Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Pathological Characteristics of Ferroptosis in Kidney Tissues in Type 2 Diabetic Patients with Diabetic Kidney Disease
Authors Li M , Zhao S, Liu Y, Wang Q, Chen Y, Zhou Y
Received 6 September 2024
Accepted for publication 23 October 2024
Published 1 November 2024 Volume 2024:17 Pages 4105—4113
DOI https://doi.org/10.2147/DMSO.S489536
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Min Li,1,2 Song Zhao,2 Yan Liu,1 Qian Wang,2 Yongzhe Chen,2 Yaru Zhou1
1Department of Endocrinology, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050051, People’s Republic of China; 2Department of Nephrology, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050051, People’s Republic of China
Correspondence: Yaru Zhou, Department of Endocrinology, The Third Hospital of Hebei Medical University, Shijiazhuang, Ziqiang Road 139, Hebei, 050051, People’s Republic of China, Tel +86-0311-88603031, Email [email protected]
Background: Diabetes kidney disease (DKD) is a common complication of diabetes and is currently considered the primary cause of end-stage renal disease. Ferroptosis has been found to participate in the development of DKD. However, no ferroptosis-related markers have been evaluated in human DKD samples. This study aimed to examine the ferroptosis-related pathological alterations in DKD samples.
Methods: This study enrolled patients with DKD at the Third Hospital of Hebei Medical University between January 2018 and December 2022, of whom 30 were diagnosed with DKD and 10 with non-DKD (CON). Clinical data of patients were collected, and hematoxylin-eosin staining (H&E), PASM, and immunohistochemical staining were performed to evaluate pathological changes and the expression of ferroptosis-related proteins, including GPX4, ACSL4, Nrf2, TfR1, FTH, and FTL.
Results: Compared with the CON group, patients with DKD exhibited significantly elevated serum creatinine levels and reduced eGFR (P < 0.05). Iron content and the expression of the ferroptosis-related protein ACSL4 were significantly increased, while the expression of Nrf2 was significantly decreased in the renal tissues of patients with DKD (P all < 0.05). There were no differences in the expression of GPX4, TfR1, FTH, or FTL between the two groups. Nrf2 and ACSL4 expression were influential factors in the occurrence of DKD and both exhibited diagnostic value for DKD. Nrf2 was a protective factor (OR, < 1), whereas ACSL4 was a risk factor (OR, > 1).
Conclusion: Ferroptosis-promoting gene profile was identified in DKD renal samples, indicating that ferroptosis may participate in the pathogenesis of DKD. The expression levels of Nrf2 and ASCL4 in the kidneys are related to the severity and progression of DKD.
Keywords: diabetes kidney disease, ferroptosis, iron overload, lipid peroxidation
Background
Diabetic kidney disease(DKD), the most common microvascular complication of diabetes, is the main cause of end-stage renal disease(ESRD). Approximately 30% of patients with type 1 diabetes and 40% of patients with type 2 diabetes progress to DKD, a serious public health problem worldwide.1 Data have indicated that in the last 20 years, most diabetic complications, such as acute myocardial infarction, death caused by hyperglycemic crisis, stroke, and amputation, have largely declined, except for ESRD,2 which places a huge economic burden on patients and society. However, to date, there are no effective interventions to delay the progression of DKD. Therefore, clarifying the pathogenesis of DKD is of great significance for relative treatment strategies.
Ferroptosis is a type of non-apoptotic regulated cell death characterized by iron-dependent lipid peroxidation,3 which is characteristics by intracellular iron overload, and iron-dependent lipid peroxide accumulation. In recent years, the role of ferroptosis in DKD have been investigated.4–7 Iron overload were found in tubular epithelial cells and in DM animal model.4,5 Ferroptosis promoting gene profile has also been observed in DKD models both in vivo and in vitro which indicating ferroptosis play important role in pathogenesis of DKD. However, very limited data are available regarding the iron content and relative gene expression in human DKD samples.
In the present study, we aimed to investigate iron content and ferroptosis-related gene expression in human kidney samples and explore their relationship with DKD.
Methods
Human Kidney Sample Collection
30 kidney tissue samples from paraffin blocks from percutaneous renal biopsies were obtained from patients with type 2 diabetes at the Third Hospital of Hebei Medical University between January 2018 and December 2022, who were pathologically diagnosed with DKD. Control kidney samples were collected from adjacent renal cancer tissues, and their pathological findings did not show specific abnormalities or only minimal glomerular changes (CON). The indication of diabetes renal biopsy are following: T1DM patient (DM duration at least 5 years) with proteinuria or hematuria or tubular urine; T2DM patients with unexplainable proteinuria, or tubular urine or hematuria and the filtration rate decreased more than 30% in DM patients without diabetes retinopathy or neuropathy. Baseline patient data regarding sex, age, blood pressure, hemoglobin, and biochemical data including albumin, blood lipids, blood glucose, uric acid were collected. 24-hour urine protein and plasma ferritin levels were also recorded.
This study was approved by the Ethics Committee of the Third Hospital of Hebei Medical University (W2023-024-1), and all participants provided written informed consent forms were signed by all subjects.
Morphological Analysis and Prussian Blue Staining
Kidney tissues were fixed in 4% neutral formaldehyde and embedded in paraffin blocks. Hematoxylin-eosin (H&E), Masson’s trichrome, and periodic acid silver methenamine(PASM)staining was performed on 4μm kidney sections. Diabetic glomerulopathy was classified as class I through IV by expert pathologists, according to the Diabetes Mellitus staging criteria.
The iron content in the kidney tissue was measured using Prussian blue staining. The slices were immersed in 20% aqueous hydrochloric acid (Iron Reagent A) for 4 min, followed by immersion in aqueous potassium ferrocyanide (Iron Reagent B) for 4 min. The slices were then rinsed with distilled water, immersed in a 0.1% Nuclear Fast Red Solution for 4–5 minutes, and then rinsed. The tissue was then subjected to two changes of graded ethanol and xylene solutions before being coverslipped.
Immunohistochemical (IHC) Staining
Slides were deparaffinized, hydrated, and incubated with primary antibodies against Nrf2 (1:50, ab62352, Abcam, Cambridge, US), GPX4 (1:800, ab125066, Abcam), ACSL4 (1:100, ab155282, Abcam), transferrin receptor protein 1(TfR1) (1:500, ab214039, Abcam), ferritin heavy chain(FTH) (1:200, ab65080, Abcam), ferritin light chain(FTL) (0.5ug/mL, ab218400, Abcam). Subsequently, a DAB staining solution (polymer method) kit (P0203, Beyotime, Shanghai, China) and horseradish peroxidase(HRP)-conjugated secondary antibody were used to detect immunoactivity. Image analysis and quantification were performed using Image-Pro Plus v6.0 analysis software (Media Cybernetics).
Statistical Analysis
Semi-quantitative immunohistochemistry data were calculated using the GraphPad Prism software (GraphPad Software, San Diego, CA, USA). Statistical analysis was performed using SPSS software (version 26.0). An independent sample t-test was used for statistical analysis between the two groups. One-way analysis of variance (ANOVA) was used for multiple group comparisons, Student Newman Keuls (SNK) q-test was used for pairwise comparison between groups, and the chi-square test was used for count data comparison between two groups. The correlation between the two factors was determined using Pearson or Spearman correlation. The influencing factors were analyzed using logistic regression analysis. The receiver operating characteristic (ROC) curve was used to investigate the diagnostic value of each index in DKD. All experimental data are expressed as mean ± standard deviation (SD), and P < 0.05.
Results
Baseline Characteristics of Subjects
Data from the present study indicated that, compared to the CON group, DKD patients exhibited significantly elevated serum creatinine levels and reduced eGFR (P < 0.05). No differences were found in age, blood pressure, hemoglobin, albumin, blood lipids, blood glucose, uric acid, 24-hour urine protein, or serum ferritin levels. As for the pathological type, 0/30 (0%), 23/30 (76.6%), 6/30 (20.0%), and 1/30 (3.33%) patients were categorized as class I, class II, class III, and class IV, respectively, according to diabetic glomerulopathy. (Table 1)
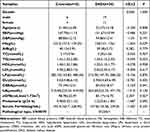 |
Table 1 Demographical Characteristics of Subjects |
Compared with the CON group, samples from DKD patients exhibited magnificent pathological alterations, including proliferation of glomerular mesangial cells and matrix (accompanied by the formation of Kimmelstiel Wilson nodules), thickening of the basement membrane, and renal interstitial fibrosis. In the present study, 23 samples were in class II, six samples were in class III, and only one sample was in class IV for DKD. (Figure 1)
Iron Content and the Expression of Ferroptosis-Related Genes in DKD Samples
Data from this study showed that, compared to the CON group, the iron content was significantly increased in the DKD samples (P < 0.01), indicating that renal iron overload was involved in the pathogenesis of DKD.
The data indicated that compared to the CON group, the expression of ACSL4 was significantly increased in the renal tissues of DKD patients, while Nrf2 expression was significantly decreased (P all < 0.01), indicating that ferroptosis promotes the gene expression profile in DKD samples. The expression of GPX4 and TfR1 tended to increase, whereas that of FTH and FTL tended to decrease, but the difference was not statistically significant (P > 0.05). (Figure 2)
Correlation Analysis of Serum Creatinine, eGFR and Ferroptosis Related Genes in Renal Tissue of DKD Patients
Data from the present study showed that CREA was negatively correlated with the gene expression of Nrf2 (r = −0.556, P = 0.001) and positively correlated with ACSL4 (r = 0.422, P = 0.020); eGFR was positively correlated with Nrf2 expression (r = 0.378, P = 0.039) and negatively correlated with ACSL4 (r = −0.456, P = 0.011) (Figure 3).
Risk Factors and Diagnostic Efficacy Analysis for the Occurrence and Development of DKD
The data indicated that the gene expression of Nrf2 and ACSL4 was an influencing factor for DKD; Nrf2 was a protective factor (OR < 1), while ACSL4 was a risk factor (OR > 1) (Table 2).
 |
Table 2 Binary Multiple Logistic Regression Analysis |
ROC analysis showed that both Nrf2 and ACSL4 expression possessed diagnostic value for DKD, with areas under the curve of 0.817 and 0.890, respectively. Sensitivity and specificity were 73.33%, 90.00%, 76.67%, and 90.00%, respectively. The diagnostic cut-off values were 0.0864 and 0.1495, respectively (Table 3 and Figure 4).
 |
Table 3 Diagnostic Efficacy Analysis of Nrf2 and ACSL4 in DKD |
 |
Figure 4 Receiver operator characteristic curve of Nrf2 and ACSL4 in the diagnosis of DKD. Nrf2, nuclear factor erythroid-2-related factor 2; ACSL4, acyl-CoA synthetase long-chain family member 4. |
Discussion
DKD is a severe microvascular complication of diabetes mellitus. The World Health Organization (WHO) predicts that by 2040, the number of diabetic patients worldwide will increase to 600 million, of which approximately 1/3 will develop DKD.8 Ferroptosis, a new form of controlled cell death associated with lipid peroxidation in an iron-dependent manner,3 has been found previously participates in the pathogenesis of many renal diseases, including DKD, acute kidney injury, renal fibrosis, and renal cell carcinoma.9–14 However, to the best of our knowledge, only few studies have investigated ferroptosis in human kidney samples.
Iron overload in the kidney tissue, in addition to triggering ferroptosis, has also been found to cause proteinuria and renal tubular injury in patients and streptozotocin (STZ)-induced diabetic rat models.15–17 In the present study, we found iron overload in kidney samples from patients with DKD, and similar results have been described in studies performed in DN models and in vitro studies performed in high-glucose-treated human renal proximal tubular (HK-2) cells.6,18,19 The application of iron chelators in DN rats was found to be renoprotective by improving renal structure and alleviating inflammation and fibrosis.20 Reducing iron-rich food intake can reduce the urinary albumin excretion rate and improve renal function in patients.21
Several key genes are involved in ferroptosis. Nuclear factor erythroid 2-related factor 2 (Nrf2) is a transcription factor that regulates cellular antioxidant gene expression,22,23 and the upregulation of Nrf2 expression can alleviate ferroptosis in DKD models in vitro and in vivo.18,24,25 Acyl-CoA synthetase long-chain family member 4 (ACSL4) is a known promoter of ferroptosis, which regulates lipid biosynthesis.26,27 Wang et al found increased renal expression of ACSL4 has been found in diabetic nephropathy (DN) models.6 In the present study, we observed a ferroptosis-promoting gene expression profile in DKD renal samples, with decreased Nrf2 and increased ACSL4 expression. Similar gene expression patterns have been previously described in DN models both in vivo and in vitro.18,28–30 In the present study, we found that renal Nrf2 and ACSL4 expression correlated with serum creatinine and eGFR, both of which showed diagnostic efficiency for DKD. It has also been previously found that ACSL4 has good predictive value for DKD.31 Moreover, compared to healthy controls, patients with lupus nephritis (LN) expressed higher levels of ACSL4. Decreased renal expression of Nrf2 was found in patients with DN and has been found to be correlated with the severity of renal damage in patients with LN32,33 no predictive value has been checked until this study. Therefore, Nrf2 and ACSL4 may provide potential strategies for assessing the prognosis assessment.
Glutathione peroxidase 4 (GPX4) is an antioxidant enzyme that can reduce lipid hydroperoxides in lipid membranes, thereby inhibiting ferroptosis,34 inactivation or absence of GPX4 lead to the accumulation of lipid peroxides, which is considered a fatal signal of ferroptosis.15,35–37 Decreased GPX4 expression was previously reported by Wang et al in kidney samples from patients.38,39 However, no alterations in GPX4 expression were observed in our study. Inconsistent results were also observed for FTH, FTL, and TfR1 expression, all of which are involved in iron accumulation. We assume that in the present study, most patients with DKD were at relatively early stages of DKD, in which compensatory responses might have occurred. However, the detailed mechanisms underlying this phenomenon require further investigation.
This study has some limitations. First, the sample size was relatively small, which might have led to data bias and the inability to obtain data stratified by different DKD stages. Second, this was a cross-sectional study, and the causal relationship between DKD and ferroptosis or iron metabolism could not be explained in detail.
Conclusion
Iron overload and a pro-ferroptotic gene expression profile have been observed in human DKD renal tissues, indicating that ferroptosis participates in the pathogenesis of DKD. Both ACSL4 and Nrf2 expression are associated with renal function. These results provide important new insights into the pathogenesis of DKD.
Data Sharing Statement
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
Ethical Statement
The experimental plan was approved by the Ethics Committee of the Third Hospital of Hebei Medical University. This study was conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff who implemented the intervention and evaluation components of the study.
Funding
This study was funded by the Medical Science Research Project of the Health Commission of Hebei Province (20230093).
Disclosure
The authors declare no conflicts of interest related to this study.
The abstract of this paper was presented at the American Diabetes Association annual meeting as a poster presentation. The poster’s abstract was published in “Poster Abstracts” in Diabetes 2024;73(Supplement_1):1787-LB, DOI: doi.org/10.2337/db24-1787-LB.
References
1. Ahmad AA, Draves SO, Rosca M. Mitochondria in diabetic kidney disease. Cells. 2021;10(11):2945. doi:10.3390/cells10112945
2. Bonner R, Albajrami O, Hudspeth J, et al. Diabetic kidney disease. Primary Care. 2020;47(4):645–659. doi:10.1016/j.pop.2020.08.004
3. Dixon SJ, Lemberg KM, Lamprecht MR, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–1072. doi:10.1016/j.cell.2012.03.042
4. Wang Y, Yue S, Cai F, et al. Treatment of berberine alleviates diabetic nephropathy by reducing iron overload and inhibiting oxidative stress. Histol Histolpathol. 2023;38(9):1009–1016. doi:10.14670/HH-18-599
5. Dominguez JH, Liu Y, Kelly KJ. Renal iron overload in rats with diabetic nephropathy. Physiol Rep. 2015;3(12):e12654. doi:10.14814/phy2.12654
6. Wang Y, Bi R, Quan F, et al. Ferroptosis involves in renal tubular cell death in diabetic nephropathy. Eur J Pharmacol. 2020;888:173574. doi:10.1016/j.ejphar.2020.173574
7. Sha W, Hu F, Xi Y, et al. Mechanism of ferroptosis and its role in type 2 diabetes mellitus. J Diabetes Res. 2021;2021:9999612. doi:10.1155/2021/9999612
8. Birabaharan M, Kaelber DC, Pettus JH, et al. Risk of new-onset type 2 diabetes in 600 055 people after COVID −19: a cohort study. Diabetes Obes Metab. 2022;24(6):1176–1179. doi:10.1111/dom.14659
9. Stockwell BR. Ferroptosis turns 10: emerging mechanisms, physiological functions, and therapeutic applications. Cell. 2022;185(14):2401–2421. doi:10.1016/j.cell.2022.06.003
10. k T, Singh TG, Kaur A. Targeting ferroptosis in ischemia/reperfusion renal injury. N-S Arch Pharmacol. 2022;396(11):1331–1341. doi:10.1007/s00210-022-02277-5
11. Zhang J, Wang B, Yuan S, et al. The role of ferroptosis in acute kidney injury. Front Mol Biosci. 2022;9:951275. doi:10.3389/fmolb.2022.951275
12. Zhang M, Tong Z, Wang Y, et al. Relationship between ferroptosis and mitophagy in renal fibrosis: a systematic review. J Drug Target. 2023;31(8):858–866. doi:10.1080/1061186X.2023.2250574
13. Yang L, Fan Y, Zhang Q. Targeting ferroptosis in renal cell carcinoma: potential mechanisms and novel therapeutics. Heliyon. 2023;9(8):e18504. doi:10.1016/j.heliyon.2023.e18504
14. Scindia Y, Ali A, Desai D, et al. Renal tubular cell ferroptosis: a new player in pathogenesis of lupus nephritis. J Immunol. 2022;208(1_supple):174–178. doi:10.4049/jimmunol.208.supp.174.08
15. Yang WS, Kim KJ, Gaschler MM, et al. Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc Natl Acad Sci. 2016;113(34):E4966–4975. doi:10.1073/pnas.1603244113
16. Dahan I, Thawho N, Farber E, et al. The iron-klotho-VDR axis is a major determinant of proximal convoluted tubule injury in haptoglobin 2-2 genotype diabetic nephropathy patients and mice. J Diabetes Res. 2018;2018:7163652. doi:10.1155/2018/7163652
17. Gao W, Li X, Gao Z, et al. Iron increases diabetes-induced kidney injury and oxidative stress in rats. Biol Trace Elem Res. 2014;160(3):368–375. doi:10.1007/s12011-014-0021-9
18. Li S, Zheng L, Zhang J, et al. Inhibition of ferroptosis by up-regulating Nrf2 delayed the progression of diabetic nephropathy. Free Radic Biol Med. 2021;162:435–449. doi:10.1016/j.freeradbiomed.2020.10.323
19. Morita T, Nakano D, Kitada K, et al. Chelation of dietary iron prevents iron accumulation and macrophage infiltration in the type I diabetic kidney. Eur J Pharmacol. 2015;756:85–91. doi:10.1016/j.ejphar.2015.03.053
20. Feng Y, Jai L, Ma W, et al. Iron chelator deferoxamine alleviates progression of diabetic nephropathy by relieving inflammation and fibrosis in rats. Biomolecules. 2023;13(8):1266. doi:10.3390/biom13081266
21. de Mello VD, Zelmanovitz T, Perassolo MS, et al. Withdrawal of red meat from the usual diet reduces albuminuria and improves serum fatty acid profile in type 2 diabetes patients with macroalbuminuria. Am J Clin Nutr. 2006;83(5):1032–1038. doi:10.1093/ajcn/83.5.1032
22. Yan R, Lin B, Jin W, et al. NRF2, a Superstar of Ferroptosis. Antioxidants. 2023;12(9):1739. doi:10.3390/antiox12091739
23. Dodson M, Castro-Portuguez R, Zhang DD. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23:101107. doi:10.1016/j.redox.2019.101107
24. Shakya A, McKee NW, Dodson M, et al. Anti-ferroptotic effects of Nrf2: beyond the antioxidant response. Mol Cells. 2023;46(3):165–175. doi:10.14348/molcells.2023.0005
25. Ji J, Tao P, Wang Q, et al. Emodin attenuates diabetic kidney disease by inhibiting ferroptosis via upregulating Nrf2 expression. Aging. 2023;15(15):7673–7688. doi:10.18632/aging.204933
26. Doll S, Proneth B, Tyurina YY, et al. ACSL4 dictates ferroptosis sensitivity by shaping cellular lipid composition. Nat Chem Biol. 2017;13(1):91–98. doi:10.1038/nchembio.2239
27. Wang Y, Zhang M, Bi R, et al. ACSL4 deficiency confers protection against ferroptosis-mediated acute kidney injury. Redox Biol. 2022;51:102262. doi:10.1016/j.redox.2022.102262
28. Fang X, Song J, Chen Y, et al. LncRNA SNHG1 knockdown inhibits hyperglycemia induced ferroptosis via miR-16-5p/ACSL4 axis to alleviate diabetic nephropathy. J Diabetes Invest. 2023;14(9):1056–1069. doi:10.1111/jdi.14036
29. Wu Y, Zhao Y, Yang HZ, et al. HMGB1 regulates ferroptosis through Nrf2 pathway in mesangial cells in response to high glucose. Biosci Rep. 2021;41(2):BSR20202924. doi:10.1042/BSR20202924
30. Zhang Q, Hu Y, Hu JE, et al. Sp1-mediated upregulation of Prdx6 expression prevents podocyte injury in diabetic nephropathy via mitigation of oxidative stress and ferroptosis. Life Sci. 2021;278:119529. doi:10.1016/j.lfs.2021.119529
31. Wu Y, Sun Y, Wu Y, et al. Predictive value of ferroptosis-related biomarkers for diabetic kidney disease: a prospective observational study. Acta Diabetol. 2023;60(4):507–516. doi:10.1007/s00592-022-02028-1
32. Nie P, Lou Y, Bai X, et al. Influence of zinc levels and Nrf2 expression in the clinical and pathological changes in patients with diabetic nephropathy. Nutr Diabetes. 2022;12(1):37. doi:10.1038/s41387-022-00212-4
33. Li J, Guo Q, Wei X, et al. Association of serum Nrf2 protein levels with disease activity and renal impairment in lupus nephritis. Front Immunol. 2024;15:1304167. doi:10.3389/fimmu.2024.1304167
34. Lei P, Bai T, Sun Y. Mechanisms of ferroptosis and relations with regulated cell death: a review. Front Physiol. 2019;10:139. doi:10.3389/fphys.2019.00139
35. Kagan VE, Mao G, Qu F, et al. Oxidized arachidonic and adrenic PEs navigate cells to ferroptosis. Nat Chem Biol. 2017;13(1):81–90. doi:10.1038/nchembio.2238
36. Zhang W, Liu Y, Liao Y, et al. GPX4, ferroptosis, and diseases. Biomed Pharmacother. 2024;174:116512. doi:10.1016/j.biopha.2024.116512
37. Forcina GC, Dixon SJ. GPX4 at the crossroads of lipid homeostasis and ferroptosis. Proteomics. 2019;19(18):e1800311. doi:10.1002/pmic.201800311
38. Kim S, Kang SW, Joo J, et al. Characterization of ferroptosis in kidney tubular cell death under diabetic conditions. Cell Death Dis. 2021;12(2):160. doi:10.1038/s41419-021-03452-x
39. Wang YH, Chang DY, Zhao MH, et al. Glutathione peroxidase 4 is a predictor of diabetic kidney disease progression in type 2 diabetes mellitus. Oxid Med Cell Longev. 2022;2022:2948248. doi:10.1155/2022/2948248
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




