Back to Journals » Drug Design, Development and Therapy » Volume 19
Oxycodone vs the Combination of Fentanyl and Remifentanil for General Anesthesia in Laparoscopic Uterine Myomas Surgery: A Prospective, Randomized, Controlled Study
Authors Xu X, Zhang H , Li J , Zhou L , Zhu S , Bao F
Received 21 February 2025
Accepted for publication 29 May 2025
Published 9 June 2025 Volume 2025:19 Pages 4979—4990
DOI https://doi.org/10.2147/DDDT.S524102
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Yan Zhu
Xiaowei Xu,1,* Honggang Zhang,1,* Jun Li,2,* Li Zhou,1,3 Shengmei Zhu,1 Fangping Bao1
1Department of Anesthesiology, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang Province, 310003, People’s Republic of China; 2Department of Anesthesiology, Shulan (Hangzhou) Hospital, Shulan International Medical College, Zhejiang Shuren University, Hangzhou, Zhejiang Province, 310022, People’s Republic of China; 3Department of Pain Medicine, Ningbo No.6 Hospital, Ningbo, Zhejiang Province, 315040, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fangping Bao Department of Anesthesiology, The First Affiliated Hospital, Zhejiang University School of Medicine, Qingchun Road 79, Hangzhou, Zhejiang Province, 310003, People’s Republic of China, Tel +8613958105226, Email [email protected] Shengmei Zhu, Department of Anesthesiology, The First Affiliated Hospital, Zhejiang University School of Medicine, Qingchun Road 79, Hangzhou, Zhejiang Province, 310003, People’s Republic of China, Tel +8613857169801, Email [email protected]
Purpose: This study evaluated whether oxycodone alone could substitute for fentanyl combined with remifentanil for general anesthesia in laparoscopic uterine myoma surgery.
Patients and Methods: 90 adult female patients were randomized into three groups: oxycodone 0.35 mg/kg (Group A), oxycodone 0.30 mg/kg (Group B), or fentanyl 5 μg/kg (Group C) for induction. Anesthesia was maintained with propofol plus saline (Groups A/B) or remifentanil (Group C). Primary outcomes included Numerical Rating Scale (NRS) pain scores in the Post-Anesthesia Care Unit (PACU). Secondary outcomes were intubation reaction, vital signs, extubation/PACU times, Ramsey Sedation Scores (RSS) in PACU, NRS pain scores and adverse events within 48 hours postoperatively.
Results: Intubation reactions were rare (one case each in Groups B/C, none in Group A). Group B had significantly lower PACU NRS scores than Group C (0.6 ± 0.7 vs 1.3 ± 1.4, P = 0.011), while Group A showed a nonsignificant trend (0.8 ± 0.9 vs 1.3 ± 1.4, P = 0.051). RSS scores, extubation/PACU times, and 48-hour NRS scores were comparable. However, oxycodone groups had longer postoperative evacuation times than fentanyl group (Group A vs Group C: 20.0 ± 7.3 hours vs 16.5 ± 5.1 hours, P=0.038; Group B vs Group C: 20.3 ± 8.2 hours vs 16.5 ± 5.1 hours, P=0.034).
Conclusion: Oxycodone alone provides superior early postoperative analgesia compared to fentanyl-remifentanil in laparoscopic myoma surgery but may delay bowel recovery.
Keywords: oxycodone, laparoscopic surgery, myomas, fentanyl, postoperative pain
Introduction
Myomas are the most common benign tumors of the female reproductive tract, with a prevalence of up to 40% during the childbearing years.1 Many patients with myomas may not exhibit obvious symptoms, while approximately 50% experience issues such as abnormal menstruation, pelvic pain, compression symptoms,2 or even infertility.3 Recently, laparoscopic hysterectomy or laparoscopic myomectomy has emerged as the most effective treatment for symptomatic uterine myomas due to its minimally invasive nature and favorable surgical outcomes, including reduced postoperative pain and shorter recovery times compared to traditional laparotomy.2 Patients undergoing laparoscopic surgery often experience moderate to severe postoperative pain, particularly visceral pain. Unlike somatic pain, visceral pain is a deep, hidden pain within the abdomen that is difficult to localize precisely. This type of pain can trigger autonomic reflexes, lead to significant discomfort and potentially provoke negative emotional responses.4 Severe postoperative pain can even lead to respiratory impairment, prolong hospitalization, and negatively impact patient prognosis and quality of life.5 Furthermore, chronic postoperative pain is often associated with early postoperative visceral pain.6
Opioids remain the cornerstone of surgical and postoperative pain relief. International Narcotics Control Board (INCB) data on country-level use of pharmaceutical opioids shows opioid analgesic use is low in Africa, Asia, Central America, the Caribbean, South America, eastern and south-eastern Europe. The United States is the country with the highest consumption of opioid drugs, mainly for chronic non-cancer pain (CNCP).7 Over time, various analgesic agents and combination strategies have been explored to enhance efficacy and minimize side effects.
The most widely used clinical analgesia protocol combines fentanyl for induction with remifentanil for maintenance. During induction, fentanyl provides rapid-onset, sustained initial analgesia while stabilizing hemodynamics. For maintenance, remifentanil enables precise dose titration, minimizes accumulation risks, and facilitates faster postoperative recovery. This regimen optimally balances analgesic efficacy with safety, and is widely used in China.
Research has shown that oxycodone is one of the widely used opioid drugs worldwide, with the greatest association with Canada.8 Oxycodone, a semisynthetic agonist of the μ-, κ-, and δ-opioid receptors, stands out among potent opioids because it induces analgesia not only through the μ-opioid receptor but also via the κ- and δ-opioid receptors.9–11 Given that the κ-receptor plays a crucial role in inhibiting visceral pain, oxycodone offers superior postoperative pain management following laparoscopic surgery.4 Moreover, oxycodone has been demonstrated to relieve neuropathic pain.12 It has proven effective for postoperative pain control and is well tolerated across various surgical procedures and patient populations.4
Oxycodone has a rapid onset time of 2 to 3 minutes13 and a prolonged duration of action, approximately 4 hours (similar to morphine),14 suggesting that it could be used as the sole opioid for general anesthesia. Oxycodone may serve as an alternative to fentanyl for induction and may provide superior analgesic efficacy compared to fentanyl for acute postoperative pain.5 Recently, intravenous (IV) oxycodone is used for the induction to prevent the hemodynamic response of tracheal intubation,15 as well as for intraoperative and postoperative pain management.16 Our findings and other research indicate that oxycodone can be safely administered as the sole opioid for induction and with/without additional dose during general anesthesia for pain management.16,17 We hypothesize that a sufficient dose of oxycodone at induction could provide enough analgesia to support general anesthesia in moderate surgery. However, it remains unclear whether the use of oxycodone alone could substitute for the combination of fentanyl and remifentanil, which is widely used for general anesthesia. If feasible, this could significantly facilitate anesthesia and analgesia management for laparoscopic myomectomy procedures.
In this study, we first proposed to evaluate the analgesic effect and safety of using oxycodone alone in laparoscopic uterine myomas surgery (laparoscopic hysterectomy or myomectomy), and compared it with the combination of fentanyl and remifentanil, to assess its clinical applicability.
Materials and Methods
Ethical Review
This study was approved by the ethics committee of the First Affiliated Hospital, College of Medicine, Zhejiang University (2017–381) (Chairman Min Zheng) on 24 March 2017 and was registered with the Chinese Clinical Trial Registry (http://www.chictr.org.cn, ChiCTR-IPR-17011085). Written informed consent was obtained from all patients. The study protocol was designed in line with the CONSORT guidelines and complies with the Declaration of Helsinki.
Patients
From December 2017 to September 2018, adult female patients classified as American Society of Anesthesiologists (ASA) Class I or II, aged 18 to 64 years, undergoing selective laparoscopic hysterectomy or laparoscopic myomectomy for symptomatic uterine myomas were enrolled. Patients were excluded if they 1) had a body mass index (BMI) >30 kg/m² or ≤18.4 kg/m², 2) had severe cardiovascular or respiratory disease, 3) had a history of difficult intubation, a predicted difficult airway, 4) had renal, liver, or hematological disorders, 5) were taking narcotics for chronic pain, or 6) had contraindications to oxycodone and parecoxib sodium. Patients were withdrawn from the study if they 1) had more than one attempt of intubation attempt, 2) could not complete the follow-up.
Randomization
Patients were randomly assigned to receive either oxycodone 0.35 mg/kg (Group A), oxycodone 0.30 mg/kg (Group B), or fentanyl 5 μg/kg (Group C) for induction according to a computer-generated random-number sequence. The study drugs were administered in a double-blind manner. An anesthesia nurse prepared a computer-generated randomization list and the blinded study medications. Syringes were labeled with the study name, consecutive patient numbers, and the intended time of use. The randomization list was securely held by the assistant nurse and was released only after the completion of the study.
Anesthesia and Interventions
The blinded study drugs were prepared according to the following protocol: 1) For induction: 0.35 mg/kg oxycodone (Hamol Limited, UK) in Group A, 0.30 mg/kg oxycodone in Group B, or 5 μg/kg fentanyl (Humanwell Healthcare Limited, China) in Group C was diluted with saline to a total volume of 20 mL. 2) For the maintenance of general anesthesia: 2 mg remifentanil (HengRui Medicine Limited, China) was diluted with saline to a total volume of 40 mL in Group C. The same dose of 40 mL saline was prepared in Group A and B. This solution was utilized for continuous infusion during general anesthesia. An additional analgesic (0.06 mg/kg oxycodone in Group A and B, or 6 μg/kg fentanyl in Group C) was diluted to 10 mL and administered at 5 mL per dose when the anesthesiologists determined that the analgesia might be insufficient during general anesthesia. 3) For the end of the operation: The “ending drug”, which consisted of 100 mg tramadol (Grünenthal Co., Ltd., Germany) diluted to 2 mL, was prepared for Group C. The same volume of saline was prepared and marked for Group A and B. This solution was administered 5 minutes prior to the end of the operation. 4) For postoperative pain management in the post-anesthesia care unit (PACU): The same additional analgesic (either oxycodone or fentanyl, as utilized during the operation) was prepared in a 10 mL solution for administration in the PACU. When patients report moderate or severe pain, the anesthesiologist in the PACU administers a 2 mL solution in a titrated manner to relieve the pain.
All patients were transferred to the operating room without receiving premedication. Standard monitors were employed to measure pulse oximetry (SpO2), electrocardiography (ECG), invasive blood pressure (BP), and bispectral index (BIS). Baseline measurements of systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were recorded with the average of three measurements in a calm state.
Induction began with the slow administration of the blinded drug (either oxycodone or fentanyl), followed by an intravenous injection of 2 mg/kg propofol (AstraZeneca, Italy) and 0.8 mg/kg rocuronium (N.V. Organon, Holland). Tracheal intubation was performed 5 minutes after induction using a video laryngoscope (TD-C-IV, Zhejiang Yu Yi Medical Equipment Co., Ltd.) and a standard endotracheal tube, conducted by experienced anesthesiologists. Patients were mechanically ventilated with a tidal volume of 8–10 mL/kg at a respiratory rate of 12 breaths per minute to maintain an end-tidal carbon dioxide partial pressure (ETCO2) of 30–40 mmHg.
Before the operation, 50 mg of parecoxib sodium (Pharmacia Healthcare Limited, UK) and 0.25 mg of palonosetron (Qilu Pharmaceutical Co., Ltd., China) were administered. General anesthesia was maintained by continuous infusion of propofol (5–10 mg/kg) to keep the BIS (BIS A-1050 Monitor, Aspect Medical Systems, Newton, MA, USA) within a range of 40–60. A continuous infusion of the blinded analgesic (remifentanil or saline) at a rate of 10–20 mL/h was also administered. An additional 5 mL of the blinded analgesic was administered if the anesthesiologist suspected insufficient analgesia. At the end of surgery, the 2 mL blinded ending drug was administered, and the propofol infusion was discontinued.
Cisatracurium was administered as needed to maintain muscle relaxation. A dose of 0.5 mg of atropine was administered intravenously if severe bradycardia occurred (HR <50 bpm), and 6 mg of ephedrine was administered for hypotensive events (a decrease in systolic blood pressure (SBP) of <30% from the baseline value or SBP <90 mmHg). For hypertensive events (an increase in SBP ≥30% from baseline), 10 mg of urapidil was administered intravenously.
The patient was transferred to the PACU after surgery, where another anesthesiologist performed extubation. The anesthesiologist gently patted the patient’s shoulder and called the patient’s name to facilitate waking up intermittently. The patient was monitored for at least 30 minutes after extubation before being transferred to the ward. If the patient reported pain and requested medication, an additional dose of the blinded drug (2 mL at a time) was administered gradually.
Within 2 days of being transferred to the ward, the patients were routinely treated with 40mg bid of parecoxib sodium. When the patients reported pain with an NRS score of 4 or higher, 100 mg tramadol was administered for additional pain relief.
Assessment
Hemodynamic parameters (SBP, DBP and HR) were recorded at the following time points: T0 = baseline (arrival in the operating room); T1 = before intubation; T2 = 1 minute after intubation; T3 = skin incision; T4 = artificial pneumoperitoneum; T5 = head-down position; T6 = 30 minutes after the start of surgery; T7 = 60 minutes after the start of surgery; T8 = end of the operation; T9 = extubation time.
The intubation reaction was recorded if SBP, DBP, or HR increased more than 20% from baseline values within 3 minutes of intubation.
Additionally, the operation time (duration of the surgical procedure), anesthesia time (from induction to cessation of propofol infusion), extubation time (from cessation of propofol infusion to extubation), and PACU time (total duration in the PACU) were recorded. The total dose of propofol and any additional analgesics (oxycodone or fentanyl) administered in each group were also noted.
A blinded observer was responsible for evaluating adverse events, sedation, and pain scores. Pain was assessed using the Numerical Rating Scale (NRS), where 0 indicates no pain and 10 indicates the worst possible pain. We recorded patients’ pain scores after extubation in the PACU, as well as at rest and during movement (eg, while coughing) at 4, 8, 12, 24, and 48 hours postoperatively. Adverse events were documented in the PACU and within 48 hours following surgery, with respiratory depression defined as a respiratory rate of fewer than 8 breaths per minute. Additionally, evacuation time was recorded.
Furthermore, the Ramsey Sedation Score (RSS) was employed to evaluate the sedation state in the PACU as follows: 1=Anxious, agitated, or restless; 2=Cooperative, oriented, and tranquil; 3=Responds to commands; 4=Responds briskly to a light glabellar tap or loud sound; 5=Responds sluggishly to a light tap or loud sound; 6=Unresponsive to stimuli.
Statistical Analysis
A sample size calculation was performed based on the expected difference in NRS changes in the PACU. In our previous study,15,16 we explored the use of oxycodone for induction and observed its effectiveness in pain management as the sole opioid in general anesthesia, with an NRS of 0.63±1.07 in the PACU. In comparison, the NRS was 1.4±1.25 for patients who received fentanyl for induction and remifentanil for maintenance. Assuming a 5% significance level, 0.8 statistical power, and a two-sided test, 28 patients were required in each group. To account for an 10% dropout rate, 30 patients were enrolled in each group, resulting in a total of 90 participants.
Statistical analyses were performed using SPSS v. 27.0 (IBM, Armonk, NY, USA). The distributions of continuous variables were assessed for normality using the Shapiro–Wilk test. Data are presented as the mean ± SD for variables with normal distributions or as the median (range) for variables with non-normal distributions. Variables with normal distributions were compared using one-way ANOVA and LSD post hoc test, while those with non-normal distributions were compared using the Kruskal–Wallis test or Mann–Whitney U-test. Count data were compared using the chi-square test or Fisher’s exact test. Ranked data were also analyzed using the Kruskal–Wallis test. P <0.05 presents statistically significant.
Results
A total of 90 patients scheduled for elective laparoscopic hysterectomy or myomectomy were enrolled and randomized into three groups. No patients were excluded, and all were included in the final analysis without withdrawn (Figure 1).
 |
Figure 1 Consolidated Standards of Reporting Trials (CONSORT) flow diagram. |
Baseline Demographics and Perioperative Characteristics
There were no statistically significant differences among the groups in terms of patient age, body mass index, operation time, anesthesia time, PACU time, or extubation time. The demographic and clinical characteristics of the patients are presented in Table 1.
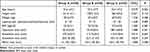 |
Table 1 Demographic and Clinical Characteristics of Patients |
Intubation Reaction
Intubation reactions occurred in 1 patient (3.3%) in Group B and Group C respectively, while no reactions were observed in Group A. SBP, DBP, and HR are presented in Figure 2. There was no statistically significant difference in any of these parameters among the three groups.
Intraoperative Medication
Additional analgesics were administered in 3 cases (10%) in Group A, 2 cases (6.7%) in Group B, and 1 case (3.3%) in Group C. There was no statistically significant difference in the comparison among the three groups. The total dose of propofol was lower in Group C compared to Group A (10.0 ± 2.4 mg/kg vs 13.3 ± 4.5 mg/kg, P = 0.0005) and compared to Group B (10.0 ± 2.4 mg/kg vs.13.0 ± 3.1 mg/kg, P = 0.0012) (Figure 3).
NRS Pain Score in PACU and 48h Postoperatively
Oxycodone reduced pain more effectively than the combination of fentanyl and remifentanil in the PACU. Group B exhibited a significantly lower NRS pain score compared to Group C (0.6±0.7 vs 1.3±1.4, P = 0.011). Although there was a trend toward a lower pain score in Group A compared to Group C (0.8±0.9 vs 1.3±1.4, P =0.051), but there was no statistically difference (Figure 4a). After extubation in the PACU, one patient in Group A had a NRS score of 4 but refused additional analgesia, whereas three patients in Group C had NRS scores higher than 4 and received additional analgesic treatment.
The pain levels were similar across all groups when assessed at rest (Figure 4c) and movement (Figure 4d) at 4, 8, 12, 24, and 48 hours postoperatively, without additional analgesia required.
Sedation in PACU
There were no significant differences in the Ramsey Sedation Scores (RSS) among the three groups in the PACU (Figure 4b). However, Group B reported three cases of excessive sedation (RSS = 4), while Group C reported two cases.
Adverse Events
Postoperative adverse events, including nausea, vomiting, dizziness, and respiratory depression, showed no significant differences among the three groups (Table 2). However, the evacuation time of Group A was significantly longer than that of Group C (20.0±7.3 hours vs 16.5±5.1 hours, P = 0.038), similar in Group B vs Group C (20.3±8.2 hours vs 16.5±5.1 hours, P = 0.034) (Figure 5).
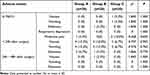 |
Table 2 Postoperative Adverse Events in the PACU and 48 hours After Surgery in the Ward |
 |
Figure 5 Evacuation time in each group. Anesthesia induction: oxycodone 0.35 mg/kg (group A), oxycodone 0.30 mg/kg (group B), or fentanyl 5 μg/kg (group C), * presents P <0.05. |
Discussion
Our non-inferiority study findings support oxycodone alone as a clinically viable alternative to the fentanyl-remifentanil combination for general anesthesia analgesia during laparoscopic hysterectomy or myomectomy. In contrast, oxycodone demonstrates superior efficacy in early postoperative analgesia but prolongs intestinal recovery.
Based on our previous ED50 and ED95 results for oxycodone induction,15 to further verify the dose-response relationship of oxycodone in preventing intubation-induced reactions, we selected oxycodone doses of 0.35 mg/kg (probit analysis for 90% of patients without intubation reaction) and 0.30 mg/kg (probit analysis for 80% of patients without intubation reaction) in this study. The results showed that all patients in Group A (oxycodone 0.35 mg/kg) and 96.7% of patients in Group B (oxycodone 0.30 mg/kg) and C (fentanyl 5 µg/kg) did not experience intubation reactions. These findings suggest that both oxycodone doses are effective and safe for induction, and 0.30 mg/kg oxycodone and 5 µg/kg fentanyl have similar effects in preventing tracheal intubation reaction. Moreover, the effective rates exceeded the predicted rates by the probit analysis, which based on data from the Dixon up-down method for ED50 may be lack of precision. Nevertheless, these oxycodone doses are higher than those used in previous reports,18 which demonstrated that oxycodone 0.2 mg/kg for endotracheal intubation was as effective as fentanyl 2 µg/kg in attenuating the hemodynamic response. This discrepancy may be attributed to the different definitions of intubation reaction. We defined the intubation reaction as an increase in SBP/DBP or HR exceeding 20% from baseline within 3 minutes of intubation, whereas that study used thresholds of over 40% for mean blood pressure (MBP) and 20% for HR within 5 minutes. The lower requirement for stable hemodynamics in the previous study may explain the lower dose of oxycodone used.
Our previous research had demonstrated the feasibility of using oxycodone as the sole opioid for the induction and maintenance of general anesthesia in minor to moderate surgeries.16 Wirz et al (Year 2018) similarly demonstrated the feasibility of oxycodone monotherapy for general anesthesia in orthopedic surgery.17 However, their reported cumulative oxycodone dose (0.16 mg/kg with isoflurane) was notably lower than the doses employed in our previous study (0.32 mg/kg with propofol). In this study, we focus on a specific type of moderate surgery to compare the analgesic effects of oxycodone alone and the combination of fentanyl and remifentanil. Ultimately, we found that oxycodone could provide stable hemodynamics during surgery (Figure 2) and Group B (oxycodone 0.3 mg/kg) offered superior analgesia than Group C (NRS: 0.6±0.7 vs 1.3±1.4, P=0.011) in the PACU. This may be attributed to: (1) the active metabolites of oxycodone, oxymorphone and noroxymorphone, which contribute to the prolonged duration of oxycodone’s action.9 (2) the nature of laparoscopic surgery, which typically involves both somatic and visceral pain.19 Given that laparoscopic surgery is minimally invasive, the pain is predominantly visceral.20 Oxycodone, as a kappa receptor agonist, plays a crucial role in inhibiting visceral pain, making it particularly effective for postoperative pain management after laparoscopic surgery compared to other opioids.21 Unexpectedly, Group A (oxycodone 0.35 mg/kg) did not provide better pain management than Group C (NRS, 0.8±0.9 vs 1.3±1.4, P =0.051) in the PACU. We speculate that this may be due to the small sample size, individual variations in opioid requirements, and differences in pain perception. For instance, one patient in Group A reported an NRS score at 4 but refused further analgesic treatment. Since there is no objective indicator, the NRS remains widely used for pain evaluation.
Our results demonstrate that the majority of patients across all three groups experienced either no pain (NRS = 0) or mild pain (NRS 1–3), with very few reporting moderate pain (NRS ≥4). This finding reflects our institutional commitment to ethical pain management, as evidenced by tramadol administration following fentanyl-remifentanil cessation to guarantee optimal postoperative analgesia. Although the observed low NRS scores demonstrate limited clinical discriminative value, the statistically significant between-group differences in PACU NRS scores (favoring oxycodone) suggest its clinical utility as a potential substitute for fentanyl-remifentanil. Future multicenter trials with expanded cohort sizes will be necessary to validate these preliminary findings and determine their clinical significance.
Additionally, no significant differences were observed in pain levels among the three groups during the subsequent 48 hours postoperatively. This finding contrasts with previous studies, which suggest that oxycodone is superior to other analgesics for up to 24 hours post-laparoscopic surgery.22 The differences were caused by the study design. In most studies, oxycodone is administered either as a single dose23 or through a patient-controlled analgesia (PCA) pump at the end of surgery,24 but one finding indicated that oxycodone demonstrated comparable efficacy to fentanyl in PCIA following laparoscopic myomectomy.25 In this study, oxycodone was administered for induction before surgery, and four hours after surgery or later was beyond its effective duration. Moreover, research has suggested that the combined use of opioids and nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce opioid dosages and associated side effects.26 Our study demonstrated that no patient required additional analgesics within 48 hours postoperatively, indicating that our medication regimen which utilized oxycodone as the sole opioid in combination with parecoxib sodium can provide sufficient analgesia for laparoscopic hysterectomy or myomectomy and eliminate the need for a PCA pump, thereby simplifying analgesic management while simultaneously minimizing adverse reactions.
Oxycodone, a long-acting opioid, raises concerns about delayed extubation due to its potential respiratory depressant effects, particularly when administered at high doses. However, in this study, there was no significant difference in extubation times among the three groups: Group A (20.0 minutes), Group B (22.5 minutes), and Group C (18.5 minutes). This outcome may be attributed to the study design. Despite we use a higher dose of oxycodone for induction, the relatively long surgical duration (80–90 minutes) likely alleviate the respiratory depressant of oxycodone and minimize its impact on extubation time.
Our previous research found that administering high doses of oxycodone as the sole opioid for general anesthesia may lead to excessive sedation.16 In this study, the overall level of sedation in the PACU was similar among the three groups, with all patients in a state of quiet cooperation, indicating safety. However, three cases of excessive sedation (RSS = 4) were observed in Group B (0.3 mg/kg oxycodone). Notably, these three patients did not experience significantly prolonged PACU stays or respiratory depression. In contrast, Group A (0.35 mg/kg oxycodone) reported zero cases. Notably, our prior research16 observed that some patients maintained normal sedation levels (RSS 2–3) despite receiving higher oxycodone doses (>0.35 mg/kg) and some patients developed oversedation at oxycodone doses 0.25–0.35 mg/Kg (unpublished data). However, the limited sample size in these studies prevented definitive conclusions regarding a dose-response relationship between oxycodone administration and sedation effects.
As with other opioids, oxycodone may cause opioid-induced bowel dysfunction (OIBD),27 which includes symptoms such as nausea, vomiting, somnolence, and constipation, due to its action on gastrointestinal μ-receptors. To prevent these symptoms, we typically administer palonosetron prior to surgery, which is a second-generation antiemetic drug with a duration of approximately 40 hours. In this study, we found that both the oxycodone and fentanyl groups experienced a limited number of cases of nausea and vomiting within 24 hours postoperatively. Additionally, some patients in the oxycodone group reported dizziness. However, there was no significant difference among the three groups. Notably, the evacuation time was significantly longer in the oxycodone group than in the fentanyl group. We hypothesize that this extended evacuation time may result from oxycodone, which inhibits gastrointestinal motility,28 reduces gastric acid secretion, increases sphincter tone,29 and affects water absorption in the intestines.30 Conversely, the combination of fentanyl and remifentanil is rapidly metabolized,31 which minimizes postoperative residual effects. Although the administration of tramadol before the end of surgery in the fentanyl group is associated with a risk of delayed evacuation, the impact of oxycodone on prolonging evacuation time remains significant. Therefore, when using oxycodone to maintain effective postoperative analgesia, it is crucial to consider its effect on gastrointestinal function recovery, which may influence the clinical decision to use oxycodone alone.
Additionally, our study found that the total amount of propofol required in oxycodone group was higher than that in fentanyl group throughout the surgical procedure. We speculate that this may result from the potent analgesic effects of continuous remifentanil infusion, which can reduce patients’ responses to surgery and decrease the need for propofol. However, it may also cause hyperalgesia, therefore, we specifically administered tramadol in fentanyl group prior to discontinuation to ensure analgesic needs.
The strength of this study lies in its randomized, double-blind, controlled design, with observations of the trial results conducted by the same investigator, which helps to minimize subjective errors in the assessment of outcomes. Additionally, this study is the first to investigates whether oxycodone alone at an adequate induction dose, supplemented intraoperatively as needed, can provide sufficient pain management for laparoscopic uterine myoma surgery under general anesthesia, thereby serving as an alternative to the fentanyl-remifentanil combination regimen.
This study has some limitations: (1) The sample size was relatively small, as it was calculated based on the expected difference in NRS changes in the PACU from our previous study. We determined that 30 patients per group represent the minimum effective baseline. Further, large sample size researches are required to establish clinical relevance and dose-dependent sedation (2) Pain assessment using the NRS involves a subjective component, as it relies on patient self-reporting. To minimize assessment bias, we employed fixed follow-up evaluators; however, since pain scores are inherently subjective and patient-reported, residual bias may persist, potentially influencing our results.
Conclusion
This exploratory study provides preliminary evidence that oxycodone alone as a potential alternative to the fentanyl-remifentanil combinations for analgesia in laparoscopic myomectomy. Oxycodone alone provides superior early postoperative analgesia compared to fentanyl-remifentanil in laparoscopic myoma surgery but may delay bowel recovery.
Data Sharing Statement
Deidentified individual participant data underlying the results reported in this article will be made available upon request to qualified researchers, along with the study protocol. Data will be accessible beginning 6 months after publication and will remain available for 5 years. Requests should be directed to the corresponding author at [email protected].
Acknowledgments
Assistance with the study: the authors thank all anesthesiologists, surgeons and nurses who contributed to the study.
Funding
Financial support and sponsorship: Hangzhou Medical and Health Technology Project B20241254.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Erden M, Uyanik E, Polat M, Ozbek IY, Yarali H, Mumusoglu S. The effect of ≤6 cm sized noncavity-distorting intramural fibroids on in vitro fertilization outcomes: a systematic review and meta-analysis. Fertil Steril. 2023;119(6):996–1007. doi:10.1016/j.fertnstert.2023.02.018
2. Amoah A, Quinn SD. Uterine-preserving treatments or hysterectomy reintervention after myomectomy or uterine artery embolisation: a retrospective cohort study of long-term outcomes. Bjog. 2023;130(7):823–831. doi:10.1111/1471-0528.17412
3. Donnez J, Taylor HS, Marcellin L, Dolmans MM. Uterine fibroid-related infertility: mechanisms and management. Fertil Steril. 2024;122(1):31–39. doi:10.1016/j.fertnstert.2024.02.049
4. Yang GW, Cheng H, Song XY, et al. Effect of oxycodone-based multimodal analgesia on visceral pain after Major laparoscopic gastrointestinal surgery: a randomised, double-blind, controlled trial. Drug Des Devel Ther. 2024;18:1799–1810. doi:10.2147/dddt.S464518
5. Raff M, Belbachir A, El-Tallawy S, et al. Intravenous oxycodone versus other intravenous strong opioids for acute postoperative pain control: a systematic review of randomized controlled trials. Pain Ther. 2019;8(1):19–39. doi:10.1007/s40122-019-0122-4
6. Blichfeldt-Eckhardt MR, Ording H, Andersen C, Licht PB, Toft P. Early visceral pain predicts chronic pain after laparoscopic cholecystectomy. Pain. 2014;155(11):2400–2407. doi:10.1016/j.pain.2014.09.019
7. Degenhardt L, Grebely J, Stone J, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet. 2019;394(10208):1560–1579. doi:10.1016/s0140-6736(19)32229-9
8. Robert M, Jouanjus E, Khouri C, Sam-Laï N, Revol B. The opioid epidemic: a worldwide exploratory study using the WHO pharmacovigilance database. Addiction. 2023;118(4):771–775. doi:10.1111/add.16081
9. Barrett JE, Shekarabi A, Inan S. Oxycodone: a current perspective on its pharmacology, abuse, and pharmacotherapeutic developments. Pharmacol Rev. 2023;75(6):1062–1118. doi:10.1124/pharmrev.121.000506
10. Marie N, Noble F. Oxycodone, an opioid like the others? Front Psychiatry. 2023;14:1229439. doi:10.3389/fpsyt.2023.1229439
11. Kinnunen M, Piirainen P, Kokki H, Lammi P, Kokki M. Updated clinical pharmacokinetics and pharmacodynamics of oxycodone. Clin Pharmacokinet. 2019;58(6):705–725. doi:10.1007/s40262-018-00731-3
12. Umukoro NN, Aruldhas BW, Rossos R, Pawale D, Renschler JS, Sadhasivam S. Pharmacogenomics of oxycodone: a narrative literature review. Pharmacogenomics. 2021;22(5):275–290. doi:10.2217/pgs-2020-0143
13. Kinnunen M, Kokki H, Hautajärvi H, et al. Oxycodone concentrations in the central nervous system and cerebrospinal fluid after epidural administration to the pregnant ewe. Basic Clin Pharmacol Toxicol. 2019;125(5):430–438. doi:10.1111/bcpt.13276
14. Leow KP, Smith MT, Williams B, Cramond T. Single-dose and steady-state pharmacokinetics and pharmacodynamics of oxycodone in patients with cancer. Clin Pharmacol Ther. 1992;52(5):487–495. doi:10.1038/clpt.1992.176
15. Kang XH, Bao FP, Zhang HG, et al. Gender affects the median effective dose and 95% effective dose of oxycodone for blunting the hemodynamic response to tracheal intubation in narcotic-naïve adult patients. Chin Med J. 2018;131(16):1958–1963. doi:10.4103/0366-6999.238138
16. Bao F, Xie Q, Zhang H, Zhu S, Kang X. Feasibility of using oxycodone as the sole opioid for induction and maintenance of general anaesthesia in minor/moderate surgery: a prospective, observational, descriptive study. J Int Med Res. 2020;48(10):300060520957500. doi:10.1177/0300060520957500
17. Wirz S, Ellerkmann RK, Soehle M, Wirtz CD. Oxycodone is safe and effective for general anesthesia. J Opioid Manag. 2018;14(2):125–130. doi:10.5055/jom.2018.0439
18. Lee YS, Baek CW, Kim DR, et al. Comparison of hemodynamic response to tracheal intubation and postoperative pain in patients undergoing closed reduction of nasal bone fracture under general anesthesia: a randomized controlled trial comparing fentanyl and oxycodone. BMC Anesthesiol. 2016;16(1):115. doi:10.1186/s12871-016-0279-x
19. Wessels J, Klinger R, Benson S, et al. Preoperative anxiolysis and treatment expectation (PATE trial): open-label placebo treatment to reduce preoperative anxiety in female patients undergoing gynecological laparoscopic surgery - study protocol for a bicentric, prospective, randomized-controlled trial. Front Psychiatry. 2024;15:1396562. doi:10.3389/fpsyt.2024.1396562
20. Sao CH, Chan-Tiopianco M, Chung KC, et al. Pain after laparoscopic surgery: focus on shoulder-tip pain after gynecological laparoscopic surgery. J Chin Med Assoc. 2019;82(11):819–826. doi:10.1097/jcma.0000000000000190
21. Lao WL, Song QL, Jiang ZM, Chen WD, Zheng XH, Chen ZH. The effect of oxycodone on post-operative pain and inflammatory cytokine release in elderly patients undergoing laparoscopic gastrectomy. Front Med Lausanne. 2021;8:700025. doi:10.3389/fmed.2021.700025
22. Li Y, Dou Z, Yang L, Wang Q, Ni J, Ma J. Oxycodone versus other opioid analgesics after laparoscopic surgery: a meta-analysis. Eur J Med Res. 2021;26(1):4. doi:10.1186/s40001-020-00463-w
23. Choi YJ, Park SW, Kwon HJ, Choi JM, Lee YM. Efficacy of early intravenous bolus oxycodone or fentanyl in emergence from general anaesthesia and postoperative analgesia following laparoscopic cholecystectomy: a randomized trial. J Int Med Res. 2015;43(6):809–818. doi:10.1177/0300060515594194
24. Hwang BY, Kwon JY, Kim E, Lee DW, Kim TK, Kim HK. Oxycodone vs. fentanyl patient-controlled analgesia after laparoscopic cholecystectomy. Int J Med Sci. 2014;11(7):658–662. doi:10.7150/ijms.8331
25. Dong P, Qu X, Yang Y, Li X, Wang C. Effect of oxycodone versus fentanyl for patient-controlled intravenous analgesia after laparoscopic hysteromyomectomy: a single-blind, randomized controlled trial. Sci Rep. 2024;14(1):20478. doi:10.1038/s41598-024-71708-5
26. Mitra S, Carlyle D, Kodumudi G, Kodumudi V, Vadivelu N. New advances in acute postoperative pain management. Curr Pain Headache Rep. 2018;22(5):35. doi:10.1007/s11916-018-0690-8
27. Candy B, Jones L, Vickerstaff V, Larkin PJ, Stone P. Mu-opioid antagonists for opioid-induced bowel dysfunction in people with cancer and people receiving palliative care. Cochrane Database Syst Rev. 2022;9(9):Cd006332. doi:10.1002/14651858.CD006332.pub4
28. Goudsward HJ, Ruiz-Velasco V, Stella SL, Willing LB, Holmes GM. Coexpressed δ-, μ-, and κ-opioid receptors modulate voltage-gated Ca(2+) channels in gastric-projecting vagal afferent neurons. Mol Pharmacol. 2024;105(3):250–259. doi:10.1124/molpharm.123.000774
29. Grønlund D, Poulsen JL, Krogh K, et al. The impact of naloxegol on anal sphincter function - Using a human experimental model of opioid-induced bowel dysfunction. Eur J Pharm Sci. 2018;117:187–192. doi:10.1016/j.ejps.2018.02.008
30. Mark EB, Bødker MB, Grønlund D, Østergaard LR, Frøkjaer JB, Drewes AM. MRI analysis of fecal volume and dryness: validation study using an experimental oxycodone-induced constipation model. J Magn Reson Imaging. 2019;50(3):733–745. doi:10.1002/jmri.26628
31. Sneyd JR. Potential responses to remifentanil supply shortages. Br J Anaesth. 2022;129(5):649–651. doi:10.1016/j.bja.2022.08.001
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




