Back to Journals » Journal of Pain Research » Volume 18
Outcomes Of Intraarticular Corticosteroid Injections into the Cervical Facet Joint Based on Single-Photon Emission Computed Tomography Imaging
Received 15 February 2025
Accepted for publication 4 May 2025
Published 14 May 2025 Volume 2025:18 Pages 2453—2458
DOI https://doi.org/10.2147/JPR.S522930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Andrea Tinnirello
Seoyon Yang,1 Min Cheol Chang2
1Department of Rehabilitation Medicine, School of Medicine, Ewha Woman’s University Seoul Hospital, Seoul, South Korea; 2Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, Taegu, South Korea
Correspondence: Min Cheol Chang, Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, 317-1, Daemyungdong, Namku, Daegu, 705-717, South Korea, Tel +82-53-620-4682, Email [email protected]
Purpose: Chronic neck pain is a prevalent condition that significantly impairs quality of life and contributes to disability. The cervical facet joint (CFJ) is a common source of neck pain, and intraarticular (IA) corticosteroid injections are widely utilized for symptom relief. However, accurately predicting treatment outcomes remains challenging. This study aimed to evaluate the utility of bone single-photon emission computed tomography (SPECT) in predicting the therapeutic response to IA corticosteroid injections in patients with CFJ-origin neck pain.
Patients and Methods: A retrospective analysis was conducted on 102 patients who underwent IA CFJ corticosteroid injections between March 2010 and December 2020. Patients were stratified into two groups based on bone SPECT findings: those with increased CFJ radiotracer uptake (SPECT+ group, n=60) and those without (SPECT− group, n=42). Pain intensity was assessed using the numeric rating scale (NRS) before treatment and at the 1-month follow-up. Treatment success was defined as a ≥ 50% reduction in NRS scores. Statistical analyses were performed to compare outcomes between groups.
Results: Both the SPECT+ and SPECT− groups exhibited significant pain reduction following IA corticosteroid injection (P < 0.001 for both groups). However, the SPECT+ group demonstrated significantly greater pain relief compared to the SPECT− group at the 1-month follow-up (P = 0.007). Furthermore, the treatment success rate was significantly higher in the SPECT+ group (63.3%) than in the SPECT− group (38.1%) (P = 0.012).
Conclusion: Bone SPECT is a valuable imaging modality for predicting the therapeutic efficacy of IA corticosteroid injections in patients with CFJ-origin neck pain. The findings suggest that increased CFJ radiotracer uptake is associated with a greater likelihood of achieving significant pain relief, underscoring the potential role of inflammation in treatment response.
Keywords: chronic pain, neck pain, zygapophyseal joint, single photon emission computed tomography computed tomography, steroids
Introduction
Chronic neck pain is among the most prevalent clinical complaints in patients presenting to pain clinics.1 It significantly impairs quality of life and is a leading cause of disability.1 The cervical facet joint (CFJ) is frequently implicated in persistent neck pain, accounting for approximately 50% of cases of chronic neck pain.2 Mechanical stress and inflammatory processes affecting the CFJ contribute to axial neck pain.3
A variety of treatment modalities, including oral analgesics, physical therapy, and interventional procedures, are employed to manage CFJ-related neck pain.3–7 Among these, intraarticular (IA) corticosteroid injection is widely utilized due to its potent anti-inflammatory effects and substantial pain-relieving properties.3 Although the number of studies on the effect of IA corticosteroid injection is limited, its pain-relieving effect has been reported to potentially last for up to 2 to 6 months and is being widely used in current clinical practice.3,8,9 Predicting the therapeutic response to IA corticosteroid injection is essential for optimizing patient management. As corticosteroids exert their effects primarily through anti-inflammatory mechanisms, patients with significant CFJ inflammation are expected to experience greater pain relief than those without substantial inflammatory involvement.10,11
Conventional imaging modalities, such as radiography, computed tomography (CT), and magnetic resonance imaging (MRI), are useful for detecting anatomical changes.12 However, these techniques have limited utility in identifying inflammation within or surrounding the CFJ.12 CT is primarily used to evaluate osseous structures and lacks sensitivity for detecting active inflammation. MRI cannot detect low-grade synovial inflammation or early inflammatory changes without overt structural abnormalities. Therefore, they are inadequate for predicting the therapeutic response to IA corticosteroid injection. Additionally, degenerative and other anatomical changes in the CFJ do not necessarily correlate with pain generation, reducing their usefulness in localizing pain sources in CFJ-related neck pain.13
Conversely, bone single-photon emission computed tomography (SPECT) imaging enables the identification of metabolically active regions associated with inflammation.14 Bone tracers preferentially accumulate in areas of increased bone remodeling and perfusion, facilitating the detection of sites of pain and inflammation within the CFJ.14,15 Thus, bone SPECT may serve as a valuable tool for predicting the therapeutic response to IA corticosteroid injection by assessing inflammation within or around the CFJ. We hypothesized that patients with increased radiotracer uptake on bone SPECT, indicating active inflammation, would experience a greater therapeutic response to IA corticosteroid injection than those without such uptake.
In this study, we evaluated the therapeutic outcomes of IA corticosteroid injection in patients with CFJ-related neck pain, stratified according to the presence of increased CFJ uptake on bone SPECT imaging.
Materials and Methods
Patients
This retrospective study was conducted at a single university hospital and included patients who underwent IA CFJ corticosteroid injections for the management of CFJ-origin neck pain between March 2010 and December 2020. The inclusion criteria were as follows:
- Age between 20 and 80 years.
- Undergoing bone SPECT prior to IA CFJ corticosteroid injection to assess potential increased radiotracer uptake in the CFJ.
- Persistent axial neck pain for at least three months preceding IA corticosteroid injection.
- ≥ 50% temporary pain relief following a diagnostic block with IA injection of 0.3 mL of 2% lidocaine.
- Baseline numeric rating scale (NRS) pain score of ≥3 (NRS: 0 = no pain, 10 = worst pain imaginable).
- Availability of follow-up evaluation at one month post-IA corticosteroid injection.
Exclusion criteria included the presence of systemic infections, coagulopathy, contrast media allergies, or rheumatic disorders. The study was approved by the Institutional Review Board of Yeungnam University Hospital. The requirement for informed consent was waived by the institutional review board of Yeungnam University Hospital owing to the retrospective nature of the study. The study was conducted in accordance with the Declaration of Helsinki. All patient data were anonymized and handled with strict confidentiality to ensure privacy and data protection.
Bone Single-Photon Emission Computed Tomography
SPECT imaging was performed approximately three hours following intravenous administration of 740 MBq technetium-99m methylene diphosphonate. Image acquisition was conducted using a dual-headed SPECT system (Hawkeye; GE Healthcare, Milwaukee, WI, USA) equipped with low-energy high-resolution collimation. The energy window was centered at 140 keV with a 20% range. The imaging protocol employed a step-and-shoot acquisition method with 3° intervals over a 180° arc and a 30-second acquisition time per stop. Image reconstruction was performed using an iterative ordered subset expectation maximization (OSEM) algorithm with two iterations and ten subsets in a 64×64 matrix. Scatter and attenuation correction were not applied. SPECT images were independently reviewed in a blinded manner by a nuclear medicine specialist with over 15 years of experience, who assessed CFJ radiotracer uptake without having information on the patients’ treatment outcomes (Figure 1).
Intraarticular Corticosteroid Injection
For IA corticosteroid injection, a posterior approach was employed with the patient in the prone position under C-arm fluoroscopy (Siemens). The patient’s upper body was supported by two pillows to maintain neck flexion, and the head was rotated 60–90° away from the injection site. The C-arm tube was then adjusted cephalad until proper alignment with the CFJ space was achieved. Intraarticular access was confirmed by the administration of a 0.3 mL contrast injection. Subsequently, a 26-gauge, 90-mm spinal needle was used to deliver 10 mg (0.25 mL) of triamcinolone acetonide in combination with 0.25 mL of 0.125% bupivacaine.
In patients exhibiting increased CFJ radiotracer uptake on bone SPECT (SPECT+ group), IA CFJ corticosteroid injections were administered directly into the CFJs demonstrating increased radiotracer uptake. In contrast, for patients without increased CFJ radiotracer uptake (SPECT− group), CFJs for IA corticosteroid injection were selected based on the distribution of pain, findings from physical examination (eg, localized tenderness), and evidence of degenerative CFJ pathology (osteophytes, bone sclerosis, or joint effusion) identified on radiographs or MRI. Throughout the follow-up period, no additional interventional pain management procedures were performed.
Outcome Measurements
Pain intensity was assessed using the NRS both prior to the injection and at the 1-month follow-up. A reduction of ≥50% in the NRS score was defined as a successful treatment outcome. The assessment of outcomes was conducted via retrospective review of patient medical records.
Statistical Analysis
Statistical analyses were conducted using SPSS 26.0. To assess data normality, Kolmogorov–Smirnov tests were performed prior to each analysis, revealing that all data were non-normally distributed. Comparisons between the SPECT+ and SPECT− groups were conducted using the Mann–Whitney U-test for continuous variables and the chi-square test for categorical variables. Changes in NRS scores within each group were analyzed using the Wilcoxon signed-rank test. A significance threshold of P < 0.05 was applied.
Results
A total of 102 patients were recruited for this study. Of these, 60 patients exhibited increased radiotracer uptake at the CFJ on bone SPECT (SPECT+ group), while 42 patients demonstrated no increased uptake (SPECT− group).
There were no significant differences between the SPECT+ and SPECT− groups in terms of sex distribution, age, pain vector, or pain duration (Mann–Whitney U-test and chi-square test, P > 0.05) (Table 1). These results suggest that the included patients were relatively homogenous in terms of baseline demographic and clinical characteristics, allowing a reliable comparison of treatment outcomes between the SPECT+ and SPECT- groups. The mean number of injected CFJs was 2.8 ± 1.3 in the SPECT+ group and 3.2 ± 1.6 in the SPECT− group, with no statistically significant difference between the groups (P = 0.310). Additionally, the NRS scores prior to treatment were comparable between the SPECT+ and SPECT− groups (P = 0.466).
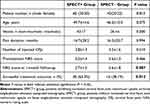 |
Table 1 Intergroup Comparison Between SPECT+ and SPECT− Groups |
In the intragroup comparison following IA corticosteroid injection, NRS scores were significantly reduced in both the SPECT+ and SPECT− groups compared to baseline (Wilcoxon signed-rank test, SPECT+ group: P < 0.001; SPECT− group: P < 0.001). In the intergroup comparison, NRS scores at one month post-treatment were significantly lower in the SPECT+ group than in the SPECT− group (P = 0.007) (Table 1). Furthermore, 38 of the 60 patients (63.3%) in the SPECT+ group achieved a successful treatment outcome, compared to 16 of the 42 patients (38.1%) in the SPECT− group. The proportion of patients with successful treatment outcomes was significantly higher in the SPECT+ group than in the SPECT− group (chi-square test, P = 0.012).
Discussion
In this study, we found that neck pain was significantly reduced in both the SPECT+ and SPECT− groups, irrespective of the presence or absence of CFJ radiotracer uptake on bone SPECT. However, patients with increased CFJ radiotracer uptake on bone SPECT (SPECT+ group) exhibited significantly greater pain reduction than those without increased uptake (SPECT− group), supporting the hypothesis that inflammation is a key determinant of the efficacy of IA corticosteroid injections. These findings highlight the potential role of SPECT imaging in predicting treatment outcomes for IA corticosteroid injections in patients with CFJ-origin neck pain.
The observed difference in treatment response between the SPECT+ and SPECT− groups is consistent with the mechanism of corticosteroids, which exert their therapeutic effects primarily through anti-inflammatory pathways.16 Patients in the SPECT+ group likely had more pronounced inflammation within or surrounding the CFJ, leading to greater pain relief following corticosteroid injection. In contrast, the SPECT− group likely included patients whose neck pain originated from structural degeneration or injury rather than active inflammation, resulting in a less pronounced response to corticosteroid therapy.
In addition, although our patients’ pain persisted for at least three months, the presence of increased radiotracer uptake on bone SPECT suggests that active inflammation may persist beyond the subacute phase. This finding is consistent with previous studies indicating that chronic CFJ pain may involve sustained inflammatory processes, which can be detected using SPECT.12,14
Our findings align with previous research on the utility of bone SPECT in identifying pain-generating joints.15,17,18 Prior studies have reported that increased radiotracer uptake on bone SPECT correlates with active inflammation, which appears to be a crucial factor associated with a favorable response to corticosteroid injections.15,17,18 The present study provides additional evidence supporting the use of SPECT as a diagnostic tool for patient selection in IA corticosteroid therapy, ultimately enhancing treatment efficiency and minimizing unnecessary procedures. Our findings have useful clinical implications, suggesting that bone SPECT can serve as a practical and objective tool for guiding patient selection for IA corticosteroid injection. By identifying patients who are more likely to benefit from the procedure, clinicians may improve treatment efficacy in managing CFJ-related neck pain.
Furthermore, the success rate of IA corticosteroid injections was significantly higher in the SPECT+ group compared to the SPECT− group, suggesting that SPECT imaging can facilitate the optimization of treatment strategies by identifying patients most likely to benefit from targeted corticosteroid therapy. Integrating SPECT into the diagnostic workflow could contribute to more personalized pain management approaches and improved clinical outcomes.
The utility of SPECT in the diagnosis and management of CFJ-origin neck pain remains a subject of debate.18,19 In 2022, Nolan et al investigated the predictive value of SPECT in identifying pain sources for targeted interventions in patients with CFJ-origin neck pain.18 Their retrospective analysis of 112 patients demonstrated that interventions, including cervical medial branch block (MBB) and IA corticosteroid injection, at CFJs exhibiting increased radiotracer uptake were significantly associated with greater pain relief at 1 day post-intervention compared to interventions at CFJs without increased radiotracer uptake. However, Nolan et al did not employ a standardized intervention protocol across all patients; rather, they combined MBB and IA corticosteroid injections without a clearly defined rationale. Additionally, their follow-up period for assessing treatment outcomes was extremely short, limiting the robustness of their conclusions. More recently, in 2024, Scholten et al conducted a retrospective study to determine whether increased radiotracer uptake on SPECT correlates with a positive response to cervical MBB.19 Analyzing a total of 43 procedures, they found no statistically significant association between increased SPECT uptake and achieving 50% or 80% pain relief following MBB. Based on these findings, the authors concluded that SPECT alone is not a reliable predictor of MBB outcomes. However, the small sample size (limited to 43 procedures) may restrict the generalizability of their results. Our study, similar to that of Nolan et al, provides evidence supporting the utility of SPECT in diagnosing the pain source in CFJ-origin neck pain and predicting treatment outcomes. Unlike previous studies that used heterogenous intervention protocols or cervical MBB, our study focused solely on the outcomes of IA corticosteroid injection based on SPECT findings.
Nevertheless, some limitations should be acknowledged. First, the retrospective nature of this study may introduce selection bias. Second, the follow-up period was limited to one month, precluding an assessment of long-term treatment efficacy. Third, we did not conduct a sample size calculation before the start of this study. Future prospective studies with larger sample sizes and longer follow-up periods are warranted to validate the usefulness of SPECT for managing CFJ-related neck pain. Additionally, studies on the effects of MBB or radiofrequency ablation based on SPECT findings are recommended to develop better personalized pain management strategies using SPECT.
In conclusion, our study underscores the clinical utility of bone SPECT in predicting therapeutic responses to IA corticosteroid injections in patients with CFJ-origin neck pain. The integration of SPECT imaging into clinical practice may facilitate the identification of suitable candidates for IA corticosteroid injection and contribute to the development of more effective, individualized treatment strategies.
Funding
This work was supported by the National Research Foundation of Korea grant funded by the Korean government (MSIT) (no. RS-2023-00219725).
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Kazeminasab S, Nejadghaderi SA, Amiri P. et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. doi:10.1186/s12891-021-04957-4
2. Hellinga MD, van Eerd M, Stojanovic MP, et al. 7. cervical facet pain: degenerative alterations and whiplash-associated disorder. Pain Pract. 2025;25(2):e70005. doi:10.1111/papr.70005
3. Lim JW, Cho YW, Lee DG, Chang MC. Comparison of intraarticular pulsed radiofrequency and intraarticular corticosteroid injection for management of cervical facet joint pain. Pain Physician. 2017;20(6):E961–967.
4. Ceylan İ, Canlı M, Kuzu Ş, et al. The effectiveness of two different treatment approaches in individuals with chronic non-specific neck pain: a randomized control trial. Turk J Health S. 2023;4(2):56–62.
5. Hurley RW, Adams MCB, Barad M, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Pain Med. 2021;22(11):2443–2524. doi:10.1093/pm/pnab281
6. Kocaman H, Yıldız NT, Canlı M, Alkan H. Comparison of the effects of mulligan mobilization technique combined with cervical stabilization exercises with the effects of cervical stabilization exercises with the effects of cervical stabilization exercises alone in chronic neck pain: randomized controlled study. Karya J Health Sci. 2023;4:227–234.
7. van Eerd M, Patijn J, Lataster A, et al. 5. Cervical facet pain. Pain Pract. 2010;10(2):113–123. doi:10.1111/j.1533-2500.2009.00346.x
8. Appeadu M, Miranda-Cantellops N, Mays B, et al. The effectiveness of intraarticular cervical facet steroid injections in the treatment of cervicogenic headache: systematic review and meta-analysis. Pain Physician. 2022;25(6):459–470.
9. Yang S, Chang MC. The effectiveness of corticosteroid injection into cervical facet joint for managing whiplash-related neck pain. Ann Palliat Med. 2022;11(8):2569–2573. doi:10.21037/apm-22-224
10. Hodgens A, Sharman T. Corticosteroids. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Available from: https://www.ncbi.nlm.nih.gov/books/NBK554612/.
11. Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids--new mechanisms for old drugs. N Engl J Med. 2005;353(16):1711–1723. doi:10.1056/NEJMra050541
12. Koppula BR, Morton KA, Al-Dulaimi R, Fine GC, Damme NM, Brown RKJ. SPECT/CT in the evaluation of suspected skeletal pathology. Tomography. 2021;7(4):581–605. doi:10.3390/tomography7040050
13. Yoo YM, Kim KH. Facet joint disorders: from diagnosis to treatment. Korean J Pain. 2024;37:3–12. doi:10.3344/kjp.23228
14. Saha S, Burke C, Desai A, Vijayanathan S, Gnanasegaran G. Gnanasegaran G. SPECT-CT: applications in musculoskeletal radiology. Br J Radiol. 2013;86(1031):20120519. doi:10.1259/bjr.20120519
15. Chang MC, Yang S. Short-term outcomes of intraarticular corticosteroid injection into the lumbar facet joint according to the findings of single-photon emission computed tomography imaging. J Pain Res. 2024;17:2357–2362. doi:10.2147/JPR.S467549
16. Claman HN. Glucocorticosteroids I: anti-inflammatory mechanisms. Hosp Pract. 1983;18(7):123–126,131–134. doi:10.1080/21548331.1983.11702591
17. Kong E, Boudier-Revéret M, Chang MC. The outcomes of intra-articular corticosteroid injection into sacroiliac joint following findings of single-photon emission computed tomography imaging: a retrospective case series. Pain Med. 2023;24(8):1017–1019. doi:10.1093/pm/pnad027
18. Nolan JE 3rd, Sundet AD, Kagan BD, Lake TJ, Krag MH, Lunardini DJ. The positive prediction of single photon emission computed tomography/ computed tomography (SPECT/CT) in the outcome of intervention for cervical facet pain. Spine J. 2022;22(10):1622–1627. doi:10.1016/j.spinee.2022.04.021
19. Scholten P, Sheikh M, Atchison J, et al. Correlating SPECT-CT activity in cervical facet joints with positive response to cervical medial branch blocks. Interv Pain Med. 2024;3(1):100393. doi:10.1016/j.inpm.2024.100393
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


