Back to Journals » Infection and Drug Resistance » Volume 18
Population Pharmacokinetics-Based Evaluation of Ceftazidime-Avibactam Dosing Regimens in Critically and Non-Critically Ill Patients With Carbapenem-Resistant Klebsiella pneumoniae
Authors Chen Y , Chen B, Huang Y, Li X, Wu J, Lin R, Chen M, Liu M, Qiu H , Cheng Y
Received 9 September 2024
Accepted for publication 29 November 2024
Published 18 February 2025 Volume 2025:18 Pages 941—955
DOI https://doi.org/10.2147/IDR.S495279
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yiying Chen,1,2,* Bo Chen,1,2,* Yingbin Huang,1,2 Xueyong Li,1 Junnan Wu,1,2 Rongqi Lin,1– 3 Ming Chen,1,2 Maobai Liu,1 Hongqiang Qiu,1,2 Yu Cheng1,2
1Department of Pharmacy, Fujian Medical University Union Hospital, Fuzhou, 350001, People’s Republic of China; 2College of Pharmacy, Fujian Medical University, Fuzhou, 350004, People’s Republic of China; 3Shanghang County Hospital, Longyan, 364200, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongqiang Qiu; Yu Cheng, Department of Pharmacy, Fujian Medical University Union Hospital, 29 Xin Quan Road, Fuzhou, Fujian, 350001, People’s Republic of China, Tel/Fax +86 591 86218591, Email [email protected]; [email protected]
Purpose: This study aimed to describe the population pharmacokinetics (PopPK) of ceftazidime-avibactam (CAZ-AVI) in adult patients, and to develop optimal dosing regimens for both non-critically ill and critically ill patients by combining different pharmacokinetic/pharmacodynamic (PK/PD) targets.
Patients and Methods: A prospective, single-center study involving patients who were infected with CRKP and received CAZ-AVI therapy was conducted. Nonlinear mixed-effect modeling was used to develop a PopPK model. The optimal dosing regimen was assessed using Monte Carlo simulation.
Results: The PopPK analysis of CAZ-AVI included 91 steady-state concentrations from 45 adult patients. The data were modeled using a one-compartment model. The typical population values of CAZ and AVI clearances were 2.96 L/h and 3.09 L/h, and the volumes of distribution were 17.76 L and 18.25 L, respectively. Our study showed that creatinine clearance (CrCL) calculated using the Cockcroft-Gault equation significantly affected the pharmacokinetics of CAZ-AVI. The Monte Carlo simulation optimized the dosing regimen for both non-critically ill and critically ill patients with varying renal functions, providing detailed supplements to the instructions.
Conclusion: Our study established a PopPK model for CAZ-AVI and proposed a reference for dosing regimen adjustment based on the severity of the disease and renal functional status.
Keywords: ceftazidime-avibactam, pharmacokinetic modeling, renal function, Monte Carlo simulation, dose optimization
Introduction
Carbapenem-resistant Klebsiella pneumoniae (CRKP) infections have become a significant threat to public health, accounting for one of the leading causes of mortality worldwide.1 New antibiotics are urgently needed to complement clinical antimicrobial therapy. Ceftazidime-avibactam (CAZ-AVI) is a combined product of ceftazidime (CAZ) and the β-lactamase inhibitor avibactam (AVI) in a fixed 4:1 ratio.2 The Infectious Diseases Society of America and the European Society for Clinical Microbiology and Infectious Diseases have recommended CAZ-AVI as a first-line drug against CRKP infections.3,4 It is approved for treating complicated intra-abdominal infections, complicated urinary tract infections, hospital-acquired pneumonia, and associated bacteremia.2
Pharmacokinetic/pharmacodynamic (PK/PD) targets are crucial for optimizing antibiotic dosing. For CAZ, successful bactericidal outcomes hinge on maintaining the free plasma concentration exceeding the minimum inhibitory concentration (MIC) for a sufficient portion of the dosing interval (% fT > MIC), with 50% fT > MIC as the widely accepted target. Similarly, in the case of AVI, Nichols et al determined that a % fT > a threshold concentration (CT) of 1 mg/L is the most relevant PK/PD index for the efficacy of AVI in restoring CAZ efficacy.5
Since the approval of CAZ-AVI by the FDA in 2015, several PK studies have been conducted based on the above PK/PD targets.6–9 These studies established a standard dosing regimen of 2.5 g q8h (2-h infusion), with adjustments for patients with creatinine clearance (CrCL) ≤ 50 mL/min using the Cockcroft-Gault equation.2 However, with the wide use of CAZ-AVI in clinical practice, concerns have emerged regarding the utility of the instruction-based dosing regimen. For instance, a multicenter study in northern China indicated that a revised regimen of 2.5 g q12h (2-h infusion) also demonstrated sufficient efficacy in patients with a CrCL > 51 mL/min.10 In contrast, a study in critically ill patients with augmented renal function (ARC) revealed that the standard dosage in the instruction was inadequate for achieving optimal PK/PD targets and microbial eradication in most of these patients.11 These findings indicate the recommended regimens in the instructions has its limitations. Roberts et al have highlighted that a 100% fT > MIC target of CAZ is correlated with improved clinical outcomes and inhibiting the development of resistance in critically ill patients compared to the 50% fT > MIC target.12 Additionally, the French Society of Pharmacology and Therapeutics (SFPT) has similarly advocated higher PK/PD targets for critically ill patients.13 Thus, it is essential to distinguish between non-critically and critically ill patients and set different PK/PD targets for patient conditions. Voices have been raised that it is necessary to set different PK/PD targets according to the clinical status of patients. Hereto, there is none of the studies proposed appropriate dosing regimens for the higher PK/PD target of CAZ-AVI.
To address this gap, we conducted a prospective study on patients who received intravenous CAZ-AVI treatment. We developed a population pharmacokinetic (PopPK) model to describe inter-individual and intra-individual variability,14 and combined the two distinct PK/PD targets to establish the optimal dosing regimen for non-critically and critically ill patients with various renal functions.
Materials and Methods
Patients and Ethics
A single-center, prospective PopPK study was conducted at Fujian Medical University Union Hospital from July 2021 to September 2023. The study was approved by the Ethics Committee of Fujian Medical University Union Hospital (No. 2019KJCX034). The study was conducted according to the Declaration of Helsinki after informing all patients in our study of the study objectives and providing written consent to participate in this study. The inclusion criteria were as follows: (1) patients ≥ 18 years; (2) patients who received intravenous CAZ-AVI therapy for verified infection with CRKP. Exclusion criteria were applied to patients who were missing key information, or whose plasma concentration exceeded the detection limit. The treatment regimen of CAZ-AVI was determined by the healthcare team, with the dose and frequency adjusted according to the renal function of the patients.
The hospital electronic medical record system provided data on CAZ-AVI doses, frequencies, concentrations, demographic information (gender, age, height, weight, indication), acute physiology and chronic health evaluation II (APACHE II, with APACHE II; > 15 defined as critically ill and APACHE II ≤ 15 defined as non-critically ill),15 continuous renal replacement therapy (CRRT), and various laboratory metrics. These metrics included total bilirubin (TBIL), direct bilirubin (DBIL), total protein (TP), albumin (ALB), alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), alkaline phosphatase (ALP), serum creatinine (SCR), and CrCL, calculated using the Cockcroft-Gault equation.16
Sample Collection and Analysis
Considering patient compliance and ethical issues, a sparse sampling strategy was used to collect 1~3 blood samples at different time points post-infusion of the same dose after reaching a steady state (at least the sixth dose after starting CAZ-AVI therapy).17 The sampling time points were determined by the clinical healthcare team. Plasma concentrations of CAZ-AVI were quantified using our previously described method of liquid chromatography-tandem mass spectrometry (LC-MS/MS; Shimadzu JasperTM HPLC system coupled to an AB SCIEX Triple QuadTM 4500MD-ESI mass spectrometer, Singapore.18 The quantification method has been validated according to the bioanalytical validation guidelines of the US Food and Drug Administration.
PopPK Modeling
PopPK analyses were performed using Phoenix NLME (version 8.1, Pharsight, Mountain View, CA, USA). The model parameters were estimated using the first-order conditional estimation and extended least squares. The base model was determined based on previous reports6–9 and the fit of the data of our study. Inter-individual variability was described using an exponential residual model, while intra-individual variability was modeled with additive, proportional, and combined error structures. If a continuous covariate was missing, the median value of that covariate was used, and the highest frequent category was employed in cases where a categorical covariate was missing. Model discrimination was based on the −2 log likelihood (−2LL), with covariate screening including demographic and laboratory information. The covariates were added to the model after median normalization or as power functions. Covariate screening was performed using a stepwise forward inclusion method (a decrease in OFV > 3.84, p < 0.05) and a backward elimination method (an increase in OFV > 10.83, p < 0.001).
Model Evaluation
Goodness-of-fit (GOF) plots were utilized to evaluate the fit of the final model, including plots of observed concentration (DV) versus individual population prediction (IPRED) and population prediction (PRED), as well as plots of conditional weighted residuals (CWRES) versus time after the last dose (TAD) and PRED. The prediction-corrected visual predictive check (pc-VPC) was employed to assess the predictive accuracy of the final model by comparing the 90% confidence intervals (CIs) of simulated concentrations with 1000 replicates, against the distribution of actual observations. Furthermore, a bootstrap method was used to examine parameter estimation accuracy and model robustness by matching the final model parameter estimates to both the median and the 95% CI of the bootstrap parameter estimates.
Monte Carlo Simulation
In this study, different PK/PD targets were set for non-critically ill and critically ill patients. The targets were set based on improved clinical efficacy and inhibited the development of resistance. For non-critically ill patients, the PK/PD target was set at 50%fT > MIC for CAZ and 50%fT > 1 mg/L for AVI,19 while critically ill patients had a more stringent target of achieving 100% fT > 4 × MIC for CAZ and 100% fT > 4 mg/L for AVI.20 Monte Carlo simulation was performed based on the final model to assess the probability of target attainment (PTA) for optimal PK/PD targets with different regimens in non-critically ill and critically ill patients. The susceptibility breakpoint of CRKP for CAZ-AVI was a MIC of ≤ 8 mg/L.21 The free plasma concentrations of CAZ and AVI were 90% and 92% of the total plasma concentration, respectively.22,23 PTA evaluation was performed across various dosing regimens and MICs in a cohort of 1000 simulated patients with differing renal function statuses. Considering the time-dependent antimicrobial properties of CAZ-AVI, our study further explored the impact of extended infusion times on PTA in critically ill patients. Achieving the PK/PD target was defined as exceeding 90% of patients meeting both CAZ and AVI targets (>90% PTA).24 From a pharmacoeconomic perspective, the utilization of lower drug doses that ensure the attainment of the target PTA is associated with reductions in healthcare costs and alleviates the financial burden on families.10 Therefore, the optimal dosing regimen was defined as achieving the PK/PD target at the MIC breakpoint (MIC = 8 mg/L) while minimizing drug costs. We posit that reducing the dosage is feasible when the optimal regimens derived from our simulation result in a lower dosage than the recommended regimens in the instructions.
Results
Patients
A cohort of 45 patients, who contributed 91 plasma samples including 33 trough and 31 peak concentrations was enrolled in the PopPK analyses. Of these individuals, 29 patients with renal insufficiency (defined as CrCL < 90 mL/min),25 and 7 patients with ARC (defined as CrCL ≥ 130 mL/min).26 The median age among the patients was 59 years (range: 18 to 94 years), with 22 patients above 60 years. During the treatment period, 15 patients received CRRT. Except in special circumstances, the blood flow rate, pre-replacement fluid flow rate, and post-replacement fluid flow rate were set to 160 mL/min, 2000 L/h, and 1000 L/h, respectively. The dosing regimen was tailored to the renal function of each patient, with an infusion time of 2 hours. A dosing regimen of 2.5g q8h was employed in 12 non-critically ill patients and 17 critically ill patients. The demographic and clinical characteristics of all patients are presented in Table 1.
 |
Table 1 Demographics and Clinical Characteristicsa |
PopPK Modeling
The evaluation of the one-compartment and two-compartment models showed a better fit for the former (CAZ: OFVone-compartment: 963.6, OFVtwo-compartment: 984.8; AVI: OFVone-compartment: 688.7, OFVtwo-compartment: 735.2). A proportional residual model was applied to both models to assess residual variability. CrCL was identified as a significant covariate in both models after the covariate screening of demographic and laboratory information. Incorporating CrCL into the final model significantly reduced the inter-individual variability in the CLs of CAZ and AVI, from 72.73% and 82.40% to 55.71% and 66.69%, respectively. The estimated parameters of the final models are shown in Tables 2 and 3. All fixed-effects parameters were estimated with high precision, with relative standard errors (RSEs) < 30%. The final PK model equations for CAZ were as follows:
 |
Table 2 Population Pharmacokinetic Model Estimates and Bootstrap Results for Ceftazidime |
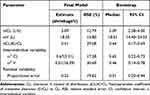 |
Table 3 Population Pharmacokinetic Model Estimates and Bootstrap Results for Avibactam |
where 2.96 is the typical value of CL, 17.76 is the typical value of V, 0.44 is the fixed parameter coefficient of CrCL, η is a random variable obeying a normal distribution with a mean of zero, and 71.3 is the median value of CrCL.
The final PK model equations for AVI were as follows:
where 3.09 is the typical value of CL, 18.25 is the typical value of V, 0.41 is the fixed parameter coefficient of CrCL, η is a random variable obeying a normal distribution with a mean of zero, and 71.3 is the median value of CrCL.
Model Evaluation
Figures 1 and 2 depict the GOF plots for the CAZ and AVI final models. The DV versus PRED and IPRED plots revealed a high degree of accuracy due to the good fit. Additionally, the CWRES versus PRED and TAD plots showed that the residuals were mainly distributed within −2 to 2, thereby manifesting the reliability of the models. Subsequently, Figure 3 shows the pc-VPC plots of CAZ and AVI concentrations versus TAD, confirming that the most of actual concentrations closely matched the 90% CIs of the simulated distribution, showing the predictive precision of the models.
The robustness of the CAZ and AVI models was further substantiated by Tables 2 and 3, which summarized the results of 1000 bootstrap simulations. The results show that all parameter estimates of the final model were within the 95% CIs obtained through the bootstrap method, and the deviation between the final model estimate and the bootstrap median parameter estimate was < 15% for all parameters. These results conspicuously demonstrate the stability and predictive accuracy of models.
Monte Carlo Simulation
Figures 4 and 5 present the PTA results for PK/PD targets in non-critically ill and critically ill patients, respectively. The results revealed a negative correlation between PTA and renal function in both patient groups within the same regimen, underscoring the necessity for tailored dosage adjustments. The data indicated that extended infusion times were significantly linked to improved PTAs at high MIC levels for critically ill patients. Additionally, Table 4 compares the recommended regimens in the instructions with the optimal regimens derived from our simulation results for both patients under different renal functions. For non-critically ill patients, the optimal dosing regimen identified in our study matches the instructions only in patients with a CrCL of 16–30 mL/min and > 90 mL/min. An increase in the dosage specified in the instructions is required for patients with CrCL ≤ 15 mL/min. Conversely, a reduction in the indicated dose is required for those with a CrCL of 31–90 mL/min. For critically ill patients, the regimen recommended in the instruction fails to achieve the higher exposure required, suggesting an adjustment to increase the dosage. Moreover, in critically ill patients with a CrCL > 30 mL/min, extending the infusion time is essential.
 |
Table 4 Comparison Between the Recommended Regimens in the Instructions and the Recommended Regimen From the Simulation Results in Our Study a,b |
Discussion
This study developed a PopPK model of CAZ-AVI in Chinese patients, and innovatively proposed optimal dosing regimens for non-critically ill patients aiming for 50%fT > MIC target, as well as for critically ill patients with 100%fT > 4 × MIC target in various renal functional statuses. Our findings revealed that the PopPK of CAZ-AVI is sufficiently characterized by a one-compartment model. CrCL was identified as a significant factor influencing the exposure of CAZ and AVI. Therefore, adjusting the CAZ-AVI dose based on renal function is imperative to ensure effective drug exposure. For critically ill patients, an increase in dosage and an extension of infusion times were deemed necessary to achieve a higher PK/PD target.
In our study, the one-compartment model demonstrated better fitting compared to the two-compartment model. Consequently, the one-compartment model was selected to describe the PK parameters of CAZ and AVI. However, a two-compartment model for CAZ and AVI was successfully developed in a PopPK study of adult indications.8 The discrepancy may be attributed to the smaller patient sample size in our study and the limited amount of plasma concentration data obtained, which were insufficient to build a more complex two-compartment model. Based on the final PopPK model in this study, the typical population values of CL for CAZ and AVI were 2.96 L/h and 3.09 L/h, respectively, and V for CAZ and AVI were 17.76 L and 18.25 L, respectively. These findings were consistent with the values of V from a PK study in healthy volunteers (VCAZ: 19.98 L, VAVI: 24.22 L). However, a notable difference was observed in the CL between our study and that study (CLCAZ: 8.14 L/h, CLAVI: 13.93 L/h),27 with our findings being significantly lower. This lower CL could be largely explained by the inclusion of 64.4% of patients with renal insufficiency in our study population, highlighting the potential impact of renal function on drug clearance. Furthermore, our results aligned closely with a study focused on a population with an average eGFR of 50 mL/min (CLCAZ: 3.2 L/h, CLAVI: 4.9 L/h).28 Although incorporating CrCL into the final models significantly reduced the inter-individual variability of CL, unexplained inter-individual variability remained in both models. Therefore, a larger-scale PopPK study incorporating more comprehensive covariates is warranted.
CAZ and AVI are excreted primarily by the kidneys.29 Therefore, renal functional status is the critical determinant of the CL of both drugs. The covariate analysis results showed that CrCL as a replacement indicator of renal function was the sole significant covariate influencing the CL of CAZ and AVI, which is consistent with previously reported studies.6–9 Despite including 33.3% of patients undergoing CRRT in our study, this factor exhibited no substantial effect on the PK of either drug. Some studies suggest that CRRT affects CL only in patients with severely impaired renal function (CrCL <10 mL/min).30–32 Since the patients with CRRT in our study had residual renal function (median CrCL for patients receiving CRRT: 69.3 mL/min), CRRT was found to be nonrelevant to CL. Li et al33 also supported the standard dosing regimen in patients receiving CRRT. However, given the small sample size of CRRT patients in our study, further research is needed to ascertain the extent to which CRRT affects the PK of both drugs.
Despite covariate analysis indicating that APACHE II scores do not significantly impact the PK of CAZ-AVI, research by Póvoa et al points out that alterations in blood flow distribution, plasma protein levels, and extracellular fluid volume among critically ill patients may influence the PK of β-lactam antibiotics.34 These alterations may result in standard dosages insufficient for achieving therapeutic drug concentrations.35 Moreover, the prevalence of deep-seated or multidrug-resistant infections in critically ill patients requires increased drug exposure to effectively manage such infections or minimize the development of resistance. Therefore, for critically ill patients, there is a compelling need to adjust the PK/PD targets from those for non-critically ill patients (50%fT > MIC for CAZ and 50%fT > 1 mg/L for AVI) to more stringent targets of 100% fT > 4 × MIC for CAZ and 100%fT > 4 mg/L for AVI.
In recent years, personalized medication has received increasing attention, emphasizing the adjustment of dosing regimes based on individual clinical conditions. The instruction supports using 2.5 g q8h (2-h infusion) as the standard dosing regimen for CAZ-AVI, with dose adjustment required only for patients with CrCL ≤ 50 mL/min,2 as shown in Table 4. However, studies have questioned these regimens. For instance, Teng et al suggested that patients with ARC may require a higher daily dose of CAZ-AVI than the standard dose.36 A multicenter observational study demonstrated a significant correlation between the adjustments of CAZ-AVI dosages and bacterial clearance rates.37 Also, inappropriate dosing may lead to drug accumulation in patients with renal insufficiency and sub-therapeutic exposures in patients with ARC.36 In addition, the different PK/PD targets of CAZ and AVI in non-critically ill and critically ill patients also dictate differences in optimal dosage regimens. Therefore, it is essential to tailor dosage regimens to individual clinical scenarios.
For non-critically ill patients, we found that the dosing regimens of instruction may be inadequate for patients with a CrCL ≤ 15 mL/min. In addition, our simulation results suggested a more cost-effective dosing regimen for patients with a CrCL of 31–90 mL/min compared to the instruction. In patients with CrCL ≤ 15 mL/min, the regimen based on instruction failed to achieve a PTA of > 90%, indicating a potential risk of treatment failure. Our simulations suggest a regimen of 0.94 g q24h (2-h infusion) for patients with a CrCL ≤ 5 mL/min, and a regimen of 0.94 g q12h (2-h infusion) for patients with a CrCL of 6–15 mL/min. In patients with a CrCL of 31–50 mL/min, our simulation results showed that a regimen of 1.25 g q12h (2-h infusion) effectively achieved > 90% PTA, contrasting with the instruction advocating the regimen of 1.25 g q8h (2-h infusion). Additionally, it was determined that the regimen of 1.25 g q8h (2-h infusion) was sufficient for patients with a CrCL of 51–90 mL/min, deviating from the recommended regimen of 2.5 g q8h (2-h infusion) from the instruction. These findings align with two dosing evaluation studies in China,10,38 and bolster the argument for a cost-effective dosing regimen for patients with a CrCL of 31–90 mL/min. It should be noted that the number of patients included in our study was relatively limited, necessitating a larger sample size to validate our simulation findings. Nonetheless, our study offers a detailed and innovative perspective on tailoring CAZ-AVI treatment for non-critical patients with renal insufficiency.
For critically ill patients, we found that the PTA of the recommended regimens in the instructions was far below 90%, significantly increasing the risk of treatment failure and the development of resistance. A study conducted on the continuous infusion of CAZ-AVI in critically ill patients indicated that extending the infusion time offers more benefits than adjusting the dosing regimen based on renal function in these patients.39 Similarly, our simulation results suggested that extended infusion should be considered in critically ill patients with CrCL > 30 mL/min. A key requirement for extended infusion is adequate drug stability after dilution. For CAZ-AVI, the reported stability extends up to 24 h at 2 to 8°C and up to 12 h below 25°C.2 Gatti et al40 and Tumbarello et al41 noted that extended infusion of CAZ-AVI was linked to higher clinical cure rates and lower mortalities. Furthermore, a study involving 10 patients with critical kidney disease who received a continuous infusion of CAZ-AVI demonstrated that none experienced CAZ-AVI-related adverse events during treatment, which indicated that extended infusion may not worsen renal dysfunction.40 Therefore, extended infusion of CAZ-AVI could be a feasible and desirable dosing strategy for critically ill patients. Han et al42 advocate for the routine use of a 4–6h infusion regime in critically ill patients. It must be emphasized that extended infusion time poses certain operational difficulties in real-world settings, particularly for critically ill patients with complex conditions and multiple medications. In such patients, extended infusion times remain a challenge. To address this, multi-channel infusion may be a viable solution.
Our study acknowledges several limitations that merit attention. Firstly, the scope of this research is limited to a single-center with a relatively small sample size which restricted our ability to develop a more complex two-compartment model, and 64.4% of the patients suffered from renal insufficiency which limited the generalizability of our results. Consequently, larger-sample studies are needed. Secondly, the lack of MIC data for the pathogens isolated from the patients limited our capacity to link the PTA results of our study with the tangible clinical outcomes observed in patients. Thirdly, there may have been some unexamined covariates, which prevented us from fully capturing inter-individual variability among patients. Therefore, more comprehensive covariate studies are needed. Fourthly, it is crucial to emphasize that the CrCL-based dose adjustments were tailored for patients with stable renal function. It has been shown that a significant portion of patients with acute kidney injury on admission experienced a reversal of their condition within 48 hours.43 In such cases, recalibrating doses based on initial CrCL may pose a risk for adverse outcomes. Consequently, implementing therapeutic drug monitoring coupled with strict renal function surveillance is advocated for these patients. To improve the clinical implementation of TDM, it is crucial to strengthen the collaboration within the medical team, including clinical pharmacists. Additionally, establishing more monitoring centers or offering remote monitoring services in regions with limited resources can improve the accessibility of TDM.44
Conclusion
In conclusion, this study successfully developed a PopPK model of CAZ-AVI in Chinese patients. It was determined that CrCL significantly influences the CL of CAZ-AVI. Monte Carlo simulation indicated that the recommended regimens in the instructions have limitations, necessitating adjustments to the dosing regimen based on the severity of the disease and renal functional status. Our study provides an innovative perspective on the individualized dosing of CAZ-AVI in non-critically ill patients with renal insufficiency. Additionally, extending the infusion times is necessary for critically ill patients. Our simulation results provide a reference for the clinical application of CAZ-AVI.
Abbreviations
ALB, Albumin; ALP, Alkaline phosphatase; ALT, Alanine aminotransferase; APACHE II, Acute physiology and chronic health evaluation II; ARC, Augmented renal function; AST, Aspartate aminotransferase; AVI, Avibactam; CAZ, Ceftazidime; CAZ-AVI, Ceftazidime-avibactam; CI, Confidence interval; CRRT, Continuous renal replacement therapy; CL, Clearance; CrCL, Creatinine clearance; CT, The threshold concentration; CWRES, Conditional weighted residuals; DBIL, Direct bilirubin; DV, Observed concentration; GGT, Gamma-glutamyl transferase; GOF, Goodness-of-fit; IPRED, Individual population prediction; MDR, Multidrug-resistant; MIC, The minimum inhibitory concentration; OFV, Objective function value; pc-VPC, Prediction-corrected visual predictive check; PD, Pharmacodynamic; PK, Pharmacokinetic; PopPK, Population pharmacokinetics; PRED, Population prediction; PTA, Probability of target attainment; SCR, Serum creatinine; TAD, Time after the last dose; TBIL, Total bilirubin; TP, Total protein; V, Volume of distribution.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
This work was supported by the Fujian Medical University Union Hospital Research and Ethics Committee (No. 2019KJCX034). The study was conducted according to the Declaration of Helsinki after informing all patients in our study of the study objectives and providing written consent to participate in this study.
Acknowledgment
The authors express gratitude to all patients who agreed to participate in the research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Fujian Province Joint Funds for the Innovation of Science and Technology (No. 2019Y9051 and No. 2021Y9038), Fujian Province Guiding Project of Science and Technology, (No. 2021Y0019), Fujian Province Natural ScienceFoundation of China (No. 2021J01761).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bonomo RA, Burd EM, Conly J, et al. Carbapenemase-producing organisms: a global scourge. Clin Infect Dis. 2017;66(8):1290. doi:10.1093/cid/cix893
2. European medicines agency summary of product characteristics: zavicefta. Available from: https://www.ema.europa.eu/en/documents/product-information/zavicefta-epar-product-information_en.pdf.
3. Paul M, Carrara E, Retamar P, et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European Society of Intensive Care Medicine). Clin Microbiol Infect. 2022;28(4):521–547. doi:10.1016/j.cmi.2021.11.025
4. Tamma PD, Aitken SL, Bonomo RA, et al. Infectious diseases society of America 2022 guidance on the treatment of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis. 2022;75(2):187–212. doi:10.1093/cid/ciac268
5. Nichols WW, Newell P, Critchley IA, et al. Avibactam pharmacokinetic/pharmacodynamic targets. Antimicrob Agents Chemother. 2018;62(6). doi:10.1128/aac.02446-17
6. Bensman TJ, Wang J, Jayne J, et al. Pharmacokinetic-pharmacodynamic target attainment analyses to determine optimal dosing of ceftazidime-avibactam for the treatment of acute pulmonary exacerbations in patients with cystic fibrosis. Antimicrob Agents Chemother. 2017;61(10):e00988–17. doi:10.1128/AAC.00988-17
7. Dimelow R, Wright JG, MacPherson M, et al. Population pharmacokinetic modelling of ceftazidime and avibactam in the plasma and epithelial lining fluid of healthy volunteers. Drugs R D. 2018;18(3):221–230. doi:10.1007/s40268-018-0241-0
8. Li J, Lovern M, Green ML, et al. Ceftazidime-avibactam population pharmacokinetic modeling and pharmacodynamic target attainment across adult indications and patient subgroups. Clin Transl Sci. 2019;12(2):151–163. doi:10.1111/cts.12585
9. Stein GE, Smith CL, Scharmen A, et al. Pharmacokinetic and pharmacodynamic analysis of ceftazidime/avibactam in critically ill patients. Surg Infect. 2019;20(1):55–61. doi:10.1089/sur.2018.141
10. Kang Y, Zhou Q, Cui J. Pharmacokinetic/pharmacodynamic modelling to evaluate the efficacy of various dosing regimens of ceftazidime/avibactam in patients with pneumonia caused by Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae: a multicentre study in northern China. J Global Antimicrob Resist. 2021;27:67–71. doi:10.1016/j.jgar.2021.07.020
11. Xu Y, Tang J, Yuan B, et al. A descriptive pharmacokinetic/pharmacodynamic analysis of ceftazidime‐avibactam in a case series of critically ill patients with augmented renal clearance. Pharmacol Res Perspect. 2023;12(1):e01163. doi:10.1002/prp2.1163
12. Roberts JA, Paul SK, Akova M, et al. DALI: defining antibiotic levels in intensive care unit patients: are current β-lactam antibiotic doses sufficient for critically ill patients? Clinl Infect Dis. 2014;58(8):1072–1083. doi:10.1093/cid/ciu027
13. Guilhaumou R, Benaboud S, Bennis Y, et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients—guidelines from the French Society of Pharmacology and Therapeutics (Société Française de Pharmacologie et Thérapeutique—SFPT) and the French Society of Anaesthesia and Intensive Care Medicine (Société Française d’Anesthésie et Réanimation—SFAR). Crit Care. 2019;23(1):104. doi:10.1186/s13054-019-2378-9
14. de Velde F, Mouton JW, de Winter BCM, et al. Clinical applications of population pharmacokinetic models of antibiotics: challenges and perspectives. Pharmacol Res. 2018;134:280–288. doi:10.1016/j.phrs.2018.07.005
15. Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi:10.1097/00003246-198510000-00009
16. Cockcroft DW, Gault H. Prediction of creatinine clearance from serum creatinine. Nephron. 2008;16(1):31–41. doi:10.1159/000180580
17. Mould DR, Upton RN. Basic concepts in population modeling, simulation, and model-based drug development. CPT. 2012;1(9):e6. doi:10.1038/psp.2012.4
18. Cheng Y, Chen M, Zhang B, et al. Rapid, simple, and economical LC-MS/MS method for simultaneous determination of ceftazidime and avibactam in human plasma and its application in therapeutic drug monitoring. J Clin Pharm Ther. 2022;47(9):1426–1437. doi:10.1111/jcpt.13693
19. Li J, Lovern M, Riccobene T, et al. Considerations in the selection of renal dosage adjustments for patients with serious infections and lessons learned from the development of ceftazidime-avibactam. Antimicrob Agents Chemother. 2020;64(4):e02105–19. doi:10.1128/AAC.02105-19
20. Gatti M, Pea F. Pharmacokinetic/pharmacodynamic target attainment in critically ill renal patients on antimicrobial usage: focus on novel beta-lactams and beta lactams/beta-lactamase inhibitors. Expert Rev Clin Pharmacol. 2021;14(5):583–599. doi:10.1080/17512433.2021.1901574
21. Nichols WW, Stone GG, Newell P, et al. Ceftazidime-avibactam susceptibility breakpoints against Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2018;62(11):e02590–17. doi:10.1128/AAC.02590-17
22. Berkhout J, Melchers MJ, van Mil AC, et al. Pharmacokinetics and penetration of ceftazidime and avibactam into epithelial lining fluid in thigh-and lung-infected mice. Antimicrob Agents Chemother. 2015;59(4):2299–2304. doi:10.1128/AAC.04627-14
23. O’Callaghan CH, Acred P, Harper PB, et al. GR 20263, a new broad-spectrum cephalosporin with anti-pseudomonal activity. Antimicrob Agents Chemother. 1980;17(5):876–883. doi:10.1128/AAC.1775.876
24. Gatti M, Rinaldi M, Bonazzetti C, et al. Could an optimized joint pharmacokinetic/pharmacodynamic target attainment of continuous infusion ceftazidime-avibactam be a way to avoid the need for combo therapy in the targeted treatment of deep-seated DTR Gram-negative infections? Antimicrob Agents Chemother. 2023;67(11):e00969–23. doi:10.1128/aac.00969-23
25. Wang M, Liu X, Tian Z. A 600 mg of fixed-dose linezolid in renally impaired patients versus 15 mg/kg intermittent dose-optimized vancomycin in renally non-impaired patients: a single centre retrospective analysis for adult patients with hospital-acquired pneumonia due to methicillin-resistant Staphylococcus aureus. Tropical Medicine and International Health. 2023;28(4):315–323. doi:10.1111/tmi.13866
26. Sahraei Z, Saffaei A, Darazam IA, et al. Evaluation of vancomycin pharmacokinetics in patients with augmented renal clearances: a randomized clinical trial. Front Pharmacol. 2022;13:1041152. doi:10.3389/fphar.2022.1041152
27. Merdjan H, Rangaraju M, Tarral A. Safety and pharmacokinetics of single and multiple ascending doses of avibactam alone and in combination with ceftazidime in healthy male volunteers: results of two randomized, placebo-controlled studies. Clin Drug Investig. 2015;35(5):307–317. doi:10.1007/s40261-015-0283-9
28. Falcone M, Menichetti F, Cattaneo D, et al. Pragmatic options for dose optimization of ceftazidime/avibactam with aztreonam in complex patients. J Antimicrob Chemother. 2020;76(4):1025–1031. doi:10.1093/jac/dkaa549
29. Marino A, Campanella E, Stracquadanio S, et al. Ceftazidime/avibactam and meropenem/vaborbactam for the management of Enterobacterales infections: a narrative review, clinical considerations, and expert opinion. Antibiotics. 2023;12(10):1521. doi:10.3390/antibiotics12101521
30. Kalaria SN, Armahizer M, McCarthy P, et al. A practice‐based, clinical pharmacokinetic study to inform levetiracetam dosing in critically ill patients undergoing continuous venovenous hemofiltration (PADRE‐01). Clin Transl Sci. 2020;13(5):950. doi:10.1111/cts.12782
31. Ulldemolins M, Vaquer S, Llauradó-Serra M, et al. Beta-lactam dosing in critically ill patients with septic shock and continuous renal replacement therapy. Critical Care. 2014;18(3):227. doi:10.1186/cc13938
32. Asín-Prieto E, Rodríguez-Gascón A, Trocóniz IF, et al. Population pharmacokinetics of piperacillin and tazobactam in critically ill patients undergoing continuous renal replacement therapy: application to pharmacokinetic/pharmacodynamic analysis. J Antimicrob Chemother. 2014;69(1):180–189. doi:10.1093/jac/dkt304
33. Li L, Li X, Xia Y, et al. Recommendation of antimicrobial dosing optimization during continuous renal replacement therapy. Front Pharmacol. 2020;11:786. doi:10.3389/fphar.2020.00786
34. Póvoa P, Moniz P, Pereira JG, et al. Optimizing antimicrobial drug dosing in critically ill patients. Microorganisms. 2021;9(7):1401. doi:10.3390/microorganisms9071401
35. Taccone FS, Laterre PF, Dugernier T, et al. Insufficient β-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care. 2010;14(4):R126. doi:10.1186/cc9091
36. Teng XQ, Qu Q, Luo Y, et al. Therapeutic drug monitoring of ceftazidime-avibactam concentrations in carbapenem-resistant K. pneumoniae-infected patients with different kidney statuses. Front Pharmacol. 2022;13:780991. doi:10.3389/fphar.2022.780991
37. Zhuang HH, Chen Y, Hu Q, et al. Efficacy and mortality of ceftazidime/avibactam-based regimens in carbapenem-resistant Gram-negative bacteria infections: a retrospective multicenter observational study. J Infection Public Health. 2023;16(6):938–947. doi:10.1016/j.jiph.2023.04.014
38. Dai Y, Chang W, Zhou X, et al. Evaluation of ceftazidime/avibactam administration in Enterobacteriaceae and Pseudomonas aeruginosa bloodstream infections by monte carlo simulation. Drug Des Devel Ther. 2021;15:2899–2905. doi:10.2147/DDDT.S309825
39. Cojutti PG, Pai MP, Gatti M, et al. An innovative population pharmacokinetic/pharmacodynamic strategy for attaining aggressive joint PK/PD target of continuous infusion ceftazidime/avibactam against KPC- and OXA-48- producing Enterobacterales and preventing resistance development in critically ill patients. J Antimicrob Chemother. 2024;79(11):2801–2808. doi:10.1093/jac/dkae290
40. Gatti M, Pascale R, Cojutti PG, et al. A descriptive pharmacokinetic/pharmacodynamic analysis of continuous infusion ceftazidime-avibactam in a case series of critically ill renal patients treated for documented carbapenem-resistant Gram-negative bloodstream infections and/or ventilator-associated pneumonia. Int J Antimicrob Agents. 2023;61(1):106699. doi:10.1016/j.ijantimicag.2022.106699
41. Tumbarello M, Raffaelli F, Giannella M, et al. Ceftazidime-avibactam use for Klebsiella pneumoniae Carbapenemase-Producing K. pneumoniae infections: a retrospective observational multicenter study. Clin Infect Dis. 2021;73(9):1664–1676. doi:10.1093/cid/ciab176
42. Han R, Sun D, Li S, et al. Pharmacokinetic/pharmacodynamic adequacy of novel β-lactam/β-lactamase inhibitors against Gram-negative bacteria in critically ill patients. Antibiotics. 2021;10(8):993. doi:10.3390/antibiotics10080993
43. Crass RL, Rodvold KA, Mueller BA, et al. Renal dosing of antibiotics: are we jumping the gun? Clinl Infect Dis. 2019;68(9):1596–1602. doi:10.1093/cid/ciy790
44. Abdulla A, van den Broek P, Ewoldt TMJ, et al. Barriers and facilitators in the clinical implementation of beta-lactam therapeutic drug monitoring in critically ill patients: a critical review. Therapeutic Drug Monitoring. 2022;44(1):112. doi:10.1097/FTD.0000000000000937
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Optimal Teicoplanin Dosage Regimens in Critically Ill Patients: Population Pharmacokinetics and Dosing Simulations Based on Renal Function and Infection Type

Wang Y, Yao F, Chen S, Ouyang X, Lan J, Wu Z, Wang Y, Chen J, Wang X, Chen C
Drug Design, Development and Therapy 2023, 17:2259-2271
Published Date: 1 August 2023










