Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Muscular and Renal Safety of Ticagrelor with High-Intensity Statins: Retrospective Cohort Findings
Authors Alshammari AS, Shalwala AA, Alnuhait MA , Alhazmi AY, Fagieha RE, Hallabi NB, Alandijani EA, Aloufi MA, Alharbi MS, Alzahrani RS, Elkholy EM, Elrggal ME, Alotaibi AS
Received 16 January 2025
Accepted for publication 26 May 2025
Published 8 June 2025 Volume 2025:21 Pages 861—867
DOI https://doi.org/10.2147/TCRM.S515732
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor De Yun Wang
Abdullah S Alshammari,1 Amer A Shalwala,2 Mohammed A Alnuhait,1 Abdulfattah Y Alhazmi,1 Refal E Fagieha,3 Nura Bin Hallabi,1 Eyad A Alandijani,1 Mansour A Aloufi,1 Mudhhi S Alharbi,1 Reem S Alzahrani,4 Emad M Elkholy,3 Mahmoud E Elrggal,5 Abdulmalik S Alotaibi1
1Pharmaceutical Practices Department, College of Pharmacy, Umm Al-Qura University, Makkah, Saudi Arabia; 2Pharmacy Department, King Abdulaziz Hospital, Makkah, Saudi Arabia; 3Pharmaceutical Services Department, King Abdullah Medical City, Makkah, Saudi Arabia; 4Pharmaceutical Company, Al nahdi Medical Company, Dammam, Saudi Arabia; 5Department of Pharmacology and Toxicology, Faculty of Medicine, Al-Qunfudah, Umm Al-Qura University, Makkah, Saudi Arabia
Correspondence: Abdulmalik S Alotaibi, Email [email protected]
Introduction: Ticagrelor is a widely used antiplatelet agent approved in over 70 countries, including the European Union and the United States, for reducing thrombotic events in patients with acute coronary syndromes (ACS). In clinical practice, combining ticagrelor with high-intensity statins is considered standard therapy for ACS. However, recent pharmacodynamic studies and case reports suggest potential drug-drug interactions that may increase the risk of adverse events, particularly muscular and renal complications. This study aimed to evaluate these risks in a real-world clinical setting in Saudi Arabia.
Methods: This retrospective observational cohort study was conducted at the Makkah Cardiology Center, Saudi Arabia. The study included adult patients (n = 577) who were prescribed high-intensity statins, with or without concurrent ticagrelor. The primary outcomes were the incidence of statin-associated muscular complications—defined as myalgia, myopathy, myositis, or rhabdomyolysis—and acute kidney injury (AKI). Clinical data were extracted from the hospital information system, and statistical comparisons were conducted between patients receiving statin monotherapy and those receiving combination therapy.
Results: The cohort consisted predominantly of male patients (74.5%). Muscle-related complications were significantly more common in the group receiving both ticagrelor and statins (20.2%) compared to the statin-only group (10.5%) (P = 0.001). Among comorbid conditions, hypertension was the only factor significantly associated with a higher incidence of muscle-related complications. Although a trend toward increased AKI incidence was observed in the combination therapy group, this difference did not reach statistical significance.
Conclusion: This study highlights potential safety concerns related to the co-administration of ticagrelor and high-intensity statins, particularly the increased risk of muscle-related complications. While the findings on AKI were inconclusive, the results support the need for cautious use of this combination and call for larger prospective studies to further evaluate its safety profile and optimize treatment strategies.
Keywords: ticagrelor, atorvastatin, rosuvastatin, statin-associated muscle symptoms, acute kidney injury
Introduction
Ticagrelor, as the pioneering antiplatelet agent in the cyclopentyltriazolopyrimidines class, has been authorized in more than 70 countries, including the European Union and the United States, to minimize the occurrence of thrombotic events in patients afflicted with acute coronary syndromes (ACS).1,2 When used in combination with statins, it is an essential component of therapy regimens for ACS. It is well recognized for its tolerance and perceived safety.1–3 The platelet inhibition and Patient Outcomes (PLATO) study showed a significant decrease in the risk of death in patients with acute coronary syndrome (ACS) who were treated with ticagrelor compared to clopidogrel (9.8% vs 11.7%, p = 0.001).4
Understanding metabolic pathways is crucial to understanding the potential interactions between ticagrelor and statins. Ticagrelor is mainly metabolized by the enzymes CYP3A4 and CYP3A5 and also has a small inhibitory impact on CYP3A4.5,6 Statins such as atorvastatin, lovastatin, and simvastatin are mainly metabolized by CYP3A4, while fluvastatin, pitavastatin, and rosuvastatin are more dependent on CYP2C9, suggesting fewer potential interactions with ticagrelor.7–9
The complex interaction between ticagrelor and some statins, including atorvastatin and rosuvastatin, is associated with the possibility of statin toxicity, leading to drug-related adverse effects such as muscle discomfort and acute kidney injury (AKI).2,6,10 The probability of experiencing drug-related adverse effects may be due to the fact that ticagrelor inhibits atorvastatin metabolism through CYP3A4, resulting in increased levels of atorvastatin in the bloodstream.2,10 Additionally, the ability of ticagrelor to negatively affect kidney function could result in higher levels of rosuvastatin in the blood, increasing the risk of rhabdomyolysis. Additional variables that may contribute include changes in ticagrelor metabolism caused by UGT2B7 or variations in rosuvastatin levels due to polymorphisms in transporters such as OATP1B1 or P-gp.11
In 2019, Theetha Kariyanna et al, from the United States, published a notable study that included case reports and a scoping review. The study focused on the appearance of rhabdomyolysis and AKI in patients taking ticagrelor and statins at the same time. Increased levels of creatinine kinase (CK) and serum creatinine (SCr) suggested a probable pharmacological interaction that led to the discontinuation of these drugs. After receiving proper resuscitation, the patients received their P2Y12 inhibitors replaced with clopidogrel after recovery from AKI and rhabdomyolysis. Subsequent examinations conducted two months later indicated the absence of any recurrence of symptoms and consistent levels of CK. An examination of 11 documented cases has shown a connection between ticagrelor and AKI, as well as rhabdomyolysis. This study suggests that when both drugs are used together, they may lead to higher levels of statins in the body, which in turn increases the probability of experiencing negative consequences.12
Despite this knowledge, there is a lack of comprehensive research that examines the complications arising from the concurrent use of ticagrelor with high-intensity statins, particularly within the Saudi Arabian context. This study aims to bridge this gap by evaluating the complications associated with the combined use of ticagrelor and high-intensity statins.
Materials and Methods
This retrospective observational cohort study, conducted at the Makkah Cardiology Center, Saudi Arabia, aimed to assess the incidence of statin-associated muscle problems (such as myalgia, myopathy, myositis, and rhabdomyolysis), as well as AKI. The study conducted a comparison of results between people who received ticagrelor in combination with atorvastatin or rosuvastatin and those who received only atorvastatin or rosuvastatin. In this study, we included all three subtypes of Acute Coronary Syndromes (ACS): unstable angina, non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). ACS typically results from the rupture or erosion of an unstable atherosclerotic plaque within a coronary artery, leading to partial or complete thrombosis and/or distal microembolization. This process impairs myocardial blood flow and causes ischemia. Unstable angina is characterized by transient myocardial ischemia without evidence of myocyte necrosis, as indicated by the absence of elevated cardiac troponins. In contrast, myocardial infarction involves more prolonged or severe ischemia and is defined by elevated biomarkers indicative of myonecrosis. NSTEMI is generally associated with a partially occluded coronary artery, leading to subendocardial ischemia, while STEMI is typically caused by complete coronary artery occlusion, resulting in transmural myocardial infarction. The inclusion criteria for our study encompassed individuals aged 20 years or older with a diagnosis of ACS, dyslipidemia, stroke, or more than one cardiovascular indication.13 The study meticulously extracted data from the hospital information system using a dedicated Microsoft Excel-based form. Data included sociodemographic characteristics (age, sex, height, weight, BMI), medical history, concurrent medications, and laboratory test results (such as creatinine kinase, creatinine, liver enzymes, etc).
Statistical Analysis
The sample size estimate for our study was determined to be 568 patients based on several parameters. This estimation was derived from an odds ratio of 1.3 obtained from data within the FDA Adverse Event Reporting System (FAERS) 17 Public Dashboard. Taking into account an error probability of 0.05, a study power of 80%, and a one-tailed study design, this sample size was calculated to ensure adequate statistical power for our comparative analysis.
Our comparative analysis involved categorizing instances of muscle pain as “muscle issues” and identifying cases of acute kidney injury (AKI) according to the precise criteria outlined in the Kidney Disease: Improving Global Outcomes (KDIGO) classification. The KDIGO classification system defines AKI based on specific criteria, including a documented increase in blood creatinine levels by 0.3 mg / dL over 48 hours or a 1.5-fold increase from baseline within the preceding seven days.
Statistical comparisons were made using Pearson’s chi-square test, employing a predetermined significance level set at p < 0.05 to determine statistical significance. Descriptive statistics for continuous variables, such as age and weight, were presented as mean values accompanied by their respective standard deviations. Categorical variables, including gender, were summarized in terms of frequency and percentage distributions.
To ensure data integrity and accuracy, our data set was meticulously analyzed, rigorous accuracy verification, and a comprehensive analytical process. This statistical software facilitated a systematic and detailed examination of the data, allowing us to derive meaningful conclusions and insights essential for this study. We use the Statistical Package for the Social Sciences (SPSS) software, specifically version 26 from IBM®, for this purpose.
Results
The study included a total of 577 patients, and men made up the majority of the cohort. The participants had a mean age of 58.5 years and an average height of 164 cm. Acute coronary syndrome (ACS) was the main diagnosis among patients, with 89.7% of the individuals falling into this diagnostic group. A significant number of patients in the group had comorbidities, 69.8% affected by hypertension, and 66.7% affected by diabetes. Therapeutic regimens were distributed as follows: 51% received statins alone, while 48.7% received combination treatment with statins and ticagrelor. Rosuvastatin, administered at a dose of 20 mg, was the statin prescribed most frequently, with 61.9% of patients receiving this drug. The table labeled Table 1 provides a comprehensive overview of demographic and clinical variables in detail.
 |
Table 1 Baseline Characteristics |
Examination of the group of patients showed a clear difference in the appearance of muscular problems between the groups. Patients who received statin and ticagrelor medications saw a markedly higher incidence of muscle-related problems (20.2%) compared to those who received only statin treatment (10.5%). Our findings revealed a significant increase in muscle pain risk among patients taking statin and ticagrelor simultaneously, with a relative risk (RR) of 1.93, indicating that this group was nearly twice as likely to experience muscle pain compared to the control group (Figure 1). On the contrary, there was no significant difference in the incidence of AKI between the two groups. The incidence of AKI was 5.3% for patients taking statin alone and 8.44% for those taking statin and ticagrelor, as shown in Table 2. Additional data analysis revealed that, among several co-existing medical conditions, only hypertension showed a significant correlation with a higher incidence of muscular problems, as seen in Table 3.
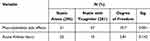 |
Table 2 Comparison Between Statin Alone and Statin with Ticagrelor Group |
 |
Table 3 Comparison Between Musculoskeletal Side Effects and No Musculoskeletal Side Effects |
 |
Figure 1 Incidence of muscle issues. |
Discussion
This study assesses the risk of muscle-related problems in individuals taking statins and ticagrelor simultaneously. It is a significant real-world investigation with a substantial sample size. The previous research consisted of case reports, which have limitations due to inherent biases and the possibility of under-reporting. Our results support previous data, demonstrating a higher incidence of muscle problems when these medications are co-administered, aligning with the suspected risk factors outlined in the literature. However, while our study revealed an increased incidence of muscle problems in patients taking statin and ticagrelor medications, it should be noted that statistical significance was not established for acute kidney injury (AKI), despite the higher incidence in this group. The lack of statistical significance for AKI underscores the complexity of establishing a direct causal relationship between these medications and renal complications.14,15
Rhabdomyolysis, a known consequence of statin therapy, is commonly associated with acute tubular necrosis caused by myoglobinuria. The possible interaction between ticagrelor and statins, namely their shared metabolism through cytochrome P450 (CYP) 3A4, raises concerns about drug interactions and concomitant toxicities, especially with atorvastatin.12 Although our study did not conclusively identify any cases of rhabdomyolysis, it should be noted that we observed five cases of significant muscle discomfort among participants. This finding underscores the need for more research to thoroughly investigate the potential for an elevated risk of rhabdomyolysis in patients receiving concurrent ticagrelor and statin therapy. In particular, the cessation of these medications followed by the subsequent resolution of acute kidney injury (AKI) and rhabdomyolysis symptoms in these cases strongly suggest a link to drug interactions. These observations highlight the critical need to increase awareness and follow-up of these adverse effects in clinical practice.5,10,12 To definitively demonstrate a link between this combination of medications and negative effects, it may be essential to increase the sample size and extend the research period.
The variation in the incidence of statin-induced myopathy between various classes is due to their differences in pharmacokinetic and lipophilic properties. Lipophilic statins, such as simvastatin and atorvastatin, have a greater tendency to accumulate in tissues beyond the liver. This could increase the chance of developing myopathy. Hydrophilic statins, such as pravastatin and rosuvastatin, have the characteristic of being hydrophilic, which means that they tend to accumulate less in the skeletal muscles.12 More research is necessary to identify the therapeutic consequences of the possibly reduced risk of muscle-related disorders associated with rosuvastatin.
The development of kidney failure caused by ticagrelor may intensify statin retention, further reducing the risk of statin-induced myopathy and further aggravated acute renal failure.12,13 Although we observed a higher incidence of AKI, our investigation could not conclusively confirm this association. The relationship between ticagrelor and rosuvastatin is influenced by several variables, such as possible metabolism via the CYP450 enzyme system, variations in transporter proteins, and genetic variants.12 Although understanding these pathways is difficult, our work emphasizes the need to conduct detailed studies of these interactions to improve patient safety. To draw conclusive conclusions about the influence of ticagrelor-induced renal degradation on statin metabolism, larger cohort studies are needed to fully understand the underlying processes.
The strength of this study lies in its rigorous methodology, employing a retrospective cohort design and comprehensive data extraction from the hospital information system, which enhances the reliability of real-world findings. However, it is important to acknowledge the inherent limitations associated with retrospective analyses. Notably, the presence of potential confounding variables, which may not have been fully accounted for, represents a significant limitation that could influence the interpretation and generalizability of the results.
This retrospective cohort study offers significant information on the safety implications of simultaneously using high-intensity statins and ticagrelor. It highlights possible concerns associated with AKI and statin-related muscle problems in a clinical setting. This study emphasizes the need for a careful evaluation, especially in patients prone to statin-related muscle problems when considering the use of this combination of medications. This statement highlights the need to perform personalized risk assessments and participate in collaborative decision-making when prescribing statins in combination with ticagrelor. It urges healthcare providers to be cautious, consider alternative treatments, or closely monitor patients who are at increased risk of experiencing these problems.
Conclusions
In conclusion, while this retrospective cohort study sheds light on safety concerns related to statin and ticagrelor, acknowledging its limitations, future research remains imperative to fully define the safety profile and optimize the treatment of patients receiving this combination therapy.
Data Sharing Statement
The data are secured to guarantee patients’ privacy.
Ethical Approval and Compliance
Ethical approval, identified by approval No. (HAPO-02-K-012-2022-03-1023), was diligently obtained from the Biomedical Research Ethics Committee at Umm Al-Qura University. This process ensured compliance with ethical standards and regulations governing research practices, including the protection of patient confidentiality and the safeguarding of participant welfare. The study was conducted in full accordance with the ethical principles outlined in the Declaration of Helsinki and its subsequent amendments.
Informed Consent Statement
The informed consent was waived due to the minimal risk associated with the design of retrospective studies.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that financial support was received for the research and/or publication of this article. This research work was funded by Umm AI-Qura University, Saudi Arabia under grant number: 25UQU4420024GSSR01.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Danielak D, Karaźniewicz-Łada M, Główka F. Ticagrelor in modern cardiology - an up-to-date review of most important aspects of ticagrelor pharmacotherapy. Expert Opin Pharmacother. 2018;19(2):103–112. doi:10.1080/14656566.2017.1421634
2. Teng R, Mitchell PD, Butler KA. Pharmacokinetic interaction studies of co-administration of ticagrelor and atorvastatin or simvastatin in healthy volunteers. Eur J Clin Pharmacol. 2013;69(3):477–487. doi:10.1007/s00228-012-1369-4
3. Akkaif MA, Ng ML, Sk Abdul Kader MA, Daud NAA, Sha’aban A, Ibrahim B. A review of the effects of ticagrelor on adenosine concentration and its clinical significance. Pharmacol Rep. 2021;73(6):1551–1564. doi:10.1007/s43440-021-00309-0
4. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–1057. doi:10.1056/NEJMoa0904327
5. Mrotzek SM, Rassaf T, Totzeck M. Ticagrelor leads to statin-induced rhabdomyolysis: a case report. Am J Case Rep. 2017;18:1238–1241. doi:10.12659/ajcr.905974
6. Vrkić Kirhmajer M, Macolić Šarinić V, Šimičević L, et al. Rosuvastatin-induced rhabdomyolysis - possible role of ticagrelor and patients’ pharmacogenetic profile. Basic Clin Pharmacol Toxicol. 2018;123(4):509–518. doi:10.1111/bcpt.13035
7. Bansal AB, Cassagnol M. HMG-CoA Reductase Inhibitors. In: StatPearls. StatPearls Publishing LLC.; 2024.
8. Ziaeian B, Dinkler J, Guo Y, Watson K. The 2013 ACC/AHA cholesterol treatment guidelines: applicability to patients with diabetes. Curr Diab Rep. 2016;16(2):13. doi:10.1007/s11892-015-0703-5
9. Bellosta S, Corsini A. Statin drug interactions and related adverse reactions: an update. Expert Opin Drug Saf. 2018;17(1):25–37. doi:10.1080/14740338.2018.1394455
10. Sibley RA, Katz A, Papadopoulos J. The interaction between rosuvastatin and ticagrelor leading to rhabdomyolysis: a case report and narrative review. Hosp Pharm. 2021;56(5):537–542. doi:10.1177/0018578720928262
11. Kido K, Wheeler MB, Seratnahaei A, Bailey A, Bain JA. Rhabdomyolysis precipitated by possible interaction of ticagrelor with high-dose atorvastatin. J Am Pharm Assoc. 2015;55(3):320–323. doi:10.1331/JAPhA.2015.14151
12. Kariyanna PT, Haseeb S, Chowdhury YS, et al. Ticagrelor and statin interaction induces rhabdomyolysis and acute renal failure: case reports and scoping review. Am J Med Case Rep. 2019;7(12):337–341. doi:10.12691/ajmcr-7-12-9
13. Rao SV, O’Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025. doi:10.1161/CIR.0000000000001309
14. Samuel G, Atanda AC, Onyemeh A, Awan A, Ajiboye O. A unique case of drug interaction between ticagrelor and statin leading to acute renal failure. Cureus. 2017;9(8). doi:10.7759/cureus.1633
15. Danielak D, Karaźniewicz-Łada M, Główka F. Assessment of the risk of rhabdomyolysis and myopathy during concomitant treatment with ticagrelor and statins. Drugs. 2018;78(11):1105–1112. doi:10.1007/s40265-018-0947-x
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

