Back to Journals » Journal of Pain Research » Volume 18
Manipulative Treatment of Myofascial Pain Syndrome: A Network Meta-Analysis Based on Randomized Controlled Trials
Authors Chen J , Yin L, Hu Q, Liu S, Zeng L
Received 24 January 2025
Accepted for publication 1 April 2025
Published 10 April 2025 Volume 2025:18 Pages 1923—1933
DOI https://doi.org/10.2147/JPR.S517869
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor King Hei Stanley Lam
Jing Chen,1,2,* Linyu Yin,1,2,* Qing Hu,1,2 Songtao Liu,1,2 Lirong Zeng3
1Department of Rehabilitation Medicine, The Affiliated Hospital of Xiangnan University, Chenzhou, Hunan, 423000, People’s Republic of China; 2College of Medical Imaging Laboratory and Rehabilitation, Xiangnan University, Chenzhou, Hunan, 423000, People’s Republic of China; 3Department of Rehabilitation Medicine, The First People’s Hospital of Chenzhou (The First Affiliated Hospital of Xiangnan University), Chenzhou, Hunan, 423000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Songtao Liu, Department of Rehabilitation Medicine, The Affiliated Hospital of Xiangnan University, No. 31,West Renmin Road, BeiHu District, Chenzhou, Hunan Province, 42300, People’s Republic of China, Tel +8613875515541, Fax +862823271, Email [email protected] Lirong Zeng, Department of Rehabilitation Medicine, The First People’s Hospital of Chenzhou (The First Affiliated Hospital of Xiangnan University), No. 102 Luojiajing, Beihu District, Chenzhou, Hunan Province, 42300, People’s Republic of China, Tel +8618075530126, Fax +862363990, Email [email protected]
Objective: Myofascial pain syndrome (MPS) is a common condition. Manual therapy is preferred over other invasive treatments due to its noninvasiveness and safety, but evidence for its effectiveness is lacking. We here conducted a comprehensive search of randomized controlled trial studies related to manipulative therapy for MPS and conducted a network meta-analysis to provide a basis for clinical applications and experimental studies.
Methods: Reports on randomized controlled trials of noninvasive therapy for MPS deposited in the China National Knowledge Infrastructure database, Chinese Science Citation Database(CSCD), Chinese Citation Database(CCD), Chinese Biomedical Database, PubMed, Embase, Cochrane Library, and Web of Science from their respective inception dates until November 10, 2024, were retrieved. A network meta-analysis was performed using Rv4.2.0 software.
Results: Fourteen studies involving 588 patients overall were included. The interventions included pain point compression, massage, and ischemic compression. Visual analogue scale scores were reported in 12 studies and the pressure pain threshold was reported in five studies. The outcomes demonstrated that manipulation had a notable effect, although not statistically significant, as compared with conventional treatment and placebo. Overall, the effect of pain-point compression was favorable. The results were stable, with no significant publication bias.
Conclusion: Manipulation was an effective treatment for MPS, but the effects were not statistically significant, based on the findings of this study. Owing to issues such as uneven methodological quality and the small sample size of the included studies, further high-quality multicenter, large-sample, randomized double-blind controlled trials are required to verify the reliability of this conclusion.
Keywords: comparative effectiveness research, musculoskeletal manipulations, myofascial pain syndromes, network meta-analysis, systematic review
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Chen has been published for this article.
Myofascial pain syndrome (MPS) is a common disorder affecting the shoulder, neck, and lumbar regions.1 It is an acute/chronic non-specific neuromuscular dysfunction that mainly manifests as muscle pain, muscle loss, and decreased muscle activity, among other symptoms.2 The lifetime prevalence rate of MPS in the general population is as high as 85%.3 MPS accounts for approximately 30–85% of skeletal muscle disorder cases. Modern lifestyle characteristics, such as increased working hours, reduced exercise, abnormal posture, and prolonged sitting, are considered high-risk factors for MPS.4 MPS has also become a significant barrier restricting work attendance and quality of life, imposing a considerable economic burden on patients and their families.
 |
Figure 1 Literature screening process. |
At present, the main treatment modalities for MPS include manual acupuncture and drug injection therapies, which have favorable effects. Nevertheless, some patients are reluctant to undergo these treatments, and the treatments also have certain risks. If not performed carefully, infections, needle-related fainting, visceral injuries, broken needles, and other adverse consequences may occur.5
Owing to the noninvasive nature and safety of manual therapy, it may be preferred over other invasive treatment approaches. Manipulative therapies, such as point compression, massage, and other therapeutic techniques, are simple and effective treatments that can be performed by therapists and are widely used in physical therapy for MPS. However, clinical research evidence regarding the manipulative treatment of MPS has been insufficient to date. The quality of evidence in some such studies has not been high, and few systematic reviews on the application of manual treatment of MPS are available.
Therefore, to explore the clinical evidence for the manipulative treatment of MPS further, we sought to synthesize the available data from evidence-based medicine. We conducted a comprehensive literature search for randomized controlled trials related to the manipulative treatment of MPS and performed a network meta-analysis to provide a reference basis for clinical applications and experimental studies related to manipulative treatment.
Methods
Study Registration
This study has been registered with PROSPERO: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024616488
Eligibility Criteria
Studies were included based on the PICOS principles. In terms of population, we included studies on patients with MPS, without restriction on sex, age, race, and nationality. As interventions, we included studies that used manipulative treatment, including massage, chiropractic care, osteopathic manipulation, mobilization, myofascial release, tuina, shiatsu, and point compression. For comparison, the included studies used conventional treatments, including the spray-and-stretch technique, thermomagnetic therapy, heat therapy, ultrasound therapy, and placebo. As outcomes, we used the visual analogue scale (VAS) score for pain.6 The VAS scale is commonly used for pain assessment. It indicates pain through a 10-cm straight line, where 0 represents “no pain at all” and 10 represents “extreme pain.” The patients were asked to mark on the line how much pain they felt before and after treatment with a higher score indicating more intense pain. Not only does it work for a variety of pain types and patient groups, but it also has a high level of accuracy, allowing it to reflect the experience of patients more accurately. The pressure-pain threshold (PPT) was also used as an outcome.7 The higher the pain threshold, the lower is the patient’s sensitivity to painful stimuli. In terms of study design, we limited the included studies to randomized controlled trials.
Exclusion Criteria
We excluded studies for which the required outcome indicators were not included in the literature or where the data on the outcome indicators were incomplete, or if serious defects were present in the research trial design. We also excluded animal experiments, reviews, case reports, conference papers, and control groups that received active recovery or other treatments that affected the recovery process.
Data Sources and Search Strategy
Reports on randomized controlled trials of tuina therapy for DOMS that were deposited in the China National Knowledge Infrastructure database, Chinese Science Citation Database, Chinese Citation Database(CCD), Chinese Biomedical Database, PubMed, Embase, Cochrane Library, and Web of Science from their inception dates through November 25, 2024 were identified. The languages in which we are conducting the search are limited to English and Chinese.The search strategy is presented in the Appendix (Supplementary Table 1 Retrieval strategy (PubMed)).
Study Selection
Two researchers independently searched and screened the literature and extracted data. First, the literature was screened based on the title and abstract. For reports that were identified as potentially eligible, the full text was read to verify eligibility for inclusion in the meta-analysis. In cases of disagreement, a third researcher adjudicated.
Data Extraction
Two researchers designed data extraction tables according to the information required and used these to extract the relevant data independently. The extracted data included the following. First, basic information included the first author, publication date, publication country, treatment modality, treatment time, and outcome index. Second, demographic characteristic of the patients included the: sample size, age, sex. Third, methodological information included the randomization method, assignment hiding scheme, blinding method, etc. When the information extracted by the two researchers was inconsistent, consensus was reached by discussion.
Risk-of-Bias in Studies
Two researchers used the Cochrane randomized Controlled Trial Bias Risk Assessment tool8 to assess the risk-of-bias. The assessment tool included the following seven items: generation of random sequences, assignment hiding, blinding of participants and intervention providers, blinding of outcome evaluators, incomplete outcome data, selective outcome reporting, and other sources of bias, each of which assessed the outcome as having low, high, or unclear risk-of-bias.
Synthesis Methods
A Bayesian random-effects model was used to compare the effects between interventions and the effectiveness of various interventions. The Markov chain Monte Carlo method was used for modeling; four Markov chains were run simultaneously, with 20000 annealing times. Modeling was completed after 50000 simulation iterations. The Deviation Information Standard (DIC) was used to compare the model fit and global consistency, and the node-splitting method was used to analyze local consistency if a closed-loop network was present. In addition, the interventions were ranked based on surface under the cumulative ranking (SUCRA), and league tables were generated to compare the differences in effects across the interventions. Subgroup and sensitivity analyses were also performed. When the number of studies included in the outcome measure was ≥10, a funnel plot was used for intuitive interpretation of publication bias. The analysis was completed using Stata15 (Stata Corp., College Station, TX, USA) and R v.4.2.2 (https://www.r-project.org/).
Results
Study Selection
The literature search identified 983 studies. EndNoteX9.1 (https://researchsoftware.com/endnote-x91-for-windows-and-mac) was used to process the literature. A total of 496 duplicate articles were excluded. Additionally, 463 articles were excluded after reading the title and abstract, and 10 articles were excluded after reading the full text. Finally, 14 randomized controlled trials were included in analysis. Figure 1 shows a flowchart of the screening process.
Study Characteristics
This review included 14 studies,9–21 with 588 patients overall: 295 patients in the experimental group, and 293 patients in the control group. The authors were from China, the Netherlands, Turkey, Iran, and Saudi Arabia. The interventions included pain-point compression, massage, and ischemic compression. The VAS score for pain was reported in 12 studies and the PPT was reported in five studies. Table 1 presents basic information on the included studies.
 |
Table 1 Basic Information of the Included Studies |
Risk-of-Bias in Studies
Regarding randomization methods, 11 studies9,10,12,14–17,19–21 used a computer-based random number generator. One study18 used an incorrect method of randomization, and two studies11,13 made no mention of randomization. Two studies15,16 used envelopes to conceal assignment. In terms of blinding, seven studies9,10,12,14,16,19,21 used single blinding, while two studies15,17 used double blinding. In some studies, patients withdrew from the study; however, the sample sizes were small. No selective reporting or other publication biases were observed in any study. Figures 2 and 3 shows the results of the risk-of-bias analysis for the included studies.
 |
Figure 2 Risk-of-bias graph. |
 |
Figure 3 Risk-of-bias summary. |
Meta Analysis
VAS Score
Twelve studies using three techniques (pain-point compression, massage, and ischemic compression) reported the VAS score for pain. Closed loops are shown in the graph. The inconsistency test results showed that, at P > 0.05, the surface network was consistent, and the consistency model was used for analysis (see Figure 4). Heterogeneity test results showed an I2 value of 11%, indicating little heterogeneity. The effect of manipulative treatment was good as compared to that of conventional treatment and placebo, but the difference in the VAS score for pain was not statistically significant (Figures 5, 6, Appendix (Supplementary Table 2 League table(VAS))). The treatments with the top-three SUCRA values were Pain-point compression (0.73), ischemic compression (0.69), and massage (0.28) (Table 2).
 |
Figure 4 Mesh correlation graph (visual analogue scale score for pain) among different techniques. |
 |
Figure 5 Forest plot of the effectiveness of different techniques compared to conventional treatment (visual analogue scale score for pain). |
 |
Figure 6 Forest plot of the effectiveness of different techniques compared with placebo (visual analogue scale score for pain). |
PPT
Five studies, including two techniques (pain-point compression and ischemic compression) reported on the PPT. The absence of closed loops was analyzed using a conformance model (Figure 7). The heterogeneity test results showed an I2 value of 3%, indicating little heterogeneity. The effect of manipulation treatment on the PPT was good as compared to that of conventional treatment and placebo, but the results were not statistically significant (Figures 8, 9, Appendix (Supplementary Table 3 League table(PPT))). The top-three SUCRA values were obtained for ischemic compression (0.65), conventional treatment (0.61), and pain-point compression (0.60) (Table 2).
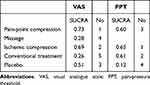 |
Table 2 SUCRA Scores Obtained for Outcome Indicators in the Included Studies |
 |
Figure 7 Network association diagram of different techniques (pain-pressure threshold). |
 |
Figure 8 Forest graph of the effectiveness of different techniques compared to conventional treatments (pain-pressure threshold). |
 |
Figures 9 Forest plot of the effectiveness of different techniques compared with placebo (pain-pressure threshold). |
Publication Bias Analysis
The Egger test of results obtained at 24 h, 48 h, and 72 h showed a small possibility of publication bias (P = 0.07).
Discussion
We conducted a network meta-analysis to assess the effectiveness of different manipulations for MPS treatment. Fourteen studies encompassing three manipulation therapies (pain-point compression, massage, and ischemic compression) were included. The VAS and PPT were used to evaluate the degree of objective pain perception. These two approaches are the most significant means of evaluating the efficacy of addressing pain symptoms in patients with MPS. The results indicated that manipulation had an effect, although it was not statistically significant as compared to conventional treatment or placebo. Overall, the effect of pain-point compression was favorable. The results were stable, with no significant publication bias.
Regarding the possible pathological mechanism of MPS, TPC can reduce the degree of contracture and ameliorate the local energy crisis by elongating the contracted muscle segment in the myofascial trigger point (MTrP) region.23 TPC can alleviate pain symptoms by activating the pain gate control system24 and descending pain inhibition system.25 When compression is complete, the rapid influx of blood supplies oxygen and carries away pain-causing substances, reducing the stimulation of nociceptors, and interrupting the abnormal endplate release of excessive acetylcholine. Moraska et al26 provided crucial evidence that TPC improved the local energy crisis in MPS in a 2013 study, in which two subjects were implanted with a set of microdialysis probes at a MTrP site in the trapezius muscle, which recorded biochemical changes in the MTrP before and after TPC treatment. They found that the local blood flow and local glucose concentration in the MTrP increased significantly after TPC treatment, signifying that the affected local muscle segments obtained sufficient energy supply to restore the normal metabolic state. In addition, TPC treatment restored the elasticity and malleability of the local muscles involved in the MTrP. In 2018, Kisilewicz et al27 utilized the MyotonPRO muscle elasticity test instrument to analyze the efficacy of TPC for the treatment of patients with MPS and superior trapezius bundles. They discovered that the overall stiffness of the trapezius muscle was significantly reduced in patients after treatment, supporting the view that TPC alleviates local muscle spasms.
Although we found no statistically significant difference with manipulation therapy, this did not imply that the results were clinically insignificant. Some studies28–30 suggested that pain-point compression therapy can significantly ameliorate the symptoms of MPS. The reasons for the nonsignificant results in our analysis may include the following: First, the form and standards of techniques were not standardized. For example, although ischemic compression at the MTrP is mechanically designed to relieve contracted soft tissue and promote fluid flow (including tissue fluid and blood) through pressure, the specific surgical methods used differ. International researchers have emphasized precise pressure at the trigger point, and the treatment is mainly through continuous pressure, whereas Chinese researchers treat the trigger point from the perspective of traditional Chinese meridians, and the application of force is not limited to the trigger point. The specific manipulations included shiatsu, finger kneading, and plucking. Second, the intensity parameters of the manipulations were not uniform. Some studies consider the subjective perception of the therapist as the basis for treatment, maintaining pressure when the nodules are touched, and applying pressure when the nodules are softened,31 while others take the pain of the patient as the basis, maintaining pressure when the patient’s main complaint reaches the maximum pain threshold, and exerting pressure when the pain decreases significantly, repeatedly.32 Chao et al33 combined patients’ pain complaints with therapists’ subjective perceptions in their own research. Although the above studies have demonstrated certain therapeutic effects, no literature on specific operational norms are available; thus, effective comparisons between different types of techniques in terms of efficacy cannot be made. Second, it may be related to the rigor of the study itself (including the inclusion of subjects, whether a blinding method was used, specific treatment methods, and measurement of indicators) and sample size. Therefore, the quality and sample size of the relevant literature need to be evaluated. We searched the Chinese clinical trial registration platform and found that many ongoing clinical studies on using manual therapy for MPS (for example, ChiCTR2300075495, ChiCTR2000030881, and ChiCTR2200058541), indicating that MPS using manual therapy holds great research value.
No previous network meta-analysis of MPS treated with different manipulations to provide evidence for clinical use has been published to date. However, this study had some limitations. Only 14 articles were included, which is a relatively small number. The outcome indicators included in each study differed, and the scale types used were difficult to standardize. Only the relatively common VAS scores and PPT measurement values could be selected for meta-analysis, whereas other parameters were difficult to include in a pooled analysis. The literature included in this study had different degrees of risk-of-bias. Moreover, this study only included Chinese and English literature, and thus a more comprehensive search and screening of existing studies could not be conducted. The results of this study were not limited by statistical significance. This is due to a number of reasons, which we have analyzed. In the future, we will further pay attention to the research updates in related fields, timely incorporate the latest research data, and update our results.
Conclusion
Based on the findings of this study, manipulation therapy was an effective treatment for MPS, but not statistically significantly different from conventional therapy or placebo, owing to issues such as inconsistent methodological quality and the small sample size of the included studies. Further high-quality multicenter, large-sample, randomized double-blind controlled trials are required in future to verify the reliability of this conclusion.
Abbreviations
MPS, myofascial pain syndrome; MTrP, myofascial trigger point; PPT, pain-pressure threshold; TPC, trigger point compression; VAS, visual analogue scale.
Data Sharing Statement
Data are available from the corresponding author (Lirong Zeng) upon request.
Acknowledgments
We thank the researchers and the study participants for their contributions.We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This work was supported by the Hunan Provincial Clinical Medical Technology demonstration base of chronic musculoskeletal pain rehabilitation (grant number:2023SK4074),the Hunan Provincial Natural Science Foundation of China (grant number:2024JJ7536),the Chronic musculoskeletal pain rehabilitation technology research and development center of Chenzhou City (grant number:2021-02-31).
Disclosure
The authors declare no conflicts of interest regarding the publication of this paper. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Shah JP, Thaker N, Heimur J, et al. Myofascial trigger points then and now: a historical and scientific perspective. PMR. 2015;7(7):746–761. doi:10.1016/j.pmrj.2015.01.024
2. Gerwin RD. Myofascial Trigger point pain syndromes. Semin Neurol. 2016;36(5):469–473. doi:10.1055/s-0036-1586262
3. Fleckenstein J, Zaps D, Ruger LJ, et al. Discrepancy Between Prevalence and Perceived Effectiveness of Treatment Methods in Myofascial Pain Syndrome: Results Ofa Cross-Sectional, Nationwide Survey. Vol. 11. BMC Musculoskelet Disord; 2010:32
4. Treaster D, Marras WS, Burr D, et al. Myofascial trigger point development from visual and postural stressors during computer. J Electromyogr Kinesiol. 2006;16(2):115–124. doi:10.1016/j.jelekin.2005.06.016
5. Yingye LIANG, Hongliang TANG, Xiongjiang W, et al. Myofascial pain syndrome of traditional Chinese medicine external treatment intervention study of. J Liaoning Trad Chin Med. 2018;(10):2229–2231. doi:10.13192/j.iSSN.1000-1719.2018.10.067
6. Faiz KW. VAS--visuell analog skala [VAS--visual analog scale]. Tidsskr nor Laegeforen. 2014;134(3):323. doi:10.4045/tidsskr.13.1145
7. Walton DM, Macdermid JC, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644–650. doi:10.2519/jospt.2011.3666
8. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928. doi:10.1136/bmj.d5928
9. Bron C, de Gast A, Dommerholt J, Stegenga B, Wensing M, Oostendorp RA. Treatment of myofascial trigger points in patients with chronic shoulder pain: a randomized, controlled trial. BMC Med. 2011;9(1:8. doi:10.1186/1741-7015-9-8.
10. Weichang H, Shan-Shan L, Zhi-Yong F, et al. A clinical study of 30 cases of low back myofascia pain syndrome treated with “trigger point” manipulation. Jiangsu J Trad Chin Med. 2013;45(08):47–49.
11. Yagci N, Uygur F, Bek N. Comparison of connective tissue massage and spray-and-stretch technique in the treatment of chronic cervical myofascial pain syndrome. Pain Clinic. 2004;16(4):469–474. doi:10.1163/1568569042664503
12. Zhixin Z, Qian G, Shudan Analysis of Therapeutic Efficacy of Ischemic Compression Technique in Treating Cervical and Shoulder Muscle-Tendon Fascia Pain Syndrome. J Chin People’s Liber Army Med College. 2015;36(9):908–910.
13. Chan YC, Wang TJ, Chang CC, et al. Short-term effects of self-massage combined with home exercise on pain, daily activity, and autonomic function in patients with myofascial pain dysfunction syndrome. J Phys Ther Sci. 2015;27(1):217–221. doi:10.1589/jps.27.217
14. Kim M, Lee M, Kim Y, Oh S, Lee D, Yoon B. Myofascial pain syndrome in the elderly and self-exercise: a single-blind, randomized, controlled trial. J Altern Complement Med. 2016;22(3):244–251. doi:10.1089/acm.2015.0205
15. Behrangrad S, Kamali F. Comparison of ischemic compression and lumbopelvic manipulation as trigger point therapy for patellofemoral pain syndrome in young adults: a double-blind randomized clinical trial. J Bodyw Mov Ther. 2017;21(3):554–564. doi:10.1016/j.jBMT.2016.08.007.
16. Jafari M, Bahrpeyma F, Togha M. Effect of ischemic compression for cervicogenic headache and elastic behavior of active trigger point in the sternocleidomastoid muscle using ultrasound imaging. J Bodyw Mov Ther. 2017;21(4):933–939. doi:10.1016/j.jBMT.2017.01.001
17. Moraska AF, Schmiege SJ, Mann JD, Butryn N, Krutsch JP. Responsiveness of myofascial trigger points to single and multiple trigger point release massages: a randomized, placebo controlled trial. Am J Phys Med Rehabil. 2017;96(9):639–645. doi:10.1097/PHM.0000000000000728
18. Luo G. Therapeutic effect of ischemic compressions on cervical and shoulder myofascial pain syndrome. Diet Care. 2017;4(26):54–55. doi:10.3969/j.iSSN.2095-8439.2017.26.064
19. Kashyap R, Iqbal A, Alghadir AH. Controlled intervention to compare the efficacies of manual pressure release and the muscle energy technique for treating mechanical neck pain due to upper trapezius trigger point. J Pain Res. 2018;11:3151–3160. doi:10.2147/JPR.S172711
20. Xinjian L, Nanjun C, Jianyu Y, et al. Compression (ischemic clinical observation on treatment of neck and shoulder myofascial pain syndrome. J Rehab. 2020;30(02):140–144. doi:10.3724/SP.j.1329.2020.02011
21. Hou X, Xu JH, Wang N, et al. Therapeutic effect of vaginal trigger point manipulation combined with bioelectric stimulation on female pelvic floor myofascial pain syndrome. J Mode Integra Chin Western Med. 2019;32(20):2803–2808+2884.
22. Zheng BX, Deng CY, Peng XX. Observation on the Therapeutic Efficacy of Myofascial Finger Technique Relaxation Combined with Neuromuscular Electrical Stimulation in Treating Pelvic Floor Myofascial Pain Syndrome. Practical Journal of Hospital Clinical Practice. 2024; 21(2):94–97.
23. BCL S, Kong ISY, Lee RKL, et al. The effect of Ai Chi aquatic therapy on individuals with knee osteoarthritis: a pilot study. J Phys Ther Sci. 2017;29(5):884–890. doi:10.1589/jpts.29.884
24. Regnaux JP, Lefevre-Colau MM, Trinquart L, et al. High-intensity versus low-intensity physical activity or exercise in people with Hip or knee osteoarthritis. Cochrane Database Syst Rev. 2015;2015(10):CD010203. doi:10.1002/14651858.CD010203.pub2
25. Kluzek S, Sanchez-Santos MT, Leyland KM, et al. Painful knee but not hand osteoarthritis is an independent predictor of mortality over 23 years follow-up of a population-based cohort of middle-aged women. Ann Rheum Dis. 2016;75(10):1749–1756. doi:10.1136/annrheumdis-2015-208056
26. Becker BE. Aquatic therapy: scientific foundations and clinical rehabilitation applications. PMR. 2009;1(9):859–872. (). doi:10.1016/j.pmrj.2009.05.017
27. Kutzner I, Richter A, Gordt K, et al. Does aquatic exercise reduce hip and knee joint loading? In vivo load measurements with instrumented implants. PLoS One. 2017;12(3):e0171972. doi:10.1371/journal.pone.0171972
28. Mckenney K, Elder AS, Elder C, et al. Myofascial release as a treatment for orthopaedic conditions: a systematic review. J Athl “Train”. 2013;13(4):522–527. doi:10.4085/1062-6050-48.3.17
29. Saxena A, Chansoria M, Tomar G, et al. Myofascial pain syndrome: an overview. J Pain Palliat Care Pharmacother. 2015;29(1):16–21. doi:10.3109/15360288.2014.997853
30. Anle X, Qiangmin H, Lijuan J, et al. Research status of ischemic compression in the treatment of myofascial pain syndrome. Massage Rehab Med. 2018;9(16):89–93.
31. Bodes-Pardo G, Pecos-Martin D, Gallego-Izquierdo T, et al. Manual treatment for cervicogenic headache and active trigger point in the sternocleidomastoid muscle: a pilot randomized clinical trial. J Manipulative Physiol Ther. 2013;36(7):403–411. doi:10.1016/j.jmpt.2013.05.022
32. Nambi GS, Sharma R, Inbasekaran D, et al. Difference in effect between ischemic compression and muscle energy technique on upper trepezius myofascial trigger points: comparative study. Int Health Alli Sci. 2013;2(1):17–22. doi:10.4103/2278-344X.110570
33. Chao YW, Lin JJ, Yang JL, et al. Kinesio taping and manual pressure release: short-term effects in subjects with myofasical trigger point. J Hand Ther. 2015;29(1):23–29. doi:10.1016/j.jht.2015.10.003
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Psychological Interventions on Abstinence in Patients with Alcohol Use Disorder: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials
Zhang P, Zhan J, Wang S, Tang Y, Chen H, Wang Y, Wei X, Wen H, Pan T, Chen Z, Tang C, Xu N, Lu L
Neuropsychiatric Disease and Treatment 2022, 18:1815-1830
Published Date: 23 August 2022
Effect of Exercise Interventions on Health-Related Quality of Life in Patients with Fibromyalgia Syndrome: A Systematic Review and Network Meta-Analysis
Zhang KD, Wang LY, Zhang ZH, Zhang DX, Lin XW, Meng T, Qi F
Journal of Pain Research 2022, 15:3639-3656
Published Date: 22 November 2022
Different Intensities of Evening Exercise on Sleep in Healthy Adults: A Systematic Review and Network Meta-Analysis
Yue T, Liu X, Gao Q, Wang Y
Nature and Science of Sleep 2022, 14:2157-2177
Published Date: 14 December 2022
Nonpharmacological Interventions for Management of the Pain-Fatigue-Sleep Disturbance Symptom Cluster in Breast Cancer Patients: A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials
He CC, Lin DM, Liu HZ, Wang FF, Guo XF, Zhang XB, Ai YQ, Meng LM
Journal of Pain Research 2023, 16:2713-2728
Published Date: 7 August 2023
Efficacy of Acupuncture-Related Therapy for Migraine: A Systematic Review and Network Meta-Analysis
Liu Y, Wang Y, Mi C, Wang Z, Han Y, Qi X, Ding X
Journal of Pain Research 2024, 17:1107-1132
Published Date: 15 March 2024

