Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 20
Influence of Urinary Incontinence Related Factors on Health-Related Quality of Life in Patients with Chronic Obstructive Pulmonary Disease: A Cross-Sectional Study
Authors Alrajhi NS, Albarrati A, Aldhahi MI , Gwada RF
Received 3 January 2025
Accepted for publication 3 June 2025
Published 12 June 2025 Volume 2025:20 Pages 1881—1892
DOI https://doi.org/10.2147/COPD.S515494
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Nada Saleh Alrajhi,1 Ali Albarrati,2 Monira I Aldhahi,3 Rehab FM Gwada2,4
1Physical Therapy Department, Prince Sultan Military Medical City, Riyadh, Saudi Arabia; 2Rehabilitation Health Sciences Department, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 3Department of Rehabilitation Sciences, College of Health and Rehabilitation Sciences, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia; 4Physical Therapy Department, National Heart Institute, Giza, Egypt
Correspondence: Monira I Aldhahi, Department of Rehabilitation Sciences, College of Health and Rehabilitation Sciences, Princess Nourah bint Abdulrahman University, P.O. Box 84428, Riyadh, 11671, Saudi Arabia, Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) is a progressive respiratory condition marked by airflow limitation and symptoms like chronic cough, breathlessness, and chest tightness. These factors, along with exacerbations and polypharmacy, may predispose COPD patients to urinary incontinence (UI). Unique challenges such as increased intra-abdominal pressure, pelvic floor weakness, and comorbidities may worsen UI and impair health-related quality of life (HRQoL). This study aimed to identify factors associated with UI severity in COPD patients and to examine its impact on HRQoL.
Methods: This cross-sectional study included 101 participants diagnosed with COPD who were reported to have UI. Participants completed the following questionnaires: the health status and UI severity were recorded using the COPD Assessment Test (CAT), International Consultation on Incontinence Questionnaire- Urinary Incontinence – short form (ICIQ-UI short form), and Incontinence Impact Questionnaire – short form (IIQ-7).
Results: UI severity was correlated with age, BMI, smoking, comorbidities, medications, chest tightness, and breathlessness. Severe UI predictors included age (OR=1.07), BMI (OR=1.09), and number of medications (OR=5.04), whereas breathlessness predicted moderate (OR=1.72) and severe UI (OR=1.87). Among COPD patients, 82.2% reported a mild impact of UI on HRQoL, and 6.9% reported a severe impact. Notably, among those experiencing moderate-to-severe HRQoL impairment, 63.6% had severe UI.
Conclusion: This study highlights urinary incontinence (UI) as a prevalent and impactful comorbidity in individuals with COPD, significantly affecting their HRQoL. UI severity was associated with clinical factors such as older age, higher body mass index (BMI), greater medication burden, and breathlessness. Notably, greater UI severity corresponded to more substantial impairments in HRQoL, with severe cases reporting greater negative effects on daily functioning. These findings underscore the importance of routine screening for UI in COPD patients and the implementation of targeted continence care strategies to enhance overall quality of life.
Plain Language Summary: This study highlights significant correlations between UI, HRQoL, and factors such as age, BMI, and breathlessness. This study emphasizes the need for routine UI screening in patients with COPD to improve HRQoL through specialized continence care.
Keywords: COPD, disease severity, health-related quality of life, urinary incontinence
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic progressive pulmonary disease that also exhibits extrapulmonary manifestations such as urinary incontinence (UI).1 Previous research indicates that urinary incontinence (UI) affects approximately 25–40% of women in the general population, with prevalence rising to around 50% among women diagnosed with chronic obstructive pulmonary disease (COPD).2 Consequently, UI represents a significant clinical concern for COPD patients due to its elevated prevalence and more pronounced impact compared to the general population. UI presents a dual challenge, affecting individuals both physically and socially, limiting daily activities, and significantly influencing health-related quality of life (HRQoL).3,4 Despite its profound implications, the extensive body of COPD literature often overlooks the factors that could be related to UI and its effect on HRQoL. Instead, the focus has primarily been on COPD itself and its substantial effects on daily life, including a notable reduction in HRQoL.5,6 This oversight highlights an evident gap in current research, emphasizing the need to explore interactions between COPD-specific factors, socio-demographic characteristics, and UI severity, and their collective impact on HRQoL. Addressing this gap will enable more informed clinical practice and contribute to improved management strategies, enhancing the overall well-being of individuals affected by both COPD and UI.
In patients with COPD, the etiology of UI in patients with COPD remains a subject of ongoing investigation. It is evident that numerous contributing factors play a role in the severity of the UI. These factors encompass a wide spectrum ranging from anatomical and mechanical factors to pathophysiological and pharmacological influences.1 It has been reported that the frequent coughing associated with COPD causes an increased intra-abdominal pressure. This increased pressure exerts mechanical forces on pelvic tissues, eventually resulting in connective tissue deformation and stress UI.7–9 Additionally, respiratory distress frequently encountered in COPD may further impair neural control mechanisms of micturition, heightening the risk of developing UI, particularly in advanced disease stages.1,10
Furthermore, the coexistence of multiple comorbidities and polypharmacy in patients with COPD plays a significant role in exacerbating the risk of UI.11,12 Anticholinergic therapy for COPD may lead to urinary discomfort; however, it is unlikely to be a direct cause of urinary incontinence.13 Previous studies on UI have predominantly focused on women, often neglecting a thorough evaluation of both respiratory and non-respiratory risk factors.1,3 In addition, there has been a paucity of studies examining the effects of UI on HRQoL and identifying predictive factors across sex in COPD patients, with a notable absence of such studies in regions such as the Middle East, including Saudi Arabia.1,14 Given the considerable prevalence of UI and its pronounced impact on QoL, there remains a critical gap in the understanding of UI in the context of COPD. This study aimed to identify factors associated with UI severity among individuals with COPD and to examine the relationship between UI severity and its impact on HRQoL in this specific population.
Materials and Methods
Study Design and Participants
This cross-sectional study involved a convenience sample of patients diagnosed with COPD and exhibiting urinary incontinence (UI). All participants presented with UI symptoms, as evidenced by scores of 3 or higher on the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF). COPD diagnosis was medically confirmed with spirometry, categorizing patients into stages I–IV according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, characterized by a FEV1/FVC ratio of less than 70%.15 Study encompassing both sexes and individuals aged 45 years and older. Exclusion criteria included pregnancy; other chronic lung diseases such as cystic fibrosis and asthma; and any medical, surgical, or rehabilitative interventions for UI conducted within the prior six months. The participants were recruited from various pulmonary hospital departments in Saudi Arabia. The sample size was calculated using G*Power 3.1.9.4 software. A medium effect size (0.30 was used. Assuming that the α error probability was 0.05, a power of 80% was considered. The acceptable sample size for this study was estimated as 84. Considering the possible missing data, the sample size was increased to 101 participants.
This study was approved by the Institutional Review Board of King Saud University (Ref. No.20/0288/IRB) and was conducted from September 2020 to February 2021, in accordance with the Declaration of Helsinki guidelines. All participants were informed of the study and provided their consent by signing a consent form. Data were collected through interviews. All participants were interviewed by the same interviewer to ensure consistency in the data-collection process.
Demographic and Clinical Data
The following demographic data were collected: sex, age, weight, height, BMI (kg/m2), marital status, education level, place of residence, and smoking history. For the specific categorization of body mass index (BMI), participants were stratified into distinct groups, including individuals characterized as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (>30 kg/m2).16 Information about the following medical-related factors was collected: symptoms of an overactive bladder, pelvic disorder as prostate/prolapse history, and pelvic procedures or operations such as vaginal/prolapse repair, hysterectomy, and/or prostatectomy. Comorbidities, including hypertension, cardiac conditions, neurological disorders, diabetes, back pain, and arthritis, were recorded for each participant.1,17 The participants’ medications were recorded using an electronic file. The total number of comorbidities and medications taken by each participant was recorded.
COPD severity was determined by the recent lung function test within the last three months and retrieved from the system, and recorded according to the GOLD guidelines.18 Participants were interviewed and asked about their respiratory symptoms, including coughing, sputum production, chest tightness, and breathlessness.
Outcome Measures
COPD Assessment Test (CAT)
It is a self-administered questionnaire that is used to evaluate the impact of COPD on health status. It includes eight questions about cough, sputum production, chest tightness, breathlessness while going up a stair/hill, activity limitations at home, confidence in leaving home, sleep, and energy. Each question was answered on a scale ranging from 0 to 5, with the overall score ranging from 0 to 40. Higher scores indicated a worsening impact of COPD on patient health. To complete the questionnaire, the participants were instructed to select one response for each question that best described their current situation.19 The Arabic version of the CAT has been found to be easy to administer, and reliable (ICC= 0.9; p= 0.001).20.
The Incontinence Questionnaire- Urinary Incontinence – Short Form (ICIQ-UI) Questionnaire
This questionnaire was used to assess the severity of UI. It consists of three questions about the frequency of UI, amount of leakage, and overall impact of UI. The score was summed from 0 to 21, and the severity of UI was defined as follows:0, no leak; 1–5, slight leakage; 6–12, moderate leakage; 13–18, severe leakage; and 19–21, serious leakage. In addition, separate items at the end of the questionnaire allowed respondents to report instances of incontinence. The participants were instructed to consider their experiences over the past four weeks when answering the questions. The Arabic version of ICIQ-UI short form is a simple questionnaire that demonstrates excellent reliability and internal consistency (α= 0.97; 95% CI: 0.88–0.98).21
The Incontinence Impact Questionnaire – Short Form (IIQ-7) Questionnaire
This questionnaire was designed to assess the effect of UI on HRQoL. It comprises seven questions that encompass various aspects such as physical activity, travel, social relations, and emotional health. Each item was rated on a three-point scale: zero (indicating no impact), one (suggesting a minor impact), two (indicating a moderate impact), and three (denoting a significant impact).22 The total score, ranging from 0 to 100, provides a quantitative measure of the HRQoL. A score below 50 signifies a mild impact, 50–70 reflects a moderate impact, and a score above 70 indicates a severe impact on HRQoL.23 The Arabic version of the IIQ-7 has been recognized for its ease of use, reliability, and valid questionnaire.24
Data Analysis
Data were analyzed using Statistical Package for Social Sciences (SPSS) version 27 (IBM Corp., Armonk, NY, USA). Data normality was examined prior to analysis. Categorical data are presented as frequency and percentage, and non-normally distributed data are reported as median and interquartile range (IQR) for quantitative variables. Categorical data were compared using the chi-squared test. The correlation coefficient (r) was used to determine the relationships between variables of interest. A multinomial logistic regression model was used to investigate the factors associated with UI severity. Two categories, severe and serious urinary leakage, were merged into severe urinary leakage, and mild urinary leakage was used as the reference category. Statistical significance was set at p-value <0.05.
Results
A total of 480 patients diagnosed with COPD were invited to participate in the study. After the screening process, 379 participants were excluded for various reasons: non-consent to participate, resolution of urinary incontinence (UI) symptoms, presence of communication barriers such as language or hearing disabilities, or the absence of available pulmonary function test results (Figure 1). Consequently, 101 participants met the inclusion criteria and were enrolled in this study. The patients median age 70 years (IQR: 62–78.5) and BMI 30.4 kg/m2 (IQR:26.5–37.8). The majority had moderate COPD (70.2%) and over half were obese (53.5%). Of all the participants, 70.3% had more than two diseases and 63.4% took at least two medications. The other demographic and medical-related factors are shown in Table 1.
 |
Table 1 Baseline Characteristics of the Demographic and Health Status of the of Participant (N=101) |
 |
Figure 1 Flow diagram of the study. |
Urinary Incontinence Severity
Table 2 shows that the patient had a COPD profile and UI characteristics. The UI severity of patients with COPD has been reported to have a median (IQR) of 10 (8–13). Patients with COPD were stratified according to UI severity as follows:12 participants were categorized as slight (11.9%), 59 as moderate (58.4%), 27 as severe (26.7%), and 3 as serious urinary leakage (3%). In terms of urinary incontinence subtypes among participants, urge urinary incontinence was the most commonly reported (85.1%), followed by stress urinary incontinence (63.4%) and mixed urinary incontinence (50.5%).
 |
Table 2 Description of the COPD Profile and UI Characteristic (N=101) |
Factors Associated with UI Severity
There was a correlation between UI severity scores and age (rs =0.26), BMI (rs=0.29), smoking status (rs =0.25), number of relevant comorbidities (rs =0.22), medications (rs =0.27), chest tightness (rs =0.25), and breathlessness (rs =0.26) (all p values < 0.05). There was a correlation between IIQ-7 score and UI severity (rs=0.43; p<0.05) (Table 3).
 |
Table 3 Correlation Between Study Variables and UI Severity |
The association between the categories of UI severity and their impact on HRQoL is shown in Table 4. It has been reported that the majority of patients with COPD 83 (82.2%) reported a mild impact on their HRQoL, while a smaller proportion 7 (6.9) reported a severe impact on their HRQoL. Among the participants who experienced moderate to severe impacts on their HRQoL, 63.6% reported severe impacts based on IIQ-7 scores. The chi-square test showed a significant association between UI severity categories and the impact on HRQoL (p=0.001).
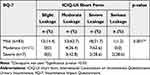 |
Table 4 Assessment of the Relationship Between UI Severity and HRQoL Using IIQ-7 |
Predictive Factors for UI Severity
Multinomial regression analysis identified several significant predictors of urinary incontinence (UI) severity in COPD patients (Table 5). Age was a significant predictor of severe UI (p = 0.04), with an OR of 1.07). BMI was also a significant predictor of severe UI (p = 0.02; OR = 1.09). Additionally, the number of relevant medications was a significant predictor of severe UI (p = 0.03, OR = 5.04). Breathlessness significantly predicted moderate UI (p = 0.01; OR = 1.72) and severe UI (p = 0.01; OR = 1.87). It was observed that for every one-unit increase in age, there was a 1.07 times greater odds ratio of experiencing severe UI (p<0.05). Similarly, for every one-unit increase in BMI, the odds ratio of severe UI increased by 1.09 (p<0.05). Furthermore, participants with COPD who reported breathlessness while going up a stair/hill were twice as likely to have moderate and severe UI, with an odds ratio of 1.87 (p<0.05).
 |
Table 5 Multinomial Regression for Factors Predicting Urinary Incontinence Severity |
Discussion
To the best of our knowledge, this is the first study in Saudi Arabia to investigate the factors associated with UI and their impact on HRQoL in patients with COPD. The current results revealed that UI severity was moderate and negatively impacted HRQoL. In the current study, it was observed that urinary incontinence (UI) had a negative impact on HRQoL, with a positive correlation between the severity of UI and the scores of HRQoL. This result is in agreement with a recent study that reported positive correlations between the IIQ-7 and ICIQ-UI short-form scores in women with UI.25 Several studies have reported similar findings in participants with UI using different outcome measurements.22,26 An early study showed a significant positive correlation between the number of UI episodes and IIQ-7 scores, indicating that an increase in the number of UI episodes would worsen the quality of life of women with UI.22 Another study found a significant positive correlation between the Urinary Distress Inventory-short form and IIQ-7 scores in relation to UI.26 In addition, one study reported that men and women with COPD and UI had poor quality of life compared to those without UI.14
Our results found that there was a significant correlation between UI severity, age, and BMI, which were identified by regression analysis as predictors of UI. This finding aligns with a previous study indicating that UI is affected by age and is considered a risk factor for UI in COPD participants.27 The increase in intra-abdominal pressure and age-related physiological changes in the smooth muscle, altered nerve transmission at the spinal and cortical levels, hypersensitivity of ion channels, and increased afferent nerve activity could be the causes of UI.12
Similar to previous studies, higher BMI was associated with more severe UI symptoms.25,28 Altaweel and Alharbi (2012) identified obesity as a significant predictor of UI.27 The presence of obesity leads to a chronic increase in intra-abdominal pressure, which in turn weakens of pelvic floor muscles and fascia, thereby increasing the likelihood and severity of UI.29,30
In current study, there was no observed correlation between UI severity and sex. This result is consistent with an earlier study that reported no significant relationship between sex and UI.31 However, some studies have reported a higher prevalence of UI in women compared than in men.31,32 This can be attributed to various factors such as urethral length, pelvic floor anatomy, giving birth, and hormonal changes.27,32 Additionally, cultural factors may play a role in the lower UI rate in men and could be cultural factors, as they are often considered embarrassing.32 Another study reported that the prevalence of UI is more common in younger women than in men, but as people get older, this difference decreases.33
The analysis conducted in this study demonstrated a significant positive correlation between breathlessness and UI occurrence. Regression analysis identified breathlessness as a predictor of UI, which aligns with a previous study that also found breathlessness to be a significant factor associated with an increase in the prevalence of UI.9 A possible justification for this is that recurrent dyspnea could cause an imbalance and ischemia in the abdominal and pelvic muscles and impair the control of urination.29,34
In this study, significant positive correlations and associated factors were found between the number of relevant medications and UI severity. This finding is consistent with that of a previous study that indicated a higher risk of UI with the consumption of more than five medications.35 Another study found that participants who used polypharmacy had a higher prevalence of UI.36 To the best of our knowledge, no previous study has investigated the association between UI severity and number of relevant medications in participants with COPD and UI.
This study had some limitations that merit consideration. First, it is essential to acknowledge that the study design is cross-sectional, which precludes the identification of causal relationships between variables. A longitudinal study is required to investigate the causal relationship between UI severity and risk factors for COPD. Second, we acknowledge that some traditionally relevant clinical and demographic variables—such as gender, BMI, and comorbidities—were not included in the final multivariable model, as they did not meet the criteria for statistical inclusion based on initial bivariate analyses. However, their exclusion may limit the ability to fully account for potential confounding or interaction effects. We recommend that future studies with larger and more diverse samples explore the role of these variables more comprehensively to strengthen the generalizability and clinical relevance of the findings. Third, focusing on a specific city could affect generalizability, because the sample may not be representative of the entire country. Fourth, the number of male participants were lower than that of female participants. It is possible that the men were either ashamed or unaware that the condition was treatable.33 However, the prevalence of UI in men is much lower than that in women, at approximately 3% to 11% overall.34 Fifth, physical distancing and quarantine during the COVID-19 pandemic was necessary because the surveys were conducted via phone, and the participants were unlikely to reply to such sensitive questions over the phone from a stranger. In addition, the participants could not reflect the COPD population because 70.2% had stage 2 COPD, 5% had stage 4 COPD, and 77.3% of the cohort were classified as overweight or obese, while no control group was included in the comparison. Finally, some questions related to predictive factors were not asked, such as pelvic pelvic disorders, delivery type, delivery of a large birthweight baby, history of episiotomy or instrumental delivery, hysterectomy, and prostate hyperplasia status.
Conclusions
The association between chronic obstructive pulmonary disease (COPD) and urinary incontinence (UI) severity has been inadequately recognized in clinical practice. This study found a moderate correlation between UI severity and health-related quality of life (HRQoL) among COPD patients. The findings suggest that UI substantially affects HRQoL in this patient population. Additionally, UI severity was associated with multiple factors, including older age, higher body mass index (BMI), greater breathlessness, and increased medication use. The multifactorial nature of UI severity underscores the necessity of routine UI screening in COPD patients, accompanied by targeted educational interventions and specialist continence clinic referrals for comprehensive management.
Data Sharing Statement
The data are available for research purposes upon reasonable request from the corresponding authors.
Ethics Approval and Informed Consent
This study was approved by the Institutional Review Board of King Saud University (Ref. No.20/0288/IRB) and was conducted from September 2020 to February 2021 in accordance with the Declaration of Helsinki guidelines. Informed consent was obtained from all participants prior to their participation in this study.
Consent for Publication
No individual or identifiable data have been published as part of this manuscript.
Acknowledgments
We would like to express our sincere appreciation to the participants for their invaluable contribution and participation in the project. Special thanks to Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R286), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia for supporting this project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2025R286), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia. The study sponsor had no role in the data analysis or collection, writing of the report, or decision to submit the paper for publication.
Disclosure
The authors declare that this research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
References
1. Battaglia S, Benfante A, Principe S, Basile L, Scichilone N. Urinary incontinence in chronic obstructive pulmonary disease: a common co-morbidity or a typical adverse effect? Drugs Aging. 2019;36(9):799–806. doi:10.1007/s40266-019-00687-4
2. Hrisanfow E, Hägglund D. The prevalence of urinary incontinence among women and men with chronic obstructive pulmonary disease in Sweden. J Clin Nurs. 2011;20(13–14):1895–1905. doi:10.1111/j.1365-2702.2010.03660.x
3. Al-Badr A, Brasha H, Al-Raddadi R, Noorwali F, Ross S. Prevalence of urinary incontinence among Saudi women. Int J Gynecol Obstet. 2012;117(2):160–163. doi:10.1016/j.ijgo.2011.12.014.
4. Bernards ATM, Berghmans BCM, Slieker-ten Hove M, Staal JB, de Bie RA, Hendriks EJM. Dutch guidelines for physiotherapy in patients with stress urinary incontinence: an update. Int Urogynecol J. 2014;25(2):171–179. doi:10.1007/s00192-013-2219-3
5. Hu J, Meek P. Health-related quality of life in individuals with chronic obstructive pulmonary disease. Heart Lung. 2005;34(6):415–422. doi:10.1016/j.hrtlng.2005.03.008.
6. Blinderman CD, Homel P, Billings JA, Tennstedt S, Portenoy RK. Symptom distress and quality of life in patients with advanced chronic obstructive pulmonary disease. J Pain Sympt Manage. 2009;38(1):115–123. doi:10.1016/j.jpainsymman.2008.07.006.
7. Jarad NA, Patel P, Buswell J. Epidemiology and risk factors of urinary incontinence in patients with chronic obstructive pulmonary disease (COPD). Formerly Bristol Medico-Chirurgical J. 2015;114:3.
8. Hirayama F, Binns CW, Lee AH, Senjyu H. Urinary incontinence in Japanese women with chronic obstructive pulmonary disease. J Phys Therap Sci. 2005;17(2):119–124. doi:10.1589/jpts.17.119.
9. Hirayama F, Lee AH, Hiramatsu T, Tanikawa Y. Breathlessness is associated with urinary incontinence in men: a community-based study. BMC Pulm Med. 2010;10(1):2. doi:10.1186/1471-2466-10-2
10. Newman DK. In men and women with COPD the presence of urinary incontinence is associated with poorer quality of life. Evid-Based Nurs. 2014;17(1):22–23. doi:10.1136/eb-2013-101290.
11. Jaitovich A, Barreiro E. Skeletal muscle dysfunction in chronic obstructive pulmonary disease. What We know and can do for our patients. Am J Respir Crit Care Med. 2018;198(2):175–186. doi:10.1164/rccm.201710-2140CI
12. Adis Medical Writers. Manage urinary incontinence in COPD depending on whether it is stress, urge or mixed. Drugs Ther Perspect. 2020;36(6):230–233. doi:10.1007/s40267-020-00735-9.
13. Hashimoto M, Hashimoto K, Ando F, Kimura Y, Nagase K, Arai K. Prescription rate of medications potentially contributing to lower urinary tract symptoms and detection of adverse reactions by prescription sequence symmetry analysis. J Pharm Health Care Sci. 2015;1(1):7. doi:10.1186/s40780-014-0004-1
14. Hrisanfow E, Hägglund D. Impact of cough and urinary incontinence on quality of life in women and men with chronic obstructive pulmonary disease. J Clin Nurs. 2013;22(1–2):97–105. doi:10.1111/j.1365-2702.2012.04143.x
15. Johns DP, Walters JA, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thoracic Dis. 2014;6(11):1557.
16. Weisell RC. Body mass index as an indicator of obesity. Asia Pac J Clin Nutr. 2002;
17. Finkelstein MM. Medical conditions, medications, and urinary incontinence. Analysis of a population-based survey. Can Family Physician. 2002;48(1):96–101.
18. Agustí A, Celli BR, Criner GJ, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit Care Med. 2023;207(7):819–837. doi:10.1164/rccm.202301-0106PP
19. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Leidy NK. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509.
20. Al-Moamary MS, Al-Hajjaj MS, Tamim HM, Al-Ghobain MO, Al-Qahtani HA, Al-Kassimi FA. The reliability of an Arabic translation of the chronic obstructive pulmonary disease assessment test. Saudi Med J. 2011;32(10):1028–1033.
21. Al-Shaikh G, Al-Badr A, Al Maarik A, Cotterill N, Al-Mandeel HM. Reliability of Arabic ICIQ-UI short form in Saudi Arabia. Urology Ann. 2013;5(1):34–38. doi:10.4103/0974-7796.106964.
22. Uebersax JS, Wyman JF, Shumaker SA, McClish DK. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Neurourol Urodynamic. 1995;14(2):131–139. doi:10.1002/nau.1930140206
23. Franco AVM, Lee F, Fynes MM. Is there an alternative to pad tests? Correlation of subjective variables of severity of urinary loss to the 1‐h pad test in women with stress urinary incontinence. BJU Int. 2008;102(5):586–590. doi:10.1111/j.1464-410X.2008.07612.x
24. El‐Azab AS, Mascha EJ. Arabic validation of the urogenital distress inventory and adapted incontinence impact questionnaires—short forms. Neurourol Urodynamic. 2009;28(1):33–39. doi:10.1002/nau.20609
25. Skorupska K, Grzybowska ME, Kubik-Komar A, Rechberger T, Miotla P. Identification of the urogenital distress inventory-6 and the incontinence impact questionnaire-7 cutoff scores in urinary incontinent women. Health Qual Life Outcomes. 2021;19(1):87. doi:10.1186/s12955-021-01721-z
26. Huang WC, Yang SH, Yang SY, Yang E, JM Y. The correlations of incontinence-related quality of life measures with symptom severity and pathophysiology in women with primary stress urinary incontinence. World J Urol. 2010;28(5):619–623. doi:10.1007/s00345-009-0485-y
27. Altaweel W, Alharbi M. Urinary incontinence: prevalence, risk factors, and impact on health related quality of life in Saudi women. Neurourol Urodynamic. 2012;31(5):642–645. doi:10.1002/nau.22201
28. Alshammari S, Alyahya MA, Allhidan RS, Assiry GA, AlMuzini HR, AlSalman MA. Effect of urinary incontinence on the quality of life of older adults in Riyadh: medical and sociocultural perspectives. Cureus. 2020;12(11). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7681939/. Accessed June 30, 2024.
29. Yu CJ, Hsu CC, Lee WC, Chiang PH, Chuang YC. Medical diseases affecting lower urinary tract function. Urological Sci. 2013;24(2):41–45. doi:10.1016/j.urols.2013.04.004.
30. Varela JE, Hinojosa M, Nguyen N. Correlations between intra-abdominal pressure and obesity-related co-morbidities. Surg Obesity Related Dis. 2009;5(5):524–528. doi:10.1016/j.soard.2009.04.003.
31. Tamanini JTN, Lebrão ML, Duarte YA, Santos JL, Laurenti R. Analysis of the prevalence of and factors associated with urinary incontinence among elderly people in the municipality of São Paulo, Brazil: SABE study (health, wellbeing and aging). Cadernos de saude publica. 2009;25:1756–1762. doi:10.1590/S0102-311X2009000800011
32. Kessler M, Facchini LA, Soares MU, Nunes BP, França SM, Thumé E. Prevalence of urinary incontinence among the elderly and relationship with physical and mental health indicators. Revista Brasileira de Geriatria e Gerontologia. 2018;21(4):397–407. doi:10.1590/1981-22562018021.180015.
33. Yates A. Addressing the gender gap in urinary continence care. Br J Nurs. 2023;32(Sup19):S11–S16. doi:10.12968/bjon.2023.32.Sup19.S11
34. Jones JS. Impaired sphincter control in the dyspnoeic. Lancet. 1977;310(8037):532–533. doi:10.1016/S0140-6736(77)90666-3
35. Lira Borges C, Cavalcante Fernandes BK, Silva Nunes Cavalcante ML, Bastos Barbosa RG, Aires Peixoto Junior A, Gomes de Menezes LC. Risk factors for urinary incontinence in institutionalized elderly. Revista Estima. 2019;17. Available from: https://search.ebscohost.com/login.aspx?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=18063144&AN=143036849&h=pXjypc%2BNIrjoxoJ%2FcNs0nNGvH%2BaqxqXLD3AatDD3mNK6S0erQiCxN5nP8HeIuz7Z7wxj%2FxbgptFywwdI8N6XYg%3D%3D&crl=c. Accessed June 30, 2024.
36. Marques LP, Schneider IJC, Giehl MWC, Antes DL, d’Orsi E. Demographic, health conditions, and lifestyle factors associated with urinary incontinence in elderly from Florianópolis, Santa Catarina, Brazil. Revista Brasileira de Epidemiologia. 2015;18(3):595–606. doi:10.1590/1980-5497201500030006.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Comparison of STAR and GOLD in Assessing Disease Severity Among High-Risk and COPD Patients: Evidence from Enjoying Breathing Program in China
Huang K, Tang X, Chu X, Niu H, Li W, Zheng Z, Peng Y, Lei J, Li Y, Li B, Yang T, Wang C
International Journal of Chronic Obstructive Pulmonary Disease 2024, 19:2751-2762
Published Date: 27 December 2024

