Back to Journals » International Journal of Nanomedicine » Volume 20
Isolating Astrocyte-Derived Extracellular Vesicles From Urine
Authors Xie XH, Chen MM, Xu SX , Mei J, Yang Q, Wang C, Lyu H, Gong Q, Liu Z
Received 25 September 2024
Accepted for publication 3 February 2025
Published 26 February 2025 Volume 2025:20 Pages 2475—2484
DOI https://doi.org/10.2147/IJN.S492381
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kamakhya Misra
Xin-hui Xie,1,* Mian-mian Chen,1,* Shu-xian Xu,1 Junhua Mei,1,2 Qing Yang,2 Chao Wang,1 Honggang Lyu,1 Qian Gong,1 Zhongchun Liu1,3
1Department of Psychiatry, Renmin Hospital of Wuhan University, Wuhan, Hubei, People’s Republic of China; 2Department of Neurology, Wuhan First Hospital, Wuhan, Hubei, People’s Republic of China; 3Taikang Center for Life and Medical Sciences, Wuhan University, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin-hui Xie; Zhongchun Liu, Department of Psychiatry, Renmin Hospital of Wuhan University, No. 99 Jiefang Road, Wuchang District, Wuhan, Hubei, 430060, People’s Republic of China, Email [email protected]; [email protected]; [email protected].
Introduction: Brain-derived extracellular vesicles (BDEVs) can cross the blood-brain barrier and enter the periphery. Therefore, quantifying and analyzing peripherally circulating BDEVs offer a promising approach to directly obtain a window into central nervous system (CNS) pathobiology in vivo. Rapidly evolving CNS diseases require high-frequency sampling, but daily venipuncture of human subjects is highly invasive and usually unfeasible.
Methods: To address this challenge, here we present a novel method for isolating astrocyte-derived extracellular vesicles from urine (uADEVs), combining urine concentration, ultracentrifugation to isolate total EVs, and then glutamate-aspartate transporter (GLAST) EV isolation using an anti-GLAST antibody.
Results: The identity of these GLAST+EVs as uADEVs was confirmed by transmission electron microscopy, nanoparticle tracking analysis, western blotting, and assessment of astrocyte-related neurotrophins.
Conclusions: Leveraging the convenience and availability of urine samples, the non-invasive uADEV approach provides a novel tool that allows high-frequency sampling to investigate rapidly evolving CNS diseases.
Keywords: urinary astrocyte-derived extracellular vesicles, human in vivo, non-invasive, central nervous system, high-frequency sampling
Introduction
Central nervous system (CNS) and neuropsychiatric diseases, such as epilepsy, neurodegenerative diseases, migraine, schizophrenia, depression, and bipolar disorder, remain a management challenge, in part due to the complex and incompletely understood underlying pathobiology.1 Although direct sampling of the CNS, such as through brain biopsy, could provide tissue for diagnostic and research purposes, the procedure is highly invasive and potentially harmful to patients. Cerebrospinal fluid (CSF) can be collected through lumbar puncture for biological analyses, but again the procedure is invasive and complications, although rare, can be serious. There is therefore a need for non-invasive biomarkers of CNS disorders.
Other characteristics of the CNS, notably the blood-brain barrier (BBB), challenge both the diagnosis and treatment of CNS disorders.2 The BBB is inherently selective, resulting in significant disparities in the expression levels of molecules found in the CNS and the periphery, making their interpretation difficult, so peripheral blood sampling, although routine, provides only limited representation of the CNS.3 Furthermore, many CNS diseases like Alzheimer’s disease (AD) and Parkinson’s disease (PD) have protracted diseases courses; others like multiple sclerosis can relapse and remit; and some, like depression, bipolar disorder, and encephalitis, can rapidly fluctuate in terms of symptom severity. Therefore, while snapshots of reliable protein biomarkers for AD and PD such as Aβ,4 tau,5 and α-synuclein6 taken annually or half-annually may be suitable for monitoring the disease course, for disorders with rapid symptom fluctuations, more frequent sampling may be necessary to capture highly dynamic changes. Except for in special settings like the intensive care unit (ICU), daily sampling of peripheral blood or CSF is impractical. Therefore, a new, rapid, and non-invasive method for capturing CNS signals is crucial for both clinical and research purposes.
Extracellular vesicles (EVs) are found in various bodily fluids, including blood, urine, tears, and saliva.7 EVs have emerged as a promising source of disease biomarkers, serving as “liquid biopsies”.8 Notably, EVs can cross the BBB bidirectionally,9 making brain-derived EVs (BDEVs) a potential “window to the brain”.10 BDEVs in peripheral blood have been examined as biomarkers of CNS diseases. In a large-sample trial, the concentrations of T-tau, P-T181-Tau, and Aβ1-42 in serum neuro-derived EVs (NDEVs) were linearly associated with their concentrations in CSF, with correlation coefficients close to 0.9.11 Furthermore, these NDEVs predicted the onset of AD.12 Similarly, in PD, α-synuclein was increased in NDEVs in patients with PD,13 and the area under the receiver operating characteristic curve (ROC) exceeded 0.9.14 In animal studies, plasma astrocyte-derived EVs (ADEVs) and their contents are correlated with brain homogenous (BH) levels.15 BDEVs in peripheral blood could therefore be good proxies of CNS status.16 While peripheral blood collection is relatively minimally invasive, daily blood sampling by venipuncture is also usually not feasible nor acceptable to patients. To overcome this limitation, we focused on another body fluid - urine - which also contains a large amount quantities of EVs.7
Here, we hypothesized that BDEVs transfer from the bloodstream to urine after plasma filtration in glomeruli, so can be isolated and analyzed as CNS-related molecules.17,18 Indeed, studies in rats have demonstrated that EVs injected into peripheral blood can be subsequently detected in urine.19 In humans, neuronal proteins have been detected in urinary total EVs (uTEVs),20 including elevated levels of ser(P)-1292 LRRK2, a PD-associated protein, in uTEVs of PD patients, which correlated with cognitive and daily function impairments.21 We therefore developed a protocol that enables enrichment of glutamate/aspartate transporter (GLAST)+EVs, believed to be ADEVs,22–30 from urine (uADEVs).
Materials and Methods
This study was conducted at Renmin Hospital of Wuhan University (Mental Health Center of Hubei Province, Wuhan, Hubei, China) in compliance with the Declaration of Helsinki (revised edition, 2013). The study protocol was approved by both the Human Ethics Committee of Renmin Hospital of Wuhan University. All participants provided informed consent and were free to withdraw from the trial at any time for any reason.
Protocol Summary
Urine samples were first concentrated and uTEVs isolated using ultracentrifugation (UC). uADEVs were isolated using biotin-anti-GLAST-antibody, similar to the isolation of ADEVs from plasma or serum.22–29,31 A flow chart of this protocol is depicted in Figure 1A.
Isolation of uTEVs
Nine healthy volunteers, six males and three females, participated in the study. The median (IQR) age of the participants was 25.0 (4.0) years 300–600 ml of fresh morning urine was collected from each participant and promptly delivered to the laboratory. Samples were processed within two hours of collection. The urine sample was centrifuged at room temperature (RT) for 30 minutes at 2,000 g, and the supernatant was collected. Subsequently, sodium chloride (NaCl) was added to a concentration of 0.58 M and the urine incubated at RT for 2 hours to eliminate urinary mucoproteins, including Tamm-Horsfall protein.32,33 The mixture was then centrifuged again at RT for 30 minutes at 8,000 g, and the supernatant was collected. The sample was filtered using a 0.45 μm filter membrane (Millipore, MA, USA, Catalog# HVLP07625), and then loaded into a concentration device (Amicon® stirred cell, Millipore, MA, USA, Catalog# UFSC40001) and ultrafiltered to a volume of 3–4 ml using a 10 kDa NMW ultrafiltration (UF) disc membrane (Millipore, MA, USA, Catalog# PLGC07610). Next, 200 ml of PBS was added, and the sample was ultrafiltered to a volume of approximately 3–4 ml, resulting in a concentrated component. The concentrated component was transferred to an ultracentrifuge tube and centrifuged at 150,000 g at 4°C for 150 minutes (SW60Ti, OptimaXE-100, Beckman Coulter, Fullerton, CA, USA). The parameter UC (duration of ultracentrifugation) was determined in a pilot study (Supplementary Material 1. The Determination of the Duration of Ultracentrifugation). The supernatant was discarded, and the precipitate was resuspended in 840 μl Dulbecco’s phosphate-buffered saline (DPBS, Beyotime, Shanghai, China, Catalog# C0221D) containing protease and phosphatase inhibitors (PPICs, Beyotime, Catalog# P1046). This resulted in a uTEV sample.
Isolation of uADEVs
Of the 840 μl uTEVs sample, 700 μl was mixed with 100 μl 3% bovine serum albumin (BSA, Beyotime, Catalog# ST023-50g) and incubated for 1 hour at RT with 8 μl of anti-GLAST (ACSA-1)-biotin antibody (Miltenyi Biotec, Bergisch Gladbach, Germany, Catalog# 130–118-984). Subsequently, 20 μl of streptavidin-agarose resin (Thermo Fisher Scientific, Waltham, MA, Catalog# 53116) and 80 μl of 3% BSA were added, followed by incubation for 60 minutes at RT. After centrifugation at 800 g for 10 minutes at 4°C and removal of the supernatant, each sample was resuspended in 200 μl of cold 0.1M glycine-HCl (pH = 3.0) by gently mixing for 30 seconds. The suspension was then centrifuged at 4,000 g for 10 minutes at 4°C, and the supernatant was collected. Several drops of 1M Tris-HCl (pH = 8.0, Beyotime, Catalog# ST780-500ml) was added to adjust the pH to 7.0. This resulted in a uGLAST+EV sample (approximately 216 μl). For western blotting and protein measurements, mammalian protein extraction reagent (M-PER, Thermo Fisher Scientific, Catalog# 78503) with PPICs was added to each uADEV or uTEV sample.
Validation of uADEVs
Transmission Electron Microscopy (TEM)
Similar to our previous ADEV studies,29,31 TEM (JEM-1230, JEOL, Tokyo, Japan) was used to image EVs. For direct evidence, immuno-electron microscopy (JEM1400, JEOL, Japan) staining for the astrocyte marker GLAST was conducted using a 10 nm gold-labeled secondary antibody for uADEVs samples.
Nanoparticle Tracking Analysis (NTA)
The diameter (nm) and concentration (particles/ml) of EV samples were determined using the ZetaView PMX 110 (Particle Metrix, Meerbusch, Germany) with ZetaView 8.04.02 nanoparticle tracking software (Particle Metrix, Meerbusch, Germany).
Western Blotting
Western blotting was conducted to detect: (i) three EV markers, using primary rabbit anti‐cluster of differentiation (CD)63 antibody (Abcam, Cambridge, UK, Catalog# ab134045), rabbit anti‐CD9 antibody (Abcam, Catalog# ab125011), and mouse anti‐Alix antibodies (Proteintech, Rosemont, IL, Catalog# 67715-1-Ig); (ii) an astrocyte marker, using rabbit anti-glial fibrillary acidic protein (GFAP) antibody (Abcam, Catalog# ab68428); (ii) and two kidney markers, using Na+-K+-Cl− cotransporter (NKCC) 2 (Abcam, Catalog# ab171747) and sodium-chloride cotransporter (NCC) (Abcam, Catalog# ab95302) antibodies.
Protein Quantification
Astrocyte-related neurotrophins (brain-derived neurotrophic factor (BDNF), epidermal growth factor (EGF), fibroblast growth factor (FGF)-2, glial cell-derived neurotrophic factor (GDNF), GFAP, nerve growth factor beta (NGF-β), and S100 calcium-binding protein B (S100B)) were measured using the Human ProcartaPlex™ Simplex kit (Thermo Fisher Scientific, Catalog# PPX-07).
Statistical Methods
For comparisons between uTEVs and uADEVs, concentrations of neurotrophins (pg/ml) were normalized to a reference of 10E+10 particles/ml, yielding values in pg/per 10E+10 particles, according to MISEV2018.7 Fold-changes in uADEVs/uTEVs ratios were calculated for both particle and neurotrophin concentrations. Welch’s two sample t-tests were employed to test differences between the uADEVs and uTEVs samples for each parameter. A two-sided p-value of <0.05 was considered statistically significant. All statistical analyses were performed using R version 4.2.0 (R Project for Statistical Computing) within RStudio version 1.4.1106 (RStudio).
Results
Validation of uTEVs and uADEVs
Figure 1 shows the schematic of uADEV isolation and their validation using NTA, TEM, and western blotting. NTA confirmed that the EV diameters were within the expected size range for small EVs. TEM images revealed characteristic EV-like structures in both uTEV and uADEV samples. Western blotting showed positive expression of three EV markers (CD63, CD9, and Alix) in both uTEV and uADEV samples. Additionally, uADEVs exhibited positive expression of an astrocyte marker (GFAP). Notably, two kidney markers, NCC2 and NKCC, were detected in the uTEV sample but not in uADEVs samples. Furthermore, immunogold electron microscopy provided direct confirmation that the GLAST molecule was present on the surface of uADEVs.
Comparisons Between uTEVs and uADEVs
Particle concentrations in uADEVs (5.3 + 1.6E+10/ml) were significantly lower than in uTEV samples (1.9 + 0.78E+12/ml). Given the sample volumes of uADEVs (216 µl) and uTEVs (840 µl), uADEVs constitute an estimated 0.86% of uTEVs. Considering the efficiency of the immune-isolation method, this might be an under estimate of the true proportion. In contrast, neurotrophin levels were significantly higher in uADEVs than in uTEVs, with 23.1 to 88.1-fold increases for the seven neurotrophins (Table 1).
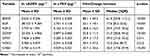 |
Table 1 Fold Changes in Target Expression in uADEVs Compared With uTEVs |
Discussion
Here we present a method to extract ADEVs from urine, paving the way for the non-invasive tracking of specific molecular in vivo signals within the CNS using an abundant, readily available biosample. This uADEVs protocol has promise as a groundbreaking, non-invasive approach for daily CNS monitoring, serving as a valuable tool for biomarker discovery and etiological studies of rapidly evolving CNS diseases.
Methodological Considerations for uADEVs Isolation and Validation
Considering the principles of this protocol, uADEVs isolation requires a target protein that is exclusively expressed on the surface of astrocytes and not on the surface of urogenital tract cells. The commonly used target is GLAST.22–29,31 To confirm the specificity of GLAST, we interrogated the Human Protein Atlas (HPA) database,34 in which GLAST showed significant expression on the surface of astrocytes in the brain and no evidence of expression by urogenital tract cells. In contrast, the commonly used target protein for extracting neuro-derived EVs, L1CAM, was expressed in the kidneys. Thus, for proof-of-concept of isolating BDEVs from urine, we selected GLAST+ EVs as uADEVs to ensure that they originated from astrocytes.
Since most EVs in uTEVs are derived from the urogenital tract,35 it is important to assess contamination of uADEVs with urogenital components. To address this, we selected two markers commonly used in urinary EV research, NKCC2 and NCC,36,37 to evaluate urogenital contamination in uADEVs. Western blot images revealed that NKCC2 and NCC were highly expressed in uTEV samples, as expected, but were barely detectable in uADEV samples (Figure 1H). This suggests minimal urogenital contamination of uADEVs samples. Combined with evidence of neurotrophic factor, these GLAST+ EVs are likely to primarily originate from astrocytes, namely, uADEVs.
Ultracentrifugation has been widely used to enrich for uTEVs, typically using parameters of 100,000 g for 70 minutes, with a second cycle to further isolate uTEVs.38–44 Although this method yields relatively pure uTEVs, the yield is low. Since uADEVs are relatively rare in uTEV samples, it was crucial to first enhance the yield of isolated uTEVs. A straightforward approach to increasing the yield is by extending the centrifugation time.45 Therefore, we conducted a preliminary experiment to optimize uTEV yield, finding that 150,000 g for 150 minutes obtained the highest yield of uTEVs (Supplementary Material 1). Moreover, TEM images (Figure 1E–G) suggested that this parameter setting did not significantly introduce contamination.
uADEV Function: Selectively Isolating CNS Signals From uTEVs
Since uADEVs are a subset of uTEVs, and some CNS-related molecules were detected in uTEVs, it might be possible to analyze uTEVs directly rather than isolating uADEVs. However, a key advantage of isolating uADEVs is that they help to ensure that the observed between-group differences in target molecules specifically originate from astrocytes, even if the same molecules are present in other cells, tissues, or organs (Figure 2).
Considering the example of cytokines, inflammation plays a crucial role in many CNS diseases, and astrocytes are major cytokines producer within the CNS.46,47 However, other immune cells throughout the body also produce cytokines. While uTEVs have been used to detect cytokines in urine,48,49 such measurements might not accurately reflect changes within the CNS due to the presence of cytokines from peripheral sources. However, measuring cytokines specifically in uADEVs could overcome this limitation and allow for more precise tracking of cytokine changes within the CNS. For instance, GFAP is a potential biomarker for diseases such as traumatic brain injury, intracerebral hemorrhage, and stroke, with elevated levels detected in the blood and urine of affected patients.50,51 However, GFAP levels may show heterogeneity due to interference from non-CNS-derived signals,52,53 limiting its reliability as a biomarker for CNS-related disease. However, enrichment of ADEVs for GFAP detection would help to reduce interference from non-CNS sources, ensuring that the signal originates specifically from the CNS rather than other cell types.54
Additionally, for ubiquitously expressed molecules, such as those in common signaling pathways or some receptors, measuring the concentration of these molecules in uTEV samples is unlikely to accurately reflect CNS levels, as uADEVs only represent ~1% of uTEVs.
Potential Benefits for Trial Design and Data Analyses
Urine is an ideal body fluid for biomarker detection, as it is abundant, easy to collect at regular, frequent intervals, and non-invasive. The enhanced temporal resolution offered by uADEVs could improve CNS disease trial design, especially for rapidly progressing diseases where timely and frequent biomarker identification is critical (Figure 3A). As detection technologies continue to advance, the required urine volume may decrease, potentially enabling hourly sampling and capturing CNS dynamics at an unprecedented level. uADEVs therefore allow us to capture in vivo molecular “movies” of the CNS, rather than capturing static “snapshots”.
Beyond biomarker discovery, uADEVs offer a valuable tool for testing potential hypotheses related to the underlying pathobiology. As illustrated in Figure 3B, if a candidate molecule’s trajectory in uADEVs aligns with, but lags behind, the symptom trajectory, the molecule is more likely to be a consequence or confounding factor rather than the cause of the observed symptom. Conversely, only candidate molecules with trajectories preceding the symptom trajectory are likely to be causal.
Identifying reliable biomarkers for rapidly changing CNS disorders like depression and bipolar disorder is difficult, primarily because both the disease and biomarker expression are highly heterogeneous. Even if all patients with a specific disease shared the same underlying molecular trajectory (unlikely, but useful for illustration), differences in sampling time points also introduce heterogeneity (Figure 3C). This “time-induced heterogeneity” can be a significant obstacle in disease monitoring. However, uADEVs, sampled at high frequency, may offer a potential solution. By capturing individual molecular trajectories over time (Figure 3D), uADEVs could provide more detailed longitudinal data for analysis. This would also allow the use of some post-hoc algorithms, like realignment based on peaks (Figure 3E), to reduce time-induced heterogeneity. While real-world data are more complex, increasing the sampling frequency with uADEVs paves the way for exploring various data processing algorithms, ultimately leading to a deeper understanding of CNS disorders. While this represents a simplified model and heterogeneity manifests in various forms with greater complexity in real-world data, we believe that high-frequency sampling provides more opportunities for data processing using multiple algorithms, enabling deeper exploration.
Furthermore, our study not only develops a novel method for CNS monitoring but also suggests a potentially new research paradigm. The uADEVs protocol can be adapted to isolate other specific EVs from uTEVs originating from various cell types, tissues, and organs. If successfully implemented, this approach could unlock the vast potential of urine samples for studying a wide range of diseases beyond the urogenital system.
Limitations
First, while we used UC here, size-exclusion chromatography (SEC) might be suitable for labs lacking this equipment. Additionally, ultrafiltration (UF) can lead to a significant loss of uTEVs. Employing high-capacity UC tubes to directly collect uTEVs without UF may potentially increase uADEV yield, but this requires further investigation. Second, the absolute particle number of uADEVs is low, limiting their use in multi-omics-based high-throughput assays. To address this limitation, we are actively developing methodologies that enable such studies using minimal quantities of uADEVs. Third, the impact of other disease states, particularly urological diseases, on uADEVs remains unclear. Further research is needed to address this question. Fourth, the mechanism by which ADEVs cross the glomerular basement membrane into urine remains unknown. Elucidating this mechanism may significantly enhance the utility of uADEVs. Fifth, this study utilized fresh urine samples, and applicability of the protocol to frozen or concentrated urine samples after thawing needs investigation. Future studies should investigate the effect of sample storage conditions on uADEVs. Furthermore, compared with unconcentrated urine samples, storing concentrated urine samples could increase the storage capacity of biobanks.
Conclusion
Here we propose a simple method for isolating urinary ADEVs, paving the way for non-invasive monitoring of CNS in vivo activity with high sampling rates, up to daily or even more frequently. This approach, coupled with appropriate signal processing algorithms, holds promise for identifying novel biomarkers or exploring the pathology of rapidly evolving CNS diseases. Furthermore, the uADEVs protocol can be further adapted to isolate other specific EVs originating from other cells types from urine samples. This holds promise for using urine to study a wider range of diseases beyond the urological system.
Acknowledgments
This work was supported by grant from the National Natural Science Foundation of China (grant number: U21A20364). This work has not received funding/assistance from any commercial organizations. The funding source had no roles in the design of this study nor the execution, analyses, interpretation of the data, or decision to submit results. Part of this paper was uploaded to medRxiv as a preprint: https://www.medrxiv.org/content/10.1101/2024.01.12.24301104v1.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Abi-Dargham A, Moeller SJ, Ali F, et al. Candidate biomarkers in psychiatric disorders: state of the field. World Psychiatry. 2023;22(2):236–262. doi:10.1002/wps.21078
2. Kadry H, Noorani B, Cucullo L. A blood-brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS. 2020;17(1):69. doi:10.1186/s12987-020-00230-3
3. Gigase FAJ, Smith E, Collins B, et al. The association between inflammatory markers in blood and cerebrospinal fluid: a systematic review and meta-analysis. Mol Psychiatry. 2023;28(4):1502–1515. doi:10.1038/s41380-023-01976-6
4. Jack CR, Bennett DA, Blennow K, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimer’s Dementia. 2018;14(4):535–562. doi:10.1016/j.jalz.2018.02.018
5. Parnetti L, Gaetani L, Eusebi P, et al. CSF and blood biomarkers for Parkinson’s disease. Lancet Neurol. 2019;18(6):573–586. doi:10.1016/S1474-4422(19)30024-9
6. Fayyad M, Salim S, Majbour N, et al. Parkinson’s disease biomarkers based on α-synuclein. J Neurochem. 2019;150(5):626–636. doi:10.1111/jnc.14809
7. Théry C, Witwer KW, Aikawa E, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the international society for extracellular vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7(1):1535750. doi:10.1080/20013078.2018.1535750
8. Liang Y, Lehrich BM, Zheng S, Lu M. Emerging methods in biomarker identification for extracellular vesicle-based liquid biopsy. J Extracell Vesicles. 2021;10(7):e12090. doi:10.1002/jev2.12090
9. Ramos-Zaldívar HM, Polakovicova I, Salas-Huenuleo E, et al. Extracellular vesicles through the blood-brain barrier: a review. Fluids Barriers CNS. 2022;19(1):60. doi:10.1186/s12987-022-00359-3
10. Shi M, Sheng L, Stewart T, Zabetian CP, Zhang J. New windows into the brain: central nervous system-derived extracellular vesicles in blood. Prog Neurobiol. 2019;175:96–106. doi:10.1016/j.pneurobio.2019.01.005
11. Jia L, Qiu Q, Zhang H, et al. Concordance between the assessment of Aβ42, T-tau, and P-T181-tau in peripheral blood neuronal-derived exosomes and cerebrospinal fluid. Alzheimer’s Dementia. 2019;15(8):1071–1080. doi:10.1016/j.jalz.2019.05.002
12. Jia L, Zhu M, Kong C, et al. Blood neuro-exosomal synaptic proteins predict Alzheimer’s disease at the asymptomatic stage. Alzheimers Dement. 2021;17(1):49–60. doi:10.1002/alz.12166
13. Dutta S, Hornung S, Kruayatidee A, et al. α-Synuclein in blood exosomes immunoprecipitated using neuronal and oligodendroglial markers distinguishes Parkinson’s disease from multiple system atrophy. Acta Neuropathol. 2021;142(3):495–511. doi:10.1007/s00401-021-02324-0
14. Jiang C, Hopfner F, Berg D, et al.. Validation of α‐synuclein in L1CAM‐immunocaptured exosomes as a biomarker for the stratification of parkinsonian syndromes. Mov Disord. 2021:
15. Delgado-Peraza F, Nogueras-Ortiz CJ, Volpert O, et al. Neuronal and astrocytic extracellular vesicle biomarkers in blood reflect brain pathology in mouse models of Alzheimer’s disease. Cells. 2021;10(5):993. doi:10.3390/cells10050993
16. Cheng L, Vella LJ, Barnham KJ, McLean C, Masters CL, Hill AF. Small RNA fingerprinting of Alzheimer’s disease frontal cortex extracellular vesicles and their comparison with peripheral extracellular vesicles. J Extracell Vesicles. 2020;9(1):1766822. doi:10.1080/20013078.2020.1766822
17. Kang M, Jordan V, Blenkiron C, Chamley LW. Biodistribution of extracellular vesicles following administration into animals: a systematic review. J Extracell Vesicles. 2021;10(8):e12085. doi:10.1002/jev2.12085
18. Iannotta D, A A, Kijas AW, Rowan AE, Wolfram J. Entry and exit of extracellular vesicles to and from the blood circulation. Nat Nanotechnol. 2024;19(1):13–20. doi:10.1038/s41565-023-01522-z
19. Cheng Y, Wang X, Yang J, et al. A translational study of urine miRNAs in acute myocardial infarction. J mol Cell Cardiol. 2012;53(5):668–676. doi:10.1016/j.yjmcc.2012.08.010
20. Wang Z, Hill S, Luther JM, Hachey DL, Schey KL. Proteomic analysis of urine exosomes by multidimensional protein identification technology (MudPIT). Proteomics. 2012;12(2):329–338. doi:10.1002/pmic.201100477
21. Fraser KB, Rawlins AB, Clark RG, et al. Ser(P)-1292 LRRK2 in urinary exosomes is elevated in idiopathic Parkinson’s disease. Mov Disord. 2016;31(10):1543–1550. doi:10.1002/mds.26686
22. Chen Y, Xia K, Chen L, Fan D. Increased interleukin-6 levels in the astrocyte-derived exosomes of sporadic amyotrophic lateral sclerosis patients. Front Neurosci-Switz. 2019;13:574. doi:10.3389/fnins.2019.00574
23. Goetzl EJ, Mustapic M, Kapogiannis D, et al. Cargo proteins of plasma astrocyte-derived exosomes in Alzheimer’s disease. The FASEB Journal. 2016;30(11):3853–3859. doi:10.1096/fj.201600756R
24. Goetzl EJ, Schwartz JB, Abner EL, Jicha GA, Kapogiannis D. High complement levels in astrocyte-derived exosomes of Alzheimer disease. Ann Neurol. 2018;83(3):544–552. doi:10.1002/ana.25172
25. Goetzl EJ, Srihari VH, Guloksuz S, Ferrara M, Tek C, Heninger GR. Decreased mitochondrial electron transport proteins and increased complement mediators in plasma neural-derived exosomes of early psychosis. Transl Psychiatry. 2020;10(1):361. doi:10.1038/s41398-020-01046-3
26. Goetzl EJ, Yaffe K, Peltz CB, et al. Traumatic brain injury increases plasma astrocyte-derived exosome levels of neurotoxic complement proteins. FASEB J. 2020;34(2):3359–3366. doi:10.1096/fj.201902842R
27. Lee EE, Winston-Gray C, Barlow JW, Rissman RA, Jeste DV. Plasma levels of neuron- and astrocyte-derived exosomal amyloid beta1-42, amyloid beta1-40, and phosphorylated tau levels in schizophrenia patients and non-psychiatric comparison subjects: relationships with cognitive functioning and psychopathology. Front Psychiatry. 2020;11:532624. doi:10.3389/fpsyt.2020.532624
28. Winston CN, Goetzl EJ, Schwartz JB, Elahi FM, Rissman RA. Complement protein levels in plasma astrocyte-derived exosomes are abnormal in conversion from mild cognitive impairment to Alzheimer’s disease dementia. Alzheimers Dement. 2019;11(1):61–66. doi:10.1016/j.dadm.2018.11.002
29. Xie XH, Lai WT, Xu SX, et al. Hyper-inflammation of astrocytes in patients of major depressive disorder: evidence from serum astrocyte-derived extracellular vesicles. Brain Behav Immun. 2022;109:S0889–1591(22)00472–X. doi:10.1016/j.bbi.2022.12.014
30. Edwardson MA, Mitsuhashi M, Van Epps D. Elevation of astrocyte-derived extracellular vesicles over the first month post-stroke in humans. Sci Rep. 2024;14(1):5272. doi:10.1038/s41598-024-55983-w
31. Xu SX, Xie XH, Yao L, et al. Human in vivo evidence of reduced astrocyte activation and neuroinflammation in patients with treatment-resistant depression following electroconvulsive therapy. Psychiatry Clin Neurosci. 2023;77(12):653–664. doi:10.1111/pcn.13596
32. Tamm I, Horsfall FL. A mucoprotein derived from human urine which reacts with influenza, mumps, and Newcastle disease viruses. J Exp Med. 1952;95(1):71–97. doi:10.1084/jem.95.1.71
33. Kosanović M, Janković M. Isolation of urinary extracellular vesicles from Tamm- Horsfall protein-depleted urine and their application in the development of a lectin-exosome-binding assay. Biotechniques. 2014;57(3):143–149. doi:10.2144/000114208
34. Uhlén M, Fagerberg L, Hallström BM, et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347(6220):
35. Zhu Q, Cheng L, Deng C, et al. The genetic source tracking of human urinary exosomes. Proc Natl Acad Sci USA. 2021;118(43):e2108876118. doi:10.1073/pnas.2108876118
36. Erdbrügger U, Blijdorp CJ, Bijnsdorp IV, et al. Urinary extracellular vesicles: a position paper by the urine task force of the international society for extracellular vesicles. J Extracell Vesicles. 2021;10(7):e12093. doi:10.1002/jev2.12093
37. Merchant ML, Rood IM, Deegens JKJ, Klein JB. Isolation and characterization of urinary extracellular vesicles: implications for biomarker discovery. Nat Rev Nephrol. 2017;13(12):731–749. doi:10.1038/nrneph.2017.148
38. Zhao Y, Wang Y, Zhao E, et al. PTRF/CAVIN1, regulated by SHC1 through the EGFR pathway, is found in urine exosomes as a potential biomarker of ccRCC. Carcinogenesis. 2020;41(3):274–283. doi:10.1093/carcin/bgz147
39. Ramirez-Garrastacho M, Berge V, Linē A, Llorente A. Potential of miRNAs in urinary extracellular vesicles for management of active surveillance in prostate cancer patients. Br J Cancer. 2022;126(3):492–501. doi:10.1038/s41416-021-01598-1
40. Lapitz A, Arbelaiz A, O’Rourke CJ, et al. Patients with cholangiocarcinoma present specific RNA profiles in serum and urine extracellular vesicles mirroring the tumor expression: novel liquid biopsy biomarkers for disease diagnosis. Cells. 2020;9(3):721. doi:10.3390/cells9030721
41. Olivares D, Perez-Hernandez J, Perez-Gil D, Chaves FJ, Redon J, Cortes R. Optimization of small RNA library preparation protocol from human urinary exosomes. J Transl Med. 2020;18(1):132. doi:10.1186/s12967-020-02298-9
42. Skotland T, Ekroos K, Kauhanen D, et al. Molecular lipid species in urinary exosomes as potential prostate cancer biomarkers. Eur J Cancer. 2017;70:122–132. doi:10.1016/j.ejca.2016.10.011
43. Øverbye A, Skotland T, Koehler CJ, et al. Identification of prostate cancer biomarkers in urinary exosomes. Oncotarget. 2015;6(30):30357–30376. doi:10.18632/oncotarget.4851
44. Zhu Q, Li Q, Niu X, et al. Extracellular vesicles secreted by human urine-derived stem cells promote ischemia repair in a mouse model of hind-limb ischemia. Cell Physiol Biochem. 2018;47(3):1181–1192. doi:10.1159/000490214
45. Cvjetkovic A, Lötvall J, Lässer C. The influence of rotor type and centrifugation time on the yield and purity of extracellular vesicles. J Extracell Vesicles. 2014;3. doi:10.3402/jev.v3.23111
46. Rothhammer V, Quintana FJ. Control of autoimmune CNS inflammation by astrocytes. Semin Immunopathol. 2015;37(6):625–638. doi:10.1007/s00281-015-0515-3
47. Van Wagoner NJ, Oh JW, Repovic P, Benveniste EN. Interleukin-6 (IL-6) production by astrocytes: autocrine regulation by IL-6 and the soluble IL-6 receptor. J Neurosci. 1999;19(13):5236–5244. doi:10.1523/JNEUROSCI.19-13-05236.1999
48. Huang JP, Lin CH, Tseng CW, Chien MH, Lee HC, Yang KD. First-trimester urinary extracellular vesicles as predictors of preterm birth: an insight into immune programming. Front Cell Dev Biol. 2023;11:1330049. doi:10.3389/fcell.2023.1330049
49. Medeiros T, Alves LS, Cabral-Castro MJ, et al. Exploring urinary extracellular vesicles and immune mediators as biomarkers of kidney injury in COVID-19 hospitalized patients. Diagnostics. 2022;12(11):2600. doi:10.3390/diagnostics12112600
50. Shemilt M, Boutin A, Lauzier F, et al. Prognostic value of glial fibrillary acidic protein in patients with moderate and severe traumatic brain injury: a systematic review and meta-analysis. Crit Care Med. 2019;47(6):e522–e529. doi:10.1097/CCM.0000000000003728
51. Kohlhase K, Frank F, Wilmes C, et al. Brain-specific biomarkers in urine as a non-invasive approach to monitor neuronal and glial damage. Eur J Neurol. 2023;30(3):729–740. doi:10.1111/ene.15641
52. Posti JP, Hossain I, Takala RSK, et al.. Glial fibrillary acidic protein and ubiquitin c-terminal hydrolase-II are not specific biomarkers for mild CT-negative traumatic brain injury. J Neurotraum. 2017;34(7):1427–1438. doi:10.1089/neu.2016.4442
53. Mehta T, Fayyaz M, Giler GE, et al. Current trends in biomarkers for traumatic brain injury. Open Access J Neurol Neurosurg. 2020;12(4):86–94.
54. Forró T, Manu DR, Băjenaru OL, Bălașa R. GFAP as astrocyte-derived extracellular vesicle cargo in acute ischemic stroke patients-a pilot study. Int J mol Sci. 2024;25(11):5726. doi:10.3390/ijms25115726
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




