Back to Journals » Journal of Pain Research » Volume 18
Opioid-Free versus Opioid-Sparing Anesthesia for Postoperative Pain and Early Recovery After Laparoscopic Cholecystectomy: A Randomized Controlled Trial
Authors Xiong M, Liu Y, Liang Y, Wang H, Zhang L, Zhang Z, Fang M
Received 20 November 2024
Accepted for publication 9 April 2025
Published 23 April 2025 Volume 2025:18 Pages 2137—2146
DOI https://doi.org/10.2147/JPR.S506147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Miaomiao Xiong,1,* Yao Liu,2,* Yingsi Liang,1,* Hailang Wang,1 Lili Zhang,1 Zhongjun Zhang,1 Ming Fang2
1Department of Anesthesiology, Affiliated Hospital of Jiangnan University, Wuxi, People’s Republic of China; 2Department of Pain Management, Affiliated Hospital of Jiangnan University, Wuxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ming Fang, Department of Pain Management, Affiliated Hospital of Jiangnan University, 1000 hefeng Road, Binhu District, Wuxi, 214000, People’s Republic of China, Email [email protected] Zhongjun Zhang, Department of Anesthesiology, Affiliated Hospital of Jiangnan University, 1000 hefeng Road, Binhu District, Wuxi, 214000, People’s Republic of China, Email [email protected]
Purpose: Enhanced recovery after surgery emphasizes effective analgesia while minimal opioid use. Opioid-free anesthesia (OFA) and opioid-sparing anesthesia (OSA) have been shown to enhance recovery by reducing opioid-induced side effects. This study compared the efficacy of OFA and OSA in managing postoperative pain and recovery after laparoscopic cholecystectomy (LC).
Patients and Methods: A single-center, randomized controlled trial was conducted with 86 adults undergoing LC. Patients received either OSA (sufentanil/remifentanil) or OFA (no opioids). Both groups received propofol, esketamine, dexmedetomidine, and erector spinae plane block. The primary outcome was pain area under the curve (AUCVAS) within 36 hours postsurgery. Secondary outcomes included hemodynamics, recovery times and bowel function.
Results: Eighty-one patients (41 and 40 in the OFA and OSA groups, respectively) completed the study. The AUCVAS scores were similar between the OFA (7.3 ± 1.4) and OSA (6.9 ± 1.3) groups (P = 0.201), the difference in AUCVAS between the two groups was 0.384 (95% CI: − 0.296, 1.064), which was significantly below the preset noninferiority threshold of 1.0, demonstrating the noninferiority of OFA. While early pain scores within the first 12 hours postanesthesia care unit (PACU) discharge were slightly higher in the OFA group, but overall pain control was sufficient in both groups. The VAS scores from PACU discharge to 36 hours postoperatively, intraoperative hemodynamic variables, and the need for rescue analgesia were comparable. OFA patients experienced a faster bowel recovery (13.8 ± 2.4 vs 15.5 ± 2.3 hours, P = 0.002). Recovery times, postoperative QoR-40 scores, and patient satisfaction were similar between the groups.
Conclusion: OFA is noninferior to OSA in pain management and hemodynamic stability, with faster bowel recovery after LC.
Keywords: opioid-free anesthesia, opioid-sparing anesthesia, postoperative pain, laparoscopic cholecystectomy, randomized controlled trial
Introduction
Opioid analgesics are a cornerstone of general anesthesia; however, their use is associated with significant side effects, including postoperative nausea and vomiting (PONV), respiratory depression, dizziness, somnolence, constipation, and opioid-induced hyperalgesia and tolerance.1 In response to these challenges, considerable research has focused on opioid-sparing anesthesia (OSA) and opioid-free anesthesia (OFA), both of which utilize multimodal analgesia to enhance postoperative recovery by minimizing opioid-related adverse effects.2,3 OFA is an approach designed to eliminate the use of opioids entirely during the perioperative period by utilizing multimodal analgesia. This strategy combines various non-opioid agents, such as dexmedetomidine, esketamine, and local anesthetics, to provide effective analgesia, reduce inflammation, and minimize central sensitization.4,5 However, findings from various studies remain controversial, particularly regarding the efficacy of OFA.6
Some investigations suggest that OFA may lead to improved recovery outcomes, including reduced postoperative morphine consumption, lower incidence of PONV, and decreased episodes of oxygen desaturation compared with opioid-based anesthesia.7,8 Nevertheless, other studies reported that OFA is linked to prolonged postoperative sedation and extended stay in the postanesthesia care unit (PACU).9,10 These discrepancies largely stem from concerns regarding excessive dexmedetomidine dosage, which may contribute to prolonged sedation.
Dexmedetomidine, a highly selective alpha-2 adrenoceptor agonist, is recognized for its sedative and analgesic properties, making it a prominent alternative in opioid-sparing strategies.11,12 Esketamine, the S (+)-isomer of ketamine, theoretically offers enhanced analgesic effects with a reduced side effect profile compared to racemic ketamine.13,14 However, the analgesic efficacy of esketamine remains controversial, particularly in the laparoscopic surgical context.
Despite being considered a minimally invasive procedure, laparoscopic cholecystectomy (LC) is often accompanied by moderate-to-severe postoperative pain and PONV.15 Intraoperative opioid-sparing strategies, particularly those involving regional nerve blocks and adjunct medications, have been shown to decrease postoperative opioid consumption.16 Ultrasound-guided erector spinae plane (ESP) block has demonstrated greater efficacy in reducing postoperative analgesic requirements and pain scores than transversus abdominis plane block following LC.17 A recent randomized controlled trial further supported the analgesic benefits of ultrasound-guided ESP block, correlating with reduced opioid needs and improved respiratory function after LC.18
Therefore, the present study aimed to evaluate the efficacy of OFA versus OSA for postoperative acute pain and early recovery after LC. We hypothesized that OFA, incorporating an ultrasound-guided ESP block and intravenous dexmedetomidine in combination with esketamine and lidocaine, may provide an analgesic profile comparable to that of OSA while minimizing perioperative analgesic consumption and associated opioid-related adverse reactions.
Materials and Methods
Study Design and Ethics
This prospective, double-anonymized, randomized, parallel, controlled study, from 2022–10-01 to 2023–06-30, was conducted in compliance with the Helsinki Declaration to evaluate the efficacy and safety of OFA versus OSA for postoperative acute pain and early recovery after LC. The study protocol was reviewed and approved by the Ethics Committee of Affiliated Hospital of Jiangnan University (approval number: LS2022014) and registered in the China Clinical Trial Registry (Trial ID: ChiCTR2200064236).
Participants
Patients scheduled for LC at the Affiliated Hospital of Jiangnan University with American Society of Anesthesiology class I–II were included in the study. Written informed consent was obtained from all participants. Exclusion criteria were respiratory, cardiac, or hepatic insufficiency, coagulopathies, psychiatric diseases, allergy or incompatibilities with experimental drugs, a history of chronic pain or opioid abuse, and inability to complete pain evaluation.
Outcomes
The primary outcome was the area under the curve (AUC) of the visual analog scale (VAS) score (AUCVAS) within 36 hours after surgery. The AUCVAS is a method used to quantify the overall intensity of pain or symptom severity over a period of time, based on repeated measurements. Compared to VAS at a single time point, the AUC for VAS was used as an effective and intuitive measure for the pain evaluation. The function for calculating the AUCVAS is  . VAS1 and VAS2 are the VAS scores at consecutive points.
. VAS1 and VAS2 are the VAS scores at consecutive points.  is the time difference between the two consecutive points. The AUC VAS was calculated using GraphPad Prism 9.0 software. Secondary outcomes included mean arterial pressure (MAP) and heart rate before anesthesia induction (T0), after induction (T1), at tracheal intubation (T2), after nerve block (T3), at skin incision (T4), 1 minute after pneumoperitoneum (T5), 30 minutes after pneumoperitoneum (T6), and at the end of surgery (T7). Additional secondary outcomes included intraoperative propofol dosage, maximum postoperative pain VAS score, time to first rescue analgesia, number and dosage of rescue analgesia (parecoxib sodium) within 48 hours postoperatively, postoperative adverse effects (PONV, constipation, urinary retention, pruritus, and delirium) within 48 hours postoperatively, and quality of recovery assessed using the QoR-40 questionnaire at 24 hours postoperatively.
is the time difference between the two consecutive points. The AUC VAS was calculated using GraphPad Prism 9.0 software. Secondary outcomes included mean arterial pressure (MAP) and heart rate before anesthesia induction (T0), after induction (T1), at tracheal intubation (T2), after nerve block (T3), at skin incision (T4), 1 minute after pneumoperitoneum (T5), 30 minutes after pneumoperitoneum (T6), and at the end of surgery (T7). Additional secondary outcomes included intraoperative propofol dosage, maximum postoperative pain VAS score, time to first rescue analgesia, number and dosage of rescue analgesia (parecoxib sodium) within 48 hours postoperatively, postoperative adverse effects (PONV, constipation, urinary retention, pruritus, and delirium) within 48 hours postoperatively, and quality of recovery assessed using the QoR-40 questionnaire at 24 hours postoperatively.
QoR-40 evaluated postoperative recovery across five domains: emotional status (9 items), physical comfort (12 items), psychological support (7 items), physical independence (5 items), and pain (7 items). Each item is rated on a five-point Likert scale, with total scores ranging from 40 (worst recovery) to 200 (best recovery).19
Randomization and Blinding
Eligible patients were randomly assigned to either the OSA (sufentanil plus remifentanil) or OFA (no opioids) group using a computer-generated block randomization list. Randomization was performed by an investigator not involved in the study. Group assignments were stored in opaque sealed envelopes, and the anesthesiologist administering the anesthesia was blinded to postoperative data collection and analysis. Neither patients nor outcome assessors were aware of the group allocation.
Procedures
Prior to surgery, all patients were instructed concerning the use of VAS to assess pain. Upon arrival to the operating room, standard monitoring (electrocardiography, noninvasive blood pressure, heart rate, peripheral oxygen saturation, and nasopharyngeal temperature) was initiated. Intravenous access was established, and patients received bolus dexmedetomidine (0.6 ug/kg over 10 minutes).
Anesthesia induction included midazolam (0.05 mg/kg), etomidate (0.3 mg/kg), cisatracurium (0.15 mg/kg), and dexamethasone (0.1 mg/kg) for tracheal intubation. The OFA group received esketamine (0.3 mg/kg) and lidocaine (1.5 mg/kg), while the OSA group received esketamine (0.2 mg/kg) and sufentanil (0.1 ug/kg) as part of their induction regimen (Table S1).
All patients underwent bilateral ultrasound-guided ESP block at the T7 vertebral level (identified by body surface markers and marked on the skin) after induction. The patients were placed in the lateral position and sterilized routinely. A high-frequency linear ultrasound transducer was placed on the posterior median line of the spine to display the spinous process and moved parallel to the longitudinal parasagittal direction of the T7 vertebra. The needle was inserted using a caudal-to-cranial method. After confirming the correct needle tip position, 20 mL of 0.375% ropivacaine was injected into the intravesical plane between the erector spinae muscle and the transverse process. Another ESP block was performed on the contralateral side.
For anesthesia maintenance, the OFA group received continuous esketamine (0.3 mg/kg/h), while the OSA group received esketamine (0.15 mg/kg/h) and remifentanil (0.05–0.15 ug/kg/min) intravenously. Propofol (4–6 mg/kg/h) was administered in both groups to maintain a bispectral index score of 40–60, with MAP and heart rate within 20% of baseline. Cisatracurium was administered as needed for muscle relaxation. Mechanical ventilation was performed using a 60% oxygen-air mixture to maintain end-tidal CO2 of 30–35 mmHg. Ephedrine (6 mg) or urapidil (12.5 mg) was administered for MAP of < 60 or > 120 mmHg, respectively, and atropine (0.5 mg) was administered for heart rate of < 45 bpm.
All anesthetics were stopped during skin closure, and azasetron (10 mg) was administered to prevent PONV. Postoperative pain at the incision site was managed with 5 mL of 1% lidocaine. Tracheal extubation was performed once adequate spontaneous ventilation and muscle strength were restored, and patients were transferred to the PACU. Rescue analgesia (parecoxib sodium 40 mg) was provided if VAS ≥ 4 within 48 hours postoperatively. Metoclopramide (10 mg) was administered for antiemetic rescue.
Statistical Analyses
Based on a pilot study with five patients in each group, the mean ACUVAS of 7.34 and 6.25 for the OFA and OSA groups were observed, with a standard deviation (SD) of 1.3. Using a noninferiority threshold of 1.0, test level (α) of 0.025, power (1 − β) of 0.90, and 1:1 ratio of patients in the two groups, the required sample size for each group was estimated to be 37. With an expected dropout rate of 10%, a total of 82 patients were enrolled.
Statistical analyses were performed using SPSS 25.0 (IBM Corporation, Armonk, NY). Continuous data were tested for normality using the Shapiro–Wilk test. Normally distributed data are expressed as mean ± SD and were compared using the independent-sample t-test. Non-normally distributed data are expressed as median (interquartile range) and were analyzed using the Mann–Whitney rank sum test. Categorical data are expressed as number (%) and were compared using the chi-square test. Repeated-measures analysis of variance was used to compare the effects of MAP and HR between the groups after considering time and its interaction effects. A noninferiority test level (α) of 0.025 was applied, while for other tests, P < 0.05 was defined as statistically significant.
Results
Demographic Data
Ninety-four patients scheduled for LC under general anesthesia was screened. After excluding five patients who did not meet the inclusion criteria, three who refused to participate, two conversions to laparotomy, and three withdrawals of consent, 81 patients (41 in the OFA and 40 in the OSA group) completed the study (Figure 1).
 |
Figure 1 CONSORT patient enrolment diagram. Abbreviation: CONSORT, Consolidated Standards of Reporting Trials. |
The baseline demographic characteristics, surgical and anesthesia duration, and use of vasoactive agents were comparable between the two groups (Table 1).
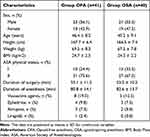 |
Table 1 Baseline Characteristics and Intraoperative Data |
Primary Outcome
The AUCVAS was 7.3 (± 1.4) in the OFA group vs 6.9 (± 1.3) in the OSA group, with no significant differences between the groups (P = 0.201) (Figure 2A). The difference in AUCVAS between the two groups was 0.384 (95% CI: −0.296, 1.064), which was significantly below the preset noninferiority threshold of 1.0, suggesting the noninferior analgesic efficacy of OFA compared to OSA. A slight elevation in VAS scores was observed within the first 12 hours after PACU discharge (Figure 2B) (secondary outcome).
 |
Figure 2 Area under curve (AUC) of Visual Analogue Scale (VAS) scores comparison between two groups (A) and at different time points after PACU discharge (B) (Group OFA, n=41; Group OSA, n=40). |
Secondary Outcomes
VAS scores from PACU discharge to 36 hours postoperatively were comparable between the groups, as were the maximum VAS scores (Figure 3A). The median VAS score at all time points was lower than the maximum postoperative VAS score of 3. Changes in MAP and HR from anesthesia induction to the end of surgery were also similar between the two groups (Figure 3B and C).
Seventeen patients in the OFA group and 14 in the OSA group required rescue analgesia with parecoxib sodium (P = 0.550) (Table 2). The time to first rescue analgesia was 7 hours postoperatively in both groups (Table 2). The awakening time, orientation recovery time, PACU stay duration, and postoperative hospital stay length were similar between the groups (P > 0.05). However, patients in the OSA group experienced a longer time to the first flatus compared to the OFA group (15.5 ± 2.3 vs 13.8 ± 2.4 hours, P = 0.002). Postoperative global QoR-40 and dimension scores (176.9 vs 178.4) and patient satisfaction scores for anesthesia (9 vs 9) were similar between the groups (P > 0.05).
 |
Table 2 Postoperative Analgesia-Related Variables and Recovery Quality |
Eleven adverse events occurred in the OFA group and nine in the OSA group. The reported events included PONV (6 in OFA vs 5 in OSA), constipation (3 vs 2), difficulty passing urine (1 vs 1), and pruritus (1 vs 1). POD (postoperative delirium) was not reported in either group (Table 3).
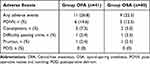 |
Table 3 Postoperative Adverse Events |
Discussion
In this single-center randomized controlled noninferiority trial, OFA using a multimodal analgesic approach with dexmedetomidine, esketamine, and ultrasound-guided ESP block was found to be noninferior to OSA in terms of analgesic effectiveness and intraoperative hemodynamic stability during LC. Importantly, OFA did not prolong awakening or orientation recovery time.
While the definition of “OFA” remains debated, its feasibility is increasingly recognized. Nevertheless, studies comparing OFA and traditional opioid anesthesia protocols continue to generate mixed results, leaving the optimal anesthetic regimen unclear.20 Multimodal analgesia, which aims to minimize opioid exposure while maintaining intraoperative stability, has emerged as a key strategy in addressing concerns over poorly controlled postoperative pain, potentially leading to long-term opioid use.21 In this study, dexmedetomidine, esketamine, and ultrasound-guided ESP block were used to ensure adequate analgesia for patients undergoing LC.
The AUC is precise and reliable for analyzing continuous variables.9 Our study showed comparable AUCVAS and postoperative analgesic requirement within 36 hours after surgery between the two groups, indicating the sufficient analgesic effect of the OFA protocol. Hemodynamic parameters, including MAP and HR, were stable in both groups, and no patient in the OFA group required conversion to opioid-inclusive anesthesia, highlighting the safety and feasibility of OFA.
Frauenknecht et al conducted a meta-analysis of 23 randomized controlled trials and concluded that OFA provided comparable analgesia to opioid-inclusive protocols, with a significantly reduced incidence of PONV.22 However, variations in populations and techniques raise questions regarding the optimal combination and dosing of adjuncts in multimodal anesthesia. Similarly, Beloeil et al prematurely terminated their study owing to severe bradycardia associated with high-dose dexmedetomidine, indicating that dosage management is critical in OFA protocols.23
Previous studies have reported conflicting outcomes regarding the effects of dexmedetomidine in OFA, particularly concerning sedation.24,25 While some studies noted faster extubation and improved recovery quality, others, such as that by Chen et al in a randomized controlled trial, reported prolonged awakening times despite a reduction in PONV.9 Similarly, significantly prolonged postoperative sedation associated with dexmedetomidine-inclusive anesthesia in patients undergoing lumpectomy has also been reported.10 Moreover, the incidence of postoperative sedation was reported to be nearly four times higher in patients receiving OFA, leading to a significantly longer PACU stay.26 Indeed, this undesired outcome is highly associated with the administration of dexmedetomidine.27–29 These discrepancies likely stem from variations in how dexmedetomidine was administered (e.g., intermittent boluses rather than continuous infusion), which could explain the comparable awakening and recovery times observed between the OFA and OSA groups. Notably, no severe bradycardia or hypoxemia occurred in either group.
The use of dexmedetomidine in opioid-free balanced anesthesia can provide adequate analgesia and intraoperative hemodynamic stability, which are typically achieved with opioids. However, the optimal dexmedetomidine dose for achieving this effect with minimal side effects has not been established, as dosages vary significantly across studies.12 To minimize its impact on awakening and orientation recovery times, we administered a bolus of dexmedetomidine (0.6 ug/kg over 10 minutes) before anesthesia induction without continuing its infusion intraoperatively. This approach resulted in the lack of significant differences between the groups in terms of awakening and orientation recovery times, which may be attributed to the lack of continuous intraoperative dexmedetomidine use. Additionally, because this study involved minimally invasive LC, a procedure associated with shorter recovery times, these findings should be interpreted with caution.
Previous research has shown that OFA may reduce PONV incidence compared to traditional opioid-based anesthesia;9,10,30 however, in our study, both the OFA and OSA groups exhibited a low PONV incidence, with no significant difference between the groups. This could be reflective of the benefits of the Enhanced Recovery After Surgery (ERAS) protocol, which is known to reduce PONV risk across board.
In addition to the dexmedetomidine bolus, our OFA protocol included intraoperative esketamine and ultrasound-guided ESP block, providing long-lasting analgesia in both the OSA and OFA groups. Consistent with previous findings, esketamine was used as an adjunct in OFA to enhance analgesia without prolonging awakening or orientation recovery time in minimally invasive surgery.31,32 Postoperative pain outcomes, including the time to first remedial analgesia and the number of analgesics administered within 48 hours postoperatively, were similar between the two groups. Notably, the OFA group had a shorter time to the first flatus, which may be due to the absence of perioperative opioids. Furthermore, no differences were observed between the groups regarding intraoperative hemodynamics or the use of vasoactive agents, suggesting that OFA provides comparable intraoperative anesthesia stability to OSA.
Limitations
This study had several limitations. First, the selected surgery (LC) has a relatively low surgical risk, and our patients were in their 40s on average. Future multicenter studies involving older patients and a broader range of surgeries with varying levels of complexity are needed to generalize the findings of OFA more comprehensively. Second, as all patients received intraoperative esketamine as part of the ERAS protocol, we did not compare the incidence of esketamine-related side effects, such as itching, mental confusion, and nightmares, between the groups. Although esketamine is considered safe in minimally invasive surgeries, its dose-dependent effects should be closely monitored. Lastly, although previous studies have demonstrated reduced PONV with OFA, we found no significant difference between groups in this study. This could be due to the low baseline PONV risk in our patients, as well as the sample size, which was calculated based on the primary outcome (AUCVAS) and may have been insufficient to detect differences in PONV.
Conclusion
This study, including one of the largest participants to date, demonstrated that under the ERAS protocol, multimodal OFA is as feasible and safe as OSA for LC. OFA may offer additional benefits, such as faster recovery of intestinal function without extending awakening or orientation recovery time.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Disclosure
Miaomiao Xiong, Yao Liu and Yingsi Liang are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Yayla A, Eskici Ilgin V, Kılınç T, Karaman Özlü Z, Ejder Apay S. Nausea and vomiting after laparoscopic cholecystectomy: analysis of predictive factors. J Perianesth Nurs. 2022;37(6):834–841. doi:10.1016/j.jopan.2022.01.002
2. Shanthanna H, Joshi GP. Opioid-free general anesthesia: considerations, techniques, and limitations. Curr Opin Anaesthesiol. 2024;37(4):384–390. doi:10.1097/ACO.0000000000001385
3. Jipa M, Isac S, Klimko A, et al. Opioid-sparing analgesia impacts the perioperative anesthetic management in major abdominal surgery. Medicina. 2022;58(4). doi:10.3390/medicina58040487.
4. Kharasch ED, Clark JD. Opioid-free anesthesia: time to regain our balance. Anesthesiology. 2021;134(4):509–514. doi:10.1097/ALN.0000000000003705
5. Adams TJ, Aljohani DM, Forget P. Perioperative opioids: a narrative review contextualising new avenues to improve prescribing. Br J Anaesth. 2023;130(6):709–718. doi:10.1016/j.bja.2023.02.037
6. Toleska M, Dimitrovski A. Is opioid-free general anesthesia more superior for postoperative pain versus opioid general anesthesia in laparoscopic cholecystectomy? Pril. 2019;40(2):81–87. doi:10.2478/prilozi-2019-0018
7. Bugada D, Lorini LF, Lavand’homme P. Opioid free anesthesia: evidence for short and long-term outcome. Minerva Anestesiol. 2021;87(2):230–237. doi:10.23736/S0375-9393.20.14515-2
8. Yu JM, Tao QY, He Y, Liu D, Niu JY, Zhang Y. Opioid-free anesthesia for pain relief after laparoscopic cholecystectomy: a prospective randomized controlled trial. J Pain Res. 2023;16:3625–3632. doi:10.2147/JPR.S432601
9. Chen L, He W, Liu X, Lv F, Li Y. Application of opioid-free general anesthesia for gynecological laparoscopic surgery under ERAS protocol: a non-inferiority randomized controlled trial. BMC Anesthesiol. 2023;23(1):34. doi:10.1186/s12871-023-01994-5
10. Qian XL, Li P, Chen YJ, Xu SQ, Wang X, Feng SW. Opioid free total intravenous anesthesia with dexmedetomidine-esketamine-lidocaine for patients undergoing lumpectomy. J Clin Med Res. 2023;15(8–9):415–422. doi:10.14740/jocmr5000
11. Piao G, Wu J. Systematic assessment of dexmedetomidine as an anesthetic agent: a meta-analysis of randomized controlled trials. Arch Med Sci. 2014;10(1):19–24. doi:10.5114/aoms.2014.40730
12. Grape S, Kirkham KR, Frauenknecht J, Albrecht E. Intra-operative analgesia with remifentanil vs. dexmedetomidine: a systematic review and meta-analysis with trial sequential analysis. Anaesthesia. 2019;74(6):793–800. doi:10.1111/anae.14657
13. Eberl S, Koers L, van Hooft J, et al. The effectiveness of a low-dose esketamine versus an alfentanil adjunct to propofol sedation during endoscopic retrograde cholangiopancreatography: a randomised controlled multicentre trial. Eur J Anaesthesiol. 2020;37(5):394–401. doi:10.1097/EJA.0000000000001134
14. Kumar K, Kirksey MA, Duong S, Wu CL. A review of opioid-sparing modalities in perioperative pain management: methods to decrease opioid use postoperatively. Anesth Analg. 2017;125(5):1749–1760. doi:10.1213/ANE.0000000000002497
15. Bisgaard T, Warltier D. Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology. 2006;104(4):835–846. doi:10.1097/00000542-200604000-00030
16. Liu Z, Bi C, Li X, Song R. The efficacy and safety of opioid-free anesthesia combined with ultrasound-guided intermediate cervical plexus block vs. opioid-based anesthesia in thyroid surgery-a randomized controlled trial. J Anesth. 2023;37(6):914–922. doi:10.1007/s00540-023-03254-9
17. Altıparmak B, Korkmaz Toker M, Uysal AI, Kuşçu Y, Gümüş Demirbilek S. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: randomized, controlled trial. J Clin Anesth. 2019;57:31–36. doi:10.1016/j.jclinane.2019.03.012
18. Yildiz M, Kozanhan B, Iyisoy MS, Canıtez A, Aksoy N, Eryigit A. The effect of erector spinae plane block on postoperative analgesia and respiratory function in patients undergoing laparoscopic cholecystectomy: a double-blind randomized controlled trial. J Clin Anesth. 2021;74:110403. doi:10.1016/j.jclinane.2021.110403
19. Myles PS, Weitkamp B, Jones K, Melick J, Hensen S. Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br J Anaesth. 2000;84(1):11–15. doi:10.1093/oxfordjournals.bja.a013366
20. Veyckemans F. Opioid-free anaesthesia: still a debate? Eur J Anaesthesiol. 2019;36(4):245–246. doi:10.1097/EJA.0000000000000964
21. Pirie K, Traer E, Finniss D, Myles PS, Riedel B. Current approaches to acute postoperative pain management after major abdominal surgery: a narrative review and future directions. Br J Anaesth. 2022;129(3):378–393. doi:10.1016/j.bja.2022.05.029
22. Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E. Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 2019;74(5):651–662. doi:10.1111/anae.14582
23. Beloeil H, Garot M, Lebuffe G, et al. Balanced opioid-free anesthesia with dexmedetomidine versus balanced anesthesia with remifentanil for major or intermediate noncardiac surgery. Anesthesiology. 2021;134(4):541–551. doi:10.1097/ALN.0000000000003725
24. Feld JM, Hoffman WE, Stechert MM, Hoffman IW, Ananda RC. Fentanyl or dexmedetomidine combined with desflurane for bariatric surgery. J Clin Anesth. 2006;18(1):24–28. doi:10.1016/j.jclinane.2005.05.009
25. Hao C, Xu H, Du J, et al. Impact of opioid-free anesthesia on postoperative quality of recovery in patients after laparoscopic cholecystectomy-a randomized controlled trial. Drug Des Devel Ther. 2023;17:3539–3547. doi:10.2147/DDDT.S439674
26. Massoth C, Schwellenbach J, Saadat-Gilani K, et al. Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy - A randomised controlled trial. J Clin Anesth. 2021;75:110437. doi:10.1016/j.jclinane.2021.110437
27. Edokpolo LU, Mastriano DJ, Serafin J, Weedon JC, Siddiqui MT, Dimaculangan DP. Discharge readiness after propofol with or without dexmedetomidine for colonoscopy: a randomized controlled trial. Anesthesiology. 2019;131(2):279–286. doi:10.1097/ALN.0000000000002809
28. Demiri M, Antunes T, Fletcher D, Martinez V. Perioperative adverse events attributed to α2-adrenoceptor agonists in patients not at risk of cardiovascular events: systematic review and meta-analysis. Br J Anaesth. 2019;123(6):795–807. doi:10.1016/j.bja.2019.07.029
29. Olutoye OA, Glover CD, Diefenderfer JW, et al. The effect of intraoperative dexmedetomidine on postoperative analgesia and sedation in pediatric patients undergoing tonsillectomy and adenoidectomy. Anesth Analg. 2010;111(2):490–495. doi:10.1213/ANE.0b013e3181e33429
30. Feng CD, Xu Y, Chen S, et al. Opioid-free anaesthesia reduces postoperative nausea and vomiting after thoracoscopic lung resection: a randomised controlled trial. Br J Anaesth. 2024;132(2):267–276. doi:10.1016/j.bja.2023.11.008
31. Hu Y, Zhang QY, Qin GC, et al. Balanced opioid-free anesthesia with lidocaine and esketamine versus balanced anesthesia with sufentanil for gynecological endoscopic surgery: a randomized controlled trial. Sci Rep. 2024;14(1):11759. doi:10.1038/s41598-024-62824-3
32. Liu J, Yin J, Yin J, et al. Effect of esketamine-based opioid-sparing anesthesia strategy on postoperative pain and recovery quality in patients undergoing total laparoscopic hysterectomy: a randomized controlled trail. Heliyon. 2024;10(3):e24941. doi:10.1016/j.heliyon.2024.e24941
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


