Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
Knowledge, Attitude, and Belief of Healthcare Professionals Toward Obesity Stigmatization
Authors Lang H , Zhang X, Yan N, Du J, Jiang X
Received 8 October 2024
Accepted for publication 14 March 2025
Published 7 April 2025 Volume 2025:18 Pages 1935—1946
DOI https://doi.org/10.2147/JMDH.S499828
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Hongmei Lang,1,* Xingping Zhang,1,* Na Yan,1 Juan Du,1 Xiaoyan Jiang2
1Department of General Medicine, Chengdu Second People’s Hospital, Chengdu, Sichuan, 610021, People’s Republic of China; 2Department of Endocrinology and Metabolism, Chongqing Emergency Medical Center, Chongqing University Central Hospital, Chongqing, 400014, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongmei Lang, Department of General Medicine, Chengdu Second People’s Hospital, No. 10 Qingyun South Street, Jinjiang District, Chengdu, Sichuan, 610021, People’s Republic of China, Tel/Fax +86-18040368202, Email [email protected] Xiaoyan Jiang, Email [email protected]
Objective: Obesity stigmatization, defined as the social devaluation and denigration of individuals because of their excess weight, represents a significant barrier to effective healthcare delivery. This study aimed to investigate healthcare professionals’ knowledge about obesity-related health impacts, attitudes regarding weight bias (negative or discriminatory attitudes toward individuals with obesity), and beliefs about the causes and nature of obesity.
Methods: This cross-sectional study was conducted among healthcare professionals between Jan, 2024 and Feb, 2024 in The Department of General Medicine, Chengdu Second People’s Hospital, using a self-designed questionnaire.
Results: A total of 388 valid questionnaires [303 (78.09%) female and a mean age of 37.71 ± 8.46 years] were included. The mean scores for knowledge, attitude, and belief were 6.70 ± 1.46 (possible range: 0– 10), 38.41 ± 5.09 (possible range: 8– 48), and 63.53 ± 15.35 (possible range: 0– 120), respectively. Multivariate logistic regression analysis revealed that having body mass index ≥ 24.0 kg/m² (OR = 0.537, 95% CI: 0.331– 0.873, P = 0.012) and nurse profession (OR = 0.546, 95% CI: 0.338– 0.883, P = 0.014) were independently associated with knowledge. Knowledge (OR = 0.754, 95% CI: 0.600– 0.949, P = 0.016), belief (OR = 0.915, 95% CI: 0.854– 0.980, P = 0.011), and age (OR = 0.950, 95% CI: 0.906– 0.995, P = 0.031) were independently associated with attitude. Moreover, structural equation modeling showed that knowledge had a significant direct effect on both belief (β = 0.845, P < 0.001) and attitude (β = − 0.944, P < 0.001), as well as belief on attitude (β = − 0.550, P < 0.001).
Conclusion: Healthcare professionals exhibited insufficient knowledge, negative attitude and belief toward obesity stigmatization. A pressing necessity arises for the implementation of targeted educational interventions and awareness programs within healthcare settings.
Keywords: knowledge, belief, attitude, healthcare professional, obesity stigmatization, cross-sectional study
Introduction
Obesity, defined by the World Health Organization as a body mass index (BMI) ≥30 kg/m², has become a major public health concern.1 The rising rates of obesity are alarming, as they are linked to an increased risk of chronic diseases, such as cardiovascular disease (CVD), diabetes, stroke, and cancer. These conditions are significant contributors to global mortality, accounting for approximately 4.8% of deaths worldwide.2,3 The health implications of obesity go beyond physical health. Individuals with obesity often face mental health challenges and psychosocial difficulties. They experience widespread discrimination and stigmatization, which significantly affects their mental well-being.4 Healthcare professionals’ perspectives warrant particular attention for several reasons. First, they are at the forefront of obesity management and their attitudes directly influence treatment outcomes.5,6 Second, their professional authority makes their beliefs particularly influential in shaping patients’ self-perception and treatment adherence. Third, healthcare settings often represent critical points of intervention where stigmatization can either be perpetuated or actively addressed.7,8 Understanding and improving healthcare professionals’ knowledge, attitudes, and beliefs is therefore fundamental to developing effective anti-stigma interventions in healthcare settings. Obesity discrimination manifests uniquely in children, who face stigmatization in educational settings, peer relationships, and family environments.9 Such early-life discrimination can significantly impact their social development, academic performance, and long-term psychological well-being.10,11 Studies have shown that individuals with obesity experience widespread discrimination across multiple life domains. In healthcare settings, this discrimination may manifest as reduced quality of care; in employment, it often appears as decreased job opportunities and lower wages; in social relationships, it frequently leads to isolation and reduced social support.12 The consequences of obesity discrimination extend beyond social impacts, affecting both psychological and physical health. Psychologically, individuals experiencing weight stigma often exhibit increased rates of depression, anxiety, and poor self-esteem. Physically, discrimination-related stress can lead to elevated cortisol levels and adverse cardiovascular responses.13,14 Obesity stigmatization in healthcare settings can significantly impact the quality and standard of clinical care. Studies have shown that weight bias among healthcare providers may lead to shortened consultation times, reduced therapeutic alliance, and delayed or avoided medical visits by patients, ultimately compromising healthcare outcomes.15 Beyond individual health implications, obesity poses substantial economic burden on healthcare systems and society at large.16
The “Knowledge-Attitude-Belief (KAB)” survey is a pivotal behavioral theory that has significantly influenced the understanding and modification of human health behaviors.17 This framework, emphasizing the interconnection between knowledge, attitude, belief, and practices, has been extensively utilized in the exploration of health behavior and decision-making processes.18 Healthcare professionals’ perspectives warrant particular attention for several reasons. First, they are at the forefront of obesity management and their attitudes directly influence treatment outcomes. Second, their professional authority makes their beliefs particularly influential in shaping patients’ self-perception and treatment adherence. Third, healthcare settings often represent critical points of intervention where stigmatization can either be perpetuated or actively addressed. Understanding and improving healthcare professionals’ knowledge, attitudes, and beliefs is therefore fundamental to developing effective anti-stigma interventions in healthcare settings. The attitude and belief of healthcare professionals play a critical role in patient care, directly impacting the quality of treatment and services provided to individuals with obesity. Recognizing and addressing any potential biases and stigmatization within this group toward obesity is crucial for enhancing the medical care experience and treatment outcomes for obese patients.
Despite numerous studies exploring the Knowledge-Attitude-Practice (KAP) concerning obesity,19–21 there remains a gap in research specifically targeting the current direction of understanding healthcare professionals’ knowledge, belief, and attitude toward obesity stigmatization. Addressing this gap, this study aimed to investigate knowledge, attitude, and belief among healthcare professionals toward obesity stigmatization.
Methods
Study Design and Participants
This cross-sectional study was conducted among healthcare professionals between Jan,2024 and Feb, 2024 in the Department of General Medicine, Chengdu Second People’s Hospital. The inclusion criteria encompassed clinical healthcare professionals currently employed in the hospital who voluntarily consented to participate in the study. Conversely, medical students, residents in training, and healthcare professionals lacking appropriate qualifications were excluded from the study. The exclusion of medical students and residents was based on the study’s focus on healthcare professionals with independent clinical practice experience and established patterns of patient interaction. Ethical approval for this study was obtained from the Medical Ethics Committee of Chengdu Second People’s Hospital (approval No: 2024023), and informed consent was duly obtained from all study participants.
Questionnaire
The questionnaire design was informed by relevant literature22–25 and underwent refinement based on feedback from five endocrinology experts. A pilot study involving a small sample size (69 participants) was conducted, resulting in a reliability coefficient of 0.701. The final questionnaire, administered in Chinese, comprises four sections: demographic information [age, gender, body mass index (BMI, with obesity defined as BMI ≥30 kg/m² according to WHO criteria), education, occupation type, professional title, department, years of working], the knowledge dimension, the belief dimension, and the attitude dimension. The knowledge dimension encompassed a total of 10 questions, each scored 1 point for a correct response and 0 points for an incorrect answer, with a score range of 0–10. The belief dimension comprises 8 questions, employing a six-point Likert scale ranging from strongly agree (6 points) to strongly disagree (1 point), yielding a score range of 8–48. The attitude dimension consists of 20 questions, graded from strongly agree (+3 points) to strongly disagree (−3 points), with reverse scoring applied to items 2–6, 10–12, 14–16, and 19–20. The total score for all 20 items, plus 60 points, constitutes the attitude score, which spans from 0 to 120. A higher attitude score indicates a more positive or favorable attitude toward obese individuals, while a lower score signifies a negative or unfavorable attitude. Adequate knowledge, positive attitude, and strong belief are defined as achieving a total score exceeding 70% for each dimension.26
Questionnaire Distribution and Quality Control
The study recruited medical professionals from various departments in hospitals located in the southeast (Sichuan province) and northwest regions of the country by coordinating with department heads to administer a questionnaire survey. While this sampling approach included geographical diversity, we acknowledge that it may not fully represent the perspectives of healthcare professionals across all regions of China. Questionnaires were distributed electronically to participants via WeChat and QQ groups for healthcare workers. An online survey platform, Sojump (https://www.wjx.cn), was utilized to deliver the questionnaires to healthcare professionals. Participants could access and complete the questionnaire by scanning a QR code using WeChat or by following a provided link. To ensure data quality and encourage comprehensive responses, a one-submission-per-IP address restriction was implemented, and all questionnaire items were made mandatory. Participants were guaranteed anonymity throughout the survey process. The research team, consisting of three doctors trained as research assistants responsible for questionnaire promotion and distribution, rigorously examined all submissions for completeness, internal consistency, and logical coherence. Investigators were well-versed in understanding the research questions and the survey process, which enhanced data accuracy and consistency. Questionnaires exhibiting logical errors, incomplete responses, or uniform answers across all items were categorized as invalid.
Sample Size Calculation
Ideally, the sample size should be a minimum of 5–10 times the number of predictors.27,28 Given that this questionnaire includes 38 independent variables, the required minimum sample size would be 190. To account for potential non-response, a 20% buffer is factored in, resulting in a final necessary sample size of 238.
Statistical Analysis
The statistical analyses were carried out using SPSS version 22 and AMOS version 22 (IBM, Armonk, NY, USA). Continuous variables were described using mean ± standard deviation (SD), and between-group comparisons were performed using t-tests or analysis of variance (ANOVA). Categorical variables were presented as n (%). Pearson’s correlation analysis was employed to assess the correlations between KAB scores. In multivariate analysis, 70% of the total score was used as the cut-off value. Univariate variables with P<0.05 were enrolled in multivariate regression. Structural equation modeling (SEM) was utilized to test the hypotheses that 1) knowledge affects attitude, 2) knowledge impacts belief, and 3) attitude influences belief. Model fit was assessed using multiple indices including chi-square/degrees of freedom ratio (χ2/df), comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). Values of χ2/df < 3, CFI and TLI > 0.95, RMSEA < 0.06, and SRMR < 0.08 indicate good model fit. Two-sided P<0.05 were considered statistically significant in this study.
Results
Initially, a total of 402 questionnaires were returned, and the following were invalid: 3 cases classified as gender outliers, 3 cases with missing age information, 8 cases with BMI values exceeding 40, and 1 case identified as an outlier in terms of work experience. Consequently, a total of 388 valid questionnaires remained, with a validity rate of 96.52%. Among these, 303 respondents (78.09%) were female, the mean age were 37.71 ± 8.46 years. Additionally, 256 respondents (65.98%) had BMI of less than 24 kg/m², 239 (61.60%) held bachelor’s degrees, 239 (61.60%) were doctors, 140 (36.08%) held intermediate professional titles, and 176 (45.36%) belonged to the department of internal medicine. The mean years of working experience among participants was 14.05 ± 8.76 years. The mean scores for knowledge, belief, and attitude were 6.70 ± 1.46 (possible range: 0–10), 38.41 ± 5.09 (possible range: 8–48), and 63.53 ± 15.35 (possible range: 0–120), respectively. Subsequent analyses of demographic differences revealed that individuals with BMI < 24.0 kg/m² (P = 0.033) and those with a doctorate degree (P = 0.012) were more likely to have higher knowledge (Table 1).
 |
Table 1 Demographic Characteristics and KAB Score |
In the domain of knowledge, the distribution of correctness rates revealed that the two knowledge items exhibiting the highest accuracy were as follows: “Obesity does not increase the risk of hypertension” (K8) with a correctness rate of 93.56%, and “People with a ‘beer belly’ have a higher risk of developing diabetes” (K1) with a correctness rate of 92.01%. Conversely, the two items with the lowest correctness rates were “To achieve significant health benefits after a person with obesity develops diabetes, it is necessary to lose at least 40% of body weight” (K3) with a correctness rate of 19.33%, and “Obesity increases the risk of food allergies” (K10) with a correctness rate of 23.45% (Supplementary Table 1).
Within the belief dimension, 51.55% of respondents concurred that individuals addicted to food typically become obese (B8), while 47.68% concurred that obesity is often the result of a physiological disorder (B2). Notably, the item “Obesity is rarely caused by a lack of willpower” (B7) stood out with 26.03% of respondents in agreement and 22.16% in disagreement, displaying a significant divergence in responses (Supplementary Table 2).
The attitude of healthcare professionals exhibited considerable variability, as indicated by 12.37% strongly agreeing that one of the worst outcomes for an individual is becoming obese (A20), 31.70% agreeing that extremely obese individuals tend to appear less well-groomed (A6), and 35.05% somewhat agreeing that a very small proportion of obese individuals would feel ashamed of their weight (A13). Conversely, 39.18% strongly disagreed that obese individuals should not expect to lead a normal life (A16), 39.43% disagreed that most obese individuals harbor resentment toward people of normal weight (A14), and 36.60% somewhat disagreed that obese individuals are typically sociable (A7) (Supplementary Table 3).
Correlation analysis showed knowledge and belief exhibited a weak positive correlation (r = 0.130, simple P = 0.010). However, knowledge and attitude showed a significant negative correlation (r = −0.125, simple P = 0.013), as were belief and attitude (r = −0.360, simple P < 0.001).
Analyzing the distribution of scores, it was observed that 123 participants (31.70%) had a knowledge score exceeding 7, 322 participants (82.99%) had a belief score higher than 33.6, and 36 participants (9.28%) achieved an attitude score greater than 84. Multivariate logistic regression analysis revealed that having BMI ≥24.0 kg/m² (OR = 0.537, 95% CI: 0.331–0.873, P = 0.012) and nurse profession (OR = 0.546, 95% CI: 0.338–0.883, P = 0.014) were independently associated with knowledge (Table 2). Furthermore, knowledge (OR = 0.754, 95% CI: 0.600–0.949, P = 0.016), belief (OR = 0.915, 95% CI: 0.854–0.980, P = 0.011), and age (OR = 0.950, 95% CI: 0.906–0.995, P = 0.031) were independently associated with attitude (Table 3).
 |
Table 2 Univariate and Multivariate Analysis for Knowledge |
 |
Table 3 Univariate and Multivariate Analysis for Attitude |
The model fit indices demonstrated excellent model fit (χ2/df = 2.31, < 3; CFI = 0.967, > 0.95; TLI = 0.956, > 0.95; RMSEA = 0.058, < 0.06; SRMR = 0.039, < 0.08) (Supplementary Table 4), indicating the proposed theoretical framework adequately explains the relationships among variables. SEM results revealed complex relationships among the three key variables. Knowledge showed a strong positive direct effect on belief (β = 0.845, simple p < 0.001), suggesting that increased knowledge levels are associated with stronger beliefs about obesity stigmatization. Interestingly, both knowledge and belief demonstrated significant negative effects on attitude (β = −0.944, simple p < 0.001 and β = −0.550, simple p < 0.001, respectively), indicating that higher levels of knowledge and stronger beliefs are associated with more negative attitudes toward obesity stigmatization. The model also revealed significant indirect effects, with belief partially mediating the relationship between knowledge and attitude (indirect effect = −0.465, simple p < 0.001) (Table 4 and Figure 1).
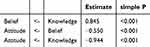 |
Table 4 SEM Results |
Discussion
The study reveals that healthcare professionals exhibit insufficient knowledge, negative attitude, and negative belief toward obesity stigmatization, highlighting a concerning gap in their understanding and perceptions. To address this issue, it is essential to implement targeted training programs and interventions aimed at improving healthcare professionals’ knowledge and promoting more empathetic and unbiased attitude toward individuals with obesity, ultimately fostering a more inclusive and supportive healthcare environment.
The findings of this study shed light on the prevailing knowledge, belief, and attitude of healthcare professionals toward obesity stigmatization, revealing a concerning gap in their understanding and perceptions. The results underscore the need for targeted interventions and educational programs within healthcare settings to address these issues effectively. The variations observed across different categories of healthcare professionals provide valuable insights into the factors influencing their perspectives. Firstly, the gender-based differences revealed that females exhibited higher scores in knowledge, belief, and attitude domains. This aligns with previous research suggesting that women tend to have more empathetic attitude and greater awareness of the complexities surrounding obesity.29,30 In contrast, male healthcare professionals may benefit from tailored training programs addressing these disparities.
Additionally, the association between BMI and knowledge scores suggests that individuals with higher BMIs tend to have lower knowledge levels. This finding is consistent with previous studies highlighting the importance of addressing bias and misconceptions associated with obesity.31–33 Studies have reported similar knowledge deficits among healthcare providers, with particular gaps in understanding the complex etiology of obesity. Similar to our findings, previous research has found that providers with higher BMI showed lower knowledge scores, suggesting a potential link between personal weight status and professional understanding of obesity stigmatization.34 Tailored educational initiatives targeting this knowledge gap should be considered. Occupational differences, with doctors demonstrating higher knowledge scores than nurses, underscore the need for specialized training in nursing education programs. The observed differences in knowledge scores based on BMI and professional roles warrant further discussion. Healthcare professionals with higher BMI might demonstrate different knowledge levels possibly due to their personal experiences with weight-related issues, which could influence their understanding and awareness of obesity stigmatization. This finding aligns with previous studies suggesting that personal weight status can affect healthcare providers’ perspectives and approach to obesity management.35 The knowledge difference between doctors and nurses might be attributed to variations in professional training, scope of practice, and patient interaction patterns.36,37 Doctors typically receive more extensive theoretical training in obesity pathophysiology and management, while nurses often have more frequent direct patient contact and practical care experience.38,39 These distinct professional characteristics suggest the need for tailored educational interventions that address the specific needs and roles of different healthcare professionals. For instance, nursing education programs might benefit from enhanced theoretical content about obesity stigmatization, while physician training could focus more on practical application and patient communication skills.40,41 Collaboration between healthcare professions can facilitate knowledge exchange and foster more comprehensive understanding of obesity-related issues. Furthermore, participants with doctorate degrees exhibited higher knowledge scores, emphasizing the potential benefits of advanced education in promoting nuanced perspectives on obesity stigmatization.42,43 The negative attitudes observed in our study are consistent with previous research on healthcare professionals’ weight bias. Studies have found comparable levels of negative attitudes among medical practitioners, with attitude scores consistently indicating the presence of weight bias.44,45 Our finding that older age is associated with more negative attitudes parallels previous research showing that experienced healthcare providers often hold more entrenched weight-related biases.
The observed correlations among knowledge, belief, and attitude indicate complex relationships among these constructs. While knowledge and belief displayed a positive correlation, knowledge and attitude were negatively correlated. This suggests that increasing knowledge alone may not necessarily lead to improved attitude. The relationship between knowledge and beliefs found in our structural equation model supports previous research that identified similar connections between healthcare providers’ knowledge levels and their beliefs about obesity stigmatization. However, our finding that increased knowledge correlates with more negative attitudes contrasts with some previous studies. Research has found that higher knowledge levels were associated with more positive attitudes toward patients with obesity, suggesting that the relationship between knowledge and attitudes may be context-dependent.46,47 Addressing negative attitude requires a multifaceted approach that goes beyond factual information dissemination.48,49 The findings from the SEM underline the significance of knowledge in influencing belief and attitude, emphasizing the importance of knowledge-focused interventions.
In the knowledge dimension, it is encouraging to note that a majority of respondents correctly recognized the association between obesity and health risks such as diabetes and colorectal cancer, indicating a baseline level of awareness. However, there were misconceptions toward the necessity of extreme weight loss for health benefits and the life expectancy of obese individuals. Given the prevalence of misconceptions, such as the belief that extreme weight loss is necessary for health benefits, interventions should provide accurate and evidence-based information on the health risks associated with obesity. These educational programs should also address the life expectancy misconceptions and emphasize the importance of a nuanced understanding of obesity-related health outcomes. Providing healthcare professionals with up-to-date resources and access to continuing education opportunities can help bridge the knowledge gap and ensure that they are well-informed when addressing obesity-related concerns with patients.50,51
Moving to the belief dimension, it is concerning to observe that a substantial proportion of healthcare professionals held stigmatizing belief related to obesity. Belief associating obesity with emotional compensation, physiological imbalances, and binge eating are indicative of negative stereotypes that can perpetuate stigmatization.52–54 Moreover, the notion that obesity is primarily caused by a lack of willpower or poor dietary habits reflects the need for targeted interventions to challenge these misconceptions. The belief that individuals may be addicted to food, akin to drug addiction, highlights the need for a nuanced understanding of the complex factors contributing to obesity. Educational programs should address the misconception that obesity is primarily a result of poor willpower or dietary habits by highlighting the multifactorial nature of obesity, including genetic, physiological, and environmental factors. Moreover, promoting empathy and sensitivity training can help healthcare professionals develop a more compassionate and non-judgmental approach when interacting with individuals with obesity. Encouraging self-awareness and reflection can also be beneficial in recognizing and addressing personal biases and belief that may affect patient care.55,56
In the attitude dimension, the findings underscore the presence of negative attitude toward obese individuals among healthcare professionals. Belief that obese individuals are inferior, less successful in their work, and less likely to be chosen as partners for marriage are indicative of bias and stigma. These attitudes can have detrimental consequences for the quality of care provided to individuals with obesity, leading to disparities in healthcare outcomes. Additionally, the belief that obese individuals are more aggressive or emotionally expressive highlights the need to challenge these stereotypes, as they can influence healthcare professionals’ interactions with their patients. Healthcare professionals should receive training on patient-centered care and communication skills, with a focus on reducing weight-based bias and discrimination. Additionally, fostering collaboration among healthcare professions is essential to create a unified approach to addressing obesity-related issues. Interdisciplinary training and teamwork can help improve attitude by promoting a shared understanding of the challenges faced by individuals with obesity and the importance of a supportive healthcare system.57,58
This study has several limitations that should be considered. First, the cross-sectional design limits our ability to establish causal relationships between variables and observe changes over time. Second, the self-reported nature of the data may introduce social desirability bias, particularly given the sensitive nature of stigmatization-related questions. Third, our sample was predominantly from two geographical regions, which may limit the generalizability of findings to other healthcare settings or regions. Finally, while we excluded medical students and residents to focus on practicing healthcare professionals, this decision may have limited our understanding of how attitudes and knowledge develop during professional training.
In conclusion, this study revealed significant gaps in healthcare professionals’ knowledge, attitudes, and beliefs regarding obesity stigmatization. Specifically, we found that healthcare professionals with higher BMI and those in nursing roles demonstrated lower knowledge scores, suggesting the need for targeted educational approaches. The complex relationships identified through structural equation modeling, particularly the interactions between knowledge, beliefs, and attitudes, highlight the need for comprehensive intervention strategies. These findings indicate that merely increasing knowledge may not be sufficient to improve attitudes, and interventions should address both cognitive and affective components of obesity stigmatization. Based on these findings, we recommend implementing multi-faceted educational interventions that: (1) address profession-specific knowledge gaps, (2) challenge existing negative beliefs about obesity, and (3) promote positive attitudes through practical clinical scenarios. Future healthcare education programs should incorporate anti-stigma training, emphasizing patient-centered care approaches and evidence-based obesity management strategies. Regular assessment of healthcare professionals’ attitudes and beliefs, coupled with continuous professional development in this area, may help create more supportive and effective healthcare environments for individuals with obesity.
Contribution to the Research Field
This study aimed to explore the knowledge, attitude, and beliefs of healthcare professionals regarding obesity stigmatization. Conducted between January and February 2024 among healthcare professionals at a specific hospital, the study found that participants generally had low scores in knowledge, exhibited negative attitudes, and held unfavorable beliefs towards obesity stigmatization. The findings highlighted that factors such as body mass index and profession influenced healthcare professionals’ knowledge levels. Additionally, knowledge was found to directly impact both belief and attitude, while belief also influenced attitude. The results underscored the urgent need for focused educational initiatives and awareness campaigns within healthcare environments to address and counteract the prevalent biases and misconceptions surrounding obesity. The study’s contribution lies in shedding light on the deficiencies in healthcare professionals’ perspectives on obesity stigmatization and advocating for targeted interventions to foster a more empathetic and informed approach within the healthcare sector.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethics Approval and Consent to Participate
I confirm that all methods were performed in accordance with the relevant guidelines. This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study has been approved by the Medical Ethics Committee of Chengdu Second People’s Hospital (No. 2024023), and informed consent was obtained from each patient.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Grants from the Chengdu Second People’s Hospital Research Project Fund (grant number 2023-RC-002).
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization. Obesity and overweight. Available from: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
2. Chung W, Park JH, Chung HS, Yu JM, Kim DS, Moon S. Utility of the Z-score of log-transformed A body shape index (LBSIZ) in the assessment for sarcopenic obesity and cardiovascular disease risk in the United States. Sci Rep. 2019;9(1):9292. doi:10.1038/s41598-019-45717-8
3. Moon S, Oh CM, Choi MK, et al. The influence of physical activity on risk of cardiovascular disease in people who are obese but metabolically healthy. PLoS One. 2017;12(9):e0185127. doi:10.1371/journal.pone.0185127
4. Durrer Schutz D, Busetto L, Dicker D, et al. European practical and patient-centred guidelines for adult obesity management in primary care. Obesity Facts. 2019;12(1):40–66. doi:10.1159/000496183
5. Perdomo CM, Cohen RV, Sumithran P, Clément K, Frühbeck G. Contemporary medical, device, and surgical therapies for obesity in adults. Lancet. 2023;401(10382):1116–1130. doi:10.1016/S0140-6736(22)02403-5
6. Wong G, Srivastava G. Obesity management in children and adolescents. Gastroenterol Clin North Am. 2023;52(2):443–455. doi:10.1016/j.gtc.2023.03.011
7. Chen Y, Dabbas W, Gangemi A, et al. Obesity management and chronic kidney disease. Semin Nephrol. 2021;41(4):392–402.
8. Kheniser K, Saxon DR, Kashyap SR. Long-term weight loss strategies for obesity. J Clin Endocrinol Metab. 2021;106(7):1854–1866. doi:10.1210/clinem/dgab091
9. Abdalla Ahmed MA, Ssemmondo E, Mark-Wagstaff C, Sathyapalan T. Advancements in the management of obesity: a review of current evidence and emerging therapies. Expert Rev Endocrinol Metab. 2024;19(3):257–268. doi:10.1080/17446651.2024.2347258
10. Pont SJ, Puhl R, Cook SR, Slusser W. Stigma experienced by children and adolescents with obesity. Pediatrics. 2017;140(6).
11. Puhl RM, Lessard LM. Weight stigma in youth: prevalence, consequences, and considerations for clinical practice. Curr Obes Rep. 2020;9(4):402–411. doi:10.1007/s13679-020-00408-8
12. Alberga AS, Pickering BJ, Alix Hayden K, et al. Weight bias reduction in health professionals: a systematic review. Clin Obes. 2016;6(3):175–188. doi:10.1111/cob.12147
13. Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141–1163.
14. Wu YK, Berry DC. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: a systematic review. J Adv Nurs. 2018;74(5):1030–1042. doi:10.1111/jan.13511
15. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–326. doi:10.1111/obr.12266
16. Goettler A, Grosse A, Sonntag D. Productivity loss due to overweight and obesity: a systematic review of indirect costs. BMJ Open. 2017;7(10):e014632. doi:10.1136/bmjopen-2016-014632
17. Tan J, Luo L, Zhang M, et al. A Chinese and Western medication adherence scale in patients with chronic kidney disease. Patient Prefer Adher. 2019;13:1487–1495. doi:10.2147/PPA.S207693
18. Tan YL, Chen ZY, He YP, Xu G, Yu ZP, Zhu JF. Awareness of tobacco control policies and anti-tobacco attitudes and behaviors among school personnel. Tob Induc Dis. 2022;20(54):1–11. doi:10.18332/tid/149926
19. Laar RA, Shi S, Ashraf MA, Khan MN, Bibi J, Liu Y. Impact of physical activity on challenging obesity in Pakistan: a Knowledge, Attitude, and Practice (KAP) study. Int J Environ Res Public Health. 2020;17(21):7802. doi:10.3390/ijerph17217802
20. Wu V, Rosen C, Pan S, Mogilner L. Screening and managing obesity: understanding paediatric residents’ knowledge, attitudes and practice. Postgrad Med J. 2022;98(1160):428–433. doi:10.1136/postgradmedj-2020-139318
21. Xue B, Zhang X, Li T, et al. Knowledge, attitude, and practice of obesity among university students. Ann Palliat Med. 2021;10(4):4539–4546. doi:10.21037/apm-21-573
22. Ip EH, Marshall S, Vitolins M, et al. Measuring medical student attitudes and beliefs regarding patients who are obese. Acad Med. 2013;88(2):282–289. doi:10.1097/ACM.0b013e31827c028d
23. Nadolsky K, Addison B, Agarwal M, et al. American association of clinical endocrinology consensus statement: addressing stigma and bias in the diagnosis and management of patients with obesity/adiposity-based chronic disease and assessing bias and stigmatization as determinants of disease severity. Endocr Pract. 2023;29(6):417–427. doi:10.1016/j.eprac.2023.03.272
24. Puhl RM, Luedicke J, Grilo CM. Obesity bias in training: attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity. 2014;22(4):1008–1015. doi:10.1002/oby.20637
25. Weghuber D, Khandpur N, Boyland E, et al. Championing the use of people-first language in childhood overweight and obesity to address weight bias and stigma: a joint statement from the European-Childhood-Obesity-Group (ECOG), the European-Coalition-for-People-Living-with-Obesity (ECPO), the International-Paediatric-Association (IPA), Obesity-Canada, the European-Association-for-the-Study-of-Obesity Childhood-Obesity-Task-Force (EASO-COTF), Obesity Action Coalition (OAC), The Obesity Society (TOS) and the World-Obesity-Federation (WOF). Pediatric Obesity. 2023;18(6):e13024. doi:10.1111/ijpo.13024
26. Lee F, Suryohusodo AA. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: a cross-sectional study. Front Public Health. 2022;10:957630. doi:10.3389/fpubh.2022.957630
27. Li H, Zheng L, Le H, et al. The mediating role of internalized stigma and shame on the relationship between COVID-19 related discrimination and mental health outcomes among back-to-school students in Wuhan. Int J Environ Res Public Health. 2020;17(24):9237.
28. Ping NI, Jing-Li C, Na L. The sample size estimation in quantitative nursing research. Chin J Nurs. 2010;45:378e80.
29. Flannery C, McHugh S, Kenny LC, et al. Exploring obstetricians’, midwives’ and general practitioners’ approach to weight management in pregnant women with a BMI ≥25 kg/m(2): a qualitative study. BMJ Open. 2019;9(1):e024808. doi:10.1136/bmjopen-2018-024808
30. Hellgren MI, Kitsche E, Groot-Zevert M, Lindblad U, Daka B. Association between body mass index and self-rated health: a Swedish population-based longitudinal study. Scand J Public Health. 2021;49(4):369–376. doi:10.1177/1403494819875012
31. Dickerson RN, Andromalos L, Brown JC, et al. Obesity and critical care nutrition: current practice gaps and directions for future research. Critical Care. 2022;26(1):283. doi:10.1186/s13054-022-04148-0
32. Fruh SM, Graves RJ, Hauff C, Williams SG, Hall HR. weight bias and stigma: impact on health. Nurs Clin North Am. 2021;56(4):479–493. doi:10.1016/j.cnur.2021.07.001
33. Westbury S, Oyebode O, van Rens T, Barber TM. Obesity stigma: causes, consequences, and potential solutions. Curr Obes Rep. 2023;12(1):10–23. doi:10.1007/s13679-023-00495-3
34. Sun T, Zhang H, Kong Z, Yang J, Jia X. Knowledge, attitude, and practice of body shape and fitness among university students in China. BMC Public Health. 2023;23(1):1208. doi:10.1186/s12889-023-16122-8
35. Zeng Q, Li N, Pan XF, Chen L, Pan A. Clinical management and treatment of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):393–405. doi:10.1016/S2213-8587(21)00047-4
36. Makarem NN, Brome D, Romani M. Knowledge, attitude, and practices of complementary and alternative medicine: a survey of physicians and nurses at an academic medical center in Beirut. Libyan J Med. 2022;17(1):2071813. doi:10.1080/19932820.2022.2071813
37. Maribbay GML, Bdair IA, Alalyani MM, Al-Shloul MN. Nurses’ knowledge, attitudes, and barriers toward pain assessment and management in Assir Region, Saudi Arabia. J Holist Nurs. 2023;41(1):90–100. doi:10.1177/08980101221076677
38. Goodarzi A, Sadeghian E, Babaei K, Khodaveisi M. Knowledge, attitude and decision-making of nurses in the resuscitation team towards terminating resuscitation and do-not-resuscitate order. Ethiop J Health Sci. 2022;32(2):413–422. doi:10.4314/ejhs.v32i2.22
39. Hirachan N, Shrestha N. Knowledge, attitude and practice of medical ethics among doctors and nurses in Pokhara Valley, Nepal. Kathmandu Univ Med J. 2022;20(80):351–358. doi:10.3126/kumj.v20i4.54275
40. Carlsson F, Jacobsson G, Lampi E. Antibiotic prescription: knowledge among physicians and nurses in western Sweden. Health Policy. 2023;130(104733):104733. doi:10.1016/j.healthpol.2023.104733
41. Ertuğrul B, Özden D. Nurses’ knowledge and attitudes regarding physical restraint in Turkish intensive care units. Nurs Crit Care. 2021;26(4):253–261. doi:10.1111/nicc.12541
42. Shah HS, Bohlen J. Implicit Bias. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC; 2025.
43. Świder K, Baska A, Babicki M, Mastalerz-Migas A, Kłoda K. Weight stigma and fat phobia in Poland - attitudes towards people living with obesity and the level of knowledge about obesity among the social media internet respondents and medical professionals. Front Nutr. 2023;10:1287783.
44. Elmaleh-Sachs A, Schwartz JL, Bramante CT, Nicklas JM, Gudzune KA, Jay M. Obesity management in adults: a review. JAMA. 2023;330(20):2000–2015. doi:10.1001/jama.2023.19897
45. Kantowski T, Schulze Zur Wiesch C, Aberle J, Lautenbach A. Obesity management: sex-specific considerations. Arch Gynecol Obstet. 2024;309(5):1745–1752.
46. Lingvay I, Cohen RV, Roux CWL, Sumithran P. Obesity in adults. Lancet. 2024;404(10456):972–987. doi:10.1016/S0140-6736(24)01210-8
47. Roomy MA, Hussain K, Behbehani HM, et al. Therapeutic advances in obesity management: an overview of the therapeutic interventions. Front Endocrinol. 2024;15(1364503). doi:10.3389/fendo.2024.1364503
48. Alisi M. Obesity among children and adolescents in Qatar: protocol for a scoping review. BMJ Open. 2022;12(2):e057427. doi:10.1136/bmjopen-2021-057427
49. Kepper MM, Walsh-Bailey C, Brownson RC, et al. Development of a health information technology tool for behavior change to address obesity and prevent chronic disease among adolescents: designing for dissemination and sustainment using the ORBIT model. Front Digit Health. 2021;3:648777.
50. Amin MR, Pednekar DD, Azgomi HF, van Wietmarschen H, Aschbacher K, Faghih RT. Sparse system identification of leptin dynamics in women with obesity. Front Endocrinol. 2022;13:769951. doi:10.3389/fendo.2022.769951
51. Aragón-Martín R, Gómez-Sánchez MDM, Martínez-Nieto JM, et al. Independent and combined association of lifestyle behaviours and physical fitness with body weight status in schoolchildren. Nutrients. 2022;14(6). doi:10.3390/nu14061208
52. Cohen R, Shikora S. Fighting weight bias and obesity stigma: a call for action. Obes Surg. 2020;30(5):1623–1624.
53. Parshakov P, Naidenova I, Assanskiy A, Nesseler C. Obesity and individual performance: the case of eSports. Int J Obesity. 2022;46(8):1518–1526. doi:10.1038/s41366-022-01142-y
54. Shah HS, Bohlen J. Implicit Bias. In: StatPearls. Treasure Island (FL) ineligible companies: StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC; 2024. Disclosure: Julie Bohlen declares no relevant financial relationships with ineligible companies.
55. Holman H, Dey S, Drobish I, et al. Obesity education in the family medicine clerkship: a US and Canadian survey of clerkship directors’ beliefs, barriers, and curriculum content. BMC med edu. 2019;19(1):169. doi:10.1186/s12909-019-1614-y
56. Salvador J, Vilarrasa N, Poyato F, Rubio M. Perceptions, Attitudes, and Barriers to Obesity Management in Spain: results from the Spanish Cohort of the International ACTION-IO Observation Study. J Clin Med. 2020;9(9):2834.
57. Hitch D, Pazsa F, Qvist A. Clinical leadership and management perceptions of inpatients with obesity: an interpretative phenomenological analysis. Int J Environ Res Public Health. 2020;17(21):8122.
58. Pakpour AH, Tsai MC, Lin YC, et al. Psychometric properties and measurement invariance of the weight self-stigma questionnaire and weight bias internalization scale in children and adolescents. Int J Clin Health Psychol. 2019;19(2):150–159. doi:10.1016/j.ijchp.2019.03.001
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Awareness, Attitude, and Beliefs Regarding Organ Donation Among the General Public in Saudi Arabia
Alghamdi A, Alsaleh AA, Alfozan OA, Qutob R, Alaryni A, Bukhari A, Hakami OA, Alhusaini BA, Alzmamy SA, Alhudayris FS, Alshuaibi LK, Alenazi AM, Alhosaini LS, Aljarba NK, AlShammari SH
International Journal of General Medicine 2023, 16:4973-4989
Published Date: 31 October 2023
Nursing Students’ Knowledge, Attitude, and Practice Regarding Disaster Preparedness: A Cross-Sectional Study
Mohamed NA, Abdel-Aziz HR, Elsehrawy MG
Risk Management and Healthcare Policy 2023, 16:2427-2437
Published Date: 14 November 2023
Knowledge, Attitudes and Practices Towards Psoriasis Among Patients and Their Family Members
Zhang X, Du H, Liu X, Liu L, Zhang T
Clinical, Cosmetic and Investigational Dermatology 2024, 17:769-782
Published Date: 3 April 2024
Knowledge, Attitudes and Practices Toward Physical Literacy Among the College Students During COVID-19 School Closure
Ma C, Yue M, Zhu X
Journal of Multidisciplinary Healthcare 2024, 17:1629-1640
Published Date: 15 April 2024
Knowledge, Attitude and Practice of Radiologists Regarding Artificial Intelligence in Medical Imaging
Huang W, Li Y, Bao Z, Ye J, Xia W, Lv Y, Lu J, Wang C, Zhu X
Journal of Multidisciplinary Healthcare 2024, 17:3109-3119
Published Date: 4 July 2024


