications, and 1-year survival were analyzed.
Results: Among the 46 patients, 29 received coil embolization and 17 underwent stent grafting. Immediate hemostasis was achieved in all cases (100%). The 1-year rebleeding rate was 8.6% (4/46), and the overall complication rate was 8.6% (4/46), with cerebral infarctions being the primary concern. Coil embolization is associated with lower rebleeding rates, while stent grafting preserves arterial patency better. The 1-year survival rate was 89.1% (41/46).
Conclusion: Endovascular interventions, including coil embolization and stent grafting, are effective in managing CBS in NPC patients after radiotherapy. Future research should focus on refining patient selection criteria and optimizing long-term outcomes.
Keywords: nasopharyngeal carcinoma, radiotherapy, endovascular treatment, Stent graft, coil embolization, carotid blowout syndrome
Introduction
Nasopharyngeal carcinoma (NPC) is a prevalent malignancy in Southeast Asia, particularly in Southern China, where radiotherapy is the cornerstone of curative treatment.1 Advances in radiotherapy, including intensity-modulated radiotherapy (IMRT), have greatly improved survival rates for NPC patients. However, these advancements have also resulted in an increased incidence of late-stage complications. One such complication is osteoradionecrosis (ORN) of the skull base, which arises from radiation-induced damage to bone tissue, leading to bone necrosis and exposure.2 The exposure of the skull base, coupled with impaired ciliary function in the nasopharynx due to radiation-induced damage, diminishes the self-cleansing ability of the nasopharynx, thereby heightening the risk of local infection. These factors, in combination with direct radiation-induced injury to the carotid artery, contribute to the development of carotid blowout syndrome (CBS), which is characterized by pseudoaneurysm formation and subsequent rupture.3
CBS is associated with high mortality if not treated promptly due to massive hemorrhage. Conventional treatments, such as surgical ligation, bypass grafting, or radial artery high-flow bypass, are often challenging because of radiation-induced tissue changes, increasing the risk of complications.4 Endovascular techniques, like coil embolization and stent grafting, offer less invasive alternatives, providing immediate hemorrhage control with lower complication rates.5
Recent studies indicate that coil embolization, while effective in achieving hemostasis, may pose risks such as cerebral infarction due to compromised blood flow. On the other hand, stent grafting, which maintains arterial patency, has been associated with a higher risk of rebleeding if not properly placed.6 Current evidence supports individualized treatment strategies that take into account the patient’s vascular anatomy, the location of the pseudoaneurysm, and the extent of collateral circulation.
This study retrospectively assesses the outcomes of endovascular treatments for CBS in NPC patients, providing a comprehensive analysis of the risks and benefits of both coil embolization and stent grafting. By reviewing the factors influencing treatment success, this study aims to provide insights to improve future interventional strategies.
Methods
Inormal Information
The study was conducted in accordance with the Declaration of Helsinki and other ethical principles for medical research involving human subjects. This retrospective study was conducted at Zhongshan People’s Hospital and included 46 NPC patients who developed CBS following radiotherapy. All patients underwent endovascular intervention between January 2016 and July 2023. Our previous study (PMID:39229254) provided a foundational understanding of interventional approaches to CBS, focusing on a smaller patient cohort and conventional treatment techniques.7
Building on this prior work, the current study aims to advance the field by: 1. Expanding the Patient Cohort: This study includes a larger and more comprehensive cohort, allowing for more robust statistical analysis and a deeper understanding of treatment outcomes. 2. Introducing Novel Techniques: The use of the Willis intracranial covered stent is a key innovation not covered in our previous research. This advanced technique has shown promise in improving the safety and efficacy of interventions for CBS. 3. Highlighting a Unique Clinical Case: A particularly rare and complex case of bilateral internal carotid artery involvement is reported, providing valuable insights into the management of such challenging scenarios. 4. Providing Updated Outcomes: By including the latest clinical data and interventional advancements, this study contributes updated insights into the management of CBS in NPC patients.
The study was approved by the hospital’s ethics committee and was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Written informed consent was obtained from all patients. Primary outcomes measured included immediate hemostasis, rebleeding rates, complications (such as cerebral infarction), and 1-year survival.
Inclusion criteria: (1) Patients with a histologically confirmed diagnosis of NPC and a history of radiotherapy. (2) CBS diagnosis confirmed via imaging, including digital subtraction angiography (DSA) or enhanced computed tomography (CT). (3) Significant hemorrhage (nasal bleeding >300mL or recurrent bleeding unresponsive to conservative treatments)
Exclusion criteria: (1) Carotid artery rupture due to causes unrelated to radiotherapy. (2) Patients with severe comorbidities (eg, severe heart, lung, or kidney dysfunction) that would increase the procedural risk.
Preoperative Preparation
Prior to the intervention, it is essential to conduct comprehensive laboratory evaluations, which include a complete blood count, liver and renal function tests, cardiac function evaluations, coagulation profiles, and enhanced computed tomography (CT) of the carotid arteries. Additionally, measures such as nasal packing, aggressive fluid resuscitation, and blood transfusions should be implemented to address hemorrhagic shock.
Endovascular Treatment Protocol
All procedures were carried out in an interventional radiology room, using the Seldinger technique for vascular access via the femoral artery. Once vascular access was successfully established, selective angiography was performed on the carotid arteries to accurately pinpoint the site of rupture. Based on the angiographic findings, one of two intervention strategies was implemented.
Coil Embolization
Coil embolization should be applied to patients with sufficient collateral circulation. Detachable coils are systematically placed to effectively occlude the pseudoaneurysm. Before proceeding with the embolization, a balloon occlusion test is conducted to assess the adequacy of collateral circulation, ensuring that surrounding tissues receive sufficient blood flow throughout the procedure.
Stent Grafting
For patients with straightforward vascular anatomy but poor collateral circulation, a covered stent was positioned across the pseudoaneurysm. This technique facilitates the sealing of the ruptured artery while maintaining blood flow and significantly mitigating the risk of ischemic complications in scenarios with inadequate collateral circulation. After successful hemostasis, patients receiving stent implantation were started on an antiplatelet regimen on postoperative day three. The regimen included a daily dose of 75 mg clopidogrel and 100 mg aspirin, continued for at least six months. Routine coagulation assessments were conducted, with medication dosage adjusted as needed. In the event of nasopharyngeal bleeding, it was crucial to discontinue antiplatelet therapy immediately to prevent further complications.
For patients who exhibit a positive balloon occlusion test and are deemed unsuitable for stent placement, the available treatment options include: 1. Conservative medical management; 2. Ligation of the common carotid/internal carotid artery; 3. Coil embolization of the internal carotid artery.
Evaluation of Efficacy
(1) Immediate Hemostasis: Defined as cessation of bleeding within 24 hours of the procedure. (2) Rebleeding Rate: Recurrence of hemorrhage was tracked within one year of the initial intervention. (3) Complications: Procedure-related complications, including cerebral infarction and neurological deficits, were documented. (4) Survival Rate: The overall survival rate was evaluated one year post-procedure.
Statistical Analysis
Mean±standard deviation were used as descriptive statistics, the number and percentages were used for categorical data.
Results
This retrospective analysis included 46 patients diagnosed with CBS following radiotherapy for NPC. Of the initial 55 patients, 9 were excluded as their families opted out of treatment following intraoperative angiography. The final cohort consisted of 38 males (82.6%) and 8 females (17.4%), with a mean age of 59.3 ± 9.7 years (range: 37–74 years). The mean interval between radiotherapy and CBS was 7.7±3.2 years (range: 2–15 years). All patients had received intensity-modulated radiation therapy (IMRT) for nasopharyngeal carcinoma (NPC), with the total radiation dose to the primary tumor ranging from 68 to 72 Gy, delivered over 30 to 34 fractions. Furthermore, 17 of these patients underwent a second course of radiation therapy (re-irradiation) with doses between 45 and 60 Gy. A total of 17 patients received concomitant chemotherapy: 8 patients received chemotherapy combined with radiotherapy during initial treatment, while 9 patients received chemotherapy after tumor recurrence. In cases of CBS, 7 cases were located in the common carotid artery, 27 cases in the C1 segment (cervical segment) of the internal carotid artery, 9 cases in the C2 segment (petrous segment) of the internal carotid artery, 2 cases in the C3 segment (lacerum segment) of the internal carotid artery, and 1 case in the C4 segment (cavernous segment) of the internal carotid artery (Table 1).
 |
Table 1 Baseline Characteristics of CBS Patients |
The patient presented with otorrhagia (n = 5) and epistaxis (n = 45). DSA angiography confirmed the presence of internal carotid artery pseudoaneurysms in 46 patients, of which 9 had pseudoaneurysms with contrast extravasation along the carotid sheaths. The lesions were located on the right side in 20 patients and on the left side in 26 patients. No external carotid arterial anomalies were detected in any of the patients. 17 patients underwent stent implantation, and Figure 1 illustrates the perioperative situation of a CBS patient who received carotid artery stenting. 29 patients underwent coil embolization, and Figure 2 illustrates the perioperative situation of a CBS patient who received carotid artery coil embolization.
1. Immediate Hemostasis: Immediate hemostasis was achieved in all patients (100%) following either coil embolization or stent grafting. 2. Rebleeding Rate: The 1-year rebleeding rate was 8.6% (4/46). Three patients in the stent-grafting group and one in the coil embolization group experienced rebleeding and required further intervention. 3. Complications: Four patients 8.6% (4/46) developed procedure-related complications. Two patients who underwent internal carotid coil occlusion developed massive cerebral infarctions (Figure 3). One of these patients died, while the other survived with no severe neurological symptoms. Two patients who underwent carotid artery coil embolization developed mild neurological symptoms, but these resolved within one week. Follow-up brain MRI showed no signs of acute cerebral infarction. 4. Survival Rate: The overall 1-year survival rate was 89.1% (41/46). Three patients died within the year from causes unrelated to the endovascular procedure. Two patients who were treated with stents died due to rebleeding. 19 patients underwent secondary nasal surgery, which involved the removal of necrotic tissue and flap reconstruction of the nasopharyngeal region (Table 2).
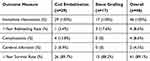 |
Table 2 Comparison of Treatment Outcomes for CBS |
Both treatment modalities achieved high immediate hemostasis rates. Coil embolization was associated with a lower rebleeding rate, while stent grafting offered better preservation of arterial patency. However, coil embolization had a slightly higher complication rate, with more patients experiencing cerebral infarction.
Discussion
CBS is a rare but life-threatening complication that may develop in patients with NPC who have received radiotherapy.8 CBS typically presents as rupture or impending rupture of the carotid artery or its branches, often presenting in severe hemorrhage. The pathogenesis of CBS is strongly associated with radiation-induced vascular injury, leading to progressive damage to the blood vessels. Radiotherapy can induce endothelial cell injury, fibrosis, and weakening of the arterial wall, ultimately contributing to the formation of pseudoaneurysms or direct vascular rupture.
Regarding the potential impact of chemotherapy on the risk of CBS, current literature is limited. Some studies suggest that chemotherapy drugs, especially platinum-based agents like cisplatin and taxanes, have direct vascular toxic effects. These drugs can damage the vascular endothelium, increasing blood vessel fragility, which may contribute to pseudoaneurysm formation or rupture. Additionally, chemotherapy may exacerbate vascular damage caused by radiotherapy, further compromising carotid artery integrity. However, the exact role of chemotherapy in CBS remains unclear, and further studies are needed to elucidate this relationship.
In this study, we retrospectively evaluated the efficacy and clinical outcomes of endovascular treatments for CBS in NPC patients. Our analysis focused on two primary therapeutic interventions: coil embolization and stent grafting.9 Coil embolization involves the insertion of coils into the affected artery to induce clotting and seal the pseudoaneurysm, effectively stopping the bleeding. This approach, while often successful, can lead to arterial occlusion, which compromise blood flow and increase the risk of ischemic complications, such as stroke.
On the other hand, stent grafting is a technique that uses a covered stent to reinforce the damaged arterial wall, maintaining the patency of the vessel while excluding the pseudoaneurysm from circulation. Stent grafting aims to preserve arterial integrity and mitigate the risk of ischemic complications. However, the risk of rebleeding and stent-related complications, such as infection or stent migration, remains a concern.10
At the 1-year follow-up, the overall rebleeding rate was 8.6%. Stent grafting was associated with a slightly higher rebleeding rate, which is likely due to stent migration or endoleaks, a known complication of stent grafts.11 On the other hand, coil embolization, though associated with a lower rebleeding rate, was linked to a higher incidence of cerebral infarction due to the occlusion of major arteries. Two patients in our study developed cerebral infarctions following coil embolization.
Recent studies have shown that while stent grafts preserve arterial patency, they carry a risk of long-term complications, such as rebleeding and stent thrombosis, particularly in patients with ongoing tumor invasion or infection. Additionally, coil embolization, though effective in controlling bleeding, compromises blood flow to the brain, increasing the risk of ischemic complications, particularly in patients with poor collateral circulation. Given the distinct mechanisms of action and clinical indications for these two techniques, they are not typically used in combination. Future studies should focus on optimizing patient selection for each treatment modality and exploring ways to minimize complications.
The 1-year survival rate in our study was 89.1%. While the primary cause of mortality was not directly related to the endovascular interventions, it is important to note that the overall prognosis of patients with CBS remains poor due to the advanced stage of their underlying cancer and the cumulative effects of radiotherapy.12 The results of our study highlight the importance of early diagnosis and timely intervention, as delayed treatment can significantly worsen outcomes.
This study underscores the importance of individualized treatment strategies in the management of CBS in NPC patients. While both coil embolization and stent grafting are effective in achieving immediate hemostasis, the choice of treatment should be guided by patient-specific factors, including vascular anatomy, collateral circulation, and overall health status. In the future, a more refined approach that incorporates advanced imaging techniques and risk stratification models may help reduce complications and improve long-term outcomes for CBS patients.
In patients exhibiting unstable arterial flow and significant hypotension, the carotid compression test may be utilized as an alternative to the balloon occlusion test. The primary benefit of this approach is the reduced duration of the testing process; however, this may result in an elevated risk of neurological dysfunction following carotid artery embolization. For those who test positive on the balloon occlusion test but are not candidates for stent placement, subsequent management strategies may include conservative internal management, coil embolization of the internal carotid artery, or carotid artery ligation.13–15
In cases of hemodynamically unstable internal carotid artery rupture with substantial hemorrhage, the efficacy of conservative medical management is often limited. Many of these individuals may have previously undergone conservative treatment prior to interventional procedures, generally yielding suboptimal outcomes. Given its high surgical trauma and complexity, carotid ligation is infrequently employed. Therefore, following thorough discussions with the patient, attempting coil occlusion of the affected internal carotid artery may be prudent. This approach aims to sustain hemodynamic stability during and after the procedure while minimizing the incidence of hypotension and the likelihood of neurological complications.16
This retrospective study has several limitations: 1. All patients underwent only Computed Tomography Angiography (CTA) of the cranial vasculature post-endovascular intervention, with no conventional angiographic evaluations performed; 2. The study exclusively included emergency cases of ruptured internal carotid artery pseudoaneurysms, with participants presenting hemodynamic instability, potentially compromising the accuracy of the balloon occlusion test; 3. Throughout the study’s duration, a variety of covered stent devices were utilized.
Conclusion
This retrospective analysis indicates that endovascular intervention serves as a robust and relatively safe alternative for managing CBS in patients with NPC following radiotherapy. The findings underscore significant survival advantages while also identifying opportunities for enhancing clinical practices to minimize complications.
Abbreviations
NPC, nasopharyngeal carcinoma; IMRT, intensity-modulated radiotherapy; CBS, carotid blowout syndrome; DSA, digital subtraction angiography; CT, computed tomography; CTA, computed tomography angiography.
Data Sharing Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Statement of Ethics
This study protocol was reviewed and approved by the Ethics Committee of Zhongshan People’s Hospital, approval number 2024-104. Written informed consent was obtained from each patient.
Acknowledgment
Zhipeng Lin and Jianqiao Chen are co-first authors for this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no competing interests.
References
1. To YP, Lok CS, On TC, et al. Comparison of Treatment Modalities in Postirradiation Carotid Blowout Syndrome: a Multicenter Retrospective Review. World Neurosurg. 2021;152:e666–e672. doi:10.1016/j.wneu.2021.06.032
2. De FF, Musio D, Tombolini V. Osteoradionecrosis and intensity modulated radiation therapy. An Overview Crit Rev Oncol Hematol. 2016;107:39. doi:10.1016/j.critrevonc.2016.08.017
3. Chen HY, Ma XM, Bai YR. Repeated massive epistaxis after re-irradiation in recurrent nasopharyngeal carcinoma. Contemp Oncol (Pozn). 2014;18(5):371–376. doi:10.5114/wo.2014.45290
4. Wu WB, Zhang XB, Feng ZK, et al. Strategies for patients with recurrent nasopharyngeal carcinoma involved internal carotid artery who are intolerant to embolization. Rhinology. 2023;62(3):342–352. doi:10.4193/RhinRhin23.130
5. Wan WS, Lai V, Lau HY, et al. Endovascular treatment paradigm of carotid blowout syndrome: review of 8-years experience. Eur J Radiol. 2013;82(1):95–99. doi:10.1016/j.ejrad.2011.01.061
6. Zussman B, Gonzalez LF, Dumont A, et al. Endovascular management of carotid blowout. World Neurosurg. 2012;78(1–2):109–114. doi:10.1016/j.wneu.2011.08.024
7. Lin ZP, Zou XG, Chen Y, et al. Efficacy analysis of endovascular treatment for ruptured internal carotid artery pseudoaneurysm hemorrhage in patients with nasopharyngeal carcinoma after radiotherapy. Front Surg. 2024;11:1451570. doi:10.3389/fsurg.2024.1451570
8. Chin YC, Lin CC, Lan MY, et al. Risk factors of post-irradiation carotid blowout syndrome in patients with nasopharyngeal carcinoma. Support Care Cancer. 2024;32(10):706. doi:10.1007/s00520-024-08905-5
9. Li H, Shi Z, Zhang Q, et al. Treatment strategy of carotid blowout syndrome after radiotherapy for nasopharyngeal carcinoma. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2024;38(6):467–471. doi:10.13201/j.issn.2096-7993.2024.06.003
10. Luo CB, Lee CH, Chang FC, et al. Risk factors of recurrent carotid blowout syndrome and strategy of endovascular management. J Chin Med Assoc. 2021;85(1):109–113. doi:10.1097/JCMA.0000000000000597
11. Plaforet V, Tournier L, Deschamps F, et al. Covered Stent Graft for Treatment of Carotid Blowout Syndrome in Patients With Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg. 2024;2024:e243228. doi:10.1001/jamaoto.2024.3228
12. Jiang JL, Chang JT, Yeh CH, et al. Incidence of Carotid Blowout Syndrome in Patients with Head and Neck Cancer after Radiation Therapy: a Cohort Study. Diagnostics. 2024;14(12):1222. doi:10.3390/diagnosics14121222
13. Chang FC, Luo CB, Lirng JF, et al. Endovascular Management of Post-Irradiated Carotid Blowout Syndrome. PLoS One. 2015;10(10):e0139821. doi:10.1371/journal.pone.0139821
14. Powitzky R, Vasan N, Krempl G, et al. Carotid blowout in patients with head and neck cancer. Ann Otol Rhinol Laryngol. 2010;119(7):476–484. doi:10.1177/000348941011900709
15. Bond KM, Brinjikji W, Murad MH, et al. Endovascular treatment of carotid blowout syndrome. J Vasc Surg. 2017;65(3):883–888. doi:10.1016/j.jvs.2016.11.024
16. Liang NL, Guedes BD, Duvvuri U, et al. Outcomes of interventions for carotid blowout syndrome in patients with head and neck cancer. J Vasc Surg. 2016;63(6):1525–1530. doi:10.1016/j.jvs.2015.12.047
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




