Back to Journals » Journal of Pain Research » Volume 18
Migraine Headache and Its Related Disability Factors Among University Students in Jordan: A Cross-Sectional Study
Authors Almomani MA , Almomani BA , Al-Sawalha NA, Alqudah AA
Received 5 December 2024
Accepted for publication 4 April 2025
Published 16 April 2025 Volume 2025:18 Pages 2093—2104
DOI https://doi.org/10.2147/JPR.S504602
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Alexandre F DaSilva
Miral A Almomani,1 Basima A Almomani,2 Nour A Al-Sawalha,2 Ahmad A Alqudah3
1Department of Pediatrics and Neonatology, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 3Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan
Correspondence: Miral A Almomani, Department of Pediatrics and Neonatology, Faculty of Medicine, Jordan University of Science and Technology, P.O. Box 3030, Irbid, 22110, Jordan, Email [email protected]
Introduction: Headache is a common complaint in medical practice that affects daily activity and quality of life. University students, especially, face psychological and academic stressors that may trigger migraine, leading to functional impairment. This can hinder concentration, studying, and academic performance, resulting in disability, reduced productivity, and absenteeism. Understanding the factors contributing to headache-related disability in Jordanian students is essential for improving mental health and guiding policies to promote academic success and overall well-being.
Aim: The purpose of this study was to investigate the prevalence, features, and determinants of migraine headache-related disability among university students in Jordan.
Methods: A cross-sectional survey was conducted among university students in Jordan. An online questionnaire was distributed using social media. A convenient sample of students from different universities across geographical areas in Jordan was invited to participate in the study.
Results: Out of 1276 recruited participants, 64.97% of them have a history of headache in the previous 3 months. Of those, 80.22% probably have a diagnosis of migraine headache and 46% of them have an aura. Photophobia was the most common associated symptom (~90%) and sleep disturbance was the most reported factor trigger migraine attacks (83%). Most of the participants (82%) used analgesic medications, mainly OTC drugs (66.8%). Students with severe migraine intensity were more likely to have moderate-severe disability than those with mild/moderate intensity (OR = 1.69, 95 CI% = 1.23– 2.34, p value = 0.001). In addition, the presence of an aura was associated with moderate-severe disability (OR = 1.57, 95 CI% = 1.14– 2.16, p value = 0.006).
Conclusion: This study highlights the high prevalence of migraine headache among university students in Jordan, with photophobia and sleep disturbances identified as common triggers. The findings suggest that students with severe migraine intensity and those experiencing aura are more likely to face moderate-to-severe disability. The widespread use of analgesic medications, particularly over-the-counter drugs, underscores the need for targeted interventions to manage migraine symptoms and enhance the quality of life for affected students.
Keywords: features, disability, headache, migraine, determinants, prevalence, university students
Introduction
Headache is a common compliant in medical practice that affects daily activity and the quality of life of all age groups; children, adolescent, and adults.1 It is a significant health burden for the individual and society. Headache is divided into two types: primary and secondary. Primary headaches are presented as migraine or tension type, while secondary headaches can be caused by other underlying conditions such as infection, head injuries, vascular disorders, and brain tumor among others.1 The clinical diagnosis of headache is performed based on the criteria provided by the International Classification of Headache Disorders, 3rd edition (ICHD-3).2 According to the Global Burden of Disease 2019, migraine was ranked as the second cause of disability worldwide (among both genders and all ages) and the first place in young women.3
Migraine is the most disabling primary headache affecting adults, and the pathophysiology of migraine is still not known but can be influenced by age, genetics, eating habits and stress.4 Migraine is prevalent among university students, predominantly females, and has been linked with negative impact on academic performance and daily activity.5,6 A systematic meta review of 56 studies among university students revealed that migraine prevalence was 16.1% (range from 2.4% to 48.5%).6 Although numerous population-based studies on migraine have been conducted in Arab countries, few have specifically focused on its prevalence among university students. These studies, which included both medical and non-medical university students, reported varying degree of migraine prevalence; 11.7% and 17.27% in Egypt,7,8, 26.3% in UAE,9 35.4% in Saudi Arabia,10 27.9% in Kuwait11 and 12.2% in Oman.12 Ibrahim et al reported that female gender, family history, and chronic diseases were associated with migraine among university student in Saudi Arabia.10 Both sleep disturbance and stress were the most common reported migraine triggers among university Arab students.10–12
While global research on migraines is expanding, there is limited data on migraines among Jordanian students. Most headache studies in Jordan over the past 15 years have primarily focused on schoolchildren.1,13–15 ALBashtawy et al found 19.0% of high school students had tension-type headache and 8.8% had migraine.1 A study among adults reported that 82.3% of participants complained from headache: 36.1% was tension type, while 7.7% was migraine type.16 University students, however, face unique psychological and physical stressors, including high demands, exams, years of education, and performance pressure, all of which can disrupt sleep, elevate stress, and trigger migraine. This can negatively affect academic performance, productivity, and quality of life, with lasting effects on health and career. No previous studies in Jordan have specifically focused on migraine headache and associated determinants among university students.6,10 The main goal of this study was to determine the prevalence and features of migraine among university students in Jordan. Additionally, the study aimed to assess the impact of migraine on daily activity and productivity, as well as the approach of medication-use among migraine sufferers. This study is vital in Jordan due to the unique demographic, cultural factors, and academic pressures faced by university students, as well as differences in healthcare access across countries. Understanding these factors is essential for developing region-specific interventions. The findings will help address healthcare gaps, inform local health policies, and enhance student well-being and academic performance.
Materials and Methods
Ethics Statement
The ethical approval for this research was obtained from the institutional review boards (IRB) at the Jordan University of Science and Technology (57/140/2021). A written consent form was obtained from the participants before filling in the questionnaire, and the participants were informed about the purpose of the study, in accordance with the Declaration of Helsinki.
Study Design
A cross-sectional survey was conducted among university students in Jordan. An online questionnaire to assess migraine headache was distributed via social media over six months (from August 7, 2022, to Feb 9, 2023). The study included university students enrolled in higher education institutions in Jordan, who voluntarily completed the questionnaire. A convenient sample approach was used, inviting eligible students from various universities across the country to participate. Face validity was performed by experts in the field. The questionnaire was piloted (n = 15) to assess its content and improve clarity. Based on their feedback, several important areas for improvement were identified, leading to the following changes: rewording specific questions for clarity and better understanding, refining response options to capture a broader range of answers, improving section flow, and removing or combining unclear or redundant questions. Approximately 10 min was needed to complete the survey. At the end of the survey, a comprehensive and detailed education was provided and clearly communicated to all participants on lifestyle strategies aimed at reducing the risk of recurrent migraine attacks. Specifically, the importance of ensuring adequate and consistent sleep, eating regular meals, avoiding consumption of junk food or fizzy drinks, drinking enough water and identifying and avoiding known migraine triggers was emphasized. Additionally, specific guidance on how to manage a migraine attack when it occurs was provided. This included engaging in regular physical exercise, taking a rest or a nap when symptoms appear, creating a calm environment by resting in a quiet, dark room, applying gentle massage to the painful areas, and taking a warm shower to ease tension.
Questionnaire Items/Outcome Measures
The questionnaire items were selected from previous published literature1,10,11,16 with modifications on some items. The questionnaire consists of five sections: i) demographics (14 items), ii) initial evaluation of migraine (3 items), iii) features of migraine (10 items), iv) migraine Disability Assessment Scale (MIDAS, 7 items) and v) approach to medication use (8 items). Different demographic variables were collected from participants such as age, gender, income, program, college, year of study, habits (smoking and practice exercise), comorbidity, family history, level of vitamin D, anemia status, and number of studying hours/day.
A stepwise evaluation was used to determine the prevalence of migraine among students. The first question in this section was about headache history (in general) in the previous 3 months of study. Then, ID migraine™, a brief self-administered screening tool, was used to detect migraine among participants.17 ID migraine™ has a good validity18 and used in previous studies among university students.6,10,11 It consists of 3 items: during the last 3 months, have you had any of the following symptoms concerning headache pain: 1) Did you feel nauseated when you had headache pain?; 2) Did light bother you when you had a headache (a lot more than when there is no headache)?; 3) Did your headache limit your ability to work, study or do what you needed to do for at least 1 day?. A test diagnosis for migraine requires at least 2 out 3 positive responses. If the students are diagnosed with migraine based on ID migraine™, they continued answering other questions regarding clinical characteristics of their headache in the survey. It includes information about frequency, location of pain, time of headache, duration, intensity, associated symptoms, triggers, and alleviating factors of migraine.
Migraine Disability Assessment Scale (MIDAS) was used in the current study to assess the impact of migraine on daily activity and productivity of students during the last 3 months. MIDAS is a self-administered questionnaire to assess headache-related disability.19 It was developed,19 validated20 and translated into different languages including Arabic language.21–24 Finally, information about the approach of students to healthcare professionals and the types of medication used were collected. The total MIDAS score can be categorized into four disability grades as follows: Grade I (little or no disability) for scores between 1 and 5, Grade II (mild disability) for scores between 6 and 10, Grade III (moderate disability) for scores between 11 and 20, and Grade IV (severe disability) for scores greater than 21.19
Statistical Analysis
The SPSS was used to analyze and describe the collected data. Categorical variables were presented as count (percent) while continuous variables as mean (standard deviation, SD) or median (interquartile range, IQR). Univariate analysis was conducted using chi square for categorical data and independent t-test or Mann Whitney for continuous data as appropriate. In order to assess determinants that affect headache-related disability using MIDAS (little-no disability and mild disability versus moderate-severe disability), a multivariate analysis using binary logistic regression was performed including all variables with p < 0.2 on univariable analysis. The regression model was corrected for possible confounders by taking the variable as covariate to control for the potential effect. Odds ratio (OR) and 95% confidence interval were calculated. P-value less than 0.05 was considered statistically significant.
Results
Demographics
Out of 1526 received responses, 250 were excluded due to the complete absence of headache history and missing data related to subsequent questions about migraines, leaving 1276 responses for analysis. Of these, approximately 65% (n = 829/1276) of participants reported a history of headaches in the last 3 months. Additionally, 80.22% of participants (n = 665/829) who reported a history of headache also experienced at least two of the three symptoms commonly associated with migraine.
Most participants were females (94.2%), undergraduates (94.8%) and from non-medical majors (71.8%). The median age of participants was 21 years old, and in their first or second year. Regarding the daily routine of the participants, only 10% reported practicing or exercising daily. More than half of participants reported that they study for about 3 hours per day (60%) and sleep more than 6 hours per day (~54%). The majority of participants (91.8%) did not report having any comorbid condition. Thirty percent of participants reported that they had anemia in the previous 3 months while about 26% reported deficient levels of vitamin D in the last 3 months. Approximately, 44% of participants reported that they have a first degree family history of migraine headache. Table 1 summarizes the participants’ demographics and characteristics.
 |
Table 1 Demographics and Characteristics of Included Participants |
Initial Evaluation of Migraine Diagnosis
Out of 1276 participants, 64.97% (829/1276) of them have a history of headache in the previous 3 months. Of those, 80.22% (665/829) probably have a diagnosis of migraine headache (as they have at least 2 out of 3 positive responses of ID migraine™).
Features of Migraine Headache
Only 20% of participants who had migraine headaches were diagnosed by the physician. Approximately, 46% of participants have an aura. About half of participants (50.8%) reported a moderate level of bilateral pain that lasted less than 4 hours and usually occurred at night (~81%). The type of pain was reported by most participants (75.94%) as a compression type. The associated symptoms vary from photophobia (~90%) to abdominal pain (23%). Several factors trigger migraine attacks, such as sleep disturbance (83%), stress (78.8%), noise (63%), exposure to bright light (55.94%), among others. Being at rest position (83.91%) and in a quiet or dark room (83.61%) were the most common alleviating factors of migraine. Detailed characteristics of migraine headache are summarized in Table 2.
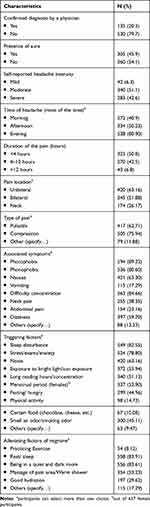 |
Table 2 Migraine Headache Features Among Participants (n = 665) |
Approach to Medication
Approximately, 12% of participants used to seek medical help for migraine relief. However, most of the participants (82%) used analgesic medications, mainly OTC drugs (66.8%), while only 12% of participants used traditional remedies for migraine relief. About 65% of participants noticed that the use of analgesics resulted in decreased migraine severity or frequency, while only 13% noticed increased frequency or severity of migraine. However, about 40% of participants developed tolerance toward the analgesics, and they had to increase the dose. Table 3 summarizes the participants’ responses toward the treatment approach.
 |
Table 3 Participants’ Approaches for Migraine Treatment |
Regarding the MIDAS categories, ~30% of participants reported little or no disability, while ~27% reported severe disability as summarized in Table 4. The results of univariate analysis for the determinants that affect headache-related disability using MIDAS (revealed the involvement of migraine intensity and aura (Table 5)). Moreover, the results of multivariate analysis showed that migraine intensity and aura were independently associated with MIDAS. Students with severe migraine intensity were more likely to have moderate-severe disability than those with mild/moderate intensity (OR = 1.69, 95 CI% = 1.23–2.34, p value = 0.001). In addition, the presence of an aura was associated with moderate-severe disability (OR = 1.57, 95 CI% = 1.14–2.16, p value = 0.006) (Table 5).
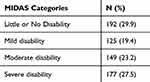 |
Table 4 Participants’ MIDAS Categorization |
 |
Table 5 Determinants of Migraine Disability Score (MIDAS) |
Discussion
Our study is considered distinctive in terms of being the foremost study of its type to estimate the prevalence of migraine among Jordanian university students. Our data revealed that 52.1% of the participants had migraine headaches, and most of them were females from non-medical majors. As a comparison, the prevalence among Indian college students was 14.12%.25 According to a meta-analysis comprising 34,904 university students, the prevalence of migraine varies from 2.4% to 48.5% across the world.6 Among college students, the overall prevalence of migraine was 16.1%.6 Nevertheless, lower migraine rates have been identified in the general population, including 7.7% in Jordan, 10.4% in Africa, 10.1% in Asia, 11.4% in Europe, and a world prevalence of 11.6%.26 Jordan seems to have lower migraine prevalence in the general population than many other parts of the world. The differences in the prevalence of migraines in may reflect intergenerational variations in prevalence, pain perception and tolerance changes.26 The higher prevalence among students may be attributable to various student-specific triggers, including young ages, stressful academic lives, sleep deprivation during examinations, and skipping meals.27
In the current study, most students who experienced migraine episodes were non-medical students. However, earlier studies were conducted on medical students and demonstrated that migraine prevalence varies widely among medical students across the world.28 It was stated that the prevalence of migraine in medical students was 17.27% in Egypt, 14.2% in Iran29 and 7.9% in Southeast China.30 On the contrary, several studies have shown a high migraine prevalence similar to the present study: 28% in India,31 27.9% in Kuwait,11 and 26.3% in Saudi Arabia.10 Noteworthy, the differences in the prevalence rates of migraine among medical students in our study compared to previous research may be attributed to variations in the number of participants and study duration. In our study, most students (80.22%) reported at least two out of three positive responses to the ID migraine™ questionnaire. This finding is double the results from two earlier studies in Sudan, which reported that 40% and 34.3% of university students experienced at least two headache attacks.32,33
In accordance with the present study findings, it is illustrated that sleep disturbance, stress, noise, and exposure to bright light were the most noticed triggering factors of the participants. Prior studies have demonstrated that the most prevalent migraine triggers were irregular/lack of sleep, stress/anxiety, noise, fatigue/physical activity and fasting.32,34,35 Additionally, menstruation was among the triggering factors in the previous research,28,30,36 which is consistent with the current study. Migraine prevalence variability between genders is that females had a significantly greater migraine than men. Women often experience higher psychosocial stress from caregiving, work-life imbalances, and societal expectations, which can trigger or worsen migraines. Gender disparities in social support, such as lack of emotional or practical help, further increase stress. Additionally, gender influences healthcare-seeking behavior—Women are more likely to seek medical care, leading to earlier diagnosis, but may have symptoms dismissed as hormonal or emotional, delaying treatment. In contrast, men may underreport symptoms due to stigma, resulting in poorer migraine management.6,37 In fact, estrogen hormone effects may partially explain this variation. Estrogen promotes the creation and release of nitric oxide and calcitonin gene-related peptides, which provoke migraine by activating and transmitting pain signals to the trigeminal nerve.37 Additionally, estrogen may enhance neuronal excitation and cause migraines by causing an imbalance in Mg2+ and Ca2+ levels.37
According to determinants affecting headache-related disability using MIDAS, students with severe migraine intensity were more likely to have a moderate-severe disability than those with mild/moderate intensity. This study supports evidence from previous observations where nearly 60% of individuals experienced moderate-to-severe disability.9 This was also similar to the findings of a systematic review where studies that provided MIDAS grade revealed that more than half of migraine sufferers were moderate to severely disabled due to migraine headaches.38 Earlier studies illustrated the prevalence of migraine with or without aura, and found that migraine without aura was more prevalent than migraine with aura (59.2% vs 40.8%, respectively)28. However, the use of MIDAS in assessing the rate of disability for patients with migraine with or without aura in the literature settings is limited. In our study, migraine with aura was significantly associated with moderate-to-severe MIDAS disability. Understanding disability severity, intensity, and aura can guide personalized treatments and enhance patient education. By integrating these factors into treatment plans (through routine screening), healthcare providers can tailor interventions (e.g cognitive-behavioral therapy) to the condition severity, improving outcomes and reducing the migraine burden.
The Global Assessment of Migraine Severity (GAMS) is another assessment method of disability.37 It has been shown that people who have migraine headache with aura are more likely to report a rise in GAMS with higher migraine severity compared to people without aura.39 There may be a genetic or racial explanation for these variations. The finding of causative mutations in three genes (CACNA1A, ATP1A2, and SCN1A) that are important in ion transport at synapses and glutamatergic transmission has provided insight into the etiology of familial hemiplegic migraine, which is a rare Mendelian condition of migraine with aura.40,41
Concerning migraine treatment, most of the participants in the current study used OTC medications such as acetaminophen and ibuprofen. This result ties well with a previous study in which acetaminophen was the most used painkiller by most migraine sufferers of Saudi students, followed by a combination of ibuprofen and acetaminophen.42 Previous studies attributed the popularity of acetaminophen to its affordability, safety, fewer gastrointestinal adverse events and its over-the-counter accessibility.12,43
In our study, there is a poor seeking of medical consultation which is comparable to those of a prior study in Saudi Arabia42 but lower than those of an Egyptian study.9 According to different studies, the consumption of OTC medications by a significant proportion of students is a potential cause of poor medical consultation for migraine.42,44 Due to the intensity of their pain, students with migraine may take an excessive quantity of OTC medications, which may create significant health issues. Consequently, an urgent need is to instruct students and encourage medical consultation to treat migraines effectively.9
It is plausible that some limitations could have affected the obtained results. The first limitation was that it was a cross-sectional study demonstrating the relationship between variables without showing a cause-and-effect relationship. The second limitation is that the study was carried out on a segment of the population (university students), thus, the outcomes cannot be generalized to the whole population. Third, the absence of clinical confirmation of migraine diagnoses is a limitation; however, due to the nature of the research design, clinical evaluations were not included. In addition, an online and self-administered survey that employs convenient sampling might be susceptible to sample and recall biases, which could contribute to an overestimation of the prevalence.
Conclusions
The current study revealed high migraine prevalence in university students. Most participants were non-medical students. In addition, students who experienced severe migraines had moderate-to-severe disabilities. Most university students used OTC medications without seeking medical advice. These findings highlight the urgent need to encourage medical consultation to treat migraines effectively. As such, further studies should be conducted with a larger sample size to validate the current findings.
Disclosure
The authors report no conflicts of interest in this work.
References
1. ALBashtawy M, Al Qadire M, Aloush S, et al. Assessment of headache among high school students in Jordan. J Sch Nurs. 2019;35(2):88–95. doi:10.1177/1059840517734613
2. Society TIH. The International Classification of Headache Disorders.
3. Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z. Lifting the burden: the global campaign against H. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020;21(1):137. doi:10.1186/s10194-020-01208-0
4. Ashina M. Migraine. N Engl J Med. 2020;383(19):1866–1876. doi:10.1056/NEJMra1915327
5. El-Metwally A, Toivola P, AlAhmary K, et al. The epidemiology of migraine headache in Arab countries: a systematic review. Sci World J. 2020;2020:4790254. doi:10.1155/2020/4790254
6. Wang X, Zhou HB, Sun JM, Xing YH, Zhu YL, Zhao YS. The prevalence of migraine in university students: a systematic review and meta-analysis. Eur J Neurol. 2016;23(3):464–475. doi:10.1111/ene.12784
7. Ragab S, Zaitoun N, Elrafie A, et al. Migraine among Egyptian medical students: prevalence, disability and psychological distress-cross sectional study. Egypt J Neurol Psychiat Neurosurg. 2023;59(1):62. doi:10.1186/s41983-023-00665-z
8. Mohamed RG, Sarhan K, Kamel B, et al. Prevalence and characteristics of headache among medical students in Egypt: a multicentric cross-sectional study. BMJ Neurol Open. 2024;6(2):e000851. doi:10.1136/bmjno-2024-000851
9. Rustom A, Audi F, Al Samsam H, Nour R, Mursi AM, Mahmoud I. Migraine awareness, prevalence, triggers, and impact on university students: a cross-sectional study. Egypt J Neurol Psychiat Neurosurg. 2022;58(1):119. doi:10.1186/s41983-022-00555-w
10. Ibrahim NK, Alotaibi AK, Alhazmi AM, Alshehri RZ, Saimaldaher RN, Murad MA. Prevalence, predictors and triggers of migraine headache among medical students and interns in King Abdulaziz University, Jeddah, Saudi Arabia. Pak J Med Sci. 2017;33(2):270–275. doi:10.12669/pjms.332.12139
11. Al-Hashel JY, Ahmed SF, Alroughani R, Goadsby PJ. Migraine among medical students in Kuwait University. J Headache Pain. 2014;15(1):26. doi:10.1186/1129-2377-15-26
12. Deleu D, Khan MA, Humaidan H, Al Mantheri Z, Al Hashami S. Prevalence and clinical characteristics of headache in medical students in Oman. Headache. 2001;41(8):798–804. doi:10.1046/j.1526-4610.2001.01146.x
13. Hussein F, Alawneh HAB. Prevalence of headache and migraine in school children in Jordan. Sudan J Public Health. 2006;1(4):3.
14. Albashtawy M, Alhroub N, Zafar Z, et al. Prevalence and Triggering Factors of Headache among Jordanian Adolescents in Al-Mafraq Region. Sci World J. 2023;2023:5548694. doi:10.1155/2023/5548694
15. Al Momani M, Almomani BA, Masri AT. The clinical characteristics of primary headache and associated factors in children: a retrospective descriptive study. Ann Med Surg. 2021;65:102374. doi:10.1016/j.amsu.2021.102374
16. Alzoubi KH, Mhaidat N, Azzam SA, et al. Prevalence of migraine and tension-type headache among adults in Jordan. J Headache Pain. 2009;10(4):265–270. doi:10.1007/s10194-009-0122-6
17. Lipton RB, Dodick D, Sadovsky R, et al. A self-administered screener for migraine in primary care: the ID Migraine validation study. Neurology. 2003;61(3):375–382. doi:10.1212/01.wnl.0000078940.53438.83
18. Cousins G, Hijazze S, Van de Laar FA, Fahey T. Diagnostic accuracy of the ID Migraine: a systematic review and meta-analysis. Headache. 2011;51(7):1140–1148. doi:10.1111/j.1526-4610.2011.01916.x
19. Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–28. doi:10.1212/wnl.56.suppl_1.s20
20. Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN. Validity of the Migraine Disability Assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain. 2000;88(1):41–52. doi:10.1016/S0304-3959(00)00305-5
21. Zandifar A, Asgari F, Haghdoost F, et al. Reliability and validity of the migraine disability assessment scale among migraine and tension type headache in Iranian patients. Biomed Res Int. 2014;2014:978064. doi:10.1155/2014/978064
22. Iigaya M, Sakai F, Kolodner KB, Lipton RB, Stewart WF. Reliability and validity of the Japanese Migraine Disability Assessment (MIDAS) Questionnaire. Headache. 2003;43(4):343–352. doi:10.1046/j.1526-4610.2003.03069.x
23. Rodriguez-Almagro D, Achalandabaso A, Rus A, Obrero-Gaitan E, Zagalaz-Anula N, Lomas-Vega R. Validation of the Spanish version of the migraine disability assessment questionnaire (MIDAS) in university students with migraine. BMC Neurol. 2020;20(1):67. doi:10.1186/s12883-020-01646-y
24. Mourad D, Hajj A, Hallit S, Ghossoub M, Khabbaz LR. Validation of the Arabic version of the Migraine Disability Assessment Scale among Lebanese patients with migraine. J Oral Facial Pain Headache. 2025;33(1):47–53. doi:10.11607/ofph.2102
25. Ray BK, Paul N, Hazra A, et al. Prevalence, burden, and risk factors of migraine: a community-based study from Eastern India. Neurol India. 2017;65(6):1280–1288. doi:10.4103/0028-3886.217979
26. Woldeamanuel YW, Cowan RP. Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci. 2017;372:307–315. doi:10.1016/j.jns.2016.11.071
27. Gu X, Xie Y. Migraine attacks among medical students in Soochow University, Southeast China: a cross-sectional study. J Pain Res. 2018;11:771. doi:10.2147/JPR.S156227
28. Oraby MI, Soliman RH, Mahmoud MA, Elfar E, Abd ElMonem NA. Migraine prevalence, clinical characteristics, and health care-seeking practice in a sample of medical students in Egypt. Egypt J Neurol Psychiat Neurosurg. 2021;57(1):26. doi:10.1186/s41983-021-00282-8
29. Ghorbani A, Abtahi SM, Fereidan-Esfahani M, et al. Prevalence and clinical characteristics of headache among medical students, Isfahan, Iran. J Res Med Sci. 2013;18(Suppl 1):S24–27.
30. Gu X, Xie Y. Migraine attacks among medical students in Soochow University, Southeast China: a cross-sectional study. J Pain Res. 2018;11:771–781. doi:10.2147/JPR.S156227
31. Menon B, Kinnera N. Prevalence and characteristics of migraine in medical students and its impact on their daily activities. Ann Indian Acad Neurol. 2013;16(2):221–225. doi:10.4103/0972-2327.112472
32. Halay S, Saror S, Abdalla A, et al. Prevalence of migraine and trigger factors among adult rural Sudanese population 2018. Curr J Appl Sci Technol. 2021;36:1–8.
33. Osman Ali MM, Abbasher Hussien Mohamed Ahmed K, Omer MEA. Prevalence of migraine headaches and their impact on the academic performance of Sudanese medical students using ID-Migraine test as a screening tool: a cross-sectional study. Brain Behav. 2022;12(5):e2588. doi:10.1002/brb3.2588
34. Shahrakai MR, Mirshekari H, Ghanbari AT, Shahraki AR, Shahraki E. Neuroscience c. Prevalence of migraine among medical students in Zahedan Faculty of Medicine (Southeast of Iran). Basic Clin Neurosci. 2011;2(2):20.
35. Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi:10.1016/S0140-6736(12)61689-4
36. Noor T, Sajjad A, Asma A. Frequency, character and predisposing factor of headache among students of medical college of Karachi. J Pak Med Assoc. 2016;66(2):159–164.
37. Gupta S, Mehrotra S, Villalon CM, Perusquia M, Saxena PR, MaassenVanDenBrink A. Potential role of female sex hormones in the pathophysiology of migraine. Pharmacol Ther. 2007;113(2):321–340. doi:10.1016/j.pharmthera.2006.08.009
38. Abu Bakar N, Tanprawate S, Lambru G, Torkamani M, Jahanshahi M, Matharu M. Quality of life in primary headache disorders: a review. Cephalalgia. 2016;36(1):67–91. doi:10.1177/0333102415580099
39. Sajobi TT, Amoozegar F, Wang M, et al. Global assessment of migraine severity measure: preliminary evidence of construct validity. BMC Neurol. 2019;19(1):53. doi:10.1186/s12883-019-1284-8
40. Bron C, Sutherland HG, Griffiths LR. Exploring the Hereditary Nature of Migraine. Neuropsychiatr Dis Treat. 2021;17:1183–1194. doi:10.2147/NDT.S282562
41. Cader ZM, Noble-Topham S, Dyment DA, et al. Significant linkage to migraine with aura on chromosome 11q24. Hum mol Genet. 2003;12(19):2511–2517. doi:10.1093/hmg/ddg252
42. Desouky DE, Zaid HA, Taha AA. Migraine, tension-type headache, and depression among Saudi female students in Taif University. J Egypt Public Health Assoc. 2019;94(1):7. doi:10.1186/s42506-019-0008-7
43. Ong JJY, De Felice M. Migraine treatment: current acute medications and their potential mechanisms of action. Neurotherapeutics. 2018;15(2):274–290. doi:10.1007/s13311-017-0592-1
44. Nandha R, Chhabra MK. Prevalence and clinical characteristics of headache in dental students of a tertiary care teaching dental hospital in Northern India. Int J Basic Clin Pharmacol. 2013;2(1):51–55.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

