Back to Journals » Infection and Drug Resistance » Volume 17
Nanopore Sequencing Technology: A Reliable Method for Pathogen Diagnosis in Elderly Patients with Community-Acquired Pneumonia
Authors Zhang X, Ye J, Wang L, Zhang L, Wang L, Jin H
Received 27 April 2024
Accepted for publication 19 August 2024
Published 24 August 2024 Volume 2024:17 Pages 3659—3667
DOI https://doi.org/10.2147/IDR.S475861
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xiyue Zhang,1,* Jian Ye,2,* Limin Wang,1 Liuhai Zhang,1 Liusheng Wang,1 Hualiang Jin1
1Department of Respiratory Medicine, Affiliated Hangzhou First People’s Hospital, School of Medicine, Westlake University, Hangzhou, People’s Republic of China; 2Department of Respiratory Medicine, Zhejiang Hospital, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hualiang Jin, Department of Respiratory Medicine, Affiliated Hangzhou First People’s Hospital, School of Medicine, Westlake University, Huansha Road 261, Hangzhou, 310006, People’s Republic of China, Tel +86 571-5600-6818, Fax +86 571-8791-4773, Email [email protected]
Purpose: Next-generation sequencing of the metagenome (mNGS) is gaining traction as a valuable tool for diagnosing infectious diseases. Compared to mNGS, pathogen detection based on Oxford Nanopore Technology further shortens the detection time. This study seeks to assess the efficacy of Nanopore sequencing in identifying pathogens associated with community-acquired pneumonia (CAP) among elderly individuals in China.
Patients and Methods: From January 2023 to June 2023, elderly patients with CAP were prospectively recruited from Hangzhou First People’s Hospital. A comprehensive set of clinical data was gathered, and bronchoalveolar lavage (BAL) fluid samples were collected. Concurrently, pathogen identification was performed using conventional microbiological diagnostic methods, Illumina sequencing, and Nanopore sequencing, and the diagnostic efficacy of pathogen detection was compared.
Results: The study included a total of 29 patients. The diagnostic positivity rates of traditional microbiological detection, Illumina sequencing, and Nanopore sequencing were 24.1%, 51.7%, and 48.3%, respectively. Their diagnostic specificities were 91.7%, 50%, and 75%, respectively. Compared to traditional microbiological detection, both Nanopore and Illumina sequencing showed significantly increased sensitivity. However, Nanopore sequencing exhibited relatively better consistency with the final clinical comprehensive diagnosis, with a Kappa value of 0.574. This outperformed traditional microbiological detection and Illumina sequencing, which had a Kappa value of 0.296 and 0.402, respectively. In addition, Nanopore sequencing required the shortest turnaround time.
Conclusion: Nanopore sequencing technology demonstrates as a reliable and rapid method for detecting pathogens in elderly patients with CAP.
Keywords: Nanopore sequencing technology, metagenomic next-generation sequencing, Elderly Community-Acquired Pneumonia, pathogen diagnosis
Introduction
As the aging process accelerates in China, community-acquired pneumonia (CAP) in the elderly is rapidly increasing, becoming one of the major threats to the elderly health.1 China has made notable progress in the prevention and treatment of respiratory diseases. However, the average annual percentage of age-standardized mortality rate for pneumonia among the urban elderly population and rural elderly men did not show significant improvement.2 With declining physiological function and increasing comorbidities among the elderly, CAP in the elderly is often more severe, with symptoms that may be atypical and easily overlooked, leading to misdiagnosis and adverse outcomes. For instance, a study on CAP in China, covering 16,585 patients, showed that the proportion of patients with pneumonia aged 65 and above was 28.7%, whereas the occurrence of pneumonia in patients aged 26–45 was only 9.2%.3 Traditional diagnostic methods for CAP rely mainly on microbiological culture and serological testing, but these methods are often less sensitive and time-consuming. For example, research has found that only 38% of adult pneumonia patients can have the pathogen identified through traditional microbiological detection.4 Progress in traditional diagnostic techniques has been limited. While some methods, like urine antigen testing, have seen recent advancements in pneumonia diagnosis, these techniques are often restricted to detecting specific pathogens.5 The overuse of broad-spectrum antibiotics is quite common among elderly pneumonia patients, who often receive antibiotic treatment before testing, making it more difficult to identify pathogens through traditional techniques. Delayed diagnosis leads to inappropriate empirical broad-spectrum antibiotic therapy, resulting in poor efficacy, prolonged hospitalization, and higher costs.6
Unlike traditional culture techniques, metagenomics next-generation sequencing (mNGS) technology directly sequences all nucleic acids in the sample without bias, combined with pathogenic microbial databases and specific algorithms to detect possible pathogenic microbial sequences in the sample.7 Based on this, both domestic and international guidelines and expert consensus have applied pathogen metagenomic detection to the clinical auxiliary diagnosis of infectious diseases, improving the process of detecting unknown pathogens.8,9 However, mNGS technology such as Illumina sequencing still has many limitations. One is that although the sequencing time has been significantly shortened, it still takes about 2 days to obtain the final result clinically. Secondly, mNGS requires sequences to be limited to a short read range of 200–500 bp, and the shorter lengths of the reads result in increased difficulty for the assembly and analysis of genomes, transcriptomes, and metagenomes.10
As sequencing technology has progressed, Nanopore sequencing, performed by Oxford Nanopore Technologies’ MinION sequencer, has become a method of choice for determining nucleotide sequences. This approach relies on detecting electrical signals produced as nucleic molecules traverse Nanopores. This approach enables the direct determination and sequencing of nucleic acid molecules, eliminating the need for PCR amplification, thereby avoiding biases and errors introduced by PCR amplification.11 Moreover, Nanopore sequencing offers longer read lengths, up to 2 Mb, greatly enhancing the accuracy of detection of various infectious pathogens. Additionally, the real-time analysis characteristic further shortens the turnaround time.12 However, due to insufficient research data of Nanopore sequencing technology on infectious diseases in China, especially lacking studies for elderly populations with CAP, this study aimed to compare the diagnostic efficacy of Nanopore sequencing technology with mNGS and traditional microbiological detection in elderly pneumonia.
Material and Methods
Patients Recruitment
This study is a prospective single-center investigation. Elderly patients over the age of 65 diagnosed with CAP and presented at Hangzhou First People’s Hospital were enrolled between January and July 2023. The diagnosis of CAP followed the 2018 Chinese Adult CAP Diagnosis and Treatment Guidelines.13 In the study, basic and clinical information about patients was collected, including age, symptoms, underlying conditions, and laboratory findings. The inclusion criteria included the following: (1) voluntary participation in this clinical study and signing of informed consent forms; (2) diagnosis meeting the above criteria for CAP; (3) agreement to undergo bronchoscopy examination and bronchoalveolar lavage, and obtain sufficient lavage fluid specimens; (4) good compliance and ability to complete the clinical study smoothly. And the exclusion criteria were: (1) Sample issues: BALF samples that did not meet the quality control standards for Illumina or Nanopore sequencing. (2) Cases with incomplete data. (3) Failure to sign the informed consent form and inability to cooperate with the researchers. The study adhered to the Declaration of Helsinki and received approval from the Medical Ethics Committee of Affiliated Hangzhou First People’s Hospital, Westlake University School of Medicine, and all patients signed informed consent forms (Approval number: ZN-20220606-0081-01).
Sample and Laboratory Testing
General patient information was collected, including age, gender, and general vital signs, as well as traditional microbiological detection such as laboratory blood routine, inflammation biomarkers, and blood antigen detection. All patients underwent bronchoscopy. Bronchoalveolar lavage fluid (BALF) was obtained following the protocol previously reported.14 We set aside 50 mL of qualified bronchoalveolar lavage fluid, using 30 mL for traditional microbiological testing, 10 mL for second-generation Illumina sequencing, and 10 mL for third-generation Nanopore sequencing.
Criteria for Pathogenic Microorganisms
The detection performance of traditional microbiological detection techniques (including traditional microbial culture, sputum smears, pathogen antigen detection, etc)., Illumina sequencing technology, and Nanopore sequencing technology for major pathogens was compared. In this study, the identification criteria for pathogenic microorganisms were as described previously:15,16 (1) This study included BALF samples obtained using fiberoptic bronchoscopy, excluding normal oropharyngeal microorganisms; (2) Microorganisms unrelated to pulmonary infections were excluded based on literature searches; (3) The species coverage ratio of bacteria, viruses, and parasites exceeded other microorganisms by 10 times, fungi by more than 5 times. For mycobacterium tuberculosis, only one sequence was determined as positive due to low DNA extraction content; (4) Microorganisms with less than three sequences for bacteria, fungi, and viruses are excluded. The identified pathogenic microorganisms, if clinically significant, are defined as clinically suspected pathogenic microorganisms; the final diagnosis of true positive pathogenic microorganisms in this study is established after discussion by two senior attending physicians in the respiratory department to serve as the final adjudicators for our study who were independent of our research. The diagnosis integrates the patient’s clinical features, traditional pathogen detection results, Illumina, Nanopore, pathological data, clinical outcomes, and other relevant factors to make a comprehensive assessment.
DNA Extraction
BALF samples were centrifuged at 14,000 g for 5 minutes. Next, after removing the supernatant, retain approximately 200 μL of supernatant and the precipitate within the centrifuge tube for subsequent use. In the third stage, add 10 μL of prepared lysozyme (20 mg/mL), incubate at 37°C for 15 minutes, then add hydrolase lytic enzyme (RT410, Tiangen Biotech, Beijing, China) for enzymatic degradation reaction, and centrifuge at 8000 g for 5 min. Finally, DNA was extracted using the TIANamp Micro DNA Kit (DP316, Tiangen Biotech, Beijing, China). DNA concentrations were quantified using a Qubit 4.0 fluorometer with the dsDNA HS Assay kit.
Library Preparation and Sequencing
For Illumina sequencing, the NEBNext Ultra II DNA Library Prep Kit (New England Biolabs Inc). was used to construct sequencing libraries, followed by sequencing on the Nextseq 550 DX (Illumina, CA, USA)17 Each sample yielded around 20 million sequence reads. Nanopore sequencing was performed on the GridION platform (Oxford Nanopore Technologies, Oxford, UK). Sequencing chips were initially quality-checked according to the manufacturer’s instructions. Upon passing quality control, libraries were constructed following the protocol of the library preparation kit and loaded onto the sequencing chips.18 Raw sequencing data were collected using the sequencing control software MinKNOW (Oxford Nanopore Technologies, Oxford, UK) and saved in fast5 format.
Bioinformatics Analyses for Illumina
The initial sequence data were subjected to a quality control process, which involved the elimination of reads with poor quality. Subsequently, the remaining high-quality reads were aligned to the human reference genome (GRCh38.p13) using the Burrows-Wheeler Aligner (BWA) to filter out any sequences originating from human sources.19 The remaining sequence data were then aligned and subsequently compared against databases containing microbial genome sequences. All pathogen sequence reference databases were sourced from NCBI RefSeq (ftp://ftp.ncbi.nlm.nih.gov/genomes/).20 Sequencing results were analyzed using IngeniSeq-MG, version 1.0, mNGS software (Zhejiang Dian Diagnostics Co., Ltd., Hangzhou, China).
Nanopore Sequencing and Data Analysis
The raw data from fast5 files were converted to fastq files using Guppy analysis software (Oxford Nanopore Technologies, Oxford, UK) with automatic evaluation of sequencing data quality. And the real-time identification and fastq file generation were performed using MinKnow software (version 1.11.5, Oxford Nanopore Technologies Ltd., Oxford, UK). Low-quality sequences were filtered out using the MinKnow software. Sequencing data underwent multi-sequence alignment and identification of pathogenic microbial sequences using Centrifuge v1.0.3 (http://www.ccb.jhu.edu/software/centrifuge/), utilizing the non-redundant nucleic acid database from the Johns Hopkins University Center for Computational Biology (Baltimore, MD, USA).
Statistical Analysis
SPSS 22.0 statistical software (SPSS Inc., Chicago, IL, United States) was utilized for the data analysis. Non-normally distributed data were represented by the median. Quantitative data were expressed as case numbers (percentages) [n (%)]. We employed the definitive identification of pathogenic microorganisms as a benchmark to assess the diagnostic accuracy of the three methods. This evaluation was conducted using either the chi-square test or Fisher’s exact test, depending on the data characteristics. The kappa value measured the consistency between the results of three techniques and final comprehensive diagnosis, respectively. A p-value < 0.05 indicated significant differences.
Results
The General Characteristics of the Study Population
In this study, a total of 35 cases of newly diagnosed elderly CAP patients were enrolled, among which 6 cases were confirmed as non-infectious diseases (1 case of tumor, 3 cases of non-infectious interstitial lung disease, and the remaining 2 cases were excluded due to finally diagnosed as non-infectious diseases). The final study population consisted of 29 cases, including 18 males and 11 females, with an average age of 69.8 years. Among them, 6 have a history of cardiovascular diseases (20.7%), 15 have chronic respiratory conditions (51.7%), and 5 have diabetes (17.2%). And 10 individuals have a smoking history (34.5%). The general information of all samples was presented in Table 1.
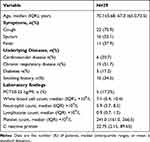 |
Table 1 Demographic and Clinical Characteristics of the 29 Patients |
Detection and Comparison of Pathogens
For the 29 patients, traditional microbiological detection identified only 5 types of bacteria and 4 types of fungi, while Illumina sequencing identified a total of 17 bacteria, 7 fungi, and 4 viruses, and Nanopore sequencing identified 9 bacteria, 5 fungi, and 6 viruses (Figure 1). After discussion by two senior physicians, the final diagnosis of true positive pathogenic microorganisms is established. Among them, traditional microbiological detection techniques identified 1 type of bacteria (Pseudomonas aeruginosa) and 2 types of fungi (Aspergillus fumigatus, Cryptococcus neoformans); Illumina identified 8 bacteria (Haemophilus influenzae, Pseudomonas aeruginosa, Klebsiella pneumoniae, Acinetobacter baumannii, Nocardia asteroides, Mycoplasma pneumoniae, Mycobacterium tuberculosis, Mycobacterium kansasii) and 5 fungi (Pneumocystis jirovecii, Candida albicans, Aspergillus niger, Aspergillus fumigatus, Fusarium spp).; Nanopore identified 7 bacteria (Haemophilus influenzae, Pseudomonas aeruginosa, Klebsiella pneumoniae, Acinetobacter baumannii, Mycoplasma pneumoniae, Mycobacterium tuberculosis, Mycobacterium kansasii) and 5 fungi (Pneumocystis jirovecii, Candida albicans, Aspergillus niger, Aspergillus fumigatus, Fusarium spp). Cytomegalovirus, Epstein-Barr virus, and Torque teno virus were the most common viruses detected by metagenomic sequencing in this study. However, based on clinical and imaging characteristics, and after discussion with two senior attending physicians, they were ultimately not considered true pathogenic microorganisms.
In terms of the types of pathogens detected, Nanopore sequencing and Illumina sequencing showed consistency in 23 cases (79.3%), including 16 cases of consistent positive results and 7 cases of consistent negative results. Therefore, Nanopore and Illumina detection rates are essentially similar, both significantly higher than those of traditional microbiological detection. Detailed information on the results of the final clinical diagnosis, traditional microbial technology, and both Illumina and Nanopore sequencing for all 35 cases included in the study can be found in the Supplementary Material (S1).
Diagnostic Performance
Using final clinical comprehensive diagnosis as the reference standard, the three techniques in this study detected true positive pathogenic microorganisms in 18 cases, with a positivity rate of 62.1%. The diagnostic positivity rates of traditional microbiological detection, Illumina sequencing, and Nanopore sequencing were 24.1%, 51.7%, and 48.3%, respectively, while their diagnostic specificities were 91.7%, 50%, and 75%, respectively. Statistical analysis showed that compared to traditional microbiological detection, both Nanopore sequencing and Illumina sequencing significantly improved sensitivity (P < 0.05). However, when comparing Nanopore sequencing with Illumina sequencing, there was no statistical difference in sensitivity and specificity (P > 0.05). Furthermore, Nanopore sequencing showed good consistency with the final clinical comprehensive diagnosis (Kappa value = 0.574, p < 0.01), and Illumina sequencing also demonstrated good consistency with the final comprehensive diagnosis (Kappa value = 0.402, p < 0.05). However, the positivity rate of traditional microbiological detection was only 24.1%, and there was a significant lack of consistency between traditional culture and the final comprehensive diagnosis (Kappa value = 0.296, p > 0.05) (Table 2).
 |
Table 2 Diagnostic Performance of Nanopore Sequencing, mNGS, and Traditional Culture |
Detection of Coinfections
In the detected truly positive infection cases, Nanopore sequencing and Illumina sequencing showed significant consistency, with no significant differences between the two techniques. Both identified 7 cases of coinfections, which were significantly higher than traditional microbiological detection techniques, where only 1 case of coinfections was detected. Among the 7 cases of coinfections, 3 cases were fungal - viral, 2 cases were bacterial - fungal, 1 case was bacterial - bacterial, and 1 case was fungal - bacterial – viral coinfection.
Discussion
In China, with the exacerbation of population aging, CAP has become prevalent among the elderly. Given that elderly patients often present with one or more underlying diseases, and the pathogens involved exhibit a wide range of diversity and complexity, the progression of the CAP in elderly tends to be swift. Consequently, there is a heightened incidence of severe pneumonia, posing a significant threat to the health of the elderly population. Therefore, early diagnosis and appropriate treatment are pivotal in enhancing the prognosis of CAP among the elderly community.21 This necessitates clinical physicians to swiftly and accurately ascertain the etiology of CAP in elderly patients.
Conventional microbial culture techniques possess several drawbacks. Studies have shown that with the use of traditional pathogen detection methods, only about 30% of pneumonia patients can identify their pathogens.22 In recent years, mNGS technology, with its advantages such as not relying on traditional microbial culture, broad pathogen coverage, and no need to preassume the presence of pathogens, has been widely used in pathogen diagnosis of respiratory infectious diseases. However, second-generation sequencing has relatively short read lengths, posing challenges in data analysis, which affects the efficiency and accuracy of assembly and alignment. Additionally, it is complex to operate, has long sequencing times, and is costly. In contrast, third-generation Nanopore sequencing technology has longer read lengths, faster sequencing speeds (>400bp/s), shorter detection cycles, lower costs, and covers core pathogens. It exhibits excellent performance in rapidly determining the etiology of pneumonia patients.23 However, whether Nanopore sequencing has superior diagnostic efficacy for the etiology of elderly pneumonia compared to second-generation sequencing, or has similar diagnostic efficacy, is currently unclear. Therefore, in this study, we systematically compared the diagnostic efficacy of three detection technologies (Nanopore sequencing, Illumina sequencing, and traditional microbiological detection) in elderly patients with CAP.
Compared to traditional detection techniques, mNGS greatly enhances the sensitivity of detecting pathogenic microorganisms. In this study, both Nanopore and Illumina sequencing detected significantly higher levels of pathogenic microorganisms in elderly pneumonia patients compared to traditional microbiological detection techniques, consistent with previous research.24 Some scholars have also compared the diagnostic efficacy of Illumina and Nanopore sequencing in the past. Previous studies have suggested that Illumina sequencing may have a relative advantage in bacterial detection positivity compared to Nanopore sequencing.12 In comparison with Illumina sequencing in this study, Nanopore sequencing detected relatively fewer pathogenic microorganisms, especially bacteria. However, there was no significant difference between Nanopore sequencing and Illumina sequencing in detecting true positive pathogenic microorganisms, both bacteria and fungi. Therefore, compared to Nanopore sequencing, Illumina sequencing in this study had a relatively higher rate of false positives. Additionally, this study suggests that Nanopore sequencing has a relatively higher specificity compared to Illumina sequencing, but statistically, there was no difference.
The next-generation metagenomic detection technology such as Nanopore sequencing further improves the concordance rate of the ultimate etiological diagnosis of pneumonia. Previous studies have suggested that compared to the final diagnosis, mNGS shows significantly higher consistency with the ultimate etiology of pneumonia than traditional detection techniques, and Nanopore sequencing has better concordance with the final diagnosis compared to Illumina sequencing.25 In this study, the kappa value between Nanopore sequencing and the clinical final diagnosis was 0.574, which was higher than that of Illumina sequencing and traditional detection techniques, indicating that among the three detection technologies, Nanopore sequencing has relatively the best consistency with the clinical final diagnosis.
Coinfections may be detrimental factors for elderly community-acquired pneumonia. Advanced detection technologies, such as Nanopore sequencing and Illumina sequencing mentioned in the previous context, play a significant role in identifying coinfections by allowing for the comprehensive analysis of genetic material present in clinical samples. The results in this study indicate that compared to traditional detection techniques, both Nanopore sequencing and Illumina sequencing significantly improve the ability to identify coinfections. Identifying coinfections is crucial for proper diagnosis and treatment because different pathogens may require different therapies. Additionally, coinfections can complicate clinical management, as they may exhibit atypical or overlapping symptoms, making diagnosis more challenging. By accurately identifying the diverse and complex array of pathogens involved, clinicians can tailor treatment strategies more effectively, thereby improving outcomes for elderly patients.
Compared to common pneumonia, elderly community-acquired pneumonia progresses relatively rapidly. The Nanopore technology’s real-time sequencing capabilities and high sensitivity make it a valuable tool for rapidly obtaining diagnostic results, giving it a relative advantage over other detection technologies. Similar to previous studies,26 Nanopore sequencing in this study required approximately 8 hours, significantly faster than Illumina sequencing (approximately 24 hours) and traditional detection techniques (24–72 hours). This indicates that Nanopore sequencing has a better advantage in early pathogen identification, thus streamlining the diagnostic process and guiding clinical adjustments to antibiotics.
In this study, there were indeed only 18 cases whose detected results were finally considered as the true positive microorganism. Among the remaining 11 patients, 8 patients had some low-sequence viruses detected, such as Cytomegalovirus and Epstein-Barr virus, as well as some low-sequence non-tuberculous mycobacteria. However, considering their imaging and laboratory results, these test results were deemed false positives. This might be because the pathogens are either part of the normal colonization or contaminants. And 3 patients had no pathogenic microorganism detected at all by three methods. As for why no pathogenic bacteria were detected, it could be due to false negative results. We considered the following factors: 1) The lesion was relatively minor, 2) antibiotics had been used for a long time before bronchoscopy, and 3) the correct lung subsegment might not be selected for lavage during the lavage operation.
Our research contains some limitations. First, this study is conducted using a single-center approach, and due to the limited sample size, there could be potential selection bias in the findings. Secondly, since only DNA sequencing was performed on all samples and not RNA sequencing, this might have led to some false-negative results. Third, given that nanopore sequencing found very few drug resistance genes, no subsequent analysis was undertaken. Fourth, unlike traditional microbial detection techniques, sequencing technology cannot provide drug sensitivity information for pathogens and carries higher risks of sample contamination or carryover. Moreover, when evaluating clinical applications, it is important to consider the costs of Nanopore and Illumina sequencing, since these rapid tests are notably more costly than traditional methods. Nevertheless, we conducted a prospective study employing advanced technologies, including Nanopore sequencing, in a precisely defined cohort of elderly patients with pneumonia. Furthermore, the superiority of Nanopore sequencing was confirmed through a comprehensive comparison of various detection methods. This technological advancement represents a significant step forward in the management of pneumonia, ensuring that patients receive targeted and appropriate care based on a comprehensive understanding of the infectious agents involved.
Conclusion
Compared to Illumina sequencing and traditional techniques, Nanopore sequencing demonstrates a higher consistency with the final comprehensive diagnosis in pathogen detection. Additionally, Nanopore sequencing offers a shorter turnaround time and may play a crucial role in rapidly and accurately identifying pathogens responsible for CAP in the elderly population. To fully evaluate the clinical benefits of nanopore sequencing in infection diagnosis and treatment, further large-sample, multi-center, and prospective studies are necessary.
Acknowledgments
We would like to thank all the patients for participating in this study.
Funding
This study was supported by the Science and Technology Project for the Development of Hangzhou Biomedical and Health Industry under Grant No. 2022WJC004, and Zhejiang Provincial Traditional Chinese Medicine Science and Technology Project under Grant No. 2023ZL123.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Berild JD, Winje BA, Vestrheim DF, et al. A Systematic Review of Studies Published between 2016 and 2019 on the Effectiveness and Efficacy of Pneumococcal Vaccination on Pneumonia and Invasive Pneumococcal Disease in an Elderly Population. Pathogens. 2020;9(4). doi:10.3390/pathogens9040259
2. Zhong P, Zhao Y, Cao Y, Chen C, Xie J, Chang C. Urban-Rural Disparity in Mortality Patterns of Respiratory Diseases Among Older Adults - China, 1987–2021. China CDC Wkly. 2023;5(50):1125–1130. doi:10.46234/ccdcw2023.210
3. Liu H, Xiao XC, Lu JY, Chen ZQ, Luo L, Yang ZC. Study on epidemic characteristics and etiology of community acquired pneumonia in Guangzhou from 2009 to 2012. Chin J Prev Med. 2013;47(12):1089–1094. PMID:24529265.
4. Jain S, Self WH, Wunderink RG, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med. 2015;373(5):415–427. doi:10.1056/NEJMoa1500245
5. Isturiz R, Grant L, Gray S, et al. Expanded Analysis of 20 Pneumococcal Serotypes Associated With Radiographically Confirmed Community-acquired Pneumonia in Hospitalized US Adults. Clin Infect Dis. 2021;73(7):1216–1222. doi:10.1093/cid/ciab375
6. Chongthanadon B, Thirawattanasoot N, Ruangsomboon O. Clinical factors associated with in-hospital mortality in elderly versus non-elderly pneumonia patients in the emergency department. BMC Pulm Med. 2023;23(1):330. doi:10.1186/s12890-023-02632-z
7. Liu Y, Qin S, Lan C, Huang Q, Zhang P, Cao W. Effectiveness of metagenomic next-generation sequencing in the diagnosis of infectious diseases: a systematic review and meta-analysis. Int J Infect Dis. 2024;142:106996. doi:10.1016/j.ijid.2024.106996
8. Rodino KG, Simner PJ. Status check: next-generation sequencing for infectious-disease diagnostics. J Clin Invest. 2024;134(4). doi:10.1172/JCI178003
9. Owaid HA, Al-Ouqaili MTS. Molecular and bacteriological investigations for the co-existence CRISPR/Cas system and beta-lactamases of types extended-spectrum and carbapenemases in Multidrug, extensive drug and Pandrug-Resistant Klebsiella pneumoniae. Saudi J Biol Sci. 2024;31(7):104022. doi:10.1016/j.sjbs.2024.104022
10. Peng JM, Du B, Qin HY, Wang Q, Shi Y. Metagenomic next-generation sequencing for the diagnosis of suspected pneumonia in immunocompromised patients. J Infect. 2021;82(4):22–27. doi:10.1016/j.jinf.2021.01.029
11. Wang Y, Zhao Y, Bollas A, Wang Y, Au KF. Nanopore sequencing technology, bioinformatics and applications. Nat Biotechnol. 2021;39(11):1348–1365. doi:10.1038/s41587-021-01108-x
12. Gu W, Deng X, Lee M, et al. Rapid pathogen detection by metagenomic next-generation sequencing of infected body fluids. Nat Med. 2021;27(1):115–124. doi:10.1038/s41591-020-1105-z
13. Cao B, Huang Y, She DY, et al. Diagnosis and treatment of community-acquired pneumonia in adults: 2016 clinical practice guidelines by the Chinese Thoracic Society, Chinese Medical Association. Clin Respir J. 2018;12(4):1320–1360. doi:10.1111/crj.12674
14. Wu X, Liang R, Xiao Y, et al. Application of targeted next generation sequencing technology in the diagnosis of Mycobacterium Tuberculosis and first line drugs resistance directly from cell-free DNA of bronchoalveolar lavage fluid. J Infect. 2023;86(4):399–401. doi:10.1016/j.jinf.2023.01.031
15. Chen H, Yin Y, Gao H, et al. Clinical Utility of In-house Metagenomic Next-generation Sequencing for the Diagnosis of Lower Respiratory Tract Infections and Analysis of the Host Immune Response. Clin Infect Dis. 2020;71(Suppl 4):S416–S426. doi:10.1093/cid/ciaa1516
16. Miao Q, Ma Y, Wang Q, et al. Microbiological Diagnostic Performance of Metagenomic Next-generation Sequencing When Applied to Clinical Practice. Clin Infect Dis. 2018;67(suppl_2):S231–S240. doi:10.1093/cid/ciy693
17. Qin F, Hu X, Wang X, et al. Utility of metagenomic Next-Generation Sequencing for simultaneously detecting pathogens and neoplasms. Heliyon. 2024;10(2):e24399. doi:10.1016/j.heliyon.2024.e24399
18. Patents. Nanopore sequencing. Nat Biotechnol. 2024;42(5):698. doi:10.1038/s41587-024-02231-1.
19. Zhang H, Shen D, Zhou J, et al. The Utility of Metagenomic Next-Generation Sequencing (mNGS) in the Management of Patients With Bronchiectasis: a Single-Center Retrospective Study of 93 Cases. Open Forum Infect Dis. 2023;10(8):ofad425. doi:10.1093/ofid/ofad425
20. Sayers EW, Beck J, Bolton EE, et al. Database resources of the National Center for Biotechnology Information. Nucleic Acids Res. 2024;52(D1):D33–D43. doi:10.1093/nar/gkad1044
21. Takazono T, Namie H, Nagayoshi Y, et al. Development of a score model to predict long-term prognosis after community-onset pneumonia in older patients. Respirology. 2024;29(8):722–730. doi:10.1111/resp.14752
22. Lin Q, Yao Y, Li X, et al. The application of nanopore targeted sequencing for pathogen diagnosis in bronchoalveolar lavage fluid of patients with pneumonia: a prospective multicenter study. Infect Dis. 2024;56(2):128–137. doi:10.1080/23744235.2023.2276785
23. Chen T, Zhang L, Huang W, et al. Detection of Pathogens and Antimicrobial Resistance Genes in Ventilator-Associated Pneumonia by Metagenomic Next-Generation Sequencing Approach. Infect Drug Resist. 2023;16:923–936. doi:10.2147/IDR.S397755
24. Zhang J, Gao L, Zhu C, et al. Clinical value of metagenomic next-generation sequencing by Illumina and Nanopore for the detection of pathogens in bronchoalveolar lavage fluid in suspected community-acquired pneumonia patients. Front Cell Infect Microbiol. 2022;12:1021320. doi:10.3389/fcimb.2022.1021320
25. Zhao X, Ge Y, Zhang Y, et al. Pathogen Diagnosis Value of Nanopore Sequencing in Severe Hospital-Acquired Pneumonia Patients. Infect Drug Resist. 2023;16:3293–3303. doi:10.2147/IDR.S410593
26. Ye J, Huang K, Xu Y, et al. Clinical application of nanopore-targeted sequencing technology in bronchoalveolar lavage fluid from patients with pulmonary infections. Microbiol Spectr. 2024;12(6):e0002624. doi:10.1128/spectrum.00026-24
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


